Bipolar depression presents treatment challenges. Even with pharmacological stabilization of bipolar symptoms, up to 60% of individuals experience recurrence of bipolar depression within two years (Miklowitz, 2008). Adverse effects of lithium, anticonvulsants, and antipsychotics contribute to illness burden, comorbidity, and treatment non adherence (Malhi, Adams & Berk, 2009). Treatment of bipolar depression with antidepressants has not been substantiated by randomized controlled trials despite historical use of antidepressants in management of bipolar depression (Frye, 2011). These pharmacological challenges underscore consideration of effective psychological interventions in clinical treatment for bipolar depression.
The effectiveness of interpersonal and social rhythm therapy (IPSRT) in lengthening the time between episodes of bipolar symptoms has been demonstrated by a two year randomized controlled trial (Frank et al., 2005). IPSRT addresses medication adherence, interpersonal stressors, and establishment of daily routines (Frank, 2005). It is postulated that changes in daily routines burden the biochemical systems which regulate sleep, energy, and mood, thereby increasing the risk for bipolar episodes in vulnerable individuals. Interpersonal stressors, such as grief, role transitions, and relationship conflicts have potential to disrupt circadian and social rhythms and adversely impact mood. By establishing daily routines for sleep, wake, meals, and purposeful activity and addressing interpersonal problems, IPSRT intervenes to “stabilize patients’ social rhythms… improve current mood and functioning and to teach patients skills that will enable them to protect themselves against the development of new affective episodes” (Frank, 2007, p. 465).
IPSRT was specifically developed to address the circadian rhythm vulnerabilities associated with bipolar disorders (Frank, 2005). Salvatore et al. (2008) found that during acute episodes of mania or mixed illness states, patients with bipolar disorder had more daytime napping, lower total daytime activity, and a two hour phase advance when compared with healthy controls. When in remission, patients demonstrated more nighttime sleep, less daytime sleep and more total sleep compared to their acute episodes of mania or mixed illness states. Patients in remission, however, continued to differ from healthy controls in overall higher total sleep time, less daytime activity, and an approximate two hour phase advance of circadian motor activity, indicating that abnormalities of circadian rhythms persisted in patients with bipolar disorder, even while well. In a prospective study utilizing the Social Rhythm Metric tool, Shen, Alloy, Abramson, and Sylvia (2008), found that less social rhythm regularity predicted a shorter time to onset of major depressive, hypomanic, and manic episodes in individuals with bipolar spectrum disorders, even after controlling for family history of bipolar disorder and initial symptoms. Shen et al. (2008) reinforces findings of Frank et al. (2005) that when patients received IPSRT, the length of their wellness increased. The literature supports the effectiveness of individual IPSRT, but little has been published regarding group IPSRT.
Limited literature exists for educational, multifamily, and cognitive-behavioral groups for bipolar disorder. Although not psychotherapy, positive outcomes have been reported for educational groups (Colom et al., 2003; Colom et al., 2009). A five year follow up of 120 individuals with bipolar disorder who were randomized to group education (education on illness, treatment adherence, prodromal symptoms, recurrence, and lifestyle regularity) or non-structured support group found that the patients in the educational group had longer time to illness recurrence, fewer recurrences, and had a lower median number of hospitalized days (Colom et al., 2009).
Multifamily psychotherapy group for individuals with bipolar I disorder resulted in fewer hospitalizations compared to individuals receiving individual family therapy or medication management alone. Solomon, Keitner, Ryan, Kelley, and Miller (2008) randomized 53 patients to multifamily group (six sessions with multiple patients and their family members), individual family therapy (6–12 sessions with one patient and the patient’s family, with number of sessions determined by family needs), or medication management without psychotherapy (weekly sessions for the first month with decreasing frequency as symptoms improved). Patients were assessed monthly over 28 months. Fewer hospitalizations occurred for patients in the multifamily group (5%) compared to patients receiving individual family therapy (31%) or medication alone (38%).
Two randomized controlled studies compared cognitive behavioral group therapy and medication to medication treatment alone in individuals with bipolar I or II disorder. Gonzalez-Isasi et al. (2010) randomized twenty patients to 13 weekly sessions of cognitive behavioral group therapy (n=10) or medication alone (n=10). The cognitive behavioral group therapy topics included illness education, identification of early warning signs, social skills training, conflict resolution, cognitive restructuring, self-esteem building, and activity planning. Improvement for the cognitive behavioral therapy group, measured by the Global Assessment of Functioning, was significant 12 months after treatment, but not immediately after treatment or six months after treatment. Da Costa et al. (2011) randomized 41 individuals to 14 weekly sessions of cognitive behavioral group therapy (n = 27) or medication alone (n = 14). The cognitive therapy included education on bipolar disorder and cognitive behavioral skills based on the treatment manual “Cognitive-Behavioral Therapy for Bipolar Disorder” (Basco & Rush, 2005). A significant decrease in symptoms of mania, depression, and anxiety were reported immediately after treatment in the cognitive behavioral group therapy. No long term data were reported.
