Abstract
Melasma is a chronic acquired hypermelanosis of the skin, characterized by irregular brown macules symmetrically distributed on sun-exposed areas of the body, particularly on the face. It is a common cause of demand for dermatological care that affects mainly women (especially during the menacme), and more pigmented phenotypes (Fitzpatrick skin types III-V). Due to its frequent facial involvement, the disease has an impact on the quality of life of patients. Its pathogeny is not yet completely understood, although there are some known triggering factors such as sun exposure, pregnancy, sexual hormones, inflammatory processes of the skin, use of cosmetics, steroids, and photosensitizing drugs. There is also a clear genetic predisposition, since over 40% of patients reported having relatives affected with the disease. In this manuscript, the authors discuss the main clinical and epidemiological aspects of melasma.
Keywords: Contraceptives, Oral contraceptives, Pregnancy, Hormones, Gonadal steroid hormones, Melanosis, Pigmentation, Skin pigmentation, Ultraviolet rays, Pigmentation disorders
INTRODUCTION
Melasma is a human melanogenesis dysfunction that results in localized, chronic acquired hypermelanosis of the skin. It occurs symmetrically on sunexposed areas of the body, and affects especially women in menacme.1
The word melasma originates from the Greek root "melas", which means black, and refers to its brownish clinical presentation. The designations: "mask of pregnancy", liver spots, uterine chloasma, chloasma gravidarum, and chloasma virginum do not fully characterize the disease, nor are semantically appropriate, although the term "chloasma" (derived from the Latin chlóos and the Greek cloazein: greenish) is still used in the medical literature.1-4
Disease descriptions can be found in the medical literature extending as far as the reports of Hippocrates (470-360 BC). The term was used to designate a series of cutaneous melanization processes, and its worsening was reported to happen after sun exposure, fire heat, cold and skin inflammations. Many years later, Joseph Plenck, in his book "Doctrine of Morbis cutaneis" identified seven variants of melasma, which he called the Ephelis (from the Greek: small spot): solaris, ignealis, vesticario, gravidarum, hepatica, dismenorrhoealis e haemorrhoidalis.5
Seminal reports on melasma in the Western medical literature date back to 1934 and 1961, respectively. In the first, the author describes the case of a 20year-old woman from London (England), who presented with brownish, upper lip lesion with welldefined margins and history of worsening after sun exposure.2 In the second, the authors described in detail the cases of 15 patients between 25 and 43 years of age, from the region of Los Angeles (USA), who presented with symmetrical hyperpigmentation of the face of unknown etiology. Among the 14 women in the study, ten got pregnant and four reported having "melanosis of pregnancy".6
EPIDEMIOLOGY
Melasma is a common dyschromia that often motivates the search for dermatological care. Its populational prevalence varies according to ethnic composition, skin phototype, and intensity of sun exposure.
In a 2010 population-based study, 1500 adults from several Brazilian states were surveyed. Pigmentation disorders were reported as the main cause of demand for dermatological care by 23.6% of men and 29.9% of women.7
According to a survey of 57,343 diagnoses performed at dermatological consultations in Brazil that was conducted by the Brazilian Society of Dermatology (BSD) in 2006, melanodermias (among them, melasma) represented the third largest group of diseases in dermatological practice, accounting for 8.4% of all complaints. This prevalence varied from 5.9% to 9.1% in the different regions of the country.8
A study conducted in Nepal in 2008 with 546 dermatological patients evidenced melasma as the fourth most frequent diagnosis and the first most commonly reported pigmentary dermatosis.9 In addition, a retrospective study conducted in Saudi Arabia, which analyzed data from 1076 dermatology patients, also described pigmentary changes as the fourth most common dermatosis.10
Another study conducted with 2,000 dermatological patients of black origin in Washington, DC, revealed that the third most commonly-cited skin disorders were pigmentary problems other than vitiligo. Of these patients, the majority had a diagnosis of postinflammatory hyperpigmentation, followed in frequency by melasma.11
The populational incidence of melasma is not precisely known. Changes occurred in recent decades due to the increase in sun exposure time spent by the population during leisure and daily activities were not substantiated in studies.12
It is known that melasma occurs in all ethnic and population groups. However, epidemiological studies have reported higher prevalence among more pigmented phenotypes, such as East Asians (Japanese, Korean and Chinese), Indian, Pakistani, Middle Eastern and Mediterranean-African. In the Americas, it is common among Hispanic-Americans and Brazilians who live in intertropical areas, where there is greater exposure to ultraviolet radiation (UVR).13-15
In a 2013 population-based study involving 515 adult employees of the University Campus of Botucatu, Sao Paulo State University, SP (Brazil), melasma was identified in 34% of women and 6% of men.16
The large miscegenation of the Brazilian population and the rather tropical climate of the country favor the development of the disease. Taking into consideration the different regions and their ethnic compositions, the authors estimate that 15-35% of adult Brazilian women are affected by melasma.16
Similarly, in a population-based survey of 855 Iranian women in the city of Ardebil in 2002, melasma was identified in 39.5% of respondents, and, among them, 9.5% were pregnant women.17
Prevalence among paddy field workers in India reached 41%.18 This and the occurrence of melasma in Andean highland children suggest that the combination of pigmentary response (phototype) and intensity of sun exposure plays an important role in the development of the disease.19
A questionnaire was also applied to an Arab population resident in Detroit (USA), and identified that 14.5% of the sample had melasma and 56.4% complained primarily of alterations in skin tone.20
Among a Latino population resident in Texas (USA), prevalence of melasma was 8.8%, and 4.0% of respondents reported past occurrence of melasma.21
Since melasma results from a local change in pigmentation, it preferably affects more strongly melanized phenotypes, and is mainly present in intermediate skin types III-V (Fitzpatrick classification), but rare in extreme skin types.
In a sample of 302 Brazilian patients, 34.4% had skin type III, 38.4% had skin type IV and 15.6% had skin type V. 22 In Tunisia, a survey of 188 women showed that: 14% had skin type III, 45% had skin type IV and 40% had skin type V.23 Similarly, a multicenter study involving 953 patients from three different Brazilian regions, identified that 13% had skin type II, 36% had skin type III, 40% had skin type IV and 10% had skin type V.24
It is theorized that individuals with skin type I fail to produce additional pigmentation, and individuals with skin type VI already produce it at maximum efficiency. Thus, skin types I and VI characterize phenotypes of stable pigmentation. This is also evidenced by the small number of cases of melasma among the European population (with predominantly low skin types) and sub-Saharan Negroid peoples.
Likewise, extreme skin types are less common in multiethnic populations. The influence of ancestry on highly mixed populations such as the Brazilian one, has not yet been properly studied in relation to disease incidence.
Studies on dermatoses that affect Latin American immigrants in Spain showed that 6.7% had some pigmentary change, compared to 3.2% of the Spanish population. Melasma occurred in 2.5% of Hispanic-Americans and 0.5% of Spaniards (OR = 5.1). In addition, among Hispanic-Americans, American Indian ancestry was reported by 65.3% of participants.25
Several studies with different ethnic groups characterized the involvement of women in menacme.22,23,26-29
In Brazil, it was found that most of the female cases (> 50%) develop between the second and fourth decades of life (20 to 35 years of age). This corroborates findings of the literature and suggests a hormonal relationship in the pathophysiology of melasma. In Tunisia, 87% of women were aged between 20 and 40 years. In India, Singapore and in a global study, the average ages of disease development were higher: 30, 34 and 38 years, respectively.22-24,28,30
There is evidence that patients with lower phototypes tend to develop the disease earlier in life. This suggests that melanin plays a photoprotective role and delays the appearance of melasma.22,24
A clear female predominance was observed in the reports of the disease, ranging from 9 or 10 to 1 (estimate range). An Indian study found a less significant prevalence (6:1), whereas in Brazil and Singapore, there was also a clear female predominance: 39:1 and 21:1, respectively.24,28,30
There are few epidemiological data characterizing the disease in men. In a study conducted in Puerto Rico, men accounted for only 10% of cases of melasma and showed the same clinical and histopathological features of the lesions as women. This shows that, although important, female sex hormones might not be an essential causal factor for the development of the disease.26
In 2009, two groups of male Mexican workers and a group of male Guatemalan workers (who have a more predominant indigenous ancestry), all residing in North Carolina (USA), were evaluated. The prevalence of melasma was higher in patients over 31 years of age (70%), in the Guatemalan group (36%), and in patients who spoke an indigenous language. This supports the hypothesis that genetic factors influence the development and prevalence of the disease.31
In another study conducted in India, an even greater discrepancy between men and women was identified: among 120 patients with melasma, 25.8% were men. In this study, sun exposure is associated with the following facts: the population has high skin types; 58.1% are outdoor workers (constantly exposed to the sun); most of the country is situated at intertropical latitudes; and people have the habit of using vegetable oils (e.g.: mustard oil) after bathing.32
Also in India, it was demonstrated that average age and disease duration were similar between men (33.5 and 3.5 years) and women (31.5 and 3.1 years). The main risk factors identified for men were: sun exposure (48.8%) and family history (39.0%). For women, risk factors were associated with pregnancy (45.3%), sun exposure (23.9%) and use of combined oral contraceptives (COC) (19.4%).32
In Tunisia, among 197 patients with melasma, nine (5%) were men with skin types IV and V. Exposure to sunlight was cited as a triggering factor in five men, and as an aggravating factor in eight men. Only three patients reported a family history of melasma.23
The prevalence of melasma during pregnancy varies greatly among the different countries studied. A cross-sectional study in Southern Brazil identified melasma in 10.7% of 224 pregnant women.33 In Iran, melasma was identified in 16% of women; in Morocco, in 37%; and in Pakistan, in 46%.23,34,35 This strengthens the evidence of hormonal involvement in the genesis of the disease, since high levels of estrogen, progesterone and melanocortin are possible triggering factors of melasma during pregnancy.36
In France, in 1994, prevalence of melasma in a group of 60 pregnant women was found to be 5.0%. A possible reason for this discrepancy between the studies could be the difference in skin types, which are higher in the Brazilian and Iranian populations, confirming the hypothesis that melasma is more common in more melanized skin types.37 Pregnancy-induced melasma is associated with an earlier development of the disease and the involvement of a greater number of facial areas. However, it does not correlate with the hyperpigmentation of other areas.22,38,39
In about 40-50% of the female patients the disease is triggered by pregnancy or by the use of oral contraceptive. 8% to 34% of women taking COC (combined hormonal oral contraceptive) develop melasma, which was also reported after hormone replacement therapy.40,41
The natural history of melasma has not yet been adequately studied. Studies show a significant reduction in prevalence after 50 years of age, which may be due to menopause and the reduction in the number and activity of melanocytes that occurs with aging.1,42
Melasma associated with pregnancy typically completely disappears (with treatment) within one year of delivery. There is 6% of spontaneous remission. However, up to 30% of patients develop some pigmentary sequela. The disease is more persistent in women who used oral contraceptive and in melasmas with more intense pigmentation. Recurrences are common in subsequent pregnancies and the chances of developing melasma for the first time during pregnancy increase with a history of multiple pregnancies.29,35,41,43
QUALITY OF LIFE
Melasma has a significant impact on appearance, causing psychosocial and emotional distress, and reducing the quality of life of the affected patients. In addition, there are high expenditures related to medical treatments and procedures whose results do not always meet the expectations of patients.
