Abstract
Objective
Models of evidence-based practice emphasize the consideration of treatment efficacy/effectiveness, clinical expertise, and patient preference in treatment selection and implementation. However, patient preference for psychiatric treatment has been understudied. The aim of this meta-analytic review was to provide an estimate of the proportion of patients preferring psychological treatment relative to medication for psychiatric disorders.
Data Sources
A literature search was conducted using PubMed, PsycINFO, and the Cochrane Collaboration Library through August, 2011 for studies written in English that assessed patient preferences for the treatment of psychiatric disorders.
Study Selection
Studies assessing the preferred type of treatment including at least one psychological treatment and one pharmacological treatment were included. Of the 641 articles initially identified, 34 met criteria for inclusion.
Data Extraction
Authors extracted relevant data including the proportion of participants reporting preference for psychological and pharmacological treatment.
Results
Across studies, the proportion preferring psychological treatment was 0.75 (95% CI: 0.69 to 0.80), which was significantly higher than equivalent preference (i.e., higher than 0.50, p < .001). Sensitivity analyses suggested that younger patients (p < .05) and women (p < .01) were significantly more like to choose psychological treatment. A preference for psychological treatment was consistently evident in both treatment-seeking and unselected samples (ps < .05), but was somewhat stronger for the unselected samples.
Conclusions
Aggregation of patient preferences across diverse settings yielded a significant three-fold preference for psychological treatment relative to medication. Given the similar efficacy of these treatments for depression and anxiety, improving access to evidence-based psychological treatment is needed to connect more patients to their preferred treatment.
Introduction
Guidelines on the application of evidence-based practice (EBP) emphasize the synthesis of empirical evidence and clinical expertise with patient values and preferences in the selection and implementation of treatments.1,2 Patient preference becomes particularly important for guiding treatment decisions for psychiatric disorders for which both psychological and pharmacological treatments demonstrate efficacy, 3-6 particularly given the absence of evidence-based decision rules (i.e., treatment matching to patient clinical or sociodemographic characteristics) for treatment selection. Consideration of patient preference may also inform policy-level decisions about allocation of resources (e.g., funding for training) for the treatment of disorders without a clearly superior option in terms of efficacy or cost. Patient preference may also directly influence outcomes; a growing body of evidence suggests that providing patients with their preferred treatment is associated with better treatment retention and clinical outcomes.7-9
Despite the importance of patient preference, few studies have explored preferences for psychiatric treatments, and no accounting of the effect size of preferences across studies (i.e., meta-analysis) has been published. The purpose of the current study was to conduct a meta-analytic review of the literature on patient preferences for psychological versus pharmacological treatments for psychiatric disorders among adults. A thorough search of the literature was conducted and potential moderating variables such as type of psychiatric disorder, sample composition (e.g., age, sex, treatment-seeking), and study design variables (e.g., the type of preference assessment) were evaluated. These major domains of variability in study design were examined to identify any systematic differences in results due to design features. Consistent with previous research,7,10 we hypothesized that participants would report a preference for psychological relative to pharmacological treatments.
As is evident below, despite a broad-based search strategy, our analyses were limited to the studies of depression, anxiety, and a small number of general mental illness studies for which preference for treatment has been investigated. Our omnibus analyses include data from both treatment-seeking and unselected samples for which participants were asked to identify their treatment preference if they were to be diagnosed with a particular disorder. The perspectives of unselected (i.e., non-treatment-seeking) samples are relevant to our meta-analysis given that, according to National Comorbidity Survey-Replication data, more than half of those with a psychiatric disorder perceive barriers (either logistical or attitudinal) to seeking mental health care and accordingly did not utilize any mental health services in the previous year.11 Hence, understanding the preferences for treatment of such unselected samples is relevant for identifying perspectives of those not presenting to care to inform outreach and mental health literacy efforts to better connect individuals to care. To account for differences between those who were currently seeking treatment and analogue samples, we also conducted sub-group analyses to clarify the strength of effects across these subsamples.
Methods
Search Strategy
The search engines PubMed, PsycINFO, and the Cochrane Collaboration library were used to identify studies published through August, 2011. The following search terms and subject headings were used in combination: patient preference, consumer preference, therapeutics, psychotherapy, drug therapy, mental disorders, depression, anxiety, insomnia, bipolar disorder, schizophrenia, substance-related disorder, eating disorder, personality disorder. In addition, the reference sections of identified articles were examined to locate any additional articles not captured by this search.
Study Selection and Data Abstraction
Consistent with guidelines for reporting of meta-analyses of observational studies, we used broad inclusion criteria; and, rather than weight analyses using study quality ratings, we conducted sensitivity analyses relating study design features to outcomes.12 Of the studies identified using this search strategy, criteria for inclusion in the analysis were: (a) use of a forced-choice assessment of participant preference for type of treatment for a psychiatric disorder; (b) inclusion of treatment options with at least one psychological treatment and one medication; and, (c) study sample including individuals with a specific psychiatric disorder diagnosis (or sub-syndromal symptoms for a disorder) or unselected samples for which participants were asked to identify their treatment preference if they were to be diagnosed with a particular disorder (i.e., analogue samples). Among studies using treatment-seeking samples, the assessment of treatment preference must have occurred prior to the selection of (or randomization to) treatment. Thus, studies of both treatment-seeking samples and unselected general or medical samples were included; nonetheless, results from each of these samples were also examined individually.
