Abstract
BACKGROUND
Intensive care units (ICUs) function frequently at capacity, requiring incoming critically ill patients to be placed in alternate geographically distinct ICUs. In some medical ICU populations, “boarding” in an overflow ICU has been associated with increased mortality. We hypothesized that surgical ICU patients experience more complications when boarding in an overflow ICU and that the frequency of these complications are greatest in boarders farthest from the home unit (HU).
METHODS
A 5-year (June 2005 to June 2010) retrospective review of a prospectively maintained ICU database was performed, and demographics, severity of illness, length of stay, and incidence of ICU complications were extracted. Distances between boarding patients’ rooms and the HU were measured. Complications occurring in patients located in the same floor (BUSF) and different floor (BUDF) boarding units were compared and stratified by distance from HU to the patient room. Logistic regression was used to develop control for known confounders.
RESULTS
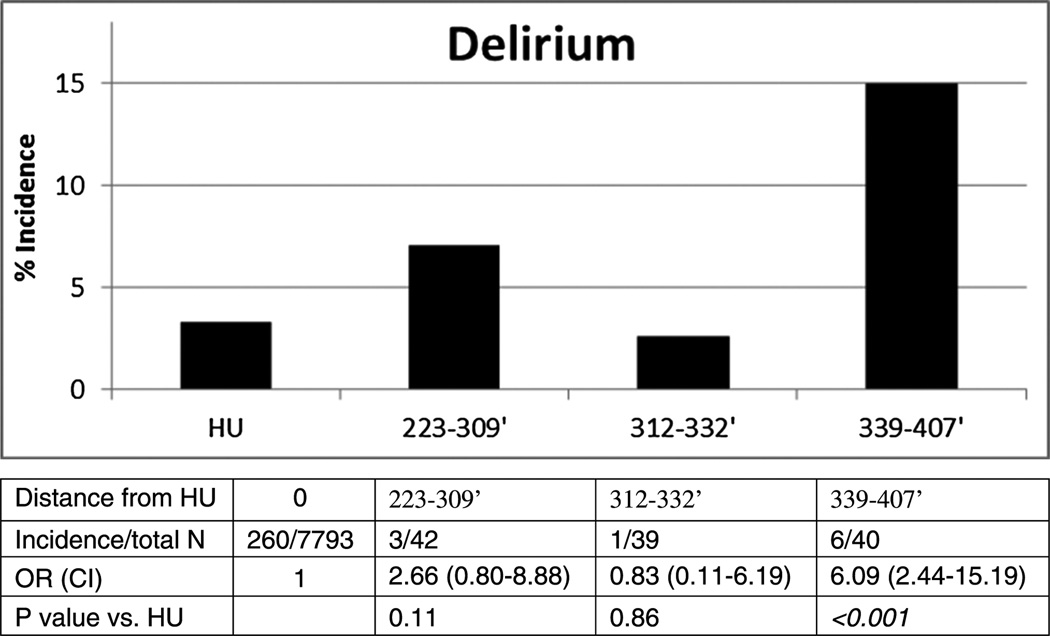
A total of 7,793 patients were admitted to the HU and 833 to a boarding unit (BUSF, n = 712; BUDF, n = 121). Boarders were younger, had a lower length of stay, and Acute Physiology and Chronic Health Evaluation II and were more of tentrauma/emergency surgery patients. Compared with in-HU patients, the incidence of aspiration pneumonia (2.2% vs. 3.6%, p < 0.01) was greater in BUSF patients and highest in those farthest from the HU (odds ratio [OR],2.39;p =0.01). Delirium occurred less often in HU than in BUDF patients (3.3% vs. 8.3 %, p < 0.01), and both delirium (OR, 6.09, p < 0.01) and ventilator-associated pneumonia (OR, 4.49, p < 0.05) were more frequent in patients farther from the HU.
CONCLUSION
Certain ICU complications occur more frequently in boarding patients particularly if they are located on a different floor or far from the HU. When surgical ICU bed availability forces overflow admissions to non–home ICUs, greater interdisciplinary awareness, education, and training may be needed to ensure equivalent care and outcomes.
LEVEL OF EVIDENCE
Epidemiologic study, level III. Therapeutic study, level IV.
Keywords: ICU boarding, off-service admissions, ICU complications, surgical intensive care
The availability of critical care resources is becoming progressively insufficient for an ever aging Western population. Recent reports have highlighted how the demand for intensive care beds continues to increase despite global cost-cutting measures that prevent their physical expansion.1 Institutions have thus used different strategies to accommodate patients who require critical care in the absence of preferred intensive care unit (ICU) accommodations.2–4 One solution has been to temporarily “board” critically ill patients in their existing hospital location such as the emergency department or the post anesthesia unit (PACU) while awaiting ICU bed availability. Several studies have suggested that such boarding practices may worsen patient outcomes and increase both length of stay (LOS) and mortality.5–7 In large hospitals where several distinct subspecialized ICUs coexist, another strategy is to admit critically ill patients to an ICU other than the preferred home (e.g., intended) ICU. The home ICU service then travels to this geographically distinct unit to administer care. A few studies have evaluated this practice, predominantly in medical ICU patients boarding in coronary care units (CCUs). Here, results vary, but some studies also have found worse outcomes with CCU boarding.3 Little is known about surgical ICU (SICU) patient outcomes when they board in subspecialized ICUs other than the preferred home SICU.