Melasma distresses patients due to the fact that it mainly affects the face, being easily visible and constantly present in everyday life. In this context, it has a negative impact on the quality of life of patients, affecting their psychological and emotional well-being, which often motivates them to search for a dermatologist.
Patients commonly report feelings of shame, low self-esteem, anhedonia, dissatisfaction, and the lack of motivation to go out. Suicidal ideas have also been reported in the literature.
In 2003, based on the Skindex-16, Balkrishnan et al. developed and validated the MelasQoL (Melasma Quality of Life Scale), a specific questionnaire consisting of 10 questions to assess the effect of melasma on emotional state, social relationships and daily activities. The English version of the MelasQoL showed high internal consistency, validity and discriminatory power when compared to the general questionnaires DLQI and Skindex-16. MelasQoL has been validated for different countries over the world, including Brazil (Chart 1).44-48
Chart 1.
MelasQoL-BP. Disease-specific questionnaire for assessing the quality of life of patients with melasma, validated for the Portuguese spoken in Brazil. The total score ranges from 10 to 70
| Answers: | 1 - Not bothered at all | |
| 2. - Mostly not bothered | ||
| 3. - Sometimes not bothered | ||
| 4. - Neutral | ||
| 5. - Bothered sometimes | ||
| 6. - Bothered most of the time | ||
| 7. - Bothered all the time | ||
| Considering your disease, melasma, how do you feel about: | ||
| 1. The appearance of your skin condition | ( ) | |
| 2. Frustration due to the appearance of your skin condition | ( ) | |
| 3. Embarrassment about the appearance of your skin condition | ( ) | |
| 4. Feeling depressed about your skin condition | ( ) | |
| 5. The effects of your skin condition on your interactions with others | ( ) | |
| (e.g.: interactions with family, friends, close relationships etc.) | ||
| 6. The effects of your skin condition on your desire to be with people | ( ) | |
| 7. Your skin condition making it hard to show affection | ( ) | |
| 8. Skin discoloration making you feel unattractive to others. | ( ) | |
| 9. Skin discoloration making you feel less vital or productive | ( ) | |
| 10. Skin discoloration affecting your sense of freedom | ( ) | |
| TOTAL | ( ) | |
In Brazil, 300 patients of both sexes from all geographic regions (North, Northeast, Midwest, Southeast and South) responded to the MelasQoL. Among the responses that predominated, it was observed that all the time or most of the time: 65% of patients reported discomfort due to the spots, 55% felt frustration and 57% were embarrassed about the aspect of their skin.46
A study conducted in Campinas (Brazil) used the MelasQoL questionnaire to assess 56 patients. It was observed that facial lesions cause great dissatisfaction, low self-esteem, withdrawal from social life, and lower productivity at work or at school.49
In another survey assessing the quality of life of 109 pregnant patients with melasma in Curitiba (Brazil), the MelasQoL-BP mean was 27.2, indicating a negative impact on these patients. It was found that the domains of quality of life most affected by melasma were those related to emotional well-being, skin appearance, frustration and embarrassment.50
There is poor correlation between the MelasQoL and the severity of the disease estimated by the score MASI (Melasma Area and Severity Index), suggesting that the subjective perception of the disease by the patient goes beyond the clinical dimension of the dyschromia.51,52 This means that treatment decisions cannot be solely based on clinical aspects, but should also take into account psychological features, approaching the aspects of greater importance for each patient.53
The MelasQoL scale also showed that patients with lower educational levels and psychiatric disorders (such as mild depression and anxiety) suffer higher emotional impact.15,52,54
The reductionist conception (adopted by many professionals) that melasma represents a purely 'cosmetic' problem restricts diagnoses and the possibility of more satisfactory treatment options that can be tailored to the individual needs of each patient.55
Due to the high degree of subjectivity of the items and the number of answer options per item, researchers should pay special attention and critique when applying the MelasQoL to more humble patients and patients with lower educational levels, in order to increase the reliability of the instrument.
ETIOLOGY, PHYSIOPATHOLOGY AND RISK FACTORS
The exact causes of melasma are unkown, although some triggering factors are described, such as sun exposure, pregnancy, use of oral contraceptives and other steroids, consumption of certain food items, ovarian tumors, intestinal parasitoses, hepatopathies, hormone replacement therapy, use of cosmetics and photosensitizing drugs, procedures and inflammatory processes of the skin, and stressful events.1,22,39,56 This suggests that the development of melasma is influenced by many factors, and depends on the interaction of environmental and hormonal influences, with susceptible genetic substrate.
Sun exposure (without burning) is the most important triggering factor for melasma. UV radiation directly induces the increase of melanogenic activity, causing the development of epidermal pigmentation and occurring more intensely in regions with melasma than in the adjacent skin.23,42
Melasma pigmentation usually improves in the winter and worsens in the summer (or immediately after intense sun exposure). Moreover, in intertropical regions, its populational incidence is increased.57-59 The use of high-protection-factor sunscreen reduces the intensity of the disease in 50%, and decreases its incidence during pregnancy in more than 90%.60,61
In the Andean population, who lives at altitudes above 2000 meters, melasma occurs in the majority of the indigenous population, including men, This is due to their melanodermic constitutional type and greater intensity of UV radiation exposure.19
UVA and UVB are the main radiations that induce melanogenesis. Infrared radiation and visible light have a significantly inferior melanogenic poten62,63 Its role in the development and maintenance of melasma is unclear. However, the authors identified nighttime workers exposed to the heat of ovens (e.g.: bakers), and professionals exposed to high intensity of light (e.g.: dentists) who experienced great difficulty in treating melasma and reported worsening after exposure to their working conditions.