Studies were excluded if they met any of the following criteria: (a) studies of treatment acceptability, perceived utility/effectiveness, or satisfaction not including pre-treatment preference assessment; (b) qualitative studies without a forced-choice preference question; and, (c) studies that were not published in a peer-reviewed journal. Two authors (RKM and ADP) extracted data from the articles and checked data for accuracy. Any inconsistencies in decisions regarding inclusion or data extraction were resolved by consensus decision.
For studies in which more than one psychological treatment (e.g., group or individual) and/or more than one medication were presented, these options were collapsed under the broader headings of psychological or pharmacological treatment. Several studies allowed participants to identify additional preferences (e.g., no preference, combined psychological and pharmacological treatment). For these studies, only participants expressing preference for psychological or pharmacological treatment were included. Sensitivity analyses were conducted to examine differences in proportions between studies that employed a dichotomous forced choice and those that included additional preference options.
Data Synthesis
The dependent variable in this analysis was the proportion of participants expressing preference for psychological treatment. The proportion expressing this preference in each study was converted to the logit scale (logit(p)=ln(p/[1-p]) and the variance of the logits estimated as var(logit(p))=1/N1+1/N2 where N1 and N2 are the numbers preferring psychological treatment and medication, respectively, and p=N1 / (N1 + N2). The logits were then combined using a random effects model, estimated by REML with SAS PROC MIXED. Estimates of the population values of the mean logit and between-study variation in the logits were then converted back to the original probability scale. Heterogeneity among the study logits was assessed with Cochrane’s Q test. When the studies are homogeneous, the sum of the squared and inverse-variance weighted deviations from the fixed effect model estimate follow a chi-square distribution with k-1 degrees of freedom. A significant deviation from this expected distribution indicates between study heterogeneity, and the need for a random effects model that assumes the underlying true logits follow an unknown (assumed normal) distribution with mean and variance to be estimated.
Sensitivity analyses were conducted by performing the same analysis in various subsets of the data of a priori interest, and also by inclusion of covariates that may moderate the proportion of subjects preferring psychological treatment. These variables included: treatment-seeking vs. non-treatment-seeking (analogue) samples, study assessment outcomes (i.e., whether more than 2 treatment choices were presented), disorder of interest, gender, and age. For the purpose of analyses, treatment-seeking was defined as patients pursuing mental health treatment in either a primary or specialty care setting. For studies that recruited participants who were not seeking treatment for mental health (e.g., patients screened as part of a primary care visit) and allowed participants to select no treatment, these studies were categorized as non-treatment-seeking. Given that the frontline treatment differs among disorders (e.g., pharmacotherapy is the clear front-line treatment for schizophrenia and bipolar disorder, whereas pharmacotherapy and psychotherapy are equally effective for anxiety and depressive disorders), our original analytic plan included subgroup analyses by psychiatric disorder. However, our search predominantly identified studies of depression and anxiety, and no studies of disorders for which pharmacotherapy is clearly the front-line treatment (see Trial Flow). Therefore, we estimated treatment preference in samples indicating preference for treatment for depression vs for any other disorder, and between studies of depression and anxiety disorders vs other/unspecified disorders (i.e. studies in which participants were asked to state preferences for mental health treatment generally).
Results
Trial Flow
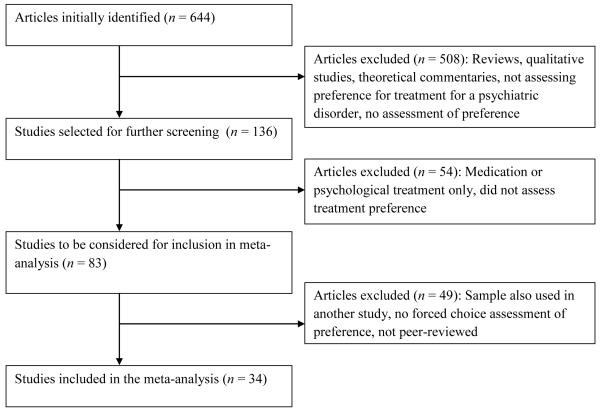
Based on the search methods used, 644 studies were initially identified and screened for inclusion/exclusion criteria. The final sample included 34 studies. For studies that did not present sufficient data in the manuscript for analysis, authors were contacted to request this information. One study was excluded because we were unable to obtain the needed data; results that were reported indicated that psychological treatment was preferred relative to medication for the treatment of depression.13 When more than one manuscript reported results from the same dataset (e.g., preliminary and final samples), we included only the manuscript describing analyses conducted with the largest sample. The study selection process is presented in Figure 1.
Figure 1.
Study selection process
Characteristics of the studies included in the analysis are presented in Table 1. The 34 studies included a total of 68,612 participants. Fifty percent of studies included treatment-seeking samples and the most commonly examined disorder was depression (65% of studies), followed by posttraumatic stress disorder (17%), other or unspecified disorders (12%), and other anxiety disorders (6%). Thus, the vast majority of studies examined depressive or anxiety disorders, with a small minority examining mental health more broadly or other related conditions (e.g., hypochondriasis).
Table 1.
