Abstract
Background:
In Iran, burns are the second most common cause of death, after traffic accidents in individuals under the age of 15 years. Many burned patients die or suffer injury due to lack of immediate care, so we need to use an alternative resuscitations to cure them immediately. Telemedicine describes the use of medical information exchanged from one site to another via electronic communications to improve patients’ health status and care. The aim of this study was to express the advantages of Telemedicine to resuscitate and care burn patients.
Materials and Methods:
This study was a narrative review. The literature was searched on fast resuscitation and care of the patients’ burn by telemedicine with the help of libraries, databases, and also searches engines available at Google, Google scholar, books and conference proceedings. In our searches, we employed the following keywords and their combinations: Telemedicine, Telecare, Burn, Burn patient, Air transport, Triage and Health Information Management in the searching areas of titles, keywords, abstracts and full texts.
Results:
In this study, more than 78 articles and reports were collected and 30 of them were selected based on their relevancy.
Conclusion:
Acute evaluation of burn patients can be performed by the telemedicine and it plays an important role in improving access to the required expertise, and raises physician confidence in treating burn patients. This can reduce under-triage or over-triage for air transport and finally lead to saving time and cost.
Keywords: Air transport, burn, patient, telemedicine, telecare, triage
INTRODUCTION
Burns have significant short- and long-term consequences for patients and their families, and are one of the most serious injuries to mankind. Outcomes for burn patients have improved dramatically over the past 20 years; however, burns still cause substantial morbidity and mortality.[1,2,3] Morbidity and mortality rise with the increasing burned surface area. It also rises with the increasing age so that even small burns may be fatal in elderly people.[4] The depth of a burn wound and/or its healing potential are the most important determinants of the therapeutic management and of the residual morbidity or scarring. So it is important to estimate the depth of the burn to assess its severity and to plan future wound care.[5] Fire is the fifth leading cause of unintentional injury and the third leading cause of fatal home injury in the United States.[6] Also, burns are the major cause of death and disability worldwide, particularly in developing countries. In Iran, burns are the second most common cause of death, after traffic accidents, among individuals under the age of 15 years.[7] Also, many burned patients die because of lack of immediate care, due to which injury becomes more severe and patients become more compromised.[1] Hence, we need to use an alternative resuscitate and care to treat them immediately.
The patients’ care should be a high priority at the emergency department (ED) for acute patient situations. The ED provides urgent clinical and para-clinical care (such as lab test, radiology, electrocardiogram) for patients that injured in accidents and incidents. The injured patients need urgent treatment according to their injury circumstances and injury rather than situations. These patients should receive resuscitative treatments in the shortest time.[8] Therefore, adequate and effective emergency management of the burn patient during the first few hours postburn can prevent the burn wound from progressing and becoming infected, and facilitate faster healing and rehabilitation and long-term functionality.[1,9] Telemedicine means use of medical information exchanged from one site to another via electronic communications for the health and education of the patient or healthcare provider and for the purpose of improving patient care.[10]
Telemedicine is one of the solutions that is useful. Recent developments in information and communications technology have the potential to revolutionize health care. The telemedicine is one of the most successful techniques in this rapidly expanding field.[11]
Of course, all technologies have weaknesses but in order to reduce them we need to recognize their weaknesses. In health management systems, information has a special role in planning, evaluation, and managing.[12] In fact, the first distinctions between developed and developing countries are the production, application, distribution and utilization of information. In this way, new technologies should help healthcare providers.[13,14,15]
It is a rapidly expanding technology involving the exchange of medical information to assist diagnosis and treatment at a distance.[16] The aim of this study was to express advantages of the Telemedicine to resuscitate and care burn patients.
MATERIALS AND METHODS
This study was a narrative review. The literature was searched for the telemedicine applications for fast resuscitation and care of the patients’ burn. Our study was divided into three phases: Literature collection, assessing, and selection. Researchers identified studies that denoted advantages of applying the telemedicine for burn patients. The literature search was conducted with the help of library search engines available at Google, Google scholar, books, and conference proceedings. The search was performed in early May in 2012 until March 2013 to ensure that our literature review is most up-to-date. In our searches, we employed the following keywords and their combinations: Telemedicine, telecare, burn, burn patient, air transport, triage, and health information management in the searching areas of titles, keywords, and abstracts from 1999-2013. Search results were reviewed for relevance to burn patients. Studies that did not report an application of telemedicine for burn patients were excluded. More than 78 articles were collected and assessed 30 of them were selected based on their relevancy.
