Abstract
Background:
Increased impedance to flow in the uterine arteries assessed by value of the Doppler is associated with adverse pregnancy outcomes, especially pre-eclampsia. We investigated the predictive value of a uterine artery Doppler in the identification of adverse pregnancy outcomes such as ‘pre-eclampsia’ and ‘small fetus for gestational age’ (SGA).
Materials and Methods:
Three hundred and seventy-nine women, with singleton pregnancy, between 18 and 40 years of age, without risk factors, randomly underwent Doppler interrogation of the uterine arteries, between 16-22 weeks of gestation. Those who had a mean pulsatility index (PI) of >1.45 were considered to have an abnormal result, and were evaluated and compared with those who had normal results for adverse pregnancy outcomes, including pre-eclampsia and small for gestational age. The relationship between the variables was assessed with the use of the chi-square test.
Results:
There were 17 cases (4.5%) of abnormal uterine artery Doppler results and 15 of them (88.2%) developed pre-eclampsia and four cases (23.5%) had neonates small for gestational age. For predicting pre-eclampsia, the mean uterine artery PI had to be >1.45, had to have a specificity of 95.5% (95% CI, 70-92%), a sensitivity of 79% (95% CI, 43-82%), a negative predictive value (NPV) of 98.9% (95% CI, 72-96%), and a positive predictive value (PPV) of 88.2% (95% CI, 68-98%). In the case of ‘small for gestational age’ it had to have a specificity of 96.5% (95% CI, 42-68%), a sensitivity of 57% (95% CI, 53-76%), an NPV of 99.2% (95% CI, 70-92%), and a PPV of 23.5% (95% CI, 30-72%).
Conclusion:
Uterine artery Doppler evaluation at 16-22 weeks of gestation might be an appropriate tool for identifying pregnancies that may be at an increased risk for development of pre-eclampsia and small fetus for gestational age.
Keywords: Adverse pregnancy outcome, pre-eclampsia, uterine artery Doppler
INTRODUCTION
The addition of Doppler flow studies of maternal and fetal vessels has provided a tool where the physiology of the maternal — fetal unit can be evaluated.[1] The relationship between abnormal uterine artery Doppler velocimetry and pre-eclampsia and intrauterine growth restriction and adverse pregnancy outcomes are well-established.[2] Maternal hypertensive disorders are often associated with inadequate blood supply to the placenta.[2] An increased risk of maternal and fetal complications have been reported in women showing an increased resistance in the uterine arteries. Abnormal uterine artery Doppler findings have shown a significant correlation with the risk of adverse perinatal outcomes such as small for gestational age and admission to Neonatal Intensive Care Units (NICU).[3] Pregnancies that are destined to result in normal term deliveries show increased diastolic blood flow velocity and loss of the early diastolic notch by 22 weeks of gestation, while pregnancies that show persistent high resistance waveforms with early diastolic notches are at risk of preterm delivery, due to pre-eclampsia, abruption, and intrauterine growth restriction (IUGR).[4] It must be presumed that a reduction in uteroplacental blood flow alone, does not result in placental insufficiency, and therefore, does not necessarily trigger pre-eclampsia or reduce fetal growth.[4] Women who have failed to modify uterine artery blood flow by 20 weeks represent one of the highest risk groups in pregnancy, particularly for the development of preterm delivery, IUGR, and early onset of pre-eclampsia. Perhaps, the potential for stratifying care is the greatest benefit of mid-trimester uterine artery Doppler screening.[4] Zemel et al., has demonstrated that changes occur in the maternal circulation as early as the first trimester in women who develop pre-eclampsia and IUGR.[5] Second trimester uterine artery pulsatility index (PI) may add more information to the prediction process of pre-eclampsia.[4] Abnormal uterine artery Doppler flow velocimetry is defined as a mean PI more than 1.45 or/and the presence of bilateral early diastolic notches.[4] Although the uterine artery Doppler has a high negative predictive value for the prediction of adverse perinatal outcomes, the strength of the association between abnormal results and adverse events is not so considerable to justify its introduction as a screening test.[4] Screening is only worthwhile if an effective preventive treatment is available.[2] If we can identify the ‘at-risk’ fetus with the use of a Doppler, to apply clinical interventions, it may result in reduced perinatal deaths and unnecessary obstetric interventions.[2] In this study, we have investigated the predictive value of uterine artery Doppler for the identification of adverse pregnancy outcomes, specially pre-eclampsia and small for gestational age.