A randomized trial comparing a group program for bipolar disorder to treatment as usual reported improved outcomes for the group program. Castle et al. (2010) randomized 84 individuals with bipolar disorder type I, II, or not otherwise specified to a 12-week program with three booster sessions (n = 42) or to a control group (n = 42). Participants were followed for nine months after treatment. The control group consisted of treatment as usual and 12 weekly telephone calls. The program topics included bipolar disorder education, stress monitoring, relapse prevention, goal setting, medication management, and skill establishment. Participants in the 12-week program had significantly lower rates of relapse and spent less time ill during the 9-month follow-up period.
The literature supports education and psychotherapy in the comprehensive treatment of bipolar disorder. Although not specific to groups, a meta-analysis of randomized trials of adjunctive therapy for bipolar disorder (included individual and group education, systematic care, cognitive-behavioral therapy, family-focused therapy, and IPSRT), concluded that psychosocial treatments are cost-effective when symptom recurrence, daily functioning, and hospitalization are considered (Miklowitz, & Scott 2009).
Positive outcomes for IPSRT group modalities have been reported at the medical center where IPSRT was developed. Swartz et al. (2009) reported a significant decline in depressive scores (p < 0.001) for outpatient IPSRT groups (12–16 sessions) and increased utilization of the gym for patients in the daily inpatient IPSRT group (average hospital stay of 11 days). The Bipolar Intensive Outpatient group program (three times weekly with three hour group sessions and variable lengths of participation) demonstrated improved scores on the Quick Inventory of Depressive Symptomatology-Self-Rated at 60 days (Swartz et al., 2011).
Positive outcomes of IPSRT and group interventions led to the design of an outpatient IPSRT group (IPSRT-G) for bipolar depression for this study. This feasibility study was conducted to evaluate effectiveness of the 2-week IPSRT-G format as an adjunct to medication for individuals with bipolar depression and to determine satisfaction with the IPSRT-G treatment. This format was chosen secondary to the identified need for an intensive, time-limited outpatient program for individuals with bipolar depression who might benefit from IPSRT, but might not be able to participate in weekly psychotherapy. Tertiary care patients discharged from inpatient psychiatric units or referred by the outpatient mood consultation clinic could receive IPSRT treatment. A 2-week IPSRT-G provides access to treatment for individuals who might not have IPSRT treatment readily available in their home areas.
Method
This study was approved by the Mayo Clinic and Winona State University Institutional Review Boards. Participants were recruited through clinicians associated with the mood disorders inpatient unit and the outpatient consultative clinic of the Midwestern tertiary care medical center between October 2009 and January 2010. These referral clinicians were provided with educational material on IPSRT-G and the study protocol and asked to refer patients for whom psychotherapy for bipolar disorder was clinically recommended. The first author attended team meetings in the inpatient unit and outpatient mood consultative clinic to review the IPSRT treatment and answer questions. Referring clinicians contacted the first author with potential participants. Potential participants were screened for eligibility by study team members excluding the first author. The inclusion criteria consisted of: adults between the ages of 18–65; Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID) (First, Spitzer, Gibbon, & Williams, 2005) confirmed bipolar I or II depression; and referral for IPSRT-G. Exclusion criteria were: mania defined by the Young Mania Rating Scale (YMRS) (Young, Biggs, Ziegler, & Meyer, 1978) score of ≥ 15; active suicidal ideation defined by the Inventory of Depressive Symptomatology-Clinician Rated (IDS-C) (Trivedi, Rush, Ibrahim et al., 2004) question # 18, (response of 3); substance abuse as defined by the Alcohol Use Disorders Identification Test-4 (AUDIT) (Bohn, Babor, & Kranzler, 1995) score ≥ 5 or endorsement of the SCID interview questions regarding substance use in the past month; active symptoms of a primary personality disorder upon review of the electronic medical record; unstable or acute medical condition; or limited English speaking proficiency. Current symptoms of alcohol abuse, substance abuse or personality disorder excluded patients from the study. A lifetime history of alcohol, substance, or personality disorder did not exclude participation. Review of the electronic medical record substantiated bipolar disorder as the primary condition being referred for treatment. After receiving a complete description of the study and associated risks, participants provided written informed consent.
This IPSRT-G feasibility study utilized a pre and post intervention design with no comparative group. Two IPSRT-G program series were conducted. Patients were assigned to one of the two group program series based upon the time of referral and their scheduling preference.