The last phase followed our proposed research framework and conducted detailed analysis with regard to the literature. We studied how the telemedicine was applied for fast resuscitation and care of the patients’ burn by analyzing the research prototypes, pilot studies and case studies in our collected literature; we identified the benefits of telemedicine adoption for burn patients. These implications can be used to guide future research in this field.
RESULTS
Although Rafii et al. mentioned that to date, few studies have been conducted on this subject in Iran, and the findings of these studies rather inconsistent.[7] According to Tehrantimes News, in 2012, 2,026 people lost their lives from burns in Iran out of which 1033 were women and 993 were men.[17] Burn injuries in Iran are much more common than in the United States and Europe.[18] Although, Iran has a well-developed system of rural health workers and clinics, covering most border areas, they need to consult with specialists for resuscitating burn patients.
It appears that telemedicine can be useful for burn patients. For example, telemedicine increases the effectiveness of treatment, and it is also involved in the training of less experienced surgeons and follow-up of burned patients.[19]
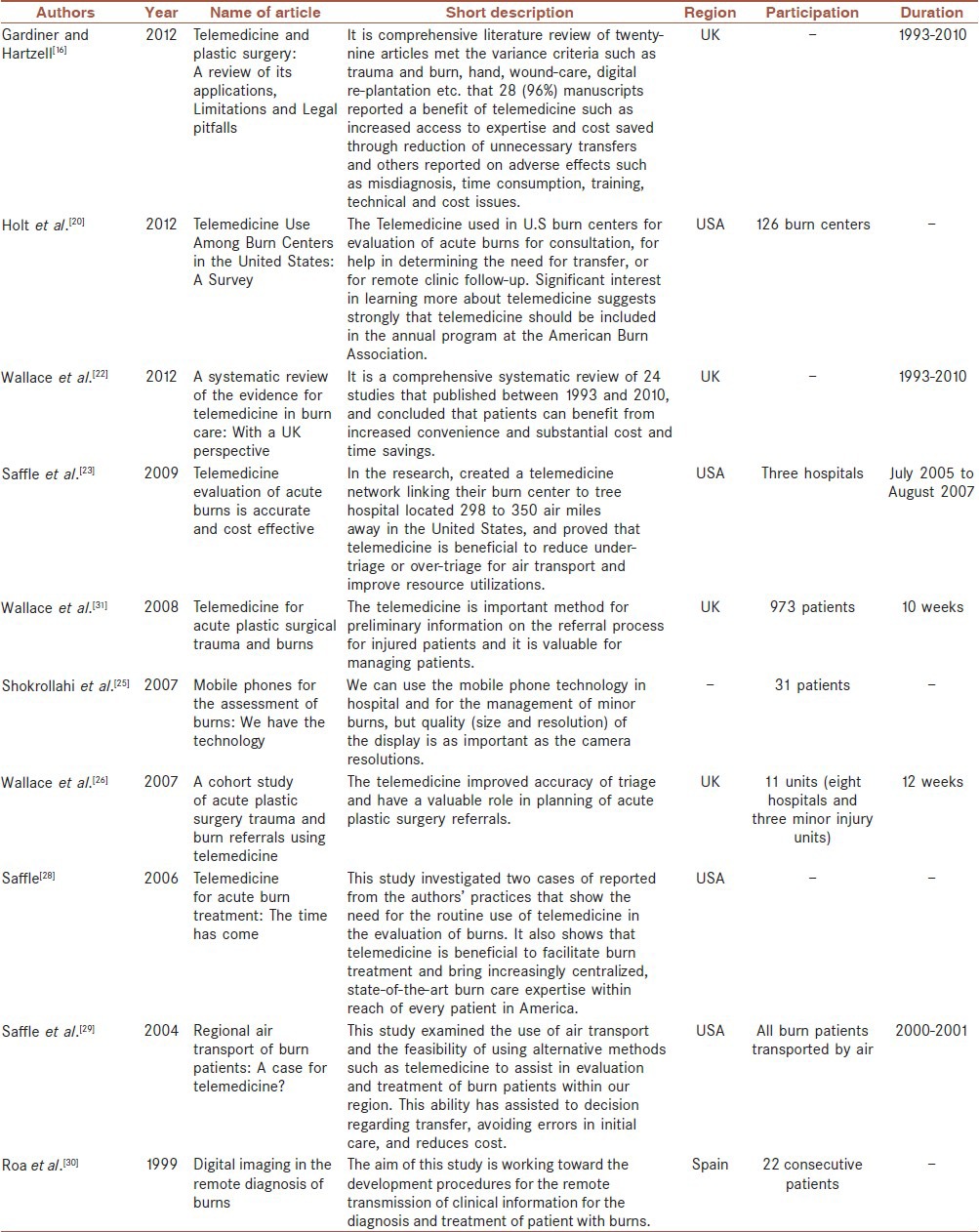
In these reviewed papers, we have included several other studies that bring additional viewpoints and use cases for this article [Table 1].[5,15,20,21,22,23,24,25,26,27,28,29,30]
Table 1.