MATERIALS AND METHODS
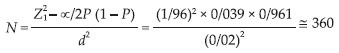
With regard to the 3.9% prevalence of pre-eclampsia[6] and according to the following formula with α = 0.05, P = 0.04, and d = 0.020, the minimum sample size would be 360.
Random sampling was used in this cross-sectional study. Three hundred and seventy-nine women with singleton pregnancy, between the age of 18 and 40 years, without any adverse obstetric or medical history, and between 16 and 22 weeks of gestational age, who referred to the Obstetric Outpatient Department in the Emam Khomeini Hospital, in Ahwaz, Iran, were selected for the purpose of this study, during 2011-2012. All the women who participated in this study were justified and selected according to their tendency and were free to quit whenever they liked. After getting their consent, those who were cooperative and interested in entering this study were submitted to Doppler interrogation on the uterine arteries. The methods of Doppler evaluation and the whole study process were initially posed in a committee established in the Ahvaz University of Medical Sciences, and all procedures were assessed and approved ethically by Local Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (research project number; U-90108). The blood flow measurements were performed by one permanent assessor by using the ‘Medison V10’ ultrasound machine equipped with a pulsed and color Doppler. The uterine artery blood velocity waveforms were recorded from both uterine arteries at the apparent crossover of the uterine and external illiac arteries with an insonation angle of <30 degrees, velocity >60 cm/second, and a sample volume of 2.0 mm. We used an abdominal probe in the lower lateral border of the uterus. The pulsatility index (PI) for each uterine artery was obtained by averaging the value of three consecutive waveforms. Next, the mean PI from the left and right uterine arteries was calculated. If the mean PI was more than 1.45, the flow velocity waveforms were considered abnormal.[4] There is not much difference between the abnormal pulsatility index values of the uterine artery Doppler from 16 to 19 weeks of gestations.[7,8] The patients were evaluated at 32 to 36 weeks of gestation for pregnancy complications such as pre-eclampsia, small fetus for gestational age, intrauterine fetal death, preterm delivery, and other adverse outcomes. After delivery, the patients and their medical files were evaluated for the detection of the above complications plus neonatal birth weight, gestational age at delivery time, and the neonatal admission into the NICU. Delivery information and perinatal outcomes were assessed according to the criteria of previously published clinical outcomes. Small for gestational age was defined as birth weight less than the tenth percentile for sex and gestational age.[6,9] Pre-eclampsia was defined as blood pressure ≥140/90 after 20 weeks of gestation and ≥1+ proteinuria in random urine samples, or ≥300 mg albumin in a 24-hour urine sample.[6] Preterm delivery was defined as delivery before 37 weeks of gestation.
Statistical analysis
For statistical analysis in this study, the following indices were used; sensitivity, specificity, positive predictive value and negative predictive value. The relationship between the variables was assessed with the use of the chi-square test.
RESULTS
Table 1 summarizes the pregnancy outcomes that were stratified by uterine arteries Doppler findings at 16-22 weeks of gestation. Among the 379 evaluated cases, who were between 18 to 40 years of age, 17 (4.5%) had abnormal uterine artery Doppler findings, which were defined by a mean pulsatility index of >1.45.
Table 1.
Perinatal outcomes and pre-eclampsia in women with abnormal uterine artery Doppler findings in comparison to those with normal results
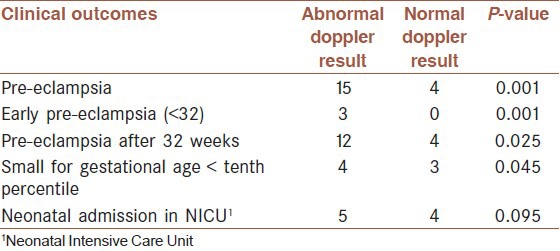
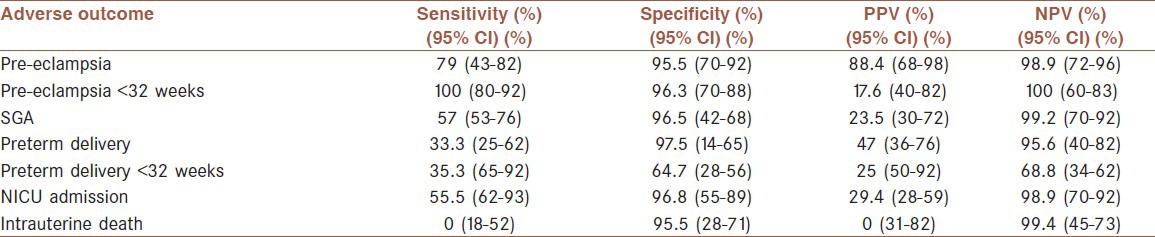
