Abstract
Majocchi's granuloma is a persistent supurative folliculitis, associated with a deep granulomatous reaction induced by dermatophytes. There are two clinical forms of Majocchi's granuloma: the superficial form that appears in healthy individuals after localized trauma; and the nodular form, which occurs in inmunocompromised patients. We present a case of nodular Majocchi's granuloma on the forearm of an immunocompetent patient. Microbiological culture and examination of a deep aspiration sample identified Trichophyton rubrum. Collecting a deep sample of tissue is essential in achieving a good diagnostic performance.
Keywords: Arthrodermataceae, Case reports, Dermatomycoses, Diagnostic techniques and procedures, Folliculitis
CASE REPORT
A 53-year-old man presented with a 2-week old, rapidly growing, plaque on the right forearm. He worked as a seasonal olive harvester and may have unknowingly been scratched by an olive branch. The patient had not been treated with topical steroids for this condition and had never shaved his forearms. At the time of the physical examination, a keloid-like plaque was observed on the right forearm (Figure 1). Direct examination of the scales and the purulent discharge revealed no bacterial or hyphal elements. Microbiological investigation of a deep-aspiration identified signs of Trichophyton rubrum (Figures 2 and 3). Antifungal susceptibility test revealed sensibility to terbinafine, itraconazole and fluconazole. Biochemical and hematological analyses were performed to assess the immunologic status of the patient. Serology for HIV virus was negative; the Thelper/T-suppressor lymphocytes ratio and chest Xray were also normal. The patient was treated with itraconazole 400mg during 8 weeks, with an excellent therapeutic response.
FIGURE 1.

Tencentimeter diameter erythematous bumpy plaque, resulting in a keloid-like or brainy appearance. Yellow crusts and follicularcentered pustules were present on the surface
FIGURE 2.

Culture on Sabouraud's dextrose agar of a deep-aspiration sample yielded heaped and glaborous, pinkcolored colonies of Trichophyton rubrum within 4–5 days
FIGURE 3.
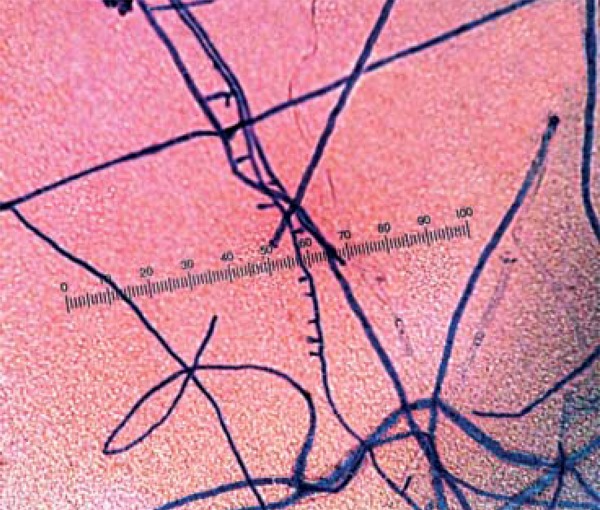
Lactophenol cotton blue mount showed septate hyphae with typical pencil- shaped macroconidia
DISCUSSION
The rupture of the hair follicle infundibulum caused by the dermatophyte infection in Majocchi's granuloma, originates dermal and subcutaneous tissue inflammation, resulting in the typical chronic erythematous and indurated plaques. Trichophyton rubrum is the most common dermatophyte isolated from Majocchi's granuloma but other fungi have been reported to be involved, including Trichophyton mentagrophytes, Trichophyton violaceum and Epidermophyton flocossum1,2 The collection of a tissue or deep-aspiration sample is required for efficient pathogen isolation and identification.3 Specific stains, such as the periodic acid-Schiff stain or Gomori methenamine-silver, may be necessary to visualize fungal elements in tissues. Follicular invasion in Majocchi's granuloma is usually endothrix. However, as in other inflammatory mycoses, like kerion, an endo-ectothrix mosaic pattern can be detected. There are two clinical forms of Majocchi's granuloma.4 The first is superficial and formed by granulomatous inflammation limited to the perifollicular area. It appears in healthy individuals after localized trauma, topical corticosteroid use, and chronic toenail or foot dermatophyte colonization. Superficial Majocchi's granuloma commonly occurs in young women who repeatedly shave their legs or after chronic corticosteroid treatment. The second is a deep form, characterized by subcutaneous granulomatous response and neutrophilic dermal abscesses. It is usually seen in inmunocompromised patients, such as transplant recipients and those with bone marrow malignancy or autoimmune diseases. Although the clinical appearance of the lesion in our study was more consistent with the deep form of Majocchi's granuloma, the patient was immunocompetent and there was no evidence of trauma, topical corticosteroid use or chronic dermatophyte colonization. There is no clear consensus on treatment regimen. However, systemic antifungals, such as azole antifungals, griseofulvin and terbinafine, are the mainstays of therapy, as they are safe and effective. The most reported regimens are itraconazole 200mg bid or terbinafine 250 mg daily. The duration of therapy should be at least 4 - 8 weeks, and treatment should be continued until all lesions have cleared.5
In conclusion, we report an unusual presentation of deep Majocchi's granuloma in an immunocompetent patient. In addition, this case highlights the importance of collecting deep microbiological samples for diagnosis.
Footnotes
Conflict of interest: None
Financial funding: None
Work performed at the University Hospital - Granada, Spain.
How to cite this article: Molina-Leyva A, Perez-Parra S, Garcia-Garcia F. Nodular plaque on the forearm. An Bras Dermatol. 2014;89(5):839-40.
REFERENCES
- 1.Chen HH, Chiu HC. Facial Majocchi's granuloma caused by Trichophyton tonsurans in an immunocompetent patient. Acta Derm Venereol. 2003;83:65–66. doi: 10.1080/00015550310002819. [DOI] [PubMed] [Google Scholar]
- 2.Bressan AL, Silva RS, Fonseca JC, Alves Mde F. Majocchi's granuloma. An Bras Dermatol. 2011;86:797–798. doi: 10.1590/s0365-05962011000400030. [DOI] [PubMed] [Google Scholar]
- 3.Gill M, Sachdeva B, Gill PS, Arora B, Deep A, Karan J. Majocchi's granuloma of the face in an immunocompetent patient. J Dermatol. 2007;34:702–704. doi: 10.1111/j.1346-8138.2007.00363.x. [DOI] [PubMed] [Google Scholar]
- 4.Kim JE, Won CH, Chang S, Lee MW, Choi JH, Moon KC. Majocchi's granuloma mimicking Kaposi sarcoma in a heart transplant patient. J Dermatol. 2011;38:927–929. [PubMed] [Google Scholar]
- 5.Romero FA, Deziel PJ, Razonable RR. Majocchi's granuloma in solid organ transplant recipients. Transpl Infect Dis. 2011;13:424–432. doi: 10.1111/j.1399-3062.2010.00596.x. [DOI] [PubMed] [Google Scholar]