Our academic medical center frequently operates at 100% bed capacity and routinely admits SICU patients to alternate subspecialty ICUs when the home SICU (HU) is full. These boarding patients are cared for by nurses from the local unit and by the surgical critical care service (SCCS) that travels between the home and boarding units.
In the current study, we sought to determine if patients boarded in a geographically distinct subspecialized ICU and cared for by a travelling SCCS experienced greater ICU complications. We further hypothesized that the patients boarding farthest from the HU were at highest risk for complications.
PATIENTS AND METHODS
The study was approved by our institutional review board. All SCCS admissions queried between June 2005 and June 2010 in the Hospital of the University of Pennsylvania Surgical ICU database were considered for study.
SCCS: Composition
Surgical patients requiring ICU care originate from 1 of 17 admitting primary services (trauma, emergency surgery [ESS], colorectal, gastrointestinal, pancreatic, hepatobiliary, otorinolaryngology, urology, bariatric, obstetrics/gynecology, vascular, endocrine/oncologic, oral maxillofacial, orthopedic, plastic, solid organ transplantation, and thoracic surgery). Patients are randomly admitted to one of two SCCS teams (gold or green). Cardiac and neurologic surgery patients are not admitted to the SCCS. Although they are cared for by the SCCS, liver transplant SICU patients were excluded from the study because they are historically always admitted to the neuro-SICU (NSICU). Week-long daytime attending intensivist coverage alternates between dedicated critical care–trained anesthesiologists and trauma surgeons. Each SCCS team is composed of ICU fellows (anesthesia, trauma and pulmonary critical care), surgical, emergency medicine, or anesthesia residents (3–6 per team in month-long rotations) and experienced8 advanced practitioners (Certified Registered Nurse Practitioner—1–2 dedicated to either team). Night time in-house coverage includes one fellow and two residents. On evenings and weekends, a telemedicine service (nurse and intensivist) monitors patients through a video camera located only in HU rooms.
Prospectively Maintained SICU Database
The database is maintained by rounding CRNPs who enter demographic data (name, medical record number, age, sex, race, room number, Acute Physiology and Chronic Health Evaluation II [APACHE II] score, ICU admission/discharge date, ICU LOS, reason for ICU admission) in every SCCS patient at admission. Each SCCS patient is evaluated daily for any of 29 mutually exclusive complications that, if present, are added to their database entry. These include delirium, atrial fibrillation, myocardial infarction, cardiac arrest, acute lung injury (ALI), adult respiratory distress syndrome (ARDS), pneumonia, aspiration pneumonia, ventilator-associated pneumonia (VAP), self-extubation, reintubation, pneumonitis, acute renal failure, abdominal compartment syndrome, gastrointestinal bleed, adrenal failure, bacteremia, Clostridium difficile colitis, fungemia, line sepsis, septic shock, severe sepsis, urinary tract infection, deep venous thrombosis, decubitus ulcers, multiple-organ failure, and ICU death. To be designated a complication, these conditions cannot be present before admission or a reason for admission to the ICU. Definitions based on national society guidelines were created by an expert panel of intensivists and did not change in the 5-year study period (Supplemental Digital Content 1 http://links.lww.com/TA/A390). Although all previously mentioned complications (including death) were reviewed, only neurologic and respiratory conditions were selected as primary outcomes for the current study because they were deemed most common and relevant.
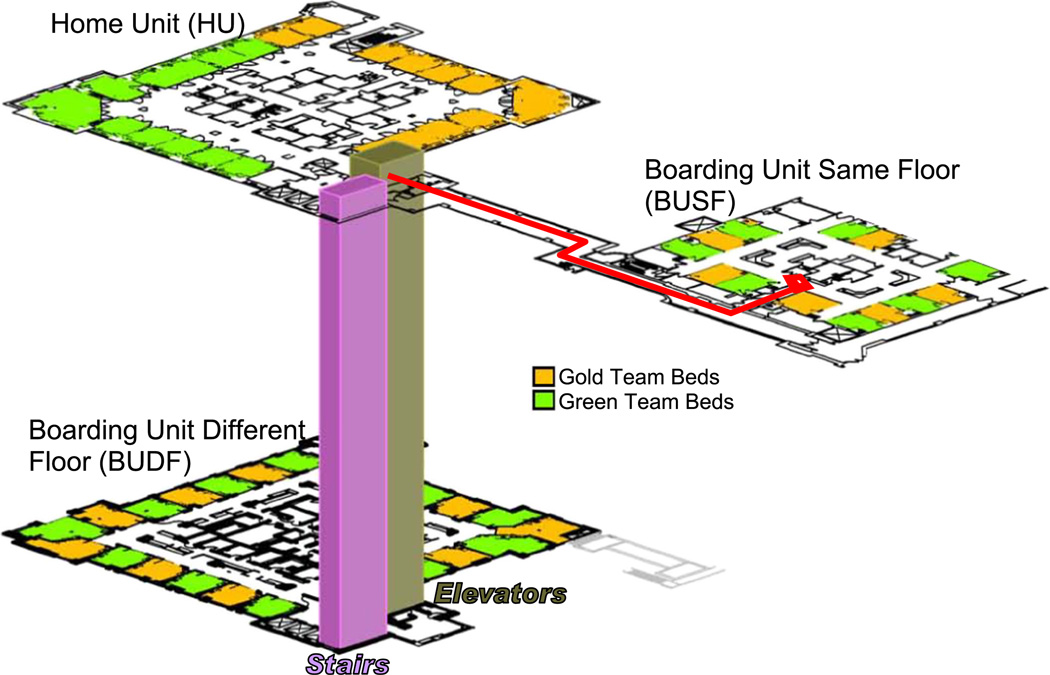
Geographic Location of Home and Boarding Units