Pre-eclampsia occurred significantly more commonly in the group with an abnormal ultrasound examination at 16-22 weeks of gestation, in comparison to pregnancies with normal ultrasound findings; including 88.2 versus 1.1% for pre-eclampsia, developing after 20 weeks of gestation, and 17.6 versus 0% for pre-eclampsia developing before 32 weeks of gestation. There was a high prevalence of other adverse obstetric outcomes in the group with abnormal ultrasound examination, compared to those who had normal ultrasound findings, such as, preterm delivery before 37 weeks of gestation, 11.8 versus 1.4%; small fetus for gestational age, 23.5 versus 0.82%; and neonatal admission to the Neonatal Intensive Care Unit (NICU), 29.4 versus 1.1%. In this study, abnormal uterine artery Doppler findings at 16-22 weeks, which were defined as pulsatility index >1.45, had a specificity of 95.5%, a sensitivity of 79%, a negative predictive value (NPV) of 98.9%, and a positive predictive value (PPV) of 88.2%, for the prediction of pre-eclampsia. For a small for gestational age fetus, it had a specificity of 96.5%, a sensitivity of 57%, a NPV of 99.2%, and a PPV of 23.5%. In predicting preterm delivery, it had a specificity of 97.5%, a sensitivity of 33.3%, a NPV of 95.6%, and a PPV of 47%, [Tables 2 and 3].
Table 2.
The number of abnormal Doppler results for each adverse outcome
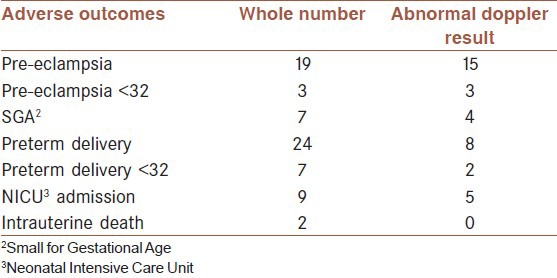
Table 3.
Sensitivity, specificity, and predictive values of abnormal Doppler results for each outcome
The findings showed that an abnormal uterine artery Doppler result had a high specificity and negative predictive value for predicting pre-eclampsia and neonatal complications like small for gestational age and neonatal admission to the NICU. Among all the cases with pre-eclampsia (19), there were five cases (26%) of fetuses small for gestational age and four of them had abnormal Doppler results and needed NICU admission. Nine cases (47%) of women with pre-eclampsia had preterm delivery (seven cases between 32-37 weeks and two cases before 32 weeks) and eight of them (88%) had abnormal Doppler result. Three cases with pre-eclampsia had developed this complication before 32 weeks, and hence, all of them had an abnormal Doppler result. Among 24 cases with preterm delivery, there were five cases of SGA, and four of them had abnormal Doppler findings.
DISCUSSION
Abnormal uterine artery Doppler result at 16-22 weeks is associated with adverse pregnancy outcomes; such as pre-eclampsia and small for gestational age. It can be used as a useful method for identifying high-risk pregnancies. Uterine artery PI >1.45 can provide further information for the prediction of these adverse outcomes, in order to conduct appropriate clinical interventions, to avoid perinatal morbidity.
According to a systematic review in 2004, which was done by Dr. Cristiane Barbieri, Doppler studies of uterine artery blood flow in the second trimester may be useful in predicting pre-eclampsia and/or intrauterine growth restriction (IUGR) (Campbell 1986-1993).[2] In normal pregnancy, the systolic to diastolic ratio or the resistance index (RI) values decrease significantly with advancing gestational age until 24-26 weeks. In the absence of this physiologic decrease, a higher incidence of hypertensive disorders and adverse perinatal outcomes could be expected. The advantage of PI and RI, among the different indices, is that they consist of the ratio of Doppler shift frequencies and thus are independent of the transmit frequency and Doppler angle.[2]
In 2005, in a research that was done by Becker R and Vonk R, uterine artery Doppler results at 20-23 weeks of gestation and adverse obstetric outcomes were evaluated.[10] They assessed the diagnostic value of Doppler sonography of the uterine arteries at 20-23 weeks as a screening procedure in a low-risk population. They evaluated uterine artery impedance in 7508 patients, using the mean PI of the left and right arteries or diastolic notching. The outcome variables were pre-eclampsia, IUGR, intrauterine/neonatal death, and preterm delivery, before 32 weeks. They showed a clear relationship between the elevation of impedance and the frequency of adverse pregnancy outcomes, with the frequency of complications varying from 3.2 to 38.4%. The mean PI in this study was considered to be 2 and they concluded that Doppler sonography of the uterine arteries at 20-23 weeks had the capacity to predict at least a part of the adverse pregnancy outcomes.[10] In our study, Doppler screening was done at 16-22 weeks and it had predicted pre-eclampsia and SGA with acceptable specificity and sensitivity.