Study Characteristics
| Study | Year | N | Disorder | Mean Age (y) |
Gender (% women) |
Treatment Seeking |
|---|---|---|---|---|---|---|
| Backenstrass et al.32 | 2006 | 415 | General | 45.3 | 59 | No |
| Becker et al.43 | 2009 | 379 | PTSD | 32.0 | 29 | No |
| Becker et al.44 | 2007 | 166 | PTSD | 18.6 | 62 | No |
| Brody et al. 45 | 2001 | 24 | Depression | 38.9 | 54 | Yes |
| Chilvers et al. 46 | 2001 | 220 | Depression | 37.3 | 74 | Yes |
| Churchill et al.47 | 2000 | 895 | Depression | 41.0 | 68 | No |
| Davidson et al.48 | 2010 | 80 | Depression | 59.3 | 54 | Yes |
| Deacon et al.49 | 2005 | 103 | Anxiety (general) | 35.4 | 53 | Yes |
| Dobscha et al.50 | 2007 | 314 | Depression | 56.7 | 7 | Yes |
| Dwight-Johnson et al.51 | 2000 | 1,187 | Depression | 44.0 | 71 | No |
| Dwight-Johnson et al.10 | 2010 | 287 | Depression | 49.8 | 84 | Yes |
| Fann et al.52 | 2009 | 145 | Depression | 42.4 | 34 | No |
| Feeny et al. Study 153 | 2009 | 74 | PTSD | 31.8 | 100 | No |
| Feeny et al. Study 253 | 2009 | 31 | PTSD | 31.0 | 100 | No |
| Feeny et al.54 | 2009 | 324 | PTSD | 19.6 | 100 | No |
| Fernandez y Garcia et al.30 | 2011 | 976 | Depression | -- | -- | No |
| Givens et al.41 | 2007 | 78,753 | Depression | -- | 74 | No |
| Goodman55 | 2009 | 455 | Depression | 31.6 | 100 | No |
| Hodges et al.33 | 2009 | 100 | Depression | 56.4 | 77 | Yes |
| Iacoviello et al.56 | 2007 | 75 | Depression | 40.0 | 53 | Yes |
| Jaycox et al.57 | 2006 | 444 | Depression | 17.2 | 75 | No |
| Kocsis et al.31 | 2009 | 429 | Depression | 45.0 | 65 | Yes |
| Kwan et al.58 | 2010 | 106 | Depression | 38.4 | 64 | Yes |
| Leykin et al.59 | 2007 | 174 | Depression | 39.6 | 59 | Yes |
| Lin et al.60 | 2005 | 335 | Depression | 57.0 | 4 | Yes |
| Mergl et al.7 | 2011 | 145 | Depression | -- | -- | Yes |
| Ogrodniczuk et al.61 | 2009 | 145 | General | -- | -- | Yes |
| Patel et al.62 | 2010 | 89 | OCD | 41.0 | -- | Yes |
| Raue et al.63 | 2009 | 60 | Depression | 51.2 | 78 | Yes |
| Unutzer et al.64 | 2003 | 1,797 | Depression | 71.2 | 65 | No |
| Van et al.65 | 2009 | 63 | Depression | -- | -- | Yes |
| Walker et al.66 | 1999 | 23 | Hypochondriasis | 47.0 | 83 | No |
| Zafar et al.67 | 2009 | 985 | General | 36.7 | 46 | No |
| Zoellner et al. 68 | 2003 | 273 | PTSD | 19.4 | 100 | No |
Note. General refers to studies in which preference was assessed for psychiatric disorders generally and not a specific diagnosis. PTSD = posttraumatic stress disorder, OCD = obsessivecompulsive disorder.
Quantitative Data Synthesis
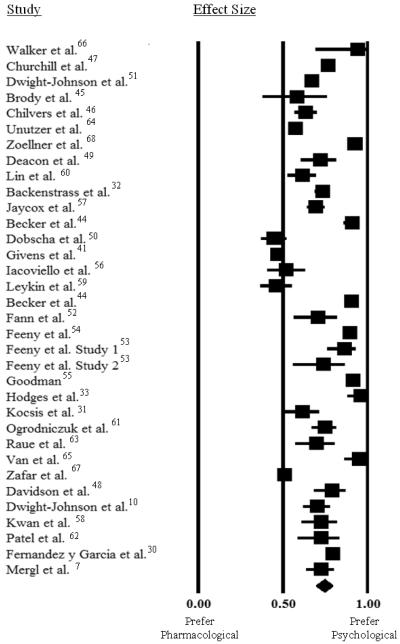
The Q test was highly significant (Q = 1,674, df = 33, p < 0.001), indicating that the studies are not homogenous. Therefore, the random effects model was adopted over the fixed effect model. Figure 2 shows the observed proportions in each of the 34 studies. Each proportion is enclosed in a 95% individual confidence interval, with standard errors computed using binomial variance. The population mean proportion preferring therapy was 0.75 (95% CI: 0.69 to 0.80), which is significantly higher than 0.50 (p < 0.001), the proportion that would indicate equal preference for psychological and pharmacological treatment. There was substantial between-study variation in the estimated true logit: 95% of all true study-specific proportions are estimated to lie within the prediction interval [0.37, 0.94].
Figure 2.
Effect Sizes (proportion) and 95% CI for Preferences for Pharmacological vs. Psychological Treatment
Subgroup Analysis
The primary analysis was repeated within subsets of the data characterized by studies that included more than two preference options (i.e., participants could also choose an alternate treatment such as combined medication and psychological treatment; n = 25 studies); studies examining the treatment of depression (n = 22) and depression or anxiety (n = 30); and treatment-seeking samples (n = 17) were examined as allowed by sample size.