The main SICU (HU) is composed of 24 beds distributed circularly around three nursing pods with touchdown spaces in each for chart documentation and computer consultation of laboratory work, radiology, and consultant notes. The principal boarding unit used when the HU is full is the NSICU. Before November 9, 2009, the NSICU was located on the same floor as the HU but in an adjacent building (boarding unit same floor [BUSF], 13 beds), requiring only horizontal travel from the HU (Fig. 1, path marked in red). After November 9, 2009, the NSICU remained the principal boarding unit but moved locations to three floors immediately below the HU (boarding unit different floor [BUDF], 22 beds). The nursing staff, physicians, treatment algorithms, physical resources, and leadership of the NSICU remained unchanged after the geographic move. A third unit, the cardiothoracic SICU, occasionally admits SCCS patients when the NSICU is also full, but their routine practice is to transfer them to the HU as soon as a bed becomes available and was thus excluded from the study before any analyses. The nursing standards, patient care nursing guidelines, nurse-to-patient ratio, average years of nursing experience, nursing certification (RN, BSN) are similar in all three ICUs.
Figure 1.
Geographical location between the Home SICU (HU), the Boarding SICU Same Floor (BUSF) and the Boarding SICU Different Floor (BUDF). In red is the travel path undertaken for the SICU service to reach BUSF patients. To reach BUDF patients the SICU service must travel directly down 3 floors using the stairs or elevators.
Distance From HU to Boarding Unit Rooms
A surveyor’s wheel was used to measure the distance between the HU and the threshold of every BUSF and BUDF patient room. Because the BUDF is located three floors below the HU, the stairs were measured linearly to obtain individual room distances. Alternatively, if team members used an elevator, average travel to each BUDF room was approximately 215 ft shorter than when using the stairs.
Statistical Analyses
Individual SCCS admissions were analyzed as one of five of the following populations: (1) all SCCS admissions (HU + boarding units], (2) HU only, (3) all boarders (BUSF + BUDF), (4) BUSF only, and (5) BUDF only. Analysis of variance with Bonferroni correction was used to evaluate differences in mean categorical parameters. Univariate analysis of categorical variables was conducted with χ2 analysis. In cases where confounding variables (APACHE II, LOS, age, sex, or proportion of trauma/ESS patients) were significantly different between groups, multivariate analysis with binomial regression controlled for identified confounders. SPSS software (version 20, SPSS, IBM Corp., Chicago, IL) was used for analysis. Continuous data are presented as mean with range and complication incidence as cases/group and odds ratio (OR) with 95% confidence intervals (CIs). A p < 0.05 was considered statistically significant.
RESULTS
Study Population
Between June 1, 2005, and June 1, 2010, 10,711 SCCS admissions were identified. Of these, 1,749 were excluded because they were either liver transplant patients or patients admitted overnight only to the PACU. Another 336 admissions boarding in the cardiothoracic SICU were also excluded. The remaining 8,626 SCCS admissions were identified as eligible for study inclusion. Of these, 7,793 (90.3%) were admitted to the HU and 833 (9.7%) were boarded in the NSICU (BUSF and BUDF). Of the 833 boarding patients, 712 were admitted to the BUSF and 121 to the BUDF. Compared with all boarders, HU patients were slightly older and had a higher APACHE II score and ICU LOS (Table 1). More admissions to the boarding units were trauma/ESS patients, the two primary services most often admitting to the SICU emergently. The most common reason for admission to the SCCS was postoperative observation following an elective routine operation such as Whipple, hepatectomy, or esophagectomy, where patient physiology is adequate and no organ failure is present, but because of the long and extensive surgery, the patient is routinely monitored for at least 24 hours in the ICU. The second most common reason was trauma observation where, for example the patient has an injury–liver laceration, cerebral hemorrhage, or flail chest–despite hemodynamic stability and no overt organ dysfunction, there is a known high risk for rapid deterioration that may require urgent intervention, and thus, close and frequent monitoring is needed.
TABLE 1.