Sexual hormones like estrogen and progestin are also related to the appearance of melasma. Pregnancy, COC and hormone replacement therapy are the most commonly cited triggering factors.40,41,64
Among 61 women who developed melasma due to the use of COC in the USA in 1967, 52 (87%) also reported having the disease during pregnancy. This indicates that a pigmentary event induced by sexual hormones may be a risk factor for a subsequent pigmentary event in predisposed individuals.41
An Indian study compared FSH, LH, prolactin, estrogen and progesterone among 36 women with melasma and controls of the same age. There were differences in the levels of 17-β-estradiol at the beginning of the menstrual cycle among the groups, suggesting that circulating estrogens may constitute a risk factor and 'maintainer' of the disease.65
In another study conducted in Pakistan with 138 women, the authors performed serum measurements of estradiol, progesterone and prolactin. The results showed a significant increase in estradiol levels both in the follicular and in the luteal phases in patients with melasma, when compared to the controls.66
Estrogens act on nuclear receptors and, in a nongenomic fashion, on melanocytes, inducing pigmentation.67 They increase the expression of melanocortin type 1 receptors (MC1R) in cultured melanocytes, which are involved in the pathophysiology of melasma.68-70 Moreover, they promote the increase of expression of PDZK1 gene, which leads to the transcription of tyrosinase, although they do not change the number of melanocytes and/or keratinocytes. The involvement of PDZK1 in the skin pigmentation of patients with melasma has also been demonstrated.71-73
Among men, there is a report of melasma development after oral therapy with stimulators of testosterone production, a compound that includes DHEA (dehydroepiandrosterone), androstenedione, indole-3-carbinol and Tribulus terrestres, a gonadotropic stimulator that increases LH secretion.74 Furthermore, increased levels of LH and reduced levels of testosterone were identified in 15 men with melasma in India.75 In France, it was reported the case of a man with complete hypogonadism - which increases LH and FSH levels, and reduces testosterone levels - who developed facial melasma.76
In pregnancy, especially in the third trimester, there is stimulus for melanogenesis, and the increased levels of placental, ovarian and pituitary hormones may justify melasma associated with pregnancy. Elevations of melanocyte-stimulating hormone (MSH), estrogen and progesterone also lead to increased transcription of tyrosinase and dopachrome tautomerase, which may be involved in the development of pigmentation in this phase.29,36
The association of melasma with endocrinopathies and autoimmune thyroid diseases has also already been suggested.77,78 However, a study conducted in Iran with 45 women with melasma and their controls evaluated the serum levels of anti-thyroid peroxidase antibodies (anti-TPO), T3, T4 and TSH, and showed no difference among the groups.79
Likewise, 20 patients with idiopathic melasma were investigated in the dermatology outpatient clinic of a university hospital in Rio de Janeiro (Brazil). It was concluded that thyreotrophic, prolactinic and gonadotropic reserves were normal, as well as the ovarian and thyroid function. Therefore, it was not possible to establish an etiological correlation between melasma and the observed hormone levels.80
Furthermore, thyropathies may affect up to 25% of women in the menacme, which may have caused some confusion, when imputing its association with the development of melasma. However, this has not been confirmed in controlled studies.22,79,80
Melasma is the most common melanodermia in individuals with brown to light brown skin. Familial predisposition (genetic component) is the most important risk factor for its development. However, no Mendelian pattern of segregation has been identified so far.1,8
The occurrence of melasma was described in two identical twins, in England, in 1987. It was triggered by hormonal stimulation and worsened after sun exposure. However, it did not occur in the other sister (not twin), which strengthens the hypothesis of genetic susceptibility to disease development.81
In a study involving 324 patients in nine centers around the world, it was observed that 48% of individuals with melasma reported family history of at least one relative with this dermatosis and, among those with a positive history, 97% were in first-degree relatives.29 In Brazil, it was identified 56% of family history among the 302 patients studied.22 Conversely, lower frequencies were identified in India (33%), and Singapore (10%), suggesting that the development of the disease may suffer epigenetic hormonal control, as well as the influence of environmental stimuli, such as UV radiation.28,30,82
When questioned about the triggering factors of melasma, the three most-cited elements by patients were: pregnancy (26-51%), sun exposure (27-51%) and COC use (16-26%).22-24,29
A prospective study conducted with 197 patients in Tunisia in 2010 evaluated aggravating factors of melasma. Sun exposure was cited as the main aggravating factor by 84% of patients, followed by the use of COC by 38% and pregnancy by 50%.23
Genetic alterations may be related to the stimulation of melanogenesis in melasma. In 2010, a South Korean study showed reduced expression of the H19 gene in patients with melasma. H19 is a gene that transcribes a non-coding RNA but which operates in imprint with the IGF2 gene (insulin-like growth factor type II).83
Decreased transcription of H19 in mixed cultures (melanocyte-keratinocyte) induces melanogenesis and melanin transfer to keratinocytes. What draws our attention is that, when trying to reproduce the experiment in cultures of isolated melanocytes, this stimulation does not repeat itself. These results suggest that H19 may play a role in the development of melasma and strengthens the hypothesis of the involvement of keratinocytes in its physiopathogenesis.84
Estrogen treatment in mixed cultures (melanocyte-keratinocyte) depleted of the gene of H19 promotes additional effect on the expression of tyrosinase. This substantiates the hypothesis of the involvement of estrogen in the pathogenesis of the disease.83
In 2011, a transcriptomic study evaluated the expression of 279 genes in skin affected by melasma, when compared with perilesional normal skin. High levels of melanin and melanogenesis-associated proteins were observed in the diseased epidermis, as well as mRNA expression of TYRP1 (tyrosinase-related protein 1). This confirms the hyperactivity of the epidermal-melanin unit in melasma. Furthermore, it was found that Wnt pathway modulator genes, such as WIF1, SFRP2 and Wnt5a, showed higher expression levels in melasma skin, which suggests their involvement in the stimulation of melanogenesis.85
Genes related to lipid metabolism such as PPARα, ALOX15B, DGAT2L3 and PPARGC1A, were less expressed in the skin with melasma, which was later confirmed by the study of the function and repair of the skin barrier in the affected skin.86
The epidermal-melanin unit usually responds to certain inflammatory stimuli through melanogenesis42,67,87 Melasma can be triggered or aggravated by cosmetic procedures that induce skin inflammation, such as peelings and therapies with light/laser. A study on the incidence of melasma associated with treatments with intense pulsed light (IPL) concluded that patients who have subclinical melasma may exacerbate the injury by using IPL. The authors suggest the use of photography with UV before treatment with IPL, in order to determine the existence of latent melasma and prevent its worsening.88
Several inflammatory mediators such as endothelin-1, stem cell factor, c-kit, GM-CSF, iNOS, and VEGF, besides having a greater number of inflammatory cells and vessels, have been described as more highly expressed in skin with melasma, when compared to normal adjacent skin.1,84,89 This supports the hypothesis that there is a greater inflammatory response of damaged skin.
The use of cosmetics and intake of certain drugs such as anticonvulsants and other photosensitizing substances have also been implicated as risk factors for melasma.90,91 Likewise, a wide variety of chemicals such as arsenic, iron, copper, bismuth, silver, gold; and drugs such as antimalarials, tetracyclines, anticonvulsants, amiodarone, sulfonylureas, among others, can cause hyperpigmentation of the skin, by depositing in the surface layers or by stimulating melanogenesis.6,92
However, a study of 76 patients with melasma found no association between the disease and the use of any chemical, suggesting that, although possible, exogenous chemical exposures are not the main etiological agent of the disease.39,92
Some patients also report the onset of melasma after stressful episodes and affective disorders (e.g.: depression).22,56 Propiomelanocortins (ACTH and MSH) are hormones related to stress, which can activate melanocortin receptors in melanocytes, inducing melanogenesis.1 There is also evidence that the melanocyte presents individualized response to stress hormones, with the same hierarchy of the hypothalamic-pituitary axis.93-95 However, we found no studies on states of anxiety among patients with melasma and healthy controls.
The possibility of the existence of a neural ele-ment associated with melasma has been suggested. Researchers in South Korea in 2009 carried out a comparative study between the affected and surrounding skin biopsies from six Asian patients. An increase in the number of keratinocytes expressing NGFR (nerve growth factor receptor), neural endopeptidase and nerve fibers in the superficial dermis of the diseased skin was evidenced.96 These findings support the hypothesis that neuropeptides may play a role in the development or maintenance of the disease.
There are few comparative studies between melasma and other melanocytic alterations. In 2008, in Iran, a case-control study with 120 patients with melasma showed it to be more prevalent among the cases: lentigines (OR = 5.2), freckles (OR = 5.9), ruby angiomas (OR = 3.2) nevi (OR = 23.0), which may indicate markers of risk phenotypes.97
The association of melasma with post-inflammatory hyperpigmentation is also poorly studied. Another study was conducted in Iran in 2013 with 200 patients with melasma associated with inflammatory acne, and control subjects of the same age with inflammatory acne only. Melasma patients were found to have a six times greater chance of developing postinflammatory hyperpigmentation. This suggests that the epidermal-melanin unit is hyper-reactive in these cases, although the authors have not checked the results according to skin phototypes.98 In Brazil, it was shown that patients with melasma and higher phenotypes presented higher frequency of post-inflammatory hyperpigmentation.24
CLINICAL PRESENTATION
Melasma is characterized by brownish macules with irregular contours and clear limits. It appears in sun-exposed areas, especially the face and cervical region, and, less commonly, in the arms and sternal region (Figures 1 and 2).1,22
FIGURE 1.

Mixed melasma. Female patient with frontal, temporal, parotid, mandibular, zygomatic, mentonian lesions and lesion in the upper lip
FIGURE 2.

Extra-facial melasma. Brown pigmentation in the neck area, an area of sun exposure due to the neckline
According to their clinical distribution, facial melasma lesions can be categorized into two types: centrofacial and peripheral. In the centrofacial type, lesions are predominant in the center of the face, i.e., in the glabellar, frontal, nasal, zygomatic, upper lip and chin areas. In the peripheral type, the fronto-temporal, preauricular and mandibular branch areas are affected.
A large proportion of patients reports having melasma lesions in both regions at the time of consultation. However, the evolutionary kinetics of the topographies of melasma has not yet been adequately elucidated.