The estimated population mean, its 95% confidence interval, and the 95% prediction interval for each of these sub-populations are displayed in Table 2. For each subset of studies, the 95% confidence interval did not include 0.50, indicating that the proportion of participants preferring psychological treatment was significantly greater than the proportion preferring medication across all subsamples. Specifically, although the preference for psychological treatment was less pronounced in treatment-seeking samples relative to non-treatment seeking samples (p = 0.03 for treatment-seeking when added as a covariate to the primary analysis), the subgroup of studies that only included treatment-seeking samples continued to demonstrate a significantly higher preference for psychotherapy than pharmacotherapy (69%; see Table 2). Similarly, the preference for psychological treatment was less pronounced in studies focused specifically on depression than in other studies (p = 0.03 for depression-focused treatment vs. all other when added as a covariate to the primary analysis), but again, continued to reflect a significant preference for psychotherapy over pharmacotherapy (70%; see Table 2). Studies that evaluated preference for a specific psychiatric disorder (including depression, anxiety disorders, and hypochondriasis) also exhibited a preference for psychological treatment (75%; CI = 0.69, 0.81), which was not significantly different from studies that examined unspecified disorders (p = 0.80). The availability of alternative preference options (e.g., combination therapy, watchful waiting/no treatment) was not associated with differences in the proportion preferring therapy (p = 0.92).
Table 2.
Subset Analyses of Proportion of Participants Preferring Psychological Treatment
| Subgroups | Mean | Lower 95% CL | Upper 95% CL | p |
|---|---|---|---|---|
|
|
||||
| Treatment Seeking Samples Only | 0.69 | 0.61 | 0.77 | <.001 |
| Samples given > 2 treatment choices | 0.75 | 0.68 | 0.80 | <.0001 |
| Samples expressing treatment preference for depression only |
0.70 | 0.62 | 0.77 | <.0001 |
Note. CL = confidence limit; p reflects significance of difference from equivalent preference (.50). Alternative treatment refers to studies in which participants had the options to select treatment options in addition to psychological or pharmacological treatments (e.g., combination therapy, exercise).
Mean age and proportion of women in each sample were added to the primary analysis as covariates. Mean age was significantly associated with the proportion preferring psychological treatment (p = 0.05), with younger samples being more likely to prefer psychological treatment than older samples. Sex was also significantly associated with the proportion preferring psychological treatment (p = 0.01), with samples with a greater proportion of women preferring therapy at higher rates.
Publication Bias
A funnel plot of the observed logits versus the reciprocals of their variances (not shown) was examined as a check for patterns consistent with possible publication bias. Asymmetry of the plot was observed, with the most precise (i.e., small variance) studies tending to have logits near zero (i.e., proportions near 0.50). The large study by Givens et al. in particular fit this pattern; however, the rest of the data also conformed to this pattern. In a set of homogeneous studies free from publication bias, this plot should have the appearance of a symmetrical inverted funnel that converges near the estimated common effect size (logit of 0.69 for this set of studies). Asymmetry is consistent with a bias mechanism by which studies that would have appeared on one side of the plot (i.e., those providing evidence opposite to the trend in the observed studies) tend to be missing. However, it is known that when the studies are not homogeneous, asymmetry is not necessarily indicative of missing study bias.14 Because this set of studies displays marked departure from homogeneity, the asymmetry of the funnel plot is not particularly informative regarding potential publication bias.
Therefore, to assess sensitivity to possible publication bias in the form of unpublished studies (of note, we did not include unpublished studies in the current analysis) that would support the hypothesis of preference for pharmacological over psychological treatment, the primary analysis was repeated with the addition of k hypothetical studies with observed logits equal to −1.09 (i.e., proportions equal to 0.25) and logit variances equal to 0.04. The proportion was chosen as the counter-null to the observed population average (i.e., the value that supports medication as strongly as the actual data support psychological treatment). The variances of the logit of these proportions was chosen to be equal to the median logit variance among the observed studies and implies a sample size of N=130 per virtual missing study. An addition of 22 of these virtual studies would be required to lead to a failure to reject the null hypothesis for the comparison of the observed proportion to equivalence (0.50). We therefore conclude that the overall preference for psychological treatment over medication is robust to publication bias.
Discussion
This meta-analysis provides evidence that adults prefer psychological to pharmacological treatment for unipolar depression and anxiety disorders. Across 34 studies spanning primary and specialty care settings as well as non-treatment-seeking samples, participants were 3 times more likely to express a preference for psychological treatment. Although preference for psychological treatment was stronger in certain sub-groups (e.g., non-treatment-seeking samples, younger samples), all subsample analyses continued to show a significant preference for psychological over pharmacologic treatments.
