Abstract
Ostraceous psoriasis is a rare form of psoriasis, characterized by lesions with firmly adhered thick scales, in various colors, with surfaces resembling oysters shells. The protracted course of clinical presentation allied with peculiar lesions and histopathological examination permit the diagnosis. Lesions are usually resistant to topical medications, requiring systemic treatment. It is important that dermatologists are able to diagnose the unusual forms of psoriasis to avoid iatrogeny. We report the case of a patient with ostraceous psoriasis treated with methotrexate.
Keywords: Clinical diagnosis, Keratosis, Psoriasis
CASE REPORT
Twenty-six years old female patient reported hyperkeratotic, pruritic cutaneous lesions in upper and lower limbs for one year. She had tubal ligation performed three years before. On examination, there were hyperkeratotic hyperchromic plaques, with white, coarse and adherent scales on the dorsal area of the fingers, elbows, anterior and posterior surfaces of the right leg, dorsolateral regions of the feet and heels (Figure 1). The toenails presented full melanonychia and onychogryphosis (Figure 2). There were no signs of arthropathy. Biopsies on lesions on the left hand and foot revealed histopathological characteristics of psoriasis (Figure 3). The diagnosis of ostraceous psoriasis was then established. Topical keratolytic agents were introduced without improvement. Acitretin 25 mg/day was prescribed with significant reduction in the thickness of the lesions after 2 months, but without complete resolution. Acitretin was replaced by methotrexate 20 mg per week. There was further improvement but without clinical remission.
FIGURE 1.

Hyperkeratotic, hyperchromic plaques, with white adherent scales on the fingers extending to the distal half of the right hand dorsum and metacarpophalangeal joints on the left hand
FIGURE 2.

Hyperkeratotic, hyperchromic plaques, with white coarse adherent scales on the distal anterior surface of the legs and dorsolateral areas of the feet. Nails with full melanonychia and onychogryphosis
FIGURE 3.
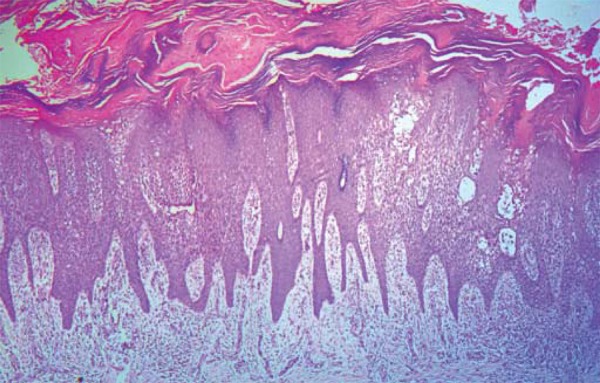
Acanthotic epidermis with regular elongation of interpapillary cones and atrophy in sections covering the dermal papillae. Focal spongiosis with intraepidermal vesicles. Hyperorthokeratotic stratum corneum, with Munro’s microabscesses
DISCUSSION
Psoriasis may present intensely hyperkeratotic lesions, thus being classified as ostraceous, rupioid and elephantine psoriasis.1,2 These varieties are extremely rare, with few reports in the literature. Some authors do not distinguish between hyperkeratotic forms of psoriasis and use the terms interchangeably. Lesions with firmly adhered thick scales, varying color and surface resembling an oyster shell are typical features of ostraceous psoriasis.2 The rupioid form is characterized by hyperkeratotic, concentric, circular and cone-shaped layers.1,2 Elephantine psoriasis lesions are defined as large, thick, plane, longstanding plaques, typically found in the dorsal area, buttocks and upper limbs.1,2
Ostraceous psoriasis should draw the attention of dermatologists by the exuberance of lesions, their resistance to topical treatments and association with psoriatic arthritis.3,4 The protracted course of the illness, associated with the peculiar appearance of the lesions and histopathological results permit the diagnosis.
Ostraceous psoriasis, verrucous Darier's disease and acquired palmoplantar keratoderma were considered as differential diagnoses in the case reported. The morphological and topographical features of the lesions, predominantly in extensor areas, favored the diagnosis of ostraceous psoriasis, which was confirmed by histological examination.
Most cases described in the literature are resistant to topical treatment, possibly because of the hyperkeratosis present in the lesions. There are reports of ostraceous psoriasis remissions with immunosuppressive and immunobiological drugs.3,4,5 In the case described here, there was no response to topical treatment. A significant reduction in the thickness of lesions was obtained with acitretin followed by methotrexate, although without complete remission.
The patient in question was noncompliant with the treatment and appropriate follow-up. She missed consultations, failed to bring in the required complementary exams and spontaneously discontinued the prescribed medications. For these reasons, we chose not to introduce immunobiological therapy.
Footnotes
Conflict of interest: None
Financial funding: None
Work performed at the Dermatology Clinic at Hospital Universitário da Universidade Federal de Sergipe (UFS) - Aracaju (SE), Brazil.
How to cite this article: Mesquita LSU, Sherlock J, Portugal FM, Mota LS, Fakhouri R, Silva SF. Case for diagnosis. Ostraceous psoriasis: a case report. An Bras Dermatol. 2014;89(5):841-2.
REFERENCES
- 1.Bernardi CDV, Schwartz J, Lecompte SM, Trez EG. Psoríase ostrácea - relato de caso. An Bras Dermatol. 2002;77:207–210. [Google Scholar]
- 2.Duque-Estrada B, Azevedo PMC, Tamler C, Avelleira JCR. Dermatologia comparativa: psoríase hiperceratósica. An Bras Dermatol. 2007;82:369–371. [Google Scholar]
- 3.Menon R. Ostraceous psoriasis presenting over distal extremities. Int J Dermatol. 2011;50:1115–1116. doi: 10.1111/j.1365-4632.2011.04873.x. [DOI] [PubMed] [Google Scholar]
- 4.Burbano C, Motta A, Díaz M, Rolón M. Psoriasis ostrácea com artritis psoriática tratada com infliximab. Rev Asoc Colomb Dermatol Cir Dermatol. 2007;15:241–243. [Google Scholar]
- 5.Arias-Santiago SA, Naranjo-Sintes R. Images in clinical medicine. Generalized ostraceous psoriasis. N Engl J Med. 2010;362:155–155. doi: 10.1056/NEJMicm0810475. [DOI] [PubMed] [Google Scholar]