A 2013 study conducted in Brazil on the epidemiological characteristics of facial melasma in Brazilian women identified the predominance of centrofacial melasma (51.7%), followed by mixed melasma (43.4%).22
In a survey of Indian patients, centrofacial melasma form was identified in 55% of cases. However, the study does not cite cases of mixed melasma.28 Another study of 188 female patients in Tunisia showed that 76% had centrofacial melasma and to 22% had mixed melasma.23
Due to its higher frequency in all series of cases, the zygomatic (or malar) melasma, has been suggested as a classification independent from other topographies. However, since it has high co-occurrence with centrofacial types - especially with glabellar lesions - it was proposed that zygomatic lesions should be included in the centrofacial classification.22
Exclusively mandibular melasma is rare, and may represent a type of poikiloderma of Civatte, since patients are often postmenopausal women who report development after extensive sun exposure, and the analysis of biopsies reveals significant actinic damage.23,99 A Brazilian study of 302 women with melasma did not find elements to differentiate mandibular forms from peripheral ones. In this study, 64.8% of mandibular lesions were associated with parotid lesions, and only two cases (3.7%) were isolated/exclusive.22 In India, an evaluation of 312 patients revealed only 1.6% of cases of exclusively mandibular melasma.28 These data lead us to reflect on the possibility of a classification into two types of melasma: centrofacial and peripheral, exclusively.
According to two studies conducted in Brazil, the most affected regions of the face were: zygoma, upper lip, forehead, nose, parotid and chin (Table 1).22,24 However, the more irradiated areas of the face do not coincide with the highest frequency of melasma sites.100
TABLE 1.
Frequence of facial topographies affected by melasma
| Topography | % |
|---|---|
| Zygomatic | 84 |
| Supralabial | 51 |
| Frontal | 50 |
| Nasal | 40 |
| Parotid | 30 |
| Mentonian | 29 |
| Glabellar | 25 |
| Temporal | 24 |
| Mandibular | 18 |
Adapted from: Tamega AA et al, 2013. 21
Although less common (10-14%), other sites may be simultaneously involved, constituting extrafacial melasma (Figure 2), which can be associated with any of the other facial patterns.101
Extrafacial melasma manifests itself as hyperchromic, irregular, symmetrical skin discolorations in the arms and forearms, neck/cervical and sternal regions and, eventually, in the back (dorso). Melasmas affecting the upper limbs occur mainly among older, menopaused women, and may be associated with hormone replacement therapy.24,102-104
Histopathological analyses of melasma lesions of the upper limbs showed findings that resemble the histological features of facial melasma. There are no epidemiological characteristics that lead to the conclusion that extrafacial melasma constitutes an independent disease.102
DIAGNOSIS
The diagnosis of melasma is essentially clinical, and poses no greater difficulties to the dermatologist.
The main differential diagnoses of melasma are freckles, solar lentigo, toxic melanodermia, Riehl's melanosis, post-inflammatory hyperpigmentation, friction melanosis, ochronosis (endogenous and exogenous), cutaneous erythematosus lupus. We can also cite: phytophotodermatosis, pellagra, endogenous phototoxicity, nevus of Ota, café au lait macules, seborrheic keratosis, Civatte's poikiloderma, acquired bilateral nevus of Ota-like macules (Hori's nevus), periorbital hyperpigmentation, erythrose pigmentaire peribuccale of Brocq, erythromelanosis follicularis faciei, facial acanthosis nigricans, drug-induced pigmentation (e.g.: amiodarone) and actinic lichen planus.105-107
In patients with higher pigmentation, pigmentary demarcation lines (PDL) may confuse the diagnosis of melasma. A study conducted with 1033 women at a hospital in Saudi Arabia found that 14% of the women had PDL.108 In another study in Texas (USA), it was found that 79% of black women had at least one PDL.109
Wood's lamp examination (340 to 400nm) highlights the difference in pigmentation of the affected skin (Figure 3). Melasmas that are more intensely seen under Wood's light examination respond better to topical treatments.30,110
FIGURE 3.
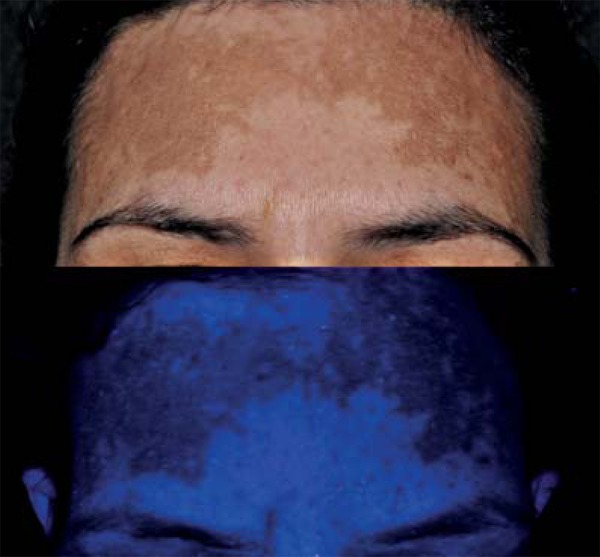
Comparison between photography with visible light (top) and with the use of Wood's lamp (bottom) highlighting the limits of the frontal macules of melasma
Dermoscopy of melasma (variable increase from 6 to 400x) shows very characteristic changes. It is possible to see the vascular component, which is present in a large number of patients (Figure 4).111 The color intensity of melanin and the regularity of the pigment network reveal the density and location of melanin. It presents dark brown color and welldefined network when located in the stratum corneum; shades of light brown and irregularity of the network when located in the lower layers of the epidermis; and blue or bluish-gray color when located in the dermis.
FIGURE 4.

Dermoscopy (polarized light) of transitional area: frontal melasma (left) and healthy skin (right). We can observe brown pigment and more intense telangiectasies in the affected area, forming an irregular network
Reflectance confocal microscopy (RCM) allows the in vivo evaluation of large areas of melasma, in a direct and noninvasive way. Hypertrophied melanocytes are displayed at high resolution, and melanin is detected in all layers of the epithelium and dermis, in all cases. This disfavors the former classification between epidermal or dermal melasma. MCR is reported as a potential technique for assessing treatment response in clinical trials.112-115
The severity of facial melasma can be estimated by using colorimetry, mexametry, and the MASI score (Melasma Area and Severity Index).
Colorimetry objectively and reproducibly quantifies and qualifies the reflex of a standardized source of monochromatic lights at a skin site. The most used colorimetric method is the L*a*b*, where the erythema is best represented by channel a* (redgreen); melanin pigmentation is proportional to the reduction in channel L* (luminance); and channel b* represents the variation between yellow and blue. It also allows the measurement of the individual typological angle (ITAO), which is calculated by the arctangent [(L*-50)/b*]x(180/π), and is inversely associated with skin pigmentation.116,117
Mexametry uses a single monochromatic source to measure surface reflectance intensities. It does not provide colorimetric values , but erythema and melanin indices of the surface. Results are reproducible and (clinically) quite intuitive.118
The MASI index was proposed by Kimbrough-Green et al, in 1994, in order to clinically quantify the severity of facial melasma. It is the most used tool for assessing the severity of melasma.116,119
The MASI score is calculated by visual inspection of the face. Three factors are assessed: the affected area (A), hyperpigmentation (D) and homogeneity of pigmentation (H). Moreover, the face is divided into four regions: forehead (F), right malar region (MR), left malar region (ML) and chin (C).119
The final MASI score is the sum of pigmentation intensity and homogeneity scores multiplied by the area score and the multiplying factor for each region (Chart 2).
CHART 2.
MASI. Scheme for calculating the index of severity of melasma. Total score ranges from 0 to 48
| Intensity of pigmentation * | Homogeneity of pigmentation * | Affected area ** | Multiplication factor | Value | ||||
|---|---|---|---|---|---|---|---|---|
| Forehead | ( | + | ) | X | X | 0.3 | ||
| Right malar | ( | + | ) | X | X | 0.3 | ||
| Left malar | ( | + | ) | X | X | 0.3 | ||
| Chin | ( | + | ) | X | X | 0.1 | ||
| MASI | SUM TOTAL |
Categories: 0 none, 1 mild, 2 moderate, 3 outstanding e 4 maximal.
Categories: 0 normal skin; 1=< 10%; 2 =10%-29%; 3 =3049%; 4 =50%-69%; 5 =70%-89%; 6 =90%-100%.
The total score correlates with the highest possible severity of the disease. The MASI score is used for documentation of lesions in clinical trials and, more recently, in studies that correlate the quality of life of patients with the severity of melasma.106
The reproducibility of the MASI score is questioned by many authors. For this reason, therapeutic outcomes should also be evaluated by using colorimetry and MelasQoL.106,119
Histologically, melasma is characterized by epidermal hyperpigmentation. The number of melanocytes is not increased. Melanocytes are hypertrophied and show a greater number of dendrites and cytoplasmic organelles, which indicates higher metabolic activity. There is an increased amount of melanin in all layers of the epidermis, and an increased number of mature melanosomes. In the dermis, there is a moderate mononuclear infiltrate, presence of mast cells, increased vascularity and elastosis. There are no differences in dermal pigmentation between the skin with melasma and the adjacent healthy skin.27,69,120
In recent years, researchers conducted investigations on protein expression by using immunohistochemistry in an attempt to understand and elucidate the pathogenesis of melasma.