According to the tenets of EBP, without evidence for the superiority of one treatment over the other, patient preference should guide selection of treatment. 1,2 According to meta-analytic review, pharmacological and psychological treatments studied in clinical trials for treatment of depression and anxiety achieve comparable outcomes. 6,15-19 Accordingly, given comparable outcome data, the preference data support empirically-based practice decisions in favor of greater rates of selection of psychological treatment for these disorders. Interestingly, recent patterns of treatment utilization reflect the opposite pattern. The past 10 years have seen a substantial increase in the prescription of antidepressant medications, which surpassed all others as the most commonly prescribed class of medication in the US in 2005. 20, 21 There is also evidence of a concurrent decrease in patients receiving psychological treatment.21 However, the available data on patient preference, efficacy, and cost-efficacy for depression and anxiety do not support this trend,22-24 and imply that many patients are not engaged in their preferred psychological treatment. It should be noted that despite high rates of initiation of antidepressant pharmacotherapy for mood and anxiety disorders, adherence to these agents over time is generally poor. 25-27 It is not clear how much initial preference for treatment plays a role in these adherence findings relative to other issues such as side effects and patient attitudinal variables and provider characteristics.27 In the absence of empirical studies on the topic, it is unclear why the shift towards pharmacological and away from psychological treatment is occurring, although limited access to evidence-based psychological treatments certainly plays some role.28, 29
Due to the limited number of studies that assessed preference for combination pharmacological and psychological treatment, we were unable to examine this preference as part of the meta-analysis. Among studies that included combination treatment as an option, many participants expressed a preference for this option, which often, 30, 31 but not always, 32, 33 was preferred over each of the monotherapies. Although combination treatment is associated with additive benefits for some disorders, 34,35 in other disorders this may be associated with either very modest or no benefit,36, 37 despite higher cost.24
We were unable to conduct sensitivity analyses examining differences among samples based on factors such as culture, race, and ethnicity. These are particularly important individual difference variables to consider given that access to treatment38 and factors such as stigma39 can vary substantially across these groups. Research on the acceptability of treatment for depression has suggested that African American and Hispanic participants report lower acceptability of medication relative to White participants.40 Similarly, one study included in the current meta-analysis found that African American, Asian/Pacific Islander, and Hispanic participants were more likely to report a preference for psychological treatment than medication relative to White participants.41 Further research is needed to understand the nature of these group differences and how this may impact access and decision-making in mental health care.
There are several limitations to the current study. First, the evaluation of preference for alternative options (e.g., combination therapy) was not possible given variability in methods across studies. It is unclear whether there would be differential preference for psychological vs. pharmacological treatment in studies with multiple preference options had participants been forced to choose between the two. However, sensitivity analyses indicated no significant differences between studies that offered more than 2 treatment options and those that used a forced-choice between psychotherapy and medication. Similarly, the settings and samples included in this meta-analysis were heterogeneous because we elected to maximize generalizability of findings. Sensitivity analyses indicated that although there was some variability among these groups in the magnitude of preference for psychological treatment, the overall preference for this treatment was maintained across the subgroups studied.
We did not include unpublished articles in this study. Although this has the potential to introduce publication bias, we elected to exclude these articles to maximize the quality of studies selected (i.e., only those identified by peer review to exhibit sufficient scientific rigor for publication). The studies included in this review did not consistently include data on illness severity, and thus we are unable to assess the association between the severity of symptoms or urgency of treatment need and preference. Examination of this and related potential moderating variables are an important future direction for this line of research.
Estimates of publication bias, such as the fail safe N have limitations and thus should be interpreted with caution. Nonetheless, across studies only 1 yielded a significant effect size in the meta-analysis in favor of medication, suggesting that these results are robust. Because the studies in this area are predominantly focused on depression and anxiety, generalizability of these results to other disorders is unclear. Our original aim was to include studies across the spectrum of psychiatric disorders; however, there were no published studies on patient preference for many psychiatric disorders or for co-occurring disorders. Future research examining preferences for other types of mental illness, in particular whether preferences vary based on the front-line treatment for disorders (e.g., pharmacotherapy for psychotic disorders), is an important question for understanding potential discrepancies between efficacy and patient preferences.
Our meta-analysis was not able to address the important question of why psychological treatment is preferred over medication. In a qualitative study of preferences for treatment for posttraumatic stress disorder, beliefs about mechanisms of treatment (e.g., talking to someone would help) and health concerns relative to medication were noted as reasons for individual preferences.42 In our analysis, we found that the preference of psychotherapy was stronger among women and younger participants, which may reflect the influence of social-contextual factors on preference (e.g., greater social acceptability of psychological treatment for women relative to men). Future research on the factors that contribute to patient preference is needed to better understand how patients derive these preferences.
In summary, the results of this meta-analytic review indicate that approximately 75% of participants prefer psychological to pharmacological treatment for depressive and anxiety disorders. This preference was observed independently across heterogeneous settings, capturing perspectives from treatment-seeking (both in primary and specialty care settings) as well as non-treatment-seeking samples. The association between patient preference and improved treatment retention and outcomes documented in other studies,7-9 and the importance of preference for guiding treatment decisions when more than one effective treatment option is available, highlight the importance of preference for treatment decision making at both the individual and policy level.
Clinical Points.
Patient preference for the treatment of psychiatric disorders is a core component of evidence-based mental health care and has been shown to impact treatment retention and outcome.
Studies across diverse settings indicate that on average patients prefer psychological treatment to pharmacological treatment for depression and anxiety at a rate of 3 to 1.
Consideration of patient preference, along with treatment efficacy and clinical expertise, may be important to optimizing outcomes in clinical settings.
Disclosures and Acknowledgments
The authors are aware of no conflicts with the content of this manuscript, nonetheless Dr. Otto would like to report past (3 years) consultant and research support from Organon (Merck), and royalties received for use of the SIGH-A from Lilly.
Portions of effort on this publication were supported by an National Institutes of Health Institutional Clinical and Translational Science Award (5UL1RR026314-02; Drs. Whitton and Welge) and National Institute of Mental Health grant R25 MH084784 (Dr. Otto). The NIH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
The other authors have no conflicts to report.