Intervention
After eligibility was confirmed and consent obtained, participants were scheduled for two 60 minute individual psychotherapy sessions followed by six 60 minute group psychotherapy sessions over two weeks.. The individual therapy topics focused on the participant’s illness timeline, interpersonal focus areas, and introduction to the Social Rhythm Metric-II (SRM-II) (Monk, Flaherty, Frank, Hoskinson, & Kupfer, 1990). Identification of the interpersonal focus areas associated with the individual’s recent episode of illness and determination of individualized target times for daily social activities is inherent in IPSRT. The target times are determined by the individual monitoring their daily social rhythms in relationship to their mood and energy levels. Individuals frequently note improved mood and energy in context of regular routines in arising, eating, interacting with others, activity, medication administration, and bedtimes. The participants were asked to monitor their daily social rhythms following the first individual session. Connections between regular routines and mood or energy were discussed in the second individual session. Difficulties utilizing the SRM-II were problem solved prior to beginning group sessions. The focus areas of grief, role transitions, and relationship conflicts were identified in the process of graphing each individual’s episodes of illness in relationship to interpersonal stressors and social rhythm disruptions and understanding relationships important to the individual through the interpersonal inventory. This individual formulation is typically developed over the first three to five sessions of the 20–24 session individual IPSRT treatment (Frank, 2005). The desire to preserve the essential components of IPSRT and to quickly identify relevant focus areas for each participant resulted in development of the two individual sessions and six group sessions format. The two individual sessions permitted a comprehensive understanding of the participant’s illness in relationship to interpersonal problems and daily social rhythms prior to the participant beginning the group. The group sessions began as soon as eight eligible participants completed the two individual therapy sessions. The session topics are outlined in Table 1.
Table 1.
Interpersonal and Social Rhythm Therapy Session with Discussion Topics
| Therapy Session | Discussion Topic |
|---|---|
| 1. Individual | Patient goals, illness timeline, SRM-II. |
| 2. Individual | Interpersonal Inventory, define patient IPSRT focus areas, SRM-II. |
| 3. Group | Group orientation, define target times for daily routines, SRM-II. |
| 4. Group | Grief and medication adherence, SRM-II. |
| 5. Group | Interpersonal disputes and effect on daily routines, SRM-II. |
| 6. Group | Role transitions and effect on daily routines, SRM-II. |
| 7. Group | Review IPSRT strategies and application to daily routines, SRM-II. |
| 8. Group | Illness management, relapse prevention, and group termination, SRM-II. |
Note. Adapted from “Treating Bipolar Disorder: A Clinician’s Guide to Interpersonal and Social Rhythm Therapy,” by E. Frank, 2005. Copyright 2005 by the Guilford Press.
All individual and group therapy sessions were facilitated by a psychiatric clinical nurse specialist with interpersonal therapy (IPT) and group psychotherapy training, as well as an understanding of the IPSRT clinician manual (Frank, 2005). Three group sessions were held each week of the two week program. The group sessions began by discussing the SRM-II and target times for the participant’s daily social routines. Homework assignments were reviewed and problems resolved. Didactic information and discussion of the group topic followed. The topics included grief, loss of health, medication adherence, interpersonal disputes, role transitions, and illness management. Topics were adapted from the IPSRT clinician manual (Frank, 2005). Each session ended with review of homework expectations (completion of the SRM-II and implementation of participant identified interpersonal or behavioral strategies). The SRM-II tracked the influence of the interpersonal or behavioral strategies on the participants’ mood, energy, and target times for daily social routines and assisted in identification of daily patterns.
Each IPSRT-G was videotaped and/or observed by a psychiatric licensed clinical social worker (LICSW) for adherence to the IPSRT-G structure and clinician manual (Frank, 2005).
Measurements
Depressive symptoms were assessed using the 30-item IDS-C (Trivedi et al., 2004). Symptoms of mania were assessed by the 11-item YMRS (Young et al., 1978). Higher scores on the IDS-C and YMRS indicate more symptoms of depression or mania. Impairment in work, social life, and family/home responsibilities were evaluated by the 3-item Sheehan Disability Scale (SDS) (Sheehan, Harnett-Sheehan, & Raj, 1996). Overall illness severity was determined by the 3-item Clinical Global Impressions-Bipolar Version (CGI-BP) (Spearing, Post, Leverich, Brandt, & Nolen, 1997). Higher scores on the SDS and CGI-BP indicate greater impairment. The Medication Compliance Assessment (MCA) was developed to quantify medication adherence. Scores range from 1 (never missed medication) to 5 (stopped medication). Satisfaction with IPSRT-G was assessed by the 8-item Client Satisfaction Questionnaire (CSQ-8); the score range is 8–32 with higher scores indicating greater satisfaction (Larsen, Attkisson, Hargreaves, & Nguyen, 1979).
Two psychiatrists and four master’s prepared clinicians were trained on administration of the rating scales. Training included rating of videotaped patient interviews. A psychiatrist (MAF) and LICSW ratings of videotaped interviews defined the acceptable range of scores. If a clinician did not score within the acceptable range, further training was provided. The clinician rated additional interviews until the score was within the acceptable range. The percent of clinicians who scored within the acceptable range at the first interview for the CGI-BP, IDS-C, and YMRS was 100%, 90%, and 83% respectively. All six clinicians scored within acceptable range by the third interview.
This feasibility study measured change in (a) mood symptoms, (b) functioning, and (c) medication adherence at baseline, at the end of IPSRT-G (2-weeks), and 12-weeks. Participant satisfaction was assessed at IPSRT-G completion with the CSQ-8.