Telemedicine and burn patients at a glance in some countries
The telemedicine is beneficial for assessment of burn depth and burn wound healing potential that it is especially important in the early hours after burns in accident and emergency department, where decision for treat or refer needs to be made.[5] Telemedicine can encourage appropriate measures to respond to minor and major burns.[23]
Saffle et al. mentioned, ‘the ability to evaluate burn patients by telemedicine may have the potential to assist decisions regarding transfer’.[29]
‘For patients with major burns, the telemedicine evaluation helped speed preparation of appropriate critical care and justify the expense and risks of air transport; patients with lesser burns were quickly identified for economical ground transport or given definitive local choir’.[23] For example one study by Shokrollahi et al. showed that ‘Camera phones appear to be reliable for the assessment of Total Burn Surface Area (TBSA) and burn depth in mirror burns. Although not assessed directly in this study, it is likely that major burns can also be estimated successfully in this way’.[25] But, how can evaluate and treatment of burns patient by telemedicine be done?
The telemedicine plays an important role in improving access to the required expertise for the burn patients. Nowadays the telemedicine is important within the field of plastic surgery. It can improve access to a highly demanded specialty and facilitate the provision of expertise at remote sites.[16] Wallace et al. expressed in their article ‘we observed improved access, earlier and more frequent senior clinician involvement by the use of the telemedicine in burn treatment’.[31]
As a result, the telemedicine raises physician confidence in treating patients.
It permits other members of the burn team, including therapists and psychologists, to participate, as well as their counterparts at the remote centre.[32]
Telemedicine images provide the qualitative benefit of confidence in the referring clinical information, as the receiving clinician seems to validate (or not) information by viewing the images, which allows greater certainty in management decisions and priority of triage.[22]
Consequently, the telemedicine reduces the need to air transport burned patient and have an important role in the triage and planning for management of patients.
Acute evaluation of burn patients by the telemedicine can reduce under-triage or over-triage for air transport.[23]
For example, in a study performed in Denmark in the duration of 3 months 97 burn patients were transferred to treatment at the national burn center. Thirty percent of these referrals were unnecessary according to the guidelines. The using of digital image transfers before admission of burn patients reduces both over-and under-triage and have a beneficial effect on the economy.[31] Also, Saffle et al. argued that ‘we created a telemedicine network between our center and three other hospitals in Idaho and Montana located 300-400 miles from the Salt Lake City. During the period of the project, 10 patients were seen by the telemedicine, while 10 were referred directly, compared to 28 patients who had all been transported by air during a prior 2-year period, overall the telemedicine has been effective in reducing patient transfers’.[23]
Mobile Tele-dermatology is as a triage system for individuals with skin lesions. It may be useful for travelers or people living in under-served areas such as rural patients.[22]
Therefore, the telemedicine helps to burn patients or patients who are in deprived areas.