Nuclear estrogen receptors were more common in keratinocytes of melasma skin, which supports the role of exposure to sex hormones as a factor that triggers or 'maintains' pigmentation.121
A greater immunoreactivity of α-MSH was also more evidenced in diseased skin than in healthy adjacent skin. The increase in the paracrine synthesis of α-MSH caused by the genetically modified epidermis is one of the main assumptions in the pathophysiology of the disease.15,69,122
In addition, UV (ultraviolet) radiation may lead to the production of multiple cytokines (interleukin-1, endothelin-1, α-MSH and ACTH) by keratinocytes, stimulating melanogenesis.15,42
Careful clinical examination and the appropriate collection of information (such as age of onset of lesions, course of disease and possible aggravators) enable the differential diagnosis, making histology rarely necessary.
FINAL CONSIDERATIONS
Persistent dysfunction of the epidermalmelanin unit - resulting in recurring pigmentation in the skin with melasma - derives from a disarray of the melanogenesis. Its regulatory components and their interactions are not well known.123
Due to the incomplete understanding of its pathogenesis, treatments of melasma aim, essentially, at blocking solar radiation (through strategies that reduce the biosynthesis, transport and transfer of melanin), and reducing the amount of epidermal melanin, instead of aiming at the causal dysfunction of the disease. Thus, long-term therapies are necessary, since recurrence rates are high. However, this matter is beyond the scope of this study.54,57,124-126
In general, prognosis of melasma is favorable. There is a reduction in its prevalence, in the intensity of lesions with age, and the attenuation of pigmentation with treatment.
It is intriguing that a more intense melanogenic response behavior occurs in melasma lesions than in adjacent healthy areas, since both are subjected to similar photo-exposure schemes. This suggests a postsomatic genetic mosaicism behavior of the pigmentary system, whose genomic substrate is not yet fully understood.
Controlled epidemiological studies may support hypotheses for research on pathophysiology, therapeutic strategies, as well as promote primary prevention in risk groups.
Footnotes
Conflict of Interest: None.
Financial Support: None.
How to cite this article: Handel AC, Miot LDB, Miot HA. Melasma: a clinical and epidemiological review. An Bras Dermatol. 2014;89(5):771-82.
Study conducted at the Department of Dermatology and Radiotherapy, Faculdade de Medicina de Botucatu - Universidade Estadual Paulista "Julio de Mesquita Filho" (FMB-Unesp) - Botucatu (SP), Brazil.
REFERENCES
- 1.Miot LD, Miot HA, Silva MG, Marques ME. Physiopathology of melasma. An Bras Dermatol. 2009;84:623–635. doi: 10.1590/s0365-05962009000600008. [DOI] [PubMed] [Google Scholar]
- 2.Corsi H. Chloasma Virginum Periorale. Proc R Soc Med. 1935;28:1169–1169. [PMC free article] [PubMed] [Google Scholar]
- 3.Lindsay HC. Chloasma uterinum. Arch Derm Syphilol. 1946;53:58–58. [PubMed] [Google Scholar]
- 4.Bolanca I, Bolanca Z, Kuna K, Vukovic A, Tuckar N, Herman R, et al. Chloasma-the mask of pregnancy. Coll Antropol. 2008;32:139–141. [PubMed] [Google Scholar]
- 5.Plenck JJ. Doctrina de Morbis Cutaneis. Qua hi morbi in suas classes, genera et species redingtur. Vienna, J.F: Van Overbeke; 1776. [Google Scholar]
- 6.Newcomer VD, Lindberg MC, Sternberg TH. A melanosis of the face ("chloasma") Arch Dermatol. 1961;83:284–299. doi: 10.1001/archderm.1961.01580080114013. [DOI] [PubMed] [Google Scholar]
- 7.Lupi O, Nunes S, Gomes Neto A, Pericles C. Doenças dermatológicas no Brasil perfil atitudinal e epidemiológico. An Bras Dermatol. 2010;85:S5–S19. [Google Scholar]
- 8.Sociedade Brasileira de Dermatologia SBD Nosologic profile of dermatologic visits in Brazil. 2006;81:545–554. [Google Scholar]
- 9.Walker SL, Shah M, Hubbard VG, Pradhan HM, Ghimire M. Skin disease is common in rural Nepal: results of a point prevalence study. Br J Dermatol. 2008;158:334–338. doi: 10.1111/j.1365-2133.2007.08107.x. [DOI] [PubMed] [Google Scholar]
- 10.Alakloby OM. Pattern of skin diseases in Eastern Saudi Arabia. Saudi Med J. 2005;26:1607–1610. [PubMed] [Google Scholar]
- 11.Halder RM, Grimes PE, McLaurin CI, Kress MA, Kenney Jr JA. Incidence of common dermatoses in a predominantly black dermatologic practice. Cutis. 1983;32:388–390. [PubMed] [Google Scholar]
- 12.Souza SR, Fischer FM, Souza JM. Suntanning and risk of cutaneous melanoma: a literature review. Rev Saude Publica. 2004;38:588–598. doi: 10.1590/s0034-89102004000400018. [DOI] [PubMed] [Google Scholar]
- 13.Taylor SC. Epidemiology of skin diseases in ethnic populations. Dermatol Clin. 2003;21:601–607. doi: 10.1016/s0733-8635(03)00075-5. [DOI] [PubMed] [Google Scholar]
- 14.Perez M, Luke J, Rossi A. Melasma in Latin Americans. J Drugs Dermatol. 2011;10:517–523. [PubMed] [Google Scholar]
- 15.Sheth VM, Pandya AG. Melasma a comprehensive update: part I. J Am Acad Dermatol. 2011;65:689–697. doi: 10.1016/j.jaad.2010.12.046. [DOI] [PubMed] [Google Scholar]
- 16.Ishiy PS, Silva LR, Penha MA, Handel AC, Miot HA. Skin diseases reported by workers from the campus of UNESP Rubião Jr, Botucatu-SP (Brazil) An Bras Dermatol. 2014;89:529–531. doi: 10.1590/abd1806-4841.20142875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edalatkhah H, Amani F, Rezaifar G. Prevalence of melasma in women in Ardebil city in 2002. Iran J Dermatol. 2004;7:72–77. [Google Scholar]
- 18.Shenoi SD, Davis SV, Rao S, Rao G, Nair S. Dermatoses among paddy field workers--a descriptive, cross-sectional pilot study. Indian J Dermatol Venereol Leprol. 2005;71:254–258. doi: 10.4103/0378-6323.16617. [DOI] [PubMed] [Google Scholar]
- 19.Scheinfeld NS. Melasma. Skinmed. 2007;6:35–37. doi: 10.1111/j.1540-9740.2007.06338.x. [DOI] [PubMed] [Google Scholar]
- 20.El-Essawi D, Musial JL, Hammad A, Lim HW. A survey of skin disease and skinrelated issues in Arab Americans. J Am Acad Dermatol. 2007;56:933–938. doi: 10.1016/j.jaad.2007.01.031. [DOI] [PubMed] [Google Scholar]
- 21.Werlinger KD, Guevara IL, González CM, Rincón ET, Caetano R, Haley RW, et al. Prevalence of self-diagnosed melasma among premenopausal Latino women in Dallas and Fort Worth, Tex. Arch Dermatol. 2007;143:424–425. doi: 10.1001/archderm.143.3.424. [DOI] [PubMed] [Google Scholar]
- 22.Tamega Ade A, Miot LD, Bonfietti C, Gige TC, Marques ME, Miot HA. Clinical patterns and epidemiological characteristics of facial melasma in Brazilian women. J Eur Acad Dermatol Venereol. 2013;27:151–156. doi: 10.1111/j.1468-3083.2011.04430.x. [DOI] [PubMed] [Google Scholar]
- 23.Guinot C, Cheffai S, Latreille J, Dhaoui MA, Youssef S, Jaber K, et al. Aggravating factors for melasma: a prospective study in 197 Tunisian patients. J Eur Acad Dermatol Venereol. 2010;24:1060–1069. doi: 10.1111/j.1468-3083.2010.03592.x. [DOI] [PubMed] [Google Scholar]
- 24.Hexsel D, Lacerda DA, Cavalcante AS, Machado Filho CA, Kalil CL, Ayres EL, et al. Epidemiology of melasma in Brazilian patients: a multicenter study. Int J Dermatol. 2013;53:440–444. doi: 10.1111/j.1365-4632.2012.05748.x. [DOI] [PubMed] [Google Scholar]
- 25.Albares Tendero MP, Belinchón Romero I, Ramos Rincón JM, Sánchez Payá J, Costa AL, Pérez Crespo M, et al. Dermatoses in Latin American immigrants seen in a tertiary hospital. Eur J Dermatol. 2009;19:157–162. doi: 10.1684/ejd.2008.0600. [DOI] [PubMed] [Google Scholar]