Analysis
Quantitative data were analyzed with JMP 8 statistical software using the Wilcoxon Signed-Ranks Test (z statistic, two tailed) to examine the difference between baseline, and 2-, and 12-week measures of symptoms, functioning, and medication adherence. Statistical significance was set at p ≤ 0.05. Descriptive statistics summarized participant characteristics.
Findings
Eighteen of 31 referred patients provided written informed consent. Of the 18, four were ineligible secondary to mania or failure to have SCID confirmed bipolar disorder. Nine of the fourteen eligible patients began one of the two IPSRT-G programs [index depression of 4.38 ± 3.9 months with moderate symptom severity as measured by the IDS-C (mean 31.88 ± 12)]. Five (63%) started the first IPSRT-G program with one participant ending after the first session. Two of the initial eight participants requested to start the second IPSRT-G program after not starting the first IPSRT-G. Four participants (50%) started the second IPSRT-G with one ending after the first session. Seven out of nine participants (78%) completed all group sessions and homework. All seven participants who continued after the first IPSRT-G attended all six sessions and completed the assigned homework. The mean interval between the individual sessions and IPSRT-G was 19 days (range 1 – 67 days). The majority of participants (86%) began IPSRT-G within 33 days of the individual sessions. One participant elected to defer participation to 67 days by attending the second IPSRT-G program. The only male participant who completed the program could not be reached for the 12-week follow-up. The demographic characteristics of the participants are displayed in Tables 2–3. The participants who withdrew (n = 2) had a mean age of 24.5 ± 4.95 years, depression duration of 3.5 ± 3.53 months, and a diagnosis of bipolar I disorder. Their mean ratings on the IDS-C, SDS and YMRS were 28 ± 14.14; 12.5 ± 4.94; 8 ± 8.48 respectively. The participants who completed IPSRT-G (n = 7) had a mean age of 46 ± 16.97 years, index depression duration of 4.64 ± 4.21 months, and 57% (4/7) had a bipolar I diagnosis. Their mean ratings on the IDS-C, SDS and YMRS were 33 ± 12.34; 22 ± 3.74; 6.71 ± 3.55 respectively.
Table 2.
Characteristics of Participants (n = 9) Who Began IPSRT-G as a Percentage of the Sample (no. in parentheses) and Mean (SD)
| Characteristic | M (SD) | % (no.) |
|---|---|---|
| Age | 41.22 (17.57) | |
| Female | 77% (7) | |
| Caucasian | 100% (9) | |
| Education (years) | 14.66 (1.87) | |
| Marital Status | ||
| Married | 33% (3) | |
| Single | 55% (5) | |
| Widowed | 11% (1) | |
| Employment Status | ||
| Full time | 44% (4) | |
| Part time | 22% (2) | |
| Student | 11% (1) | |
| Disabled | 11% (1) | |
| Unemployed | 11% (1) | |
| Bipolar I | 66% (6) | |
| Bipolar II | 33% (3) | |
| DSM IV-TR co morbidities (lifetime) | ||
| Anxiety Disorder | 22% (2) | |
| Personality Disorder | 22% (2) | |
| Alcohol Use Disorder | 44% (4) | |
| Index depression length in months | 4.38 (3.88) | |
Table 3.
Medication Taken by Participants (n = 9) who Began IPSRT-G as a Percentage of the Sample (no. in parentheses), Mean Dose and Range
| Medication | % (no.) | Dose in Milligrams M(SD) | Dose Range in Milligrams |
|---|---|---|---|
| Mood Stabilizer | |||
| divalproex sodium | 33% (3) | 1000 (433.01) | 750–1500 |
| lamotrigine | 44% (4) | 181.25 (114.33) | 25–300 |
| lithium | 33% (3) | 1000 (0) | 900–1200 |
| Antianxiety | |||
| alprazolam | 11% (1) | 1 (0) | 1 |
| clonazepam | 22 % (2) | 1.75 (1.76) | 0.5–3 |