Saffle findings showed that rural patients are at increased risk of death from burns that many of these problems with access to health care that the telemedicine could do much to solve.[28]
These finally lead to saving time and expense, through the reduction of inappropriate patient transfer and face-to-face follow-up.[16]
According to another study by Saffle et al. ‘the ability to evaluate burn patients by the telemedicine may have the potential to assist decisions regarding transfer, avoid errors in initial care, and reduce cost’.[29]
CONCLUSION
Acute evaluation of burn patients can be performed by the telemedicine and it plays an important role in improving access to the required expertise, and raises physician confidence in treating burn patients. This can reduce under-triage or over-triage for air transport and finally lead to saving time and cost. Therefore, telemedicine is effective in fast resuscitation and care of the patients’ burn and we should specially use of this technique for rural and inaccessible areas.
RECOMMENDATIONS
In many countries, including Iran, there are no accurate statistics of burn patients. Therefore, the researchers recommend that information of burn patients and damaged areas collect and transfer to academic centres to recognize required equipment and facilities and screen victims. Then this information through portable equipment can transfer to healthcare centres and other care organizations.
Public education about these technologies is necessary in order to know how to report critical information to health workers and policymakers.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Grobler RC. Emergency management of the patient with severe burns in the emergency unit. Prof Nurs Today. 2012;16:37–45. [Google Scholar]
- 2.Mirmohammadi SJ, Mehrparvar AH, Kazemeini K, Mostaghaci M. Epidemiologic characteristics of occupational burns in yazd, Iran. Int J Prev Med. 2013;4:723–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Fatemi MJ, Salehi H, Akbari H, Alinejad F, Saberi M, Mousavi SJ, et al. The effect of levamisole on mortality rate among patients with severe burn injuries. J Res Med Sci. 2013;18:795–800. [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. Management of Burns. World Health Organization. 2007. [Last accessed on 2012 Dec 15]. Available from: http://www.who.int/surgery/publications/Burns_management.pdf .
- 5.Monstrey S, Hoeksema H, Verbelen J, Pirayesh A, Blondeel P. Assessment of burn depth and burn wound healing potential. Burns. 2008;34:761–9. doi: 10.1016/j.burns.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Ortiz-Pujols SM, Thompson K, Sheldon GF, Fraher E, Ricketts T, Cairns BA. Burn care: Are there sufficient providers and facilities? Bull Am Coll Surg. 2011;96:33–7. [PubMed] [Google Scholar]
- 7.Rafii MH, Saberi HR, Hosseinpour M, Fakharian E, Mohammadzadeh M. Epidemiology of Pediatric Burn Injuries in Isfahan, Iran. Arch Trauma Res. 2012;1:27–30. doi: 10.5812/atr.5295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ajami S, Ketabi S, Yarmohammadian MH, Bagherian H. Wait time in Emergency Department (ED) Processes. Med Arch J. 2012;66:34–8. doi: 10.5455/medarh.2012.66.53-57. [DOI] [PubMed] [Google Scholar]
- 9.Burns. MedlinePlus Medical Encyclopedia. 2012. [Last accessed on 2012 Dec 15]. Available from: http://www.Nlm.nih.gov/medlineplus/ency/article/000030.htm .
- 10.WebMd. Webster's new world medical dictionary: Webster's new world. 2008 [Google Scholar]
- 11.Benger J. A review of telemedicine in accident and emergency: The story so far. J Accid Emerg Med. 2000;17:157–64. doi: 10.1136/emj.17.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ajami S, Torabian F. Mobile technology in healthcare. J Inform Tech Soft Engg. 2013;S7:e006. [Google Scholar]
- 13.Ajami S, Arzani-Birgani A. The use of telemedicine to treat prisoners. J Inform Tech Soft Engg. 2013;7:2. [Google Scholar]
- 14.Ajami S, Mohammadi-Bertiani Z. Training and its Impact on Hospital Information System (HIS) Success. J Inform Technol Soft Engg. 2012;2:1–7. [Google Scholar]
- 15.Ajami S, Lamoochi P. Applying Telemedicine During Disasters. J Inform Tech Soft Engg. 2013;S7:e005. [Google Scholar]
- 16.Gardiner S, Hartzell TL. Telemedicine and plastic surgery: A review of its applications, limitations and legal pitfalls. J Plast Reconstr Aesthet Surg. 2012;65:e47–53. doi: 10.1016/j.bjps.2011.11.048. [DOI] [PubMed] [Google Scholar]
- 17.TEHRANTIMES. 2,000 burn deaths recorded in Iran last year. Tehran. 2013. [Last accessed on 2012 Dec 15]. Available from: http://www.tehrantimes.com/society/107791-2000-burn-deaths-recorded-in-iran-last-year .