- 26.Grimes PE. Melasma. Etiologic and therapeutic considerations. Arch Dermatol. 1995;131:1453–1457. doi: 10.1001/archderm.131.12.1453. [DOI] [PubMed] [Google Scholar]
- 27.Kang WH, Yoon KH, Lee ES, Kim J, Lee KB, Yim H, et al. Melasma: histopathological characteristics in 56 Korean patients. Br J Dermatol. 2002;146:228–237. doi: 10.1046/j.0007-0963.2001.04556.x. [DOI] [PubMed] [Google Scholar]
- 28.Achar A, Rathi SK. Melasma: a clinico-epidemiological study of 312 cases. Indian J Dermatol. 2011;56:380–382. doi: 10.4103/0019-5154.84722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ortonne JP, Arellano I, Berneburg M, Cestari T, Chan H, Grimes P, et al. A global survey of the role of ultraviolet radiation and hormonal influences in the development of melasma. J Eur Acad Dermatol Venereol. 2009;23:1254–1262. doi: 10.1111/j.1468-3083.2009.03295.x. [DOI] [PubMed] [Google Scholar]
- 30.Goh CL, Dlova CN. A retrospective study on the clinical presentation and treatment outcome of melasma in a tertiary dermatological referral centre in Singapore. Singapore Med J. 1999;40:455–458. [PubMed] [Google Scholar]
- 31.Pichardo R, Vallejos Q, Feldman SR, Schulz MR, Verma A, Quandt SA, et al. The prevalence of melasma and its association with quality of life in adult male Latino migrant workers. Int J Dermatol. 2009;48:22–26. doi: 10.1111/j.1365-4632.2009.03778.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarkar R, Jain RK, Puri P. Melasma in Indian males. Dermatol Surg. 2003;29:204–204. [PubMed] [Google Scholar]
- 33.Hexsel D, Rodrigues TC, Dal'Forno T, Zechmeister-Prado D, Lima MM. Melasma and pregnancy in southern Brazil. J Eur Acad Dermatol Venereol. 2009;23:367–368. doi: 10.1111/j.1468-3083.2008.02885.x. [DOI] [PubMed] [Google Scholar]
- 34.Wong RC, Ellis CN. Physiologic skin changes in pregnancy. J Am Acad Dermatol. 1984;10:929–940. doi: 10.1016/s0190-9622(84)80305-9. [DOI] [PubMed] [Google Scholar]
- 35.Moin A, Jabery Z, Fallah N. Prevalence and awareness of melasma during pregnancy. Int J Dermatol. 2006;45:285–288. doi: 10.1111/j.1365-4632.2004.02470.x. [DOI] [PubMed] [Google Scholar]
- 36.Martin AG, Leal-Khouri S. Physiologic skin changes associated with pregnancy. Int J Dermatol. 1992;31:375–378. doi: 10.1111/j.1365-4362.1992.tb02662.x. [DOI] [PubMed] [Google Scholar]
- 37.Estève E, Saudeau L, Pierre F, Barruet K, Vaillant L, Lorette G. Physiological cutaneous signs in normal pregnancy: a study of 60 pregnant women. Ann Dermatol Venereol. 1994;121:227–231. [PubMed] [Google Scholar]
- 38.Wade TR, Wade SL, Jones HE. Skin changes and diseases associated with pregnancy. Obstet Gynecol. 1978;52:233–242. [PubMed] [Google Scholar]
- 39.Elling SV, Powell FC. Physiological changes in the skin during pregnancy. Clin Dermatol. 1997;15:35–43. doi: 10.1016/s0738-081x(96)00108-3. [DOI] [PubMed] [Google Scholar]
- 40.Wu IB, Lambert C, Lotti TM, Hercogová J, Sintim-Damoa A, Schwartz RA. Melasma. G Ital Dermatol Venereol. 2012;147:413–418. [PubMed] [Google Scholar]
- 41.Resnik S. Melasma induced by oral contraceptive drugs. JAMA. 1967;199:601–605. [PubMed] [Google Scholar]
- 42.Videira IF, Moura DF, Magina S. Mechanisms regulating melanogenesis. An Bras Dermatol. 2013;88:76–83. doi: 10.1590/S0365-05962013000100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alves GF, Nogueira LSC, Varella TCN. Dermatologia e gestação. An Bras Dermatol. 2005;80:179–186. [Google Scholar]
- 44.Balkrishnan R, McMichael AJ, Camacho FT, Saltzberg F, Housman TS, Grummer S, et al. Development and validation of a health-related quality of life instrument for women with melasma. Br J Dermatol. 2003;149:572–577. doi: 10.1046/j.1365-2133.2003.05419.x. [DOI] [PubMed] [Google Scholar]
- 45.Dominguez AR, Balkrishnan R, Ellzey AR, Pandya AG. Melasma in Latina patients: cross-cultural adaptation and validation of a quality-of-life questionnaire in Spanish language. J Am Acad Dermatol. 2006;55:59–66. doi: 10.1016/j.jaad.2006.01.049. [DOI] [PubMed] [Google Scholar]
- 46.Cestari TF, Hexsel D, Viegas ML, Azulay L, Hassun K, Almeida AR, et al. Validation of a melasma quality of life questionnaire for Brazilian Portuguese language: the MelasQoL-BP study and improvement of QoL of melasma patients after triple combination therapy. Br J Dermatol. 2006;156:13–20. doi: 10.1111/j.1365-2133.2006.07591.x. [DOI] [PubMed] [Google Scholar]
- 47.Misery L, Schmitt AM, Boussetta S, Rahhali N, Taieb C. Melasma: measure of the impact on quality of life using the French version of MELASQOL after cross-cultural adaptation. Acta Derm Venereol. 2010;90:331–332. doi: 10.2340/00015555-0837. [DOI] [PubMed] [Google Scholar]
- 48.Dogramaci AC, Havlucu DY, Inandi T, Balkrishnan R. Validation of a melasma quality of life questionnaire for the Turkish language: the MelasQoL-TR study. J Dermatolog Treat. 2009;20:95–99. doi: 10.1080/09546630802287553. [DOI] [PubMed] [Google Scholar]
- 49.Costa A, Pereira MO, Moisés TA, Cordeiro T, Silva ARD, Amazonas FTP, et al. Avaliação da melhoria na qualidade de vida de portadoras de melasma após uso de combinação botânica à base de Bellis perennis, Glycyrrhiza glabra e Phyllanthus emblica comparado ao da hidroquinona, medido pelo MELASQoL. Surg Cosm Dermatol. 2011;3:207–212. [Google Scholar]
- 50.Purim KS, Avelar MF. Photoprotection, melasma and quality of life in pregnant women. Rev Bras Ginecol Obstet. 2012;34:228–234. doi: 10.1590/s0100-72032012000500007. [DOI] [PubMed] [Google Scholar]
- 51.Cestari T, Adjadj L, Hux M, Shimizu MR, Rives VP. Cost-effectiveness of a fixed combination of hydroquinone/tretinoin/fluocinolone cream compared with hydroquinone alone in the treatment of melasma. J Drugs Dermatol. 2007;6:153–160. [PubMed] [Google Scholar]
- 52.Freitag FM, Cestari TF, Leopoldo LR, Paludo P, Boza JC. Effect of melasma on quality of life in a sample of women living in southern Brazil. J Eur Acad Dermatol Venereol. 2008;22:655–662. doi: 10.1111/j.1468-3083.2007.02472.x. [DOI] [PubMed] [Google Scholar]
- 53.Renzi C, Abeni D, Picardi A, Agostini E, Melchi CF, Pasquini P, et al. Factors associated with patient satisfaction with care among dermatological outpatients. Br J Dermatol. 2001;145:617–623. doi: 10.1046/j.1365-2133.2001.04445.x. [DOI] [PubMed] [Google Scholar]
- 54.Sheth VM, Pandya AG. Melasma: a comprehensive update: part II. J Am Acad Dermatol. 2011;65:699–714. doi: 10.1016/j.jaad.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 55.Rendon MI. Utilizing combination therapy to optimize melasma outcomes. J Drugs Dermatol. 2004;3:S27–S34. [PubMed] [Google Scholar]
- 56.Wolf R, Wolf D, Tamir A, Politi Y. Melasma: a mask of stress. Br J Dermatol. 1991;125:192–193. doi: 10.1111/j.1365-2133.1991.tb06075.x. [DOI] [PubMed] [Google Scholar]
- 57.Victor FC, Gelber J, Rao B. Melasma: a review. J Cutan Med Surg. 2004;8:97–102. doi: 10.1007/s10227-004-0158-9. [DOI] [PubMed] [Google Scholar]
- 58.Rigopoulos D, Gregoriou S, Katsambas A. Hyperpigmentation and melasma. J Cosmet Dermatol. 2007;6:195–202. doi: 10.1111/j.1473-2165.2007.00321.x. [DOI] [PubMed] [Google Scholar]
- 59.Katsambas A, Antoniou C. Melasma. Classification and treatment. J Eur Acad Dermatol Venereol. 1995;4:217–223. [Google Scholar]
- 60.Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seité S, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738–742. doi: 10.1111/j.1468-3083.2007.02185.x. [DOI] [PubMed] [Google Scholar]
- 61.Miot HA, Miot LD. Re: Topical 10% zinc sulfate solution for treatment of melasma. Dermatol Surg. 2009;35:2050–2051. doi: 10.1111/j.1524-4725.2009.01333.x. [DOI] [PubMed] [Google Scholar]