| lorazepam | 22% (2) | 2 (1.41) | 1–3 |
| Antipsychotic | |||
| aripiprazole | 11% (1) | 2 (0) | 2 |
| olanzapine | 11% (1) | 10 (0) | 10 |
| quetiapine | 11% (1) | 350 (0) | 350 |
| Antidepressant | |||
| bupropion | 11% (1) | 150 (0) | 150 |
| amitriptyline | 11% (1) | 25 (0) | 25 |
| fluoxetine | 11% (1) | 40 (0) | 40 |
| sertraline | 11% (1) | 100 (0) | 100 |
| trazodone | 22% (2) | 125 (35.35) | 100–200 |
| venlafaxine | 11% (1) | 112.5 (0) | 112.5 |
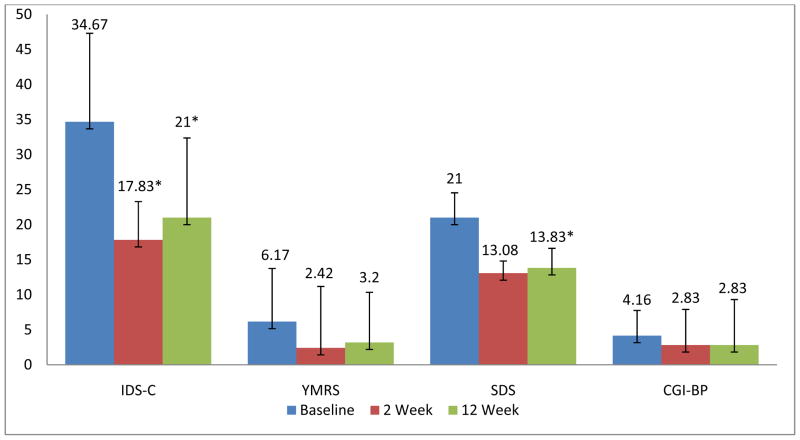
Quantitative data are presented in Table 4 and Figure 1. An equal number of participants diagnosed with bipolar I disorder (3/6) and bipolar II disorder (3/6) completed IPSRT-G and the 12-week telephone call. Depression scores (IDS-C) were significantly lower at 2-weeks (z = 10.5, p = 0.03) and 12-weeks (z = 10.5, p = 0.03) indicating decreased depressive symptoms at completion of IPSRT-G was maintained at 12-weeks. At 2-weeks, half (3/6) of the participants had a 50% reduction in IDS-C scores and 33% (2/6) met remission criteria (IDS-C score ≤ 12). At 12-weeks, 33% (2/6) had a 50% reduction in IDS-C scores and 16% (1/6) met remission criteria (IDS-C score ≤ 12). There was no worsening depression or induction of mania. Mania (YMRS) improved, but not significantly from baseline (mean 6.17 ± 3.54) to 2-weeks (mean 2.42 ± 1.74, z = 9.5, p = 0.06) or 12-weeks (mean 3.2 ± 2.79, z = 6, p = 0.25). Functioning (SDS) improved, but not significantly from baseline (mean 21. 33 ± 3.61), to 2-weeks (mean 13.08 ± 5.08, z = 9.0, p = 0.09). However, SDS scores improved significantly from baseline to 12-weeks (mean 13.83 ± 6.49, z = 10.5, p = 0.03). Overall bipolar illness severity (CGI-BP) improved, but not significantly from baseline (mean 4.16 ± 0.41) to 2-weeks (mean 2.83 ± 1.33, z = 3.0, p = 0.25) or 12-weeks (mean 2.83 ± 0.98, z = 7.5, p = 0.06). Mean medication adherence (MCA) was high at baseline (1.2 ± 0.49) and did not differ significantly at 2-weeks (1.33 ± 0.52, z = −0.5, p = 1.0) or 12-weeks (1.3 ± 0.82, z = −0.5, p = 1.0).
Table 4.
Baseline, 2 Week, and 12 Week Intervention Mean, Standard Deviation, Median, and Range of IPSRT-G Mood, Functioning, and Medication Compliance Scores
| Baseline (n = 9)
|
2 week (n = 7)
|
12 week (n = 6)
|
||||
|---|---|---|---|---|---|---|
| M (SD) | Median (Range) | M (SD) | Median (Range) | M (SD) | Median (Range) | |
| IDS-C | 31.88 (12.00) | 28 (17–47) | 18.71 (5.50) | 22 (12–24) | 21 (11.37) | 15.5 (11–36) |
| YMRS | 7 (4.33) | 5 (2–14) | 2.5 (1.61) | 3 (0–4.5) | 3.2 (2.79) | 2.5 (0–7) |
| CGI-BP | 4 (0.70) | 4 (3–5) | 2.85 (1.21) | 3 (1–4) | 2.83 (0.98) | 2.5 (2–4) |
| SDS | 19.88 (5.57) | 21 (9–26) | 15.5 (7.90) | 11 (8–30) | 13.83 (6.49) | 14.5 (5–22) |
| MCA | 1.33 (0.5) | 1 (1–2) | 1.43 (0.53) | 1 (1–2) | 1.3 (0.82) | 1 (1–3) |
IDS-C = Inventory of Depressive Symptomatology Clinician-Rated; YMRS = Young Mania Rating Scale. CGI-BP = Clinical Global Impressions-Bipolar version; SDS = Sheehan Disability Scale; MCA = Medication Compliance Assessment.
Figure 1.
Improving Depression, Mania, Functioning, and Overall Illness Severity Mean Scores of IPSRT-G Completers (n = 6). IDS-C = Inventory of Depressive Symptomatology Clinician-Rated; YMRS = Young Mania Rating Scale; SDS= Sheehan Disability Scale; CGI-BP= Clinical Global Impressions-Bipolar version. One standard deviation is represented by the standard deviation bars attached to each column. *Statistically significant difference from baseline utilizing the Wilcoxon signed ranks test, p = 0.03.
