Abstract
Objectives
Reports on the challenges and lessons learned from the Pacific Island American Health Study engagement with community-based organizations (CBOs) and faith-based organizations (FBOs) in Pacific Islander (PI) communities and mechanisms to facilitate the collection of robust data.
Methods
Academic–community partnership building was achieved with PI CBOs and FBOs. Focus group meetings were organized to plan various aspects of the study, develop questionnaire themes and protocols for survey, assist with the interviewer recruitment process, and strategize data dissemination plan.
Lessons Learned
The PIA-HS represents a model for overcoming challenges in data collection among small understudied populations. FBOs represent a valuable resource for community-based participatory research (CBPR) data collection and for effective interventions.
Conclusion
The study methodology can be replicated for other racial/ethnic groups with high levels of religiosity combined with concentrated levels of residential clustering. Expansion of the Pacific Islander American Health Study (PIA-HS) to include other PI subgroups is encouraged.
Keywords: Community-based participatory research, community health partnerships data collection health care evaluation mechanisms health care quality, access, evaluation, vulnerable populations, Pacific Islands, Samoan American, Tongan American
CBPR is a collaborative approach “intended to bring together researchers and communities to establish trust, share power, foster co-learning, enhance strengths and resources, build capacity, and examine and address community-identified needs and health problems.”1 The aim of CBPR is “to increase knowledge and understanding … and integrate the knowledge gained with interventions and policy and social change to improve the health and quality of life of community members2,3 Among hard-to-reach and poorly understood populations not routinely captured in national-level studies, CBPR represents a very promising approach because it engages community partners as active participants in the research process, sharing in decision making and ownership of project outcomes. Participatory research is especially appropriate for PI communities, because their small population size makes them difficult to capture in population-based surveys. Because we currently lack robust epidemiological information on PIs and subgroups, it is almost impossible to develop meaningful policies and interventions to improve the health and well-being of Pacific Peoples.4-6 Furthermore, there is a legacy of “parachute consultants” or “mosquito scientists” conducting research and collecting data in PI communities without the open sharing of knowledge, as well as inequitable perceptions of ownership in all research phases7 The balance between evidence-based research and action often fails to provide tangible benefits for PI communities. Participatory research addresses these inequalities by enforcing a model of shared ownership of resources. The PIA-HS was developed specifically to overcome these barriers and be responsive to recommendations for improved data by PI stakeholders.8
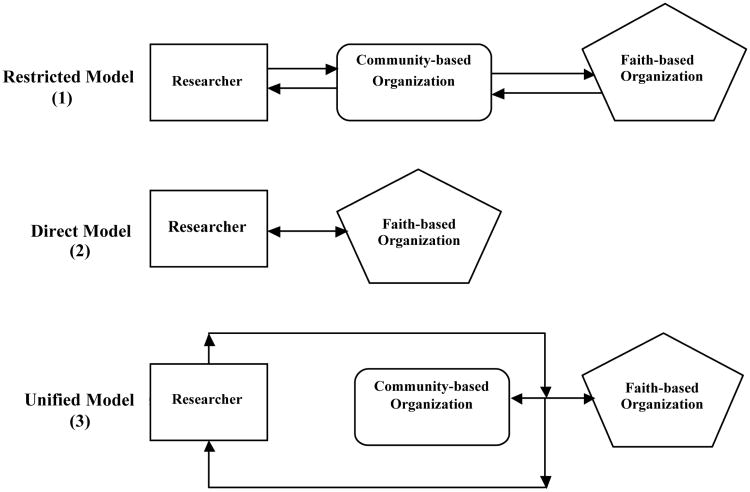
Building on the strengths and resources of researchers at the University of Michigan's (UM) Institute for Social Research and PI community-based and faith-based community leaders in California, this paper discusses the viability of three CBPR models—(1) restricted model, (2) direct model and (3) unified model—highlighting the utility of these models for doing research in PI communities. We also report on the challenges and lessons learned from the PIA-HS, with special focus on the distinct roles of CBOs and FBOs in PI communities, and the utility that the partnership offers in facilitating the collection of robust data.