Composition and Population Characteristics of Home and Boarding Unit Patients
| HU (n = 7,793) | All Boarded (BUSF + BUDF) (n = 833) | BUSF Only (n = 712) | BUDF Only (n = 121) | ||
|---|---|---|---|---|---|
| Age, mean (range) | 56.2 (13–101) | 54.1 (12–96)* | 53.8 (12–96)* | 55.5 (19–95) | |
| Sex, male, % | 60.4 | 59.5 | 59.6 | 59.5 | |
| Race,% | White | 69.3 | 66.6 | 66.7 | 66.1*** |
| African American | 23.9 | 26.1 | 24.9 | 33.1 | |
| Asian | 0.9 | 1.1 | 1.1 | 0.8 | |
| Other | 5.9 | 6.2 | 7.3 | 0 | |
| ICU LOS, mean (range), d | 4.5 (1–248) | 4.0 (1–156)† | 4.0 (1–156)† | 3.7 (1–43) | |
| Trauma or ESS, % | 37.5 | 45.5* | 43.8* | 55.4*** | |
| APACHE II, mean (range) | 15.2 (0–59) | 14.1 (0–50)* | 13.7 (0–49)* | 16.4 (0–50)** |
p < 0.001 versus HU.
p < 0.01 versus BUSF.
p < 0.05 versus HU.
Boarding Patients and the Incidence of Complications (All Boarders)
The nursing standards, patient care nursing guidelines, nurse-to-patient ratio, average years of nursing experience, and nursing certification (RN, BSN) were similar in the home and boarding units. However, the proportion of staff nurses with Certification for Adult, Pediatric and Neonatal Critical Care (CCRN) was greater (41%) than in either boarding unit (31%). In contrast, 30% of the boarding unit nurses were certified in neuroscience (Certified Neuroscience Registered Nurse) but none in the HU. When evaluating all (29) tracked complications (and death), none was found to occur more often in HU than in boarded patients. However, boarders had higher rates of aspiration pneumonia than those of HU patients (boarders, 3.4 vs. nonboarders, 2.2 %, p = 0.02) (Table 2). When controlling for LOS, APACHE II score, and proportion of trauma/ESS patients, this difference remained significant. The risk of having any complication (excluding death) was slightly higher in boarded patients.
TABLE 2.
Complications in HU and all Combined Boarding Patients
| HU (n = 7,793) | All Boarded (BUSF + BUDF) (n = 833) | p Univariate | p Multivariate* | |
|---|---|---|---|---|
| Aspiration pneumonia | 168 (2.2%) | 28 (3.4%) | 0.02 | 0.009 |
| VAP | 342 (4.4%) | 38 (4.6%) | 0.44 | 0.132 |
| Pneumonia otherwise not specified | 116 (1.5%) | 18 (2.2%) | 0.09 | 0.11 |
| Pneumonitis | 70 (0.9%) | 7 (0.8%) | 0.53 | 0.71 |
| ARDS | 141 (1.8%) | 10 (1.2%) | 0.12 | 0.28 |
| ALI | 223 (2.9%) | 19 2.3 (%) | 0.20 | 0.57 |
| Self-extubation | 147 (1.9%) | 10 (1.2%) | 0.10 | 0.15 |
| Reintubation | 257 (3.3%) | 26 (3.1%) | 0.44 | 0.71 |
| Delirium | 260 (3.3%) | 24 (2.9%) | 0.28 | 1.0 |
| Any complication (excluding death) | 1,116 (14.3%) | 130 (15.6%) | 0.17 | 0.006 |
| ICU death | 392 (4.9%) | 49 (5.9%) | 0.16 | 0.11 |
Controlling for ICU LOS, APACHE II, and trauma/ESS ratio.
Patients Boarding in an Adjacent Unit on the Same Floor (BUSF)
To remove the potential confounding effect of vertical travel to horizontal distances between HU and boarding beds, BUSF and BUDF admissions were analyzed independently. Aspiration pneumonia occurred more often in BUSF patients even after multivariate analysis (Table 3). However, delirium seemed to occur more often in the HU (3.3% vs. BUSF, 2.0%; p = 0.02), but this difference was lost with multivariate analysis. The risk of suffering any complication was slightly higher in the BUSF population. No complication occurred significantly more often in the HU than in the BUSF.
TABLE 3.
Complications in the BUSF and HU: The Effect of Greater Linear Distance for SCCS Teams to Travel
| HU (n = 7,793) | BUSF (n = 712) | p Univariate | p Multivariate* | |
|---|---|---|---|---|
| Aspiration pneumonia | 168 (2.2%) | 26 (3.6%) | 0.01 | 0.003 |
| VAP | 342 (4.4%) | 32 (4.5%) | 0.48 | 0.24 |
| Pneumonia otherwise not specified | 116 (1.5%) | 16 (2.2%) | 0.08 | 0.10 |
| Pneumonitis | 70 (0.9%) | 6 (0.8%) | 0.54 | 0.95 |
| ARDS | 141 (1.8%) | 9 (1.3%) | 0.18 | 0.38 |
| ALI | 223 (2.9%) | 16 (2.2%) | 0.20 | 0.40 |
| Self-extubation | 147 (1.9%) | 9 (1.3%) | 0.15 | 0.23 |
| Reintubation | 257 (3.3%) | 19 (2.7%) | 0.22 | 0.75 |
| Delirium | 260 (3.3%) | 14 (2.0%) | 0.02 | 0.15 |
| Any complication (excluding death) | 1,116 (14.3%) | 108 (15.2%) | 0.28 | 0.02 |
| ICU death | 392 (5.0%) | 41 (5.8%) | 0.22 | 0.11 |
Controlling for ICU LOS, APACHE II, and trauma/ESS ratio.