Satisfaction with IPSRT-G was high reflected by a mean CSQ-8 score of 26.83 ± 3.18 (95% CI = 23.48 – 30.17), a score range of 23 – 32, and a maximum possible score of 32.
Therapist fidelity was 100% adherent to the outlined IPSRT-G structure. The identified topic, review of SRM-II, and problem solving were addressed in each session.
Discussion
The preliminary findings suggest that IPSRT-G delivered adjunctive to medication in an intensive 2-week program is feasible and may contribute to improved depressive symptoms and maintenance of improvement at 12-weeks for women with bipolar disorder. The trend toward improvement in mania scores supports the overall mood stabilizing benefit of IPSRT-G and the unlikelihood that depression switching to mania is responsible for the outcome. Despite improvement, only 33% met remission criteria at 2-weeks and 16% met remission criteria at 12-weeks.
Improved functioning (SDS) was first significant at 12-weeks which may reflect the need for a period of symptom improvement prior to a change in functioning. Gonzalez-Isasi et al. (2010) reported improved functioning after cognitive behavioral group therapy 12 months after treatment, but not immediately after treatment or at six months. Notably, IPSRT-G participants improved in functioning despite only 16% of participants meeting criteria for remission of depressive symptoms. The IPSRT focus on management of interpersonal stressors and establishment of daily routines may directly improve social, occupational, and home functioning despite symptom persistence. Frank et al. (2008) indicate “simply treating the symptoms of the disorder does not often yield satisfactory results in the wider domains of psychosocial and occupational functioning” (pp.1562). Identifying factors which improve functioning is an opportunity for further research. Obtaining data regarding functioning, symptoms and social rhythm regularity at 6-month intervals over a two year period might provide further understanding of how social rhythms and symptoms impact functioning. Comparing the 2-week IPSRT-G program to a 3-week IPSRT-G program, weekly IPSRT-G, and individual IPSRT might determine if symptoms or functioning differ with these treatment delivery modalities.
IPSRT-G satisfaction scores are similar to mean CSQ-8 scores reported for individual IPSRT for bipolar II depression (n = 17, 26.8 ± 5.1 and 27.6 ± 5.9, Swartz, Frank, Frankel, Novick, & Houck, 2009) and group cognitive behavioral intervention for anxiety (n = 102, 24.44 ± 3.47, Houghton & Saxon, 2007). The IPSRT-G study supports the literature regarding patient satisfaction with IPSRT and group psychotherapy modalities. A larger, heterogeneous sample could provide further evidence regarding patient satisfaction with IPSRT-G as a treatment modality for individuals with bipolar depression.
Medication adherence did not contribute to the anti-depressive effect of IPSRT-G. Adherence did not change significantly from baseline, immediately after IPSRT-G or 12-weeks after IPSRT-G. This study supports the conclusions of Colom et al. (2003) that therapeutic factors, other than medication adherence, may impact effectiveness of psychological interventions for bipolar disorder.
The participant characteristics of this sample may reflect individuals who respond positively to IPSRT-G. The participants who withdrew (n = 2), cited reasons other than group as the reason for their withdrawal and had a diagnosis of bipolar I disorder; it may be that these participants had more symptoms of mixed bipolar depression as evidenced by higher YMRS scores, and were less likely to engage in psychotherapy. Gender may influence the effectiveness of IPSRT-G. Frank et al. (2008) found that occupational functioning improved earlier in females receiving IPSRT, suggesting gender differences in response. Six females and one male completed the IPSRT-G program; however the male did not complete the 12-week phone call. The symptom and functioning improvement in this study may be specific to females. A larger sample, including both males and females, and longer follow-up would be necessary to determine whether differences in response are due to gender or diagnosis and whether IPSRT-G needs to be adapted for these differences.
There are inherent limitations in the study design. Generalizability and conclusions are limited by the small sample of all females, absence of comparative group analysis, heterogeneity of medications, difficulty differentiating psychotherapeutic from pharmacological effects, and naturalistic clinical practice design. Without a larger heterogeneous sample and comparative group, it is difficult to attribute the anti-depressive response entirely to IPSRT-G or to identify the specific therapeutic factors contributing to symptom or functioning improvement.
Practice Implications
IPSRT-G provides a feasible adjunctive treatment for individuals experiencing a bipolar depressive episode. Further investigation is needed to determine optimal delivery strategies and to define the unique benefits of psychotherapeutic and pharmacological interventions for symptom and functioning improvement. Comparing the 2-week format to a 3-week or weekly IPSRT-G format may assist in determining the most effective group delivery method for routine clinical practice. Next steps include comparing 2-week IPSRT-G to medication treatment as usual and follow-up over 1–2 years.