References
- 1.American Psychological Association . APA Presidential Task Force on Evidence-based Practice. American Psychological Association; Washington, DC: 2006. [Google Scholar]
- 2.American Psychiatric Association . American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorder Compendium. American Psychiatric Association; Arlington, VA: 2006. [Google Scholar]
- 3.Barlow DH, Gorman JM, Shear MK, et al. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA. 2000;283(19):2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- 4.Butler AC, Chapman JE, Forman EM, et al. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26(1):17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Dimidjian S, Hollon SD, Dobson KS, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consult Clin Psychol. 2006;74(4):658–70. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- 6.Roshanaei-Moghaddam B, Pauly MC, Atkins DC, et al. Relative effects of CBT and pharmacotherapy in depression versus anxiety: is medication somewhat better for depression, and CBT somewhat better for anxiety? Depress Anxiety. 2011;28(7):560–7. doi: 10.1002/da.20829. [DOI] [PubMed] [Google Scholar]
- 7.Mergl R, Henkel V, Allgaier AK, et al. Are treatment preferences relevant in response to serotonergic antidepressants and cognitive-behavioral therapy in depressed primary care patients? Results from a randomized controlled trial including a patients’ choice arm. Psychother Psychosom. 2011;80(1):39–47. doi: 10.1159/000318772. [DOI] [PubMed] [Google Scholar]
- 8.Prefence Collaborative Review Group Patients’ preferences within randomised trials: systematic review and patient level meta-analysis. BMJ. 2008;337:a1864. doi: 10.1136/bmj.a1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swift JK, Callahan JL, Collmer BM. Preferences. J Clin Psychol. 2011;67(2):155–62. doi: 10.1002/jclp.20759. [DOI] [PubMed] [Google Scholar]
- 10.Dwight-Johnson M, Lagomasino IT, Hay J, et al. Effectiveness of collaborative care in addressing depression treatment preferences among low-income Latinos. Psychiatr Serv. 2010;61(11):1112–8. doi: 10.1176/ps.2010.61.11.1112. [DOI] [PubMed] [Google Scholar]
- 11.Mojtabai R, Olfson M, Sampson NA, et al. Barriers to mental health treatment: Results from the National Comorbidity Survey Replication. Psychol Med. 2011;41(8):1751–61. doi: 10.1017/S0033291710002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 13.Chandra A, Scott MM, Jaycox LH, et al. Racial/ethnic differences in teen and parent perspectives toward depression treatment. J Adolesc Health. 2009;44(6):546–553. doi: 10.1016/j.jadohealth.2008.10.137. [DOI] [PubMed] [Google Scholar]
- 14.Lau J, Ioannidis JP, Terrin N, et al. The case of the misleading funnel plot. BMJ. 2006 Sep 16;333(7568):597–600. doi: 10.1136/bmj.333.7568.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Driessen E, Cuijpers P, Hollon SD, et al. Does pretreatment severity moderate the efficacy of psychological treatment of adult outpatient depression? A meta-analysis. J Consult Clin Psychol. 2010;78(5):668–680. doi: 10.1037/a0020570. [DOI] [PubMed] [Google Scholar]
- 16.Eddy KT, Dutra L, Bradley R, et al. A multidimensional meta-analysis of psychotherapy and pharmacotherapy for obsessive-compulsive disorder. Clin Psychol Rev. 2004;24(8):1011–1030. doi: 10.1016/j.cpr.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 17.Goncalves DC, Byrne GJ. Interventions for generalized anxiety disorder in older adults: Systematic review and meta-analysis. J Anxiety Disord. 2012;26(1):1–11. doi: 10.1016/j.janxdis.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 18.Mitte K. A meta-analysis of the efficacy of psycho- and pharmacotherapy in panic disorder with and without agoraphobia. J Affect Disord. 2005;88(1):27–45. doi: 10.1016/j.jad.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Spielmans GI, Berman MI, Usitalo AN. Psychotherapy versus second-generation antidepressants in the treatment of depression: a meta-analysis. J Nerv Ment Dis. 2011;199(3):142–149. doi: 10.1097/NMD.0b013e31820caefb. [DOI] [PubMed] [Google Scholar]
- 20.Cherry DK, Woodwell DA, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2005 summary. Advance data from vital and health statistics. No. 387. National Center for Health Statistics; Hyattsville, MD: 2007. [PubMed] [Google Scholar]
- 21.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–856. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- 22.Byford S, Barrett B, Roberts C, et al. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive behavioural therapy in adolescents with major depression. Br J Psychiatry. 2007;191:521–527. doi: 10.1192/bjp.bp.107.038984. [DOI] [PubMed] [Google Scholar]
- 23.Heuzenroeder L, Donnelly M, Haby MM, et al. Cost-effectiveness of psychological and pharmacological interventions for generalized anxiety disorder and panic disorder. Aust N Z J Psychiatry. 2004;38(8):602–612. doi: 10.1080/j.1440-1614.2004.01423.x. [DOI] [PubMed] [Google Scholar]
- 24.McHugh RK, Otto MW, Barlow DH, et al. Cost-efficacy of individual and combined treatments for panic disorder. J Clin Psychiatry. 2007;68(7):1038–1044. doi: 10.4088/jcp.v68n0710. [DOI] [PubMed] [Google Scholar]