- 62.Mahmoud BH, Ruvolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, et al. Impact of long-wavelength UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092–2097. doi: 10.1038/jid.2010.95. [DOI] [PubMed] [Google Scholar]
- 63.Mahmoud BH, Hexsel CL, Hamzavi IH, Lim HW. Effects of visible light on the skin. Photochem Photobiol. 2008;84:450–462. doi: 10.1111/j.1751-1097.2007.00286.x. [DOI] [PubMed] [Google Scholar]
- 64.Adalatkhan H, Amani F. The Correlation between melasma, ovarian cysts and androgenic hormones (a case control study) Res Biol Sci. 2007;2:593–596. [Google Scholar]
- 65.Hassan I, Kaur I, Sialy R, Dash RJ. Hormonal milieu in the maintenance of melasma in fertile women. J Dermatol. 1998;25:510–512. doi: 10.1111/j.1346-8138.1998.tb02445.x. [DOI] [PubMed] [Google Scholar]
- 66.Mahmood K, Nadeem M, Aman S, Hameed A, Kazmi AH. Role of estrogen, progesterone and prolactin in the etiopathogenesis of melasma in females. J Pak Assoc Dermatol. 2011;21:241–247. [Google Scholar]
- 67.Costin GE, Hearing VJ. Human skin pigmentation: melanocytes modulate skin color in response to stress. FASEB J. 2007;21:976–994. doi: 10.1096/fj.06-6649rev. [DOI] [PubMed] [Google Scholar]
- 68.Scott MC, Suzuki I, Abdel-Malek ZA. Regulation of the human melanocortin 1 receptor expression in epidermal melanocytes by paracrine and endocrine factors and by ultraviolet radiation. Pigment Cell Res. 2002;15:433–439. doi: 10.1034/j.1600-0749.2002.02051.x. [DOI] [PubMed] [Google Scholar]
- 69.Miot LD, Miot HA, Polettini J, Silva MG, Marques ME. Morphologic changes and the expression of alpha-melanocyte stimulating hormone and melanocortin-1 receptor in melasma lesions: a comparative study. Am J Dermatopathol. 2010;32:676–682. doi: 10.1097/DAD.0b013e3181cd4396. [DOI] [PubMed] [Google Scholar]
- 70.Im S, Lee ES, Kim W, On W, Kim J, Lee M, et al. Donor specific response of estrogen and progesterone on cultured human melanocytes. J Korean Med Sci. 2002;17:58–64. doi: 10.3346/jkms.2002.17.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kim NH, Cheong KA, Lee TR, Lee AY. PDZK1 upregulation in estrogen-related hyperpigmentation in melasma. J Invest Dermatol. 2012;132:2622–2631. doi: 10.1038/jid.2012.175. [DOI] [PubMed] [Google Scholar]
- 72.Ediger TR, Kraus WL, Weinman EJ, Katzenellenbogen BS. Estrogen receptor regulation of the Na+/H+ exchange regulatory factor. Endocrinology. 1999;140:2976–2982. doi: 10.1210/endo.140.7.6885. [DOI] [PubMed] [Google Scholar]
- 73.Stemmer-Rachamimov AO, Wiederhold T, Nielsen GP, James M, Pinney-Michalowski D, Roy JE, et al. NHE-RF, a merlin-interacting protein, is primarily expressed in luminal epithelia, proliferative endometrium, and estrogen receptorpositive breast carcinomas. Am J Pathol. 2001;158:57–62. doi: 10.1016/S0002-9440(10)63944-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Burkhart CG. Chloasma in a man due to oral hormone replacement. Skinmed. 2006;5:46–47. doi: 10.1111/j.1540-9740.2006.04323.x. [DOI] [PubMed] [Google Scholar]
- 75.Sialy R, Hassan I, Kaur I, Dash RJ. Melasma in men: a hormonal profile. J Dermatol. 2000;27:64–65. doi: 10.1111/j.1346-8138.2000.tb02122.x. [DOI] [PubMed] [Google Scholar]
- 76.Poisson Chloasma in a man with total hypogonadism. Bull Soc Fr Dermatol Syphiligr. 1957;64:777–778. [PubMed] [Google Scholar]
- 77.Pérez M, Sánchez JL, Aguiló F. Endocrinologic profile of patients with idiopathic melasma. J Invest Dermatol. 1983;81:543–545. doi: 10.1111/1523-1747.ep12522896. [DOI] [PubMed] [Google Scholar]
- 78.Lutfi RJ, Fridmanis M, Misiunas AL, Pafume O, Gonzalez EA, Villemur JA, et al. Association of melasma with thyroid autoimmunity and other thyroidal abnormalities and their relationship to the origin of the melasma. J Clin Endocrinol Metab. 1985;61:28–31. doi: 10.1210/jcem-61-1-28. [DOI] [PubMed] [Google Scholar]
- 79.Yazdanfar A, Hashemi B. Association of Melasma with Thyroid Autoimmunity: A Case-Control Study. Iran J Dermatol. 2010;13:51–53. [Google Scholar]
- 80.Sacre RC, Fernandes NC, Vaisman M, Tendrich M. Melasma idiopático: avaliação das funções tireoidiana, prolactínica e gonadal feminina. An Bras Dermatol. 1996;71:195–198. [Google Scholar]
- 81.Hughes BR. Melasma occurring in twin sisters. J Am Acad Dermatol. 1987;17:841–841. doi: 10.1016/s0190-9622(87)80279-7. [DOI] [PubMed] [Google Scholar]
- 82.Dynoodt P, Mestdagh P, Van Peer G, Vandesompele J, Goossens K, Peelman LJ, et al. Identification of miR-145 as a key regulator of the pigmentary process. J Invest Dermatol. 2013;133:201–209. doi: 10.1038/jid.2012.266. [DOI] [PubMed] [Google Scholar]
- 83.Kim NH, Lee CH, Lee AY. H19 RNA downregulation stimulated melanogenesis in melasma. Pigment Cell Melanoma Res. 2010;23:84–92. doi: 10.1111/j.1755-148X.2009.00659.x. [DOI] [PubMed] [Google Scholar]
- 84.Passeron T. Melasma pathogenesis and influencing factors - an overview of the latest research. J Eur Acad Dermatol Venereol. 2013;27:5–6. doi: 10.1111/jdv.12049. [DOI] [PubMed] [Google Scholar]
- 85.Kang HY, Suzuki I, Lee DJ, Ha J, Reiniche P, Aubert J, et al. Transcriptional profiling shows altered expression of wnt pathway- and lipid metabolism-related genes as well as melanogenesis-related genes in melasma. J Invest Dermatol. 2011;131:1692–1700. doi: 10.1038/jid.2011.109. [DOI] [PubMed] [Google Scholar]
- 86.Lee DJ, Lee J, Ha J, Park KC, Ortonne JP, Kang HY. Defective barrier function in melasma skin. J Eur Acad Dermatol Venereol. 2012;26:1533–1537. doi: 10.1111/j.1468-3083.2011.04337.x. [DOI] [PubMed] [Google Scholar]
- 87.Tomita Y, Maeda K, Tagami H. Melanocyte-stimulating properties of arachidonic acid metabolitespossible role in postinflammatory pigmentation. Pigment Cell Res. 1992;5:357–361. doi: 10.1111/j.1600-0749.1992.tb00562.x. [DOI] [PubMed] [Google Scholar]
- 88.Negishi K, Kushikata N, Tezuka Y, Takeuchi K, Miyamoto E, Wakamatsu S. Study of the incidence and nature of "very subtle epidermal melasma" in relation to intense pulsed light treatment. Dermatol Surg. 2004;30:881–886. doi: 10.1111/j.1524-4725.2004.30257.x. [DOI] [PubMed] [Google Scholar]
- 89.Kim EH, Kim YC, Lee ES, Kang HY. The vascular characteristics of melasma. J Dermatol Sci. 2007;46:111–116. doi: 10.1016/j.jdermsci.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 90.Pathak MA, Fitzpatrick TB, Kraus EW. Usefulness of retinoic acid in the treatment of melasma. J Am Acad Dermatol. 1986;15:894–899. doi: 10.1016/s0190-9622(86)70247-8. [DOI] [PubMed] [Google Scholar]
- 91.Duarte I, Campos Lage AC. Frequency of dermatoses associated with cosmetics. Contact Dermatitis. 2007;56:211–213. doi: 10.1111/j.1600-0536.2006.01051.x. [DOI] [PubMed] [Google Scholar]
- 92.Sanchez NP, Pathak MA, Sato S, Fitzpatrick TB, Sanchez JL, Mihm Jr MC. Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study. J Am Acad Dermatol. 1981;4:698–710. doi: 10.1016/s0190-9622(81)70071-9. [DOI] [PubMed] [Google Scholar]
- 93.Slominski AT, Botchkarev V, Choudhry M, Fazal N, Fechner K, Furkert J, et al. Cutaneous expression of CRH and CRH-R. Is there a "skin stress response system?". Ann N Y Acad Sci. 1999;885:287–311. doi: 10.1111/j.1749-6632.1999.tb08686.x. [DOI] [PubMed] [Google Scholar]
- 94.Slominski A, Zbytek B, Semak I, Sweatman T, Wortsman J. CRH stimulates POMC activity and corticosterone production in dermal fibroblasts. J Neuroimmunol. 2005;162:97–102. doi: 10.1016/j.jneuroim.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 95.Slominski A, Zbytek B, Szczesniewski A, Semak I, Kaminski J, Sweatman T, et al. CRH stimulation of corticosteroids production in melanocytes is mediated by ACTH. Am J Physiol Endocrinol Metab. 2005;288:E701–E706. doi: 10.1152/ajpendo.00519.2004. [DOI] [PubMed] [Google Scholar]