Torres C and Raynor B et al., studied the uterine artery score and adverse pregnancy outcomes in a low-risk population during the second trimester in 2005.[11] The uterine artery score assigned one point to each abnormal parameter (RI >0.57, PI >1.0, S/D ratio >2.6 and notching) for each uterine artery, ranging from 0 (normal findings in both uterine arteries) to 8 (all abnormal in both arteries). Adverse outcomes included pre-eclampsia, IUGR, and preterm delivery before 37 weeks. A score of 5 or more was associated with significant differences in the outcomes. In predicting pre-eclampsia, the score of 5 or more had a specificity of 89.5%, a sensitivity of 25%, an NPV of 77%, and a PPV of 46%. For IUGR, the score had a specificity of 86.3%, a sensitivity of 16.7%, an NPV of 81%, and a PPV of 23%.[11] In our study, the mean PI of uterine artery Doppler measurement more than 1.45 was considered abnormal at 16-22 weeks, which was found in 4.5% of the patients. Abnormal Doppler findings in predicting pre-eclampsia had a specificity of 95.5%, a sensitivity of 79%, an NPV of 98.9%, and a PPV of 88.2%. For SGA it had a specificity of 96.5%, a sensitivity of 57%, an NPV of 99.2%, and a PPV of 23.5%.
Bower et al., examined the uterine arteries in 2058 pregnancies at 18-22 weeks.[12] Abnormal results were defined as an RI > ninety-fifth percentile or the presence of early diastolic notches in either of the two uterine arteries, which was found in 16% of the pregnancies. They found a sensitivity of 75% for pre-eclampsia and 46% for IUGR, and the specificity for both was 86%. The sensitivity for birth weight below the tenth percentile was 38%.
Valensise et al., examined the uterine arteries in 272 primigravidas at 22 weeks of gestation.[13] Abnormal results, including a mean RI of >0.58, were found in 9.6% of the patients. The sensitivity of the test to predict pre-eclampsia was 89% and for IUGR it was 67%. The specificity was 93% and 95%, respectively.
Toal M and Keating S et al., evaluated the adverse perinatal outcomes in high-risk women with abnormal uterine artery Doppler images and studied the prognostic role of abnormal uterine artery Doppler at 19-23 weeks of gestation, in 2007.[4] They also evaluated the placental shape and texture abnormalities in this gestation period. They showed that the combined abnormal uterine artery Doppler findings and placental dysmorphology identified a subset of women who were at risk for adverse outcomes, such as intrauterine fetal death, delivery before 32 weeks of gestation, and IUGR. In our study, Doppler screening was done at 16-22 weeks and we evaluated all the women with singleton pregnancies and without abnormal obstetric or medical history. We did not include the placental shape. The abnormal Doppler result had identified women at risk for pre-eclampsia, SGA, and also neonatal admission to the NICU.
In a study that was done by Kleinrouweler et al., in 2012, the second trimester uterine artery Doppler was evaluated for the identification of nulliparous women at risk for pre-eclampsia.[14] They included datasets in which patients’ characteristics, second trimester Doppler ultrasound findings, and the occurrence of pre-eclampsia in nulliparous women were available. Eight datasets containing 6708 women were used, and 302 cases (4.5%) developed pre-eclampsia. The best predictor of different Doppler findings was the combination of the mean PI or RI and bilateral notching. Addition of patients’ characteristics, body mass index (BMI) or blood pressure, improved the identification of women at risk for pre-eclampsia. In our study, a mean PI of >1.45 was used and 5% of the women developed pre-eclampsia, and 79% of them had abnormal uterine artery Doppler results. We did not include the patients’ characteristics and the Doppler had a PPV of 88.2% for the prediction of pre-eclampsia.
CONCLUSION
Abnormal uterine artery Doppler studies at 16-22 weeks may be associated with subsequent adverse outcomes. It can be a useful screening tool for pre-eclampsia and the associated perinatal morbidity, such as small for gestational age and preterm delivery. Nevertheless, to do interventions in order to prevent adverse outcomes based on abnormal Doppler results, more studies are needed.