- 25.Beland SG, Tournier M, Galbaud du Fort G, et al. Economic impact of nonpersistence with antidepressant treatment in the adult population of Quebec: a comparative cost-effectiveness approach. Value Health. 2011;14(4):492–498. doi: 10.1016/j.jval.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 26.Goethe JW, Woolley SB, Cardoni AA, et al. Selective serotonin reuptake inhibitor discontinuation: side effects and other factors that influence medication adherence. J Clin Psychopharmacol. 2007 Oct;27(5):451–8. doi: 10.1097/jcp.0b013e31815152a5. [DOI] [PubMed] [Google Scholar]
- 27.Bambauer KZ, Soumerai SB, Adams AS, et al. Provider and patient characteristics associated with antidepressant nonadherence: the impact of provider specialty. J Clin Psychiatry. 68(6):867–73. doi: 10.4088/jcp.v68n0607. 200. [DOI] [PubMed] [Google Scholar]
- 28.McHugh RK, Barlow DH. The dissemination and implementation of evidence-based psychological treatments. A review of current efforts. Am Psychol. 2010;65(2):73–84. doi: 10.1037/a0018121. [DOI] [PubMed] [Google Scholar]
- 29.Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to resuce the burden of mental illness. Perspectives on Psychological Science. 2011;6(1):21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- 30.Fernandez Y, Garcia E, Franks P, et al. Depression treatment preferences of Hispanic individuals: exploring the influence of ethnicity, language, and explanatory models. J Am Board Fam Med. 2011;24(1):39–50. doi: 10.3122/jabfm.2011.01.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kocsis JH, Leon AC, Markowitz JC, et al. Patient preference as a moderator of outcome for chronic forms of major depressive disorder treated with nefazodone, cognitive behavioral analysis system of psychotherapy, or their combination. J Clin Psychiatry. 2009;70(3):354–361. doi: 10.4088/jcp.08m04371. [DOI] [PubMed] [Google Scholar]
- 32.Backenstrass M, Joest K, Frank A, et al. Preferences for treatment in primary care: a comparison of nondepressive, subsyndromal and major depressive patients. Gen Hosp Psychiatry. 2006;28(2):178–180. doi: 10.1016/j.genhosppsych.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 33.Hodges L, Butcher I, Kleiboer A, et al. Patient and general practitioner preferences for the treatment of depression in patients with cancer: how, who, and where? J Psychosom Res. 2009;67(5):399–402. doi: 10.1016/j.jpsychores.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 34.Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342(20):1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- 35.Safren SA, Sprich S, Mimiaga MJ, et al. Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. JAMA. 2010;304(8):875–880. doi: 10.1001/jama.2010.1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Otto MW, Smits JAJ, Reese HE. Combined psychotherapy and pharmacotherapy for mood and anxiety disorders in adults: Review and analysis. Clin Psychology Sci Pract. 2005;12:72–86. [Google Scholar]
- 37.Otto MW, McHugh RK, Kantak KM. Combined pharmacotherapy and cognitive-behavioral therapy for anxiety disorders: Medication effects, glucocorticoids, and attenuated outcomes. Clin Psychology Sci Pract. 2010;17:91–103. doi: 10.1111/j.1468-2850.2010.01198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alegría M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Services. 2008;59(11):1264–72. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davis RG, Ressler KJ, Schwartz AC, et al. Treatment barriers for low-income, urban African Americans with undiagnosed posttraumatic stress disorder. J Trauma Stress. 2008;21(2):218–22. doi: 10.1002/jts.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cooper LA, Gonzales JJ, Gallo JT, et al. The acceptability of treatment for depression and African-American, Hispanic, and White primary care patients. Med Care. 2003;41(4):479–89. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 41.Givens JL, Houston TK, Van Voorhees BW, et al. Ethnicity and preferences for depression treatment. Gen Hosp Psychiatry. 2007;29(3):182–191. doi: 10.1016/j.genhosppsych.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 42.Angelo FN, Miller HE, Zoellner LA, et al. “I need to talk about it”: a qualitative analysis of trauma-exposed women’s reasons for treatment choice. Behav Ther. 2008;39(1):13–21. doi: 10.1016/j.beth.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Becker CB, Meyer G, Price JS, et al. Law enforcement preferences for PTSD treatment and crisis management alternatives. Behav Res Ther. 2009;47(3):245–253. doi: 10.1016/j.brat.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 44.Becker CB, Darius E, Schaumberg K. An analog study of patient preferences for exposure versus alternative treatments for posttraumatic stress disorder. Behav Res Ther. 2007;45(12):2861–2873. doi: 10.1016/j.brat.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 45.Brody AL, Saxena S, Stoessel P, et al. Regional brain metabolic changes in patients with major depression treated with either paroxetine or interpersonal therapy: preliminary findings. Arch Gen Psychiatry. 2001;58(7):631–640. doi: 10.1001/archpsyc.58.7.631. [DOI] [PubMed] [Google Scholar]