The BUSF: Boarding Farthest From the HU and the Incidence of Complications
When distributing the distances between BUSF rooms and the HU in three almost equal bins (377–410 ft, n = 228; 411–441 ft, n = 258; 446–476 ft, n = 226), the incidence of aspiration pneumonia increased with distance, with the farthest group displaying twice the HU incidence (OR, 2.39; 95% CI, 1.22–4.67; p = 0.01) (Supplemental Digital Content 2, http://links.lww.com/TA/A391). ICU mortality in the BUSF also tended to be greatest in the farthest beds from the HU (OR, 1.7), but this failed to reach statistical significance (p = 0.06) (Supplemental Digital Content 3, http://links.lww.com/TA/A392).
Boarding Patients on a Floor Different From That of the HU: The BUDF
To determine if vertical travel (stairs or elevator use) contributed differently to travel distances, admissions to the BUDF were analyzed separately. Again, no complication occurred, with significantly greater frequency in the HU than in the BUDF (Table 4). Delirium incidence in the HU occurred less than half as often as in the BUDF (3.3% vs. 8.3%, p = 0.001). Similarly, the occurrence of any complication was slightly greater in the BUDF, but this did not reach statistical significance (p = 0.08).
TABLE 4.
Complications in the BUDF and HU: The Effect of Vertical Travel for SCCS Teams to Travel
| HU (n = 7,793) | BUDF (n = 121) | p Univariate | p Multivariate* | |
|---|---|---|---|---|
| Aspiration pneumonia | 168 (2.2%) | 2 (1.7%) | 0.52 | 0.71 |
| VAP | 342 (4.4%) | 6 (5.0%) | 0.44 | 0.24 |
| Pneumonia otherwise not specified | 116 (1.5%) | 2 (1.7%) | 0.54 | 0.85 |
| Pneumonitis | 70 (0.9%) | 1 (0.8%) | 0.70 | 0.95 |
| ARDS | 141 (1.8%) | 1 (0.8%) | 0.36 | 0.48 |
| ALI | 223 (2.9%) | 3 (2.5%) | 0.54 | 0.91 |
| Self-extubation | 147 (1.9%) | 1 (0.8%) | 0.33 | 0.38 |
| Reintubation | 257 (3.3%) | 7 (5.8%) | 0.11 | 0.09 |
| Delirium | 260 (3.3%) | 10 (8.3%) | 0.008 | 0.001 |
| Any complication excl death | 1,116 (14.3%) | 22 (18.2%) | 0.14 | 0.08 |
| ICU death | 392 (5.0%) | 8 (6.6%) | 0.27 | 0.69 |
Controlling for ICU LOS, APACHE II, trauma/ESS ratio.
The BUDF: Added Vertical Travel on Horizontal Distances Between Boarding Patients and the HU
The distances from BUDF rooms to the HU were categorized into three bins (223–309 ft, n = 42; 312–332 ft, n = 39; 339–407 ft, n = 40), as measured from the HU entrance to each BUDF room using linear distance using the stairs. Incidence of delirium was highest in the group located farthest from the HU (OR, 6.09; p < 0.001, Fig. 2). Similarly, incidence of VAP increased with distance from the HU, reaching a maximum (OR, 4.49; p = 0.02) in the farthest group from the HU (Supplemental Digital Content 4, http://links.lww.com/TA/A393). Incidence of reintubation (OR, 2.60; 95% CI, 0.755–8.959; p = 0.13) and any complication (OR, 2.22; 95% CI, 0.933– 5.268; p = 0.07) was also greatest in the farthest group from the HU although this did not reach significance.
Figure 2.
Incidence of delirium as a function of distance from the HU in the setting of added 3 floor vertical travel (BUDF). Note the significantly greater incidence in patients farthest from the HU.
DISCUSSION
In the current 5-year study, we found that boarding ICU patients in an alternate ICU increased the risk of aspiration pneumonia, which occurred most often in beds farthest from the HU. When adding a vertical component for the SCCS to travel, delirium and VAP, both occurred most often in boarding patients located farthest from the HU. None of the 29 complications were found to occur with greater frequency in the HU than in any boarding unit.
In the last decade, there has been mounting concern at the increasing demand for critical care resources in the setting of insufficient ICU bed availability.9,10 In 1999, the Society of Critical Care Medicine published triage recommendations to guide rationing of resources when faced with insufficient ICU accommodations.11 However, neither these nor other guidelines have addressed alternate locations to admit ICU patients when the intended ICU is full. Institutions have thus internally developed methods to address this mounting discrepancy.
In some centers, postoperative populations awaiting ICU admission are “boarded” in the PACU. Studies evaluating this practice found that nurse staffing and training was insufficient to face the higher patient acuity and that this was associated with a significant mortality in boarded patients.12 Yet, irrespective of where postoperative patients reside while waiting SICU admission, delay in transfer to the SICU results in a longer time spent mechanically ventilated.13
Emergency department boarding of ICU patients is also common across US hospitals. The Institute of Medicine has recently identified this as a major concern for public health1 after several studies have identified worse outcomes and increased mortality.5,6,14,15
Another option has been to board ICU patients in alternate, unrelated subspecialty ICUs. In medical ICU populations, boarding in a CCU was found to increase ICU and hospital LOS, although other similar studies found no difference in any outcome measures between such boarders and nonboarders.16
Lott et al.17 evaluated 124 ICUs admitting patients to “diagnosis-appropriate” or “diagnosis-inappropriate” ICUs and found that risk-adjusted mortality was greatest in those boarding in diagnosis-inappropriate subspecialty ICUs. In particular, patients who underwent abdominal surgery (SICU) experienced a 30% greater mortality if admitted to a diagnosis-inappropriate subspecialty ICU. Another smaller study suggested that outcome differences may have occurred because of reduced compliance with HU care guidelines (e.g., deep venous thrombosis and gastrointestinal prophylaxis) in the boarding unit.18 In our study, mortality tended to be 24% greater in the BUDF than in the HU (p = 0.69).