In context of the pharmacological challenges and recurring episodes associated with bipolar depression, IPSRT-G provides a focused, time limited psychotherapy aimed at steadying the interpersonal and circadian rhythm disruptions inherent in bipolar disorder. Stabilizing daily social routines and mitigating the impact of interpersonal stressors provides patients with an armamentarium to increase wellness and a sense of control. As one participant stated, “it’s a master class” to learn skills to manage bipolar depression. Other participants commented on the benefit of the group format in feeling less alone in coping with bipolar disorder. The dearth of literature on group psychotherapy for bipolar depression provides an opportunity for advanced practice psychiatric nurses to develop group delivery models which incorporate the benefits of group psychotherapy and individual therapy research, such as IPSRT, into group modalities to treat bipolar disorder. Augmenting pharmacological treatment with psychotherapy to reduce episodes of acute symptoms, improve interpersonal functioning, and lessen social stigma will facilitate living rather than existing with the complexities of bipolar disorder.
Advanced practice psychiatric nurses are uniquely positioned among mental health professionals to incorporate the social, interpersonal, and biological strategies represented in IPSRT and help patients live with their illness. Nurses understand the interplay between life transitions, interpersonal conflicts, grief, medication, sleep, wakefulness, nutrition, physical activity, social support and routine on daily individual functioning and illness management. Historically, nurses have been the bedside educators and problem solvers in helping patients and families cope with a variety of health conditions and to translate health information into an individual’s daily life. Advanced practice psychiatric nurses have the skills to incorporate the pharmacological and psychological treatments into a plan of care compatible with an individual’s life goals. IPSRT provides a framework for advanced practice psychiatric nurses to translate bipolar disorder research into a healthier life for an individual and offers family members the knowledge to support their loved one’s illness management.
Acknowledgments
The authors wish to acknowledge the contributions of Grant Bauer, LICSW; Joanne Ericksen, RN, CNS; Simon Kung, MD; Mary Jo Moore, MAN, RN; Randy Stone, LICSW; Cindy Stoppel; Kristin S. Vickers, PhD; Mark Williams, MD and the Department of Psychiatry and Psychology, Mayo Clinic, Rochester, Minnesota in development and implementation of this study. Editorial assistance was provided by Elizabeth Pestka, RN CNS.
Funding Sources
This research was supported, in part, by Mayo Foundation and the Center for Translational Science Activities (CTSA) at Mayo Clinic. This center is funded in part by a grant from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) (RR024150 PI: Rizza). Its contents are sole responsibility of the authors and do not necessarily represent the official view of CTSA, NCRR or NIH.
Footnotes
Declaration of Conflicting Interests
Astrid A. Hoberg, Julie Ponto, and Pamela J. Nelson report no conflict of interest with respect to the authorship and/or publication of this article.
Mark A. Frye Disclosure
Grant Support -Pfizer, National Alliance for Schizophrenia and Depression (NARSAD), National Institute of Mental Health (NIMH), National Institute of Alcohol Abuse and Alcoholism (NIAAA), Mayo Foundation
Consultant - Dainippon Sumittomo Pharma, Merck, Sepracor
CME supported Activity - Astra-Zeneca, Bristol-Myers Squibb, Eli Lilly and Co., GlaxoSmithKline, Merck, Otsuka Pharmaceuticals, Pfizer, Sanofi-Aventis
Speakers’ Bureau – NONE
Financial Interest / Stock ownership / Royalties - NONE
References
- Basco MR, Rush AJ. Cognitive-behavioral Therapy for Bipolar Disorder. New York: The Guilford Press; 2005. [Google Scholar]
- Bohn MJ, Babor TF, Kranzler HR. The alcohol use disorders identification test (AUDIT): Validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol. 1995;56(4):423–432. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- Castle D, White C, Chamberlin J, Berk M, Berk L, Lauder S, Gilbert M. Group-based psychosocial intervention for bipolar disorder: Randomised controlled trial. The British Journal of Psychiatry. 2010;196:383–388. doi: 10.1192/bjp/bp.108058263. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Reinares M, Martinez-Aran A, Torrent C, Goikolea JM, Gasto C. Psychoeducation efficacy in bipolar disorders: Beyond compliance enhancement. Journal of Clinical Psychiatry. 2003;64(9):1101–1105. doi: 10.4088/jcp.v64n0917. [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, Sanchez-Moreno J, Palomino-Otiniano R, Reinares M, Goikolea JM, Martinez-Aran A. Group psychoeducation for stabilized bipolar disorders: 5-year outcome of a randomized clinical trial. The British Journal of Psychiatry. 2009;194:260–265. doi: 10.1192/bjp.bp.107.040485. [DOI] [PubMed] [Google Scholar]
- Da Costa RT, Cheniaux E, Legnani Rosaes PA, De Carvalho MR, Da Rocha Freire RC, Versiani M, Nardi AE. The effectiveness of cognitive behavioral group therapy in treating bipolar disorder: A randomized controlled study. Revista Brasileira de Psiquiatria. 2011;33(2):144–149. doi: 10.1590/s1516-44462011000200009. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV-TR axis I disorders. New York: Biometrics Research, New York State Psychiatric Institute; Apr, 2005. revision. [Google Scholar]