- 18.Hasani L, Aghamolei T, Boushehri E, Sabili A. Analysis of hospitalized burned patients in Bandar Abbass, Iran. J Res Health Sci. 2009;9:50–3. [PubMed] [Google Scholar]
- 19.Turk E, Karagulle E, Aydogan C, Oguz H, Tarim A, Karakayali H, et al. Use of telemedicine and telephone consultation in decision-making and follow-up of burn patients: Initial experience from two burn units. Burns. 2011;37:415–9. doi: 10.1016/j.burns.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Holt B, Faraklas I, Theurer L, Cochran A, Saffle JR. Telemedicine Use Among Burn Centers in the United States: A Survey. J Burn Care Res. 2012;33:157–62. doi: 10.1097/BCR.0b013e31823d0b68. [DOI] [PubMed] [Google Scholar]
- 21.Wallace D, Pickford M. The role of telemedicine in the management of acute trauma referrals to a regional Plastic and Hand Surgery unit in the South East of England. Telemedicine techniques and applications. InTech. 2011 [Google Scholar]
- 22.Wallace D, Hussain A, Khan N, Wilson Y. A systematic review of the evidence for telemedicine in burn care: With a UK perspective. Burns. 2011;38:465–80. doi: 10.1016/j.burns.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 23.Saffle JR, Edelman L, Theurer L, Morris SE, Cochran A. Telemedicine evaluation of acute burns is accurate and cost-effective. J Trauma. 2009;67:358–65. doi: 10.1097/TA.0b013e3181ae9b02. [DOI] [PubMed] [Google Scholar]
- 24.Ebner C, Wurm EM, Binder B, Kittler H, Lozzi GP, Massone C, et al. Mobile teledermatology: A feasibility study of 58 subjects using mobile phones. J Telemed Telecare. 2008;14:2–7. doi: 10.1258/jtt.2007.070302. [DOI] [PubMed] [Google Scholar]
- 25.Shokrollahi K, Sayed M, Dickson W, Potokar T. Mobile phones for the assessment of burns: We have the technology. Emerg Med J. 2007;24:753–5. doi: 10.1136/emj.2007.046730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wallace DL, Smith RW, Pickford MA. A cohort study of acute plastic surgery trauma and burn referrals using telemedicine. J Telemed Telecare. 2007;13:282–7. doi: 10.1258/135763307781644933. [DOI] [PubMed] [Google Scholar]
- 27.Jones S, Milroy C, Pickford M. Telemedicine in acute plastic surgical trauma and burns. Ann R Coll Surg Engl. 2004;86:239–42. doi: 10.1308/147870804344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saffle JR. Telemedicine for acute burn treatment: The time has come. J Telemed Telecare. 2006;12:1–3. doi: 10.1258/135763306775321353. [DOI] [PubMed] [Google Scholar]
- 29.Saffle JR, Edelman L, Morris SE. Regional air transport of burn patients: A case for telemedicine? J Trauma. 2004;57:57–64. doi: 10.1097/01.ta.0000103992.21727.8f. [DOI] [PubMed] [Google Scholar]
- 30.Roa L, Gomez-Cia T, Acha B, Serrano C. Digital imaging in remote diagnosis of burns. Burns. 1999;25:617–23. doi: 10.1016/s0305-4179(99)00053-4. [DOI] [PubMed] [Google Scholar]
- 31.Wallace D, Jones S, Milroy C, Pickford M. Telemedicine for acute plastic surgical trauma and burns. J Plast Reconstr Aesthet Surg. 2008;61:31–6. doi: 10.1016/j.bjps.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 32.Latifi R. USA: ARTECH HOUSE; 2010. Telemedicine for trauma, emergencies, and disaster management. [Google Scholar]