Subspecialized critical care may be highly advantageous for certain conditions, but some authors have suggested that it may also compete with institutional efforts to standardize organization and management of general critical care.17 Furthermore, ICU adaptations made to build proficiency in a limited range of diagnoses may limit adaptability of personnel, to care for conditions outside the specialty unit’s expertise.4 In our study, boarding units were specialized in neurologic conditions, and reduced personnel familiarity, training, and certification with general surgical/trauma conditions may have contributed to worse outcomes in boarders.19
Greater distance between critically ill patients and their providers may also result in reduced oversight and discoordinated care, potentially delaying the evaluation of the newly arrived patient and recognition of subsequent subtle changes in their condition. Engoren20 found that each 1-hour delay in providers seeing a new critical care admission was associated with a 2.1% increased risk of death and LOS.
Medical providers may consciously or unconsciously perceive greater travel distances as a barrier to communication with bedside nursing or ancillary personnel (respiratory care, physiotherapy, etc.). It may thus seem more efficient to address several patient issues close together in the HU than to manage one in a remote boarding patient. This may lead providers to accumulate several issues on a given distant patient before travelling to their bedside. In parallel, the boarding unit nurse may also wait for several issues to collect before communicating with the home SCCS. In one large study evaluating avoidable errors occurring among surgeons and surgery residents, the inability to readily communicate with the nursing staff in person was raised as a key source of avoidable errors. This was attributed in part to less face-to-face communication between provider and bedside nurses.21 The latter point is particularly germane to the current study because redundant communication back and forth between providers (which occurs more readily when nurses and physicians are located in proximity) was a key principle identified to guide information transfer and communication best practices. It is difficult to determine exactly how adding a vertical distance to travel (i.e., stairs or elevator use) affected medical and nursing providers’ perceptions. In our study, boarding on a different floor resulted in a greater association between complications and distance from the HU.
Pneumonia, particularly VAP, is the most common infection present in SICUs,22,23 with several factors placing surgical patients at particular risk (i.e., altered gastrointestinal motility, airway/chest injury, diminished gag reflex24–27). A meticulous examination of practice patterns within both home and boarding units confirmed that all followed the same risk reduction strategies (semirecumbent position, continuous suctioning of subglottic secretions, stress ulcer prophylaxis).
Delirium is also a common complication in the ICU, and increasing evidence indicates that its incidence is greatly underestimated.28 As far as we could determine, all units used the same accepted practices to reduce ICU delirium (i.e., rapidly discontinuing benzodiazepines/opiates, optimizing sleep-wake cycles etc.29). However, we could not determine if there were differences in preexisting neurologic/psychiatric disease or the use of alcohol and drugs–important risk factors for delirium and, thus, potential confounders.
The current study has important limitations. First, it is a retrospective analysis of complications recorded in a prospective observational database. Second, certain complication definitions may now be outdated as they were chosen at the time of database launching (2003). For example, we did not use the Confusion Assessment Method to make the diagnosis of delirium, although current evidence suggests this is a preferable assessment method.29,30 Third, only HU rooms were equipped with cameras for continuous telemedicine surveillance, and we cannot be certain that telemedicine interventions in HU patients did not contribute to reduced complications. Fourth, the database could not identify patients admitted to a boarding unit who were subsequently transferred to the HU for the remainder of their ICU stay. Complications in these patients would have been assigned to the boarding unit even if they had occurred later after transfer to the HU. Fifth, greater neurologic expertise of boarding unit nursing staff may have led to greater identification of delirium in boarders. However, it was SCCS providers who independently identified complications using a single definition for all patients regardless of their location. Finally, we did not evaluate differences in boarding and HU personnel education, training, and degree of familiarity and experience with the broad range of general surgical conditions– important elements that may have affected complications.
We believe that our data establish a clear relationship between boarding of SICU patients and the development of complications. As suggested by others,31,32 what is required next is to identify in a structured manner the causative provider or system factors that can ultimately be mitigated. Perhaps, it is the long-standing experience and comfort of the interdisciplinary teams surrounded by familiar technology, infrastructure, and hierarchy of communication that has conditioned the HU for optimal performance. Much of this is acquired over time with repeated exposure to this particular population of patients. If this is the primary goal for optimal critical care outcomes, it would be simplistic and disingenuous to think that these characteristics can be rapidly transferred to the boarding unit staff without training and more constant exposure to the HU population of patients.