ACKNOWLEDGMENTS
The authors greatly appreciate the Clinical Research Development Center, Imam Khomeini Hospital. They thank the research deputy of Ahvaz Jundishapur University of Medical Sciences for the financial support (by a revised Urmia University of Medical Sciences that was approved by WMA). This study is based on a thesis of Dr. L Ahmadi that was conducted by the first author.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Scission A, Hayes E. Uterine artery Doppler Flow studies in obstetric practice. Am J Obstet Gynecol. 2009;201:121–6. doi: 10.1016/j.ajog.2009.03.027. [DOI] [PubMed] [Google Scholar]
- 2.Barbieri C. Doppler ultrasound in high risk pregnancies. Department of Obstet Gynecol of the Center for Integral Attention to Women's Health. [Last accessed on 2010 Oct 6]. Available from: http://www.gfmeroch/Medical_education_En/PGC-RH-2004/barbieri_review.htm .
- 3.Ghi T, Youssef A, Piva M, Contro E, Segata M, Guasina F, et al. The prognostic role of uterine artery Doppler studies in patients with late — onset pre-eclampsia. (e1-5).Am J Obstet Gynecol. 2009;201:36. doi: 10.1016/j.ajog.2009.02.024. [DOI] [PubMed] [Google Scholar]
- 4.Toal M, Keating S, Machin G, Dodd J, Adamson SL, Windrim RC, et al. Determinants of adverse perinatal outcome in high — risk women with abnormal uterine artery Doppler images. Am J Obstet Gynecol. 2008;198:330.e1–330- e7. doi: 10.1016/j.ajog.2007.09.031. [DOI] [PubMed] [Google Scholar]
- 5.Harrington K. Early Screening for pre-eclampsia and intrauterine growth restriction. Ultrasound Obstet Gynecol. 2011;37:623–4. doi: 10.1002/uog.9018. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham F, Leveno J, Bloom L, Hauth C, Rouse J, Spong Y. University of Texas Southwestern Medical Center at Dallas Parkland Health and Hospital System. 23rd ed. Chapters: 16,34,36,38. New York: McGraw Hill; 2010. Williams Obstetrics. [Google Scholar]
- 7.Gómez O, Figueras F, Fernández S, Bennasar M, Martínez JM, Puerto B, et al. Reference ranges for uterine artery mean pulsatility index at 11–41 weeks of gestation. Ultrasound Obstet Gynecol. 2008;32:128–32. doi: 10.1002/uog.5315. [DOI] [PubMed] [Google Scholar]
- 8.Sritippayawan S, Phupong V. Risk Assessment of Pre-eclampsia in Advanced Maternal Age by Uterine Arteries Doppler at17-21 Weeks of Gestation. J Med Assoc Thai. 2007;90:1281–6. [PubMed] [Google Scholar]
- 9.Tschudy KM. Harriet lane handbook. In: Arcara MM, editor. 19th ed. Chapter 21. Maryland, US: The Johns Hopkins Hospital; 2012. pp. 252–527. [Google Scholar]
- 10.Becker R, Vonk R, Vollert W, Entezami M. Doppler Sonography of uterine arteries at 20-23 weeks: Risk assessmen of adverse pregnancy outcome by quantification of impedance and notch. J Perinat Med. 2005;30:388–94. doi: 10.1515/JPM.2002.060. [DOI] [PubMed] [Google Scholar]
- 11.Torres C, Raynor B. Uterine artery score and adverse pregnancy outcomes in a low- risk population. Am J Obstet Grynecol. 2005;193:s167. [Google Scholar]
- 12.Bower S, Schuchter K, Campbell S. Doppler Ultrasound screening as part of routine antenatal scanning: Prediction of pre-eclampsia and intrauterine growth retardation. Br J Obstet Gynaecol. 1993;100:989–94. doi: 10.1111/j.1471-0528.1993.tb15139.x. [DOI] [PubMed] [Google Scholar]
- 13.Valensise H, Bezzeccheri V, Rizzo G, Tranquilli AL, Garzetti GG, Romanini C. Doppler velocimetery of uterine artery as a screening test for gestational hypertension. Ultrasound Obstet Gynecol. 1993;3:18–22. doi: 10.1046/j.1469-0705.1993.03010018.x. [DOI] [PubMed] [Google Scholar]
- 14.Kleinrouweler CE, Bossuyt PM, Thilaganathan B, Vollebregt KC, Ramírez JA, Ohkuchi A, et al. The added value of second trimester uterine artery Doppler in the identification of nulliparous women at increased risk for pre-eclampsia. Am J Obstet Gynecol. 2012;20:s182–3. doi: 10.1002/uog.12435. [DOI] [PubMed] [Google Scholar]