- Frank E. Treating bipolar disorder: A clinician’s guide to interpersonal and social rhythm therapy. New York: The Guilford Press; 2005. [Google Scholar]
- Frank E. Interpersonal and social rhythm therapy: A means of improving depression and preventing relapse in bipolar disorder. Journal of Clinical Psychology: In Session. 2007;63(5):463–473. doi: 10.1002/jclp.20371. [DOI] [PubMed] [Google Scholar]
- Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, Monk T. Two year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archives of General Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- Frank E, Soreca I, Swartz HA, Fagiolini AM, Mallinger AG, Thase ME, Kupfer DJ. The role of interpersonal and social rhythm therapy in improving occupational functioning in patients with bipolar I disorder. American Journal of Psychiatry. 2008;165(12):1559–1565. doi: 10.1176/appi.ajp.2008.07121953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye MA. Bipolar depression-A focus on depression. New England Journal of Medicine. 2011;364:51–59. doi: 10.1056/NEJMcp1000402. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Isasi A, Echeburua E, Mosquera F, Ibanez B, Aizpura F, Gonzalez-Pinto A. Long-term efficacy of a psychological intervention program for patients with refractory bipolar disorder: A pilot study. Psychiatry Research. 2010;176:161–165. doi: 10.1016/j.psychres.2008.06.047. [DOI] [PubMed] [Google Scholar]
- Houghton S, Saxon D. An evaluation of large group CBT psycho-education for anxiety disorders delivered in routine practice. Patient Education and Counseling. 2007;68:107–110. doi: 10.1016/j.pec.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- Malhi GS, Adams D, Berk M. Medicating mood with maintenance in mind: bipolar depression pharmacotherapy. Bipolar Disorders. 2009;11(Suppl 2):55–76. doi: 10.1111/j.1399-5618.2009.00711.x. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: State of the evidence. American Journal of Psychiatry. 2008;165(11):1408–1419. doi: 10.1176/appi.ajp.2008.08040488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Scott J. Psychosocial treatments for bipolar disorder: Cost-effectiveness, mediating mechanisms, and future directions. Bipolar Disorders. 2009;11(Suppl 2):110–122. doi: 10.1111/j.1399-5618.2009.00715.x. [DOI] [PubMed] [Google Scholar]
- Monk TH, Flaherty JF, Frank E, Hoskinson MA, Kupfer DJ. The Social Rhythm Metric: An instrument to quantify the daily rhythms of life. Journal of Nervous and Mental Disease. 1990;178:120–126. doi: 10.1097/00005053-199002000-00007. [DOI] [PubMed] [Google Scholar]
- Salvatore P, Ghidini S, Zita G, De Panfilis C, Lambertino S, Maggini C, Baldessarini RJ. Circadian activity rhythm abnormalities in ill and recovered bipolar I disorder patients. Bipolar Disorders. 2008;10:256–265. doi: 10.1111/j.1399-5618.2007.00505.x. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. International Clinical Psychopharmacology. 1996;11(Suppl 3):89–95. doi: 10.1097/00004850-199606003-00015. [DOI] [PubMed] [Google Scholar]
- Shen GHC, Alloy LB, Abramson LY, Sylvia LG. Social rhythm regularity and the onset of affective episodes in bipolar spectrum individuals. Bipolar Disorders. 2008;10:520–529. doi: 10.1111/j.1399-5618.2008.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon DA, Keitner GI, Ryan CE, Kelley J, Miller IW. Preventing recurrence of bipolar I mood episodes and hospitalizations: Family psychotherapy plus pharmacotherapy versus pharmacotherapy alone. Bipolar Disorders. 2008;10:798–805. doi: 10.1111/j.1399-5618.2008.00624.x. [DOI] [PubMed] [Google Scholar]
- Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the Clinical Global Impressions (CGI) scale for use in bipolar illness (BP): The CGI-BP. Psychiatry Research. 1997;73:159–171. doi: 10.1016/s0165-1781(97)00123-6. [DOI] [PubMed] [Google Scholar]
- Swartz HA, Frank E, Frankel DR, Novick D, Houck P. Psychotherapy as monotherapy for the treatment of bipolar II depression: A proof of concept study. Bipolar Disorders. 2009;11:89–94. doi: 10.1111/j.1399-5618.2008.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Frank E, O’Toole K, Newman N, Kiderman H, Carlson S, Ghinassi F. Implementing interpersonal and social rhythm therapy for mood disorders across a continuum of care. Psychiatric Services. 2011;62(11):1377–1380. doi: 10.1176/appi.ps.62.11.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Maihoefer C, O’Toole K, Buck N, Kiderman H, Henschke P, Frank E. Group interpersonal and social rhythm therapy across the continuum of care in routine practice settings. Poster presented at the 162nd Annual Meeting of the American Psychiatric Association; San Francisco, CA. 2009. May, [Google Scholar]
- Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, Kashner TM. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: A psychometric evaluation. Psychological Medicine. 2004;34(1):73–82. doi: 10.1017/s0033291703001107. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity, and sensitivity. British Journal of Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]