However, these data have led our critical care group to pursue a number of strategies to track and mitigate correctable elements associated with SICU boarding:
The concept of “repatriating” patients to the HU as soon as HU beds become available may need further exploration, although the idea of adding yet one more hand off to a new team of nursing providers has been shown in itself to increase complications.33
Additional education of nursing and ancillary disciplines and travelling medical teams now stresses the particular vulnerability of boarding patients and ensures at least an equal sense of ownership of those patients with clear and readily available communication channels (telephone, pagers, telemedicine cameras) between boarding unit staff and the HU medical team.
We are also creating a multidisciplinary forum where all disciplines of the different units are invited to discuss safety events occurring in boarded patients to identify real and perceived barriers to care and communications related to boarding. These events will be tracked by one of the hospital patient safety officers (J.L.P.) and brought to the institution’s quality and safety board to formulate concrete provider education initiatives and correct faulty system processes.
Finally, we have now consolidated the plan to bring boarding unit patients into the telemedicine watch, with intensivists alerted to their boarding status and keeping them under continuous watch.
CONCLUSION
This preliminary work indicates that boarding SICU patients elsewhere from the HU should be recognized as inherently adding a proportion of risk to the subsequent care and management of the critically ill patient. It further underscores an urgent need to formulate concrete interdisciplinary strategies to identify provider and system factors to mitigate the effects of a practice that will not likely disappear in the current environment of reduced critical care resources.
Supplementary Material
ACKNOWLEDGMENT
We would like to thank Anthony B. Annechino, University of Pennsylvania Real Estate, Design & Construction, for design of the three dimensional map of the SICU layout and Juulia Enberg, summer student, for the collection of surveyor wheel distance data between SICU and boarding unit beds.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
AUTHORSHIP
J.L.P. and P.M.R. designed this study. J.L.P. and M.P.R. conducted the literature search and collected data. M.D., D.N.H. and N.W.B. performed data analysis. J.L.P., N.W.B., S.R.A., D.N.H., B.A.K., C.A.S., C.W.S. and P.M.R. contributed to data interpretation. J.L.P. and N.W.B. wrote the manuscript. All authors participated in critical revision. J.L.P. and N.W.B. equally contributed to the first authorship of this manuscript.
DISCLOSURE
The authors declare no conflicts of interest.
REFERENCES
- 1.Institute of Medicine. [Accessed June 30, 2013];The future of emergency care in the United States health care system. doi: 10.1197/j.aem.2006.07.011. Available at: http://www.iom.edu. [DOI] [PubMed]
- 2.Sidlow R, Aggarwal V. “The MICUisfull”:one hospital’s experience with an overflow triage policy. Jt Comm J Qual Patient Saf. 2011;37:456–460. doi: 10.1016/s1553-7250(11)37058-4. [DOI] [PubMed] [Google Scholar]
- 3.American College of Emergency Physicians (ACEP) Boarding of admitted and intensive care patients in the emergency department. Policy statement. Ann Emerg Med. 2011;58:110. doi: 10.1016/j.annemergmed.2011.04.027. [DOI] [PubMed] [Google Scholar]
- 4.Angus DC, Black N. Improving care of the critically ill: institutional and health-care system approaches. Lancet. 2004;363:1314–1320. doi: 10.1016/S0140-6736(04)16007-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chalfin DB, Trzeciak S, Likourezos A, et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 6.Singer AJ, Thode HC, Jr, Viccellio P, et al. The association between length of emergency department boarding and mortality. Acad Emerg Med. 2011;18:1324–1329. doi: 10.1111/j.1553-2712.2011.01236.x. [DOI] [PubMed] [Google Scholar]
- 7.Ziser A, Alkobi M, Markovits R, et al. The postanaesthesia care unit as a temporary admission location due to intensive care and ward overflow. Br J Anaesth. 2002;88:577–579. doi: 10.1093/bja/88.4.577. [DOI] [PubMed] [Google Scholar]
- 8.Gracias VH, Sicoutris CP, Stawicki SP, et al. Critical care nurse practitioners improve compliance with clinical practice guidelines in “semiclosed” surgical intensive care unit. J Nurs Care Qual. 2008;23:338–344. doi: 10.1097/01.NCQ.0000323286.56397.8c. [DOI] [PubMed] [Google Scholar]
- 9.Wild C, Narath M. Evaluating and planning ICUs: methods and approaches to differentiate between need and demand. Health Policy. 2005;71:289–301. doi: 10.1016/j.healthpol.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 10.Ewart GW, Marcus L, Gaba MM, et al. The critical care medicine crisis: a call for federal action: a white paper from the critical care professional societies. Chest. 2004;125:1518–1521. doi: 10.1378/chest.125.4.1518. [DOI] [PubMed] [Google Scholar]
- 11.SCCM. Guidelines for ICU Admission, Discharge, and Triage. [Accessed June 30, 2013];Society of Critical Care Medicine. 1999 Available at http://wwwlearnicuorg/Pages/Guidelinesaspx.