- 96.Bak H, Lee HJ, Chang SE, Choi JH, Kim MN, Kim BJ. Increased expression of nerve growth factor receptor and neural endopeptidase in the lesional skin of melasma. Dermatol Surg. 2009;35:1244–1250. doi: 10.1111/j.1524-4725.2009.01219.x. [DOI] [PubMed] [Google Scholar]
- 97.Adalatkhah H, Sadeghi-bazargani H, Amini-sani N, Zeynizadeh S. Melasma and its association with different types of nevi in women: A case-control study. BMC Dermatol. 2008;8:3–3. doi: 10.1186/1471-5945-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Adalatkhah H, Sadeghi Bazargani H. The association between melasma and postinflammatory hyperpigmentation in acne patients. Iran Red Crescent Med J. 2013;15:400–403. doi: 10.5812/ircmj.5358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mandry Pagan R, Sanchez JL. Mandibular melasma. P R Health Sci J. 2000;19:231–234. [PubMed] [Google Scholar]
- 100.Diffey BL, Tate TJ, Davis A. Solar dosimetry of the face: the relationship of natural ultraviolet radiation exposure to basal cell carcinoma localisation. Phys Med Biol. 1979;24:931–939. doi: 10.1088/0031-9155/24/5/006. [DOI] [PubMed] [Google Scholar]
- 101.Gupta AK, Gover MD, Nouri K, Taylor S. The treatment of melasma: a review of clinical trials. J Am Acad Dermatol. 2006;55:1048–1065. doi: 10.1016/j.jaad.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 102.Ritter CG, Fiss DV, Borges da Costa JA, de Carvalho RR, Bauermann G, Cestari TF. Extra-facial melasma: clinical, histopathological, and immunohistochemical casecontrol study. J Eur Acad Dermatol Venereol. 2013:271088–271094. doi: 10.1111/j.1468-3083.2012.04655.x. [DOI] [PubMed] [Google Scholar]
- 103.O'Brien TJ, Dyall-Smith D, Hall AP. Melasma of the arms associated with hormone replacement therapy. Br J Dermatol. 1999;141:592–593. doi: 10.1046/j.1365-2133.1999.03079.x. [DOI] [PubMed] [Google Scholar]
- 104.O'Brien TJ, Dyall-Smith D, Hall AP. Melasma of the forearms. Australas J Dermatol. 1997;38:35–37. doi: 10.1111/j.1440-0960.1997.tb01097.x. [DOI] [PubMed] [Google Scholar]
- 105.Pandya AG, Guevara IL. Disorders of hyperpigmentation. Dermatol Clin. 2000;18:91-8,ix. doi: 10.1016/s0733-8635(05)70150-9. [DOI] [PubMed] [Google Scholar]
- 106.Pandya A, Berneburg M, Ortonne JP, Picardo M. Guidelines for clinical trials in melasma. Pigmentation Disorders Academy. Br J Dermatol. 2006;156:21–28. doi: 10.1111/j.1365-2133.2006.07590.x. [DOI] [PubMed] [Google Scholar]
- 107.Al-Aboosi M, Abalkhail A, Kasim O, Al-Khatib A, Qarqaz F, Todd D, et al. Friction melanosis: a clinical, histologic, and ultrastructural study in Jordanian patients. Int J Dermatol. 2004;43:261–264. doi: 10.1111/j.1365-4632.2004.01606.x. [DOI] [PubMed] [Google Scholar]
- 108.Al-Samary A, Al Mohizea S, Bin-Saif G, Al-Balbeesi A. Pigmentary demarcation lines on the face in Saudi women. Indian J Dermatol Venereol Leprol. 2010;76:378–381. doi: 10.4103/0378-6323.66585. [DOI] [PubMed] [Google Scholar]
- 109.James WD, Carter JM, Rodman OG. Pigmentary demarcation lines: a population survey. J Am Acad Dermatol. 1987;16:584–590. doi: 10.1016/s0190-9622(87)70078-4. [DOI] [PubMed] [Google Scholar]
- 110.Ponzio HA, Cruz M. Acurácia do exame sob a lâmpada de Wood na classificação dos cloasmas. An Bras Dermatol. 1993;68:325–328. [Google Scholar]
- 111.Barcauí CB, Pereira FBC, Tamler C, Fonseca RMR. Classificação do melasma pela dermatoscopia: estudo comparativo com lâmpada de Wood. Surg Cosm Dermatol. 2009;1:115–119. [Google Scholar]
- 112.Kang HY, Bahadoran P, Suzuki I, Zugaj D, Khemis A, Passeron T, et al. In vivo reflectance confocal microscopy detects pigmentary changes in melasma at a cellular level resolution. Exp Dermatol. 2010;19:e228–e233. doi: 10.1111/j.1600-0625.2009.01057.x. [DOI] [PubMed] [Google Scholar]
- 113.Kang HY, Bahadoran P. Application of in vivo reflectance confocal microscopy in melasma classification. J Am Acad Dermatol. 2012;67:157–157. doi: 10.1016/j.jaad.2012.02.046. [DOI] [PubMed] [Google Scholar]
- 114.Ardigo M, Cameli N, Berardesca E, Gonzalez S. Characterization and evaluation of pigment distribution and response to therapy in melasma using in vivo reflectance confocal microscopy: a preliminary study. J Eur Acad Dermatol Venereol. 2010;24:1296–1303. doi: 10.1111/j.1468-3083.2010.03633.x. [DOI] [PubMed] [Google Scholar]
- 115.Costa MC, Eljaiek HV, Abraham LS, Azulay-Abulafia L, Ardigo M. In vivo reflectance confocal microscopy in a typical case of melasma. An Bras Dermatol. 2012;87:782–784. doi: 10.1590/s0365-05962012000500021. [DOI] [PubMed] [Google Scholar]
- 116.Kimbrough-Green CK, Griffiths CE, Finkel LJ, Hamilton TA, Bulengo-Ransby SM, Ellis CN, et al. Topical retinoic acid (tretinoin) for melasma in black patients. A vehicle-controlled clinical trial. Arch Dermatol. 1994;130:727–733. [PubMed] [Google Scholar]
- 117.Taylor S, Westerhof W, Im S, Lim J. Noninvasive techniques for the evaluation of skin color. J Am Acad Dermatol. 2006;54:S282–S290. doi: 10.1016/j.jaad.2005.12.041. [DOI] [PubMed] [Google Scholar]
- 118.Pratchyapruit W, Vashrangsi N, Sindhavananda J, Tagami H. Instrumental analysis of the pattern of improvement and that of recurrence of melasma in Thai females treated with Kligman-Willis triple combination therapy: confirmation by using its two different formulae. Skin Res Technol. 2011;17:226–233. doi: 10.1111/j.1600-0846.2010.00489.x. [DOI] [PubMed] [Google Scholar]
- 119.Pandya AG, Hynan LS, Bhore R, Riley FC, Guevara IL, Grimes P, et al. Reliability assessment and validation of the Melasma Area and Severity Index (MASI) and a new modified MASI scoring method. J Am Acad Dermatol. 2011;64:78–83. 78-83,83.e1-2. doi: 10.1016/j.jaad.2009.10.051. [DOI] [PubMed] [Google Scholar]
- 120.Hernández-Barrera R, Torres-Alvarez B, Castanedo-Cazares JP, Oros-Ovalle C, Moncada B. Solar elastosis and presence of mast cells as key features in the pathogenesis of melasma. Clin Exp Dermatol. 2008;33:305–308. doi: 10.1111/j.1365-2230.2008.02724.x. [DOI] [PubMed] [Google Scholar]
- 121.Jang YH, Lee JY, Kang HY, Lee ES, Kim YC. Oestrogen and progesterone receptor expression in melasma: an immunohistochemical analysis. J Eur Acad Dermatol Venereol. 2010;24:1312–1316. doi: 10.1111/j.1468-3083.2010.03638.x. [DOI] [PubMed] [Google Scholar]
- 122.Im S, Kim J, On WY, Kang WH. Increased expression of alpha-melanocyte-stimulating hormone in the lesional skin of melasma. Br J Dermatol. 2002;146:165–167. doi: 10.1046/j.1365-2133.2002.4513_3.x. [DOI] [PubMed] [Google Scholar]
- 123.Damoa AS, Lambert W, Schwartz R. Melasma: Insight into a distressing dyschromia. Aesthet Dermatol. 2006;8:1–6. [Google Scholar]
- 124.Sardesai VR, Kolte JN, Srinivas BN. A clinical study of melasma and a comparison of the therapeutic effect of certain currently available topical modalities for its treatment. Indian J Dermatol. 2013;58:239–239. doi: 10.4103/0019-5154.110842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ball Arefiev KL, Hantash BM. Advances in the treatment of melasma: a review of the recent literature. Dermatol Surg. 2012;38:971–984. doi: 10.1111/j.1524-4725.2012.02435.x. [DOI] [PubMed] [Google Scholar]
- 126.Rajaratnam R, Halpern J, Salim A, Emmett C. Interventions for melasma. Cochrane Database Syst Rev. 2010: doi: 10.1002/14651858.CD003583.pub2. [DOI] [PubMed] [Google Scholar]