- 46.Chilvers C, Dewey M, Fielding K, et al. Counselling versus Antidepressants in Primary Care Study Group Antidepressant drugs and generic counselling for treatment of major depression in primary care: randomised trial with patient preference arms. BMJ. 2001;322(7289):772–775. doi: 10.1136/bmj.322.7289.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Churchill R, Khaira M, Gretton V, et al. Nottingham Counselling and Antidepressants in Primary Care (CAPC) Study Group Treating depression in general practice: factors affecting patients’ treatment preferences. Br J Gen Pract. 2000;50(460):905–906. [PMC free article] [PubMed] [Google Scholar]
- 48.Davidson KW, Rieckmann N, Clemow L, et al. Enhanced depression care for patients with acute coronary syndrome and persistent depressive symptoms: coronary psychosocial evaluation studies randomized controlled trial. Arch Intern Med. 2010;170(7):600–608. doi: 10.1001/archinternmed.2010.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deacon BJ, Abramowitz JS. Patients’ perceptions of pharmacological and cognitive-behavioral treatments for anxitey disorders. Behav Ther. 2005;36(2):139–145. doi: 10.1016/j.brat.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 50.Dobscha SK, Corson K, Gerrity MS. Depression treatment preferences of VA primary care patients. Psychosomatics. 2007;48(6):482–488. doi: 10.1176/appi.psy.48.6.482. [DOI] [PubMed] [Google Scholar]
- 51.Dwight-Johnson M, Sherbourne CD, Liao D, et al. Treatment preferences among depressed primary care patients. J Gen Intern Med. 2000;15(8):527–534. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fann JR, Jones AL, Dikmen SS, et al. Depression treatment preferences after traumatic brain injury. J Head Trauma Rehabil. 2009;24(4):272–278. doi: 10.1097/HTR.0b013e3181a66342. [DOI] [PubMed] [Google Scholar]
- 53.Feeny NC, Zoellner LA, Mavissakalian MR, et al. What would you choose? Sertraline or prolonged exposure in community and PTSD treatment seeking women. Depress Anxiety. 2009;26(8):724–731. doi: 10.1002/da.20588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Feeny NC, Zoellner LA, Kahana SY. Providing a treatment rationale for PTSD: Does what we say matter? Behav Res Ther. 2009 Sep;47(9):752–760. doi: 10.1016/j.brat.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. 2009;36(1):60–69. doi: 10.1111/j.1523-536X.2008.00296.x. [DOI] [PubMed] [Google Scholar]
- 56.Iacoviello BM, McCarthy KS, Barrett MS, et al. Treatment preferences affect the therapeutic alliance: implications for randomized controlled trials. J Consult Clin Psychol. 2007;75(1):194–198. doi: 10.1037/0022-006X.75.1.194. [DOI] [PubMed] [Google Scholar]
- 57.Jaycox LH, Asarnow JR, Sherbourne CD, et al. Adolescent primary care patients’ preferences for depression treatment. Adm Policy Ment Health. 2006;33(2):198–207. doi: 10.1007/s10488-006-0033-7. [DOI] [PubMed] [Google Scholar]
- 58.Kwan BM, Dimidjian S, Rizvi SL. Treatment preference, engagement, and clinical improvement in pharmacotherapy versus psychotherapy for depression. Behav Res Ther. 2010;48(8):799–804. doi: 10.1016/j.brat.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leykin Y, Derubeis RJ, Gallop R, et al. The relation of patients’ treatment preferences to outcome in a randomized clinical trial. Behav Ther. 2007;38(3):209–217. doi: 10.1016/j.beth.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 60.Lin P, Campbell DG, Chaney EF, et al. The influence of patient preference on depression treatment in primary care. Ann Behav Med. 2005;30(2):164–173. doi: 10.1207/s15324796abm3002_9. [DOI] [PubMed] [Google Scholar]
- 61.Ogrodniczuk JS, Piper WE, Joyce AS, et al. Alexithymia and treatment preferences among psychiatric outpatients. Psychother Psychosom. 2009;78(6):383–384. doi: 10.1159/000235981. [DOI] [PubMed] [Google Scholar]
- 62.Patel SR, Simpson HB. Patient preferences for obsessive-compulsive disorder treatment. J Clin Psychiatry. 2010;71(11):1434–1439. doi: 10.4088/JCP.09m05537blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Raue PJ, Schulberg HC, Heo M, et al. Patients’ depression treatment preferences and initiation, adherence, and outcome: a randomized primary care study. Psychiatr Serv. 2009;60(3):337–343. doi: 10.1176/appi.ps.60.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Unützer J, Katon W, Callahan CM, et al. Depression treatment in a sample of 1,801 depressed older adults in primary care. J Am Geriatr Soc. 2003;51(4):505–514. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- 65.Van HL, Dekker J, Koelen J, et al. Patient preference compared with random allocation in short-term psychodynamic supportive psychotherapy with indicated addition of pharmacotherapy for depression. Psychother Res. 2009;19(2):205–212. doi: 10.1080/10503300802702097. [DOI] [PubMed] [Google Scholar]
- 66.Walker J, Vincent N, Furer P, et al. Treatment preference in hypochondriasis. J Behav Ther Exp Psychiatry. 1999;30(4):251–258. doi: 10.1016/s0005-7916(99)00027-0. [DOI] [PubMed] [Google Scholar]
- 67.Zafar AM, Jawaid A, Ashraf H, et al. Psychotherapy as a treatment modality for psychiatric disorders: Perceptions of general public of Karachi, Pakistan. BMC Psychiatry. 2009;9:37. doi: 10.1186/1471-244X-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zoellner LA, Feeny NC, Cochran B, et al. Treatment choice for PTSD. Behav Res Ther. 2003;41(8):879–886. doi: 10.1016/s0005-7967(02)00100-6. [DOI] [PubMed] [Google Scholar]