- 12.Kiekkas P, Poulopoulou M, Papahatzi A, et al. Workload of postanaesthesia care unit nurses and intensive care overflow. Br J Nurs. 2005;14:434–438. doi: 10.12968/bjon.2005.14.8.17935. [DOI] [PubMed] [Google Scholar]
- 13.O’Callaghan DJ, Jayia P, Vaughan-Huxley E, et al. An observational study to determine the effect of delayed admission to the intensive care unit on patient outcome. Crit Care. 2012;16:R173. doi: 10.1186/cc11650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35:63–68. doi: 10.1016/s0196-0644(00)70105-3. [DOI] [PubMed] [Google Scholar]
- 15.Schull MJ, Vermeulen M, Slaughter G, et al. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44:577–585. doi: 10.1016/j.annemergmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Shanaah CAS, Milcarek B, Dellinger RP, Parrillo J, Zanotti S. Caring for critically ill patients outside the medical-surgical intensive care unit: does location have an impact on patient outcomes? (Abstract) CCM. 2006;34:A130. [Google Scholar]
- 17.Lott JP, Iwashyna TJ, Christie JD, et al. Critical illness outcomes inspecialty versus general intensive care units. Am J Respir Crit Care Med. 2009;179:676–683. doi: 10.1164/rccm.200808-1281OC. [DOI] [PubMed] [Google Scholar]
- 18.Vishnupriya K, Falade O, Workneh A, et al. Does sepsis treatment differ between primary and overflow intensive care units? J Hosp Med. 2012;7:600–605. doi: 10.1002/jhm.1955. [DOI] [PubMed] [Google Scholar]
- 19.Forster A, Tugwell P, van Walraven C. An hypothesis paper on practice environment and the provision of health care: could hospital occupancy rates effect quality? J Qual Clin Pract. 2000;20:69–74. doi: 10.1046/j.1440-1762.2000.00371.x. [DOI] [PubMed] [Google Scholar]
- 20.Engoren M. The effect of prompt physician visits on intensive care unit mortality and cost. Crit Care Med. 2005;33:727–732. doi: 10.1097/01.ccm.0000157787.24595.5b. [DOI] [PubMed] [Google Scholar]
- 21.Williams RG, Silverman R, Schwind C, et al. Surgeon information transfer and communication: factors affecting quality and efficiency of inpatient care. Ann Surg. 2007;245:159–169. doi: 10.1097/01.sla.0000242709.28760.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown DL, Hungness ES, Campbell RS, et al. Ventilator-associated pneumonia in the surgical intensive care unit. J Trauma. 2001;51:1207–1216. doi: 10.1097/00005373-200112000-00034. [DOI] [PubMed] [Google Scholar]
- 23.CDC. CfDCaP. [Accessed May 23, 2013];Ventilator-associated pneumonia (VAP) event. 2013 Available at http://wwwlearnicuorg/Pages/Guidelinesaspx from: http://wwwcdcgov/nhsn/PDFs/pscManual/6pscVAPcurrentpdf.
- 24.Ibanez J, Penafiel A, Raurich JM, et al. Gastroesophageal reflux in intubated patients receiving enteral nutrition: effect of supine and semirecumbent positions. JPEN J Parenter Enteral Nutr. 1992;16:419–422. doi: 10.1177/0148607192016005419. [DOI] [PubMed] [Google Scholar]
- 25.Sirvent JM, Torres A, Vidaur L, et al. Tracheal colonisation within 24 h of intubation in patients with head trauma: risk factor for developing early-onset ventilator-associated pneumonia. Intensive Care Med. 2000;26:1369–1372. doi: 10.1007/s001340000611. [DOI] [PubMed] [Google Scholar]
- 26.Croce MA, Tolley EA, Fabian TC. A formula for prediction of post-traumatic pneumonia based on early anatomic and physiologic parameters. J Trauma. 2003;54:724–729. doi: 10.1097/01.TA.0000054643.54218.C5. discussion 729–730. [DOI] [PubMed] [Google Scholar]
- 27.Ashraf M, Ostrosky-Zeichner L. Ventilator-associated pneumonia: a review. Hosp Pract. 1995;40:93–105. doi: 10.3810/hp.2012.02.950. [DOI] [PubMed] [Google Scholar]
- 28.van Eijk MM, Slooter AJ. Delirium in intensive care unit patients. Semin Cardiothorac Vasc Anesth. 2010;14:141–147. doi: 10.1177/1089253210371495. [DOI] [PubMed] [Google Scholar]
- 29.Inouye SK. Delirium in older persons. N Engl J Med. 2006;354:1157–1165. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 30.Bigatello LM, Amirfarzan H, Haghighi AK, et al. Effects of routine monitoring of delirium in a surgical/trauma intensive care unit. J Trauma Acute Care Surg. 2013;74:876–883. doi: 10.1097/TA.0b013e31827e1b69. [DOI] [PubMed] [Google Scholar]
- 31.Pronovost P, Holzmueller CG, Needham DM, et al. How will we know patients are safer? An organization-wide approach to measuring and improving safety. Crit Care Med. 2006;34:1988–1995. doi: 10.1097/01.CCM.0000226412.12612.B6. [DOI] [PubMed] [Google Scholar]
- 32.Pronovost PJ, Berenholtz SM, Goeschel C, et al. Improving patient safety in intensive care units in Michigan. J Crit Care. 2008;23:207–221. doi: 10.1016/j.jcrc.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 33.Parmentier-Decrucq E, Poissy J, Favory R, et al. Adverse events during intrahospital transport of critically ill patients: incidence and risk factors. Ann Intensive Care. 2013;3:10. doi: 10.1186/2110-5820-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.