Background
Over the past decades, the PI population has steadily grown in the United States through the increase of migrants from the U.S.-Associated Pacific Islands, and immigrants from independent Pacific Island countries. Together PIs comprise over 20 distinct ethnicities, cultures, languages, and histories.9,10 Traditionally, PIs have been aggregated with Asians to form the broad Asian PI (API) category. In 1997, the Office of Management and Budget revised the federal classification on race and ethnicity, disaggregating APIs into Asian Americans and Native Hawaiian and Other PIs 11,12 Despite this revision, robust data on PI populations continue to remain sparse. The PIA-HS was designed to ultimately provide representative data on all PI populations. The initial 2-year project began in June 2009 after several presentations and discussions between UM researchers and PI stakeholders and policy leaders at the Asian Pacific Islander American Health Forum Health Summit in 2006, NHPI Town Hall Meeting, Health Brain Trust, and HHS Advisory Committee on Minority Health convening in Washington, DC, in 2007. The overarching concern was the need for robust baseline health information and whether it is feasible to collect representative survey data on PI Americans using innovative sampling approaches.
Los Angeles and San Mateo Counties were identified for the initial phase of the study because of their high concentration of Samoan and Tongan communities and geographical variation between southern and northern parts of California. PIs tend to reside in tightly clustered communities with families deeply embedded in local faith-based groups. As former migrants and immigrants from the Pacific where a person's loyalty and membership is linked to the “village community” upon entry to the United States, places of worship such as faith-based communities routinely become the social substitutes for the social network of the village. FBOs also provide valuable resources, information, and services needed by new migrants and immigrants to negotiate state and local regulatory systems. Researchers based at the UM and Harvard University worked collaboratively to develop the questionnaire and sample design for the survey. Select questions from established survey instruments—National Health Interview Survey, California Health Interview Survey, National Survey on American Lives, and the Chicago Community Adult Health Study—were identified to provide comparable baseline health information. The measures included anthropomorphic indicators, health condition and health behavior, disability, women's and men's health, mental health and psychosocial factors, health insurance, healthcare utilization and access, adolescent health, and key components of core health beliefs and health-seeking behaviors and strategies.
A random sample of Samoan and Tongan households was derived from FBOs located in the study areas. The study populations represent two distinct PI populations who share similar cultures and demographic profiles, and are likewise chronically understudied and underserved. Each household from the stratified roster was screened and a randomly selected adult (≥18 years) and adolescent (13–17) was administered an age-appropriate questionnaire in English by Samoan and Tongan bilingual college-educated community members. All interviewers were required to successfully complete a 2-day interviewer training program administered by the Institute for Social Research and the UM Program for Education and Evaluation in Responsible Research and Scholarship. The time to complete the questionnaires varied between adults (1 hour) and adolescents (30 minutes). The study received human subject's protection approval from UM's Internal Review Board, as well as a Certificate of Confidentiality from the National Institutes of Health. When data entry is complete, the research team will collaborate with community leaders to develop strategies for the analysis, interpretation, and dissemination of survey results.
Engaging Community Members
Figure 1 presents three models for CBPR in PI communities. The restricted model represents a CBPR approach wherein the researcher operates through the CBO to gain access to the community and FBO leaders. This model is useful when the researcher is an outsider and not a member of the community. The CBO, a nonprofit organization whose mission and role within the community matches the goals of the research will serve as both a gateway and a gatekeeper, hopefully facilitating research access when it benefits a community and discouraging it when it does not. The direct model represents a CBPR approach where the researcher works directly with the FBO owing to the lack of an appropriate CBO to provide entry into the community as well as direct access to the local FBO. This approach is particularly efficient if the researcher is able to engage the FBO leaders and researched community directly. Because faith-based leaders and elders of the community are highly revered in PI culture, obtaining direct contact and the approval of faith-based leaders and community elders represents the highest endorsement to conduct research in PI communities. The unified model represents a CBPR approach where the researcher works with both the CBO and the FBO simultaneously, with the CBO acting as an equal partner with the FBO, rather than as a gatekeeper controlling access to the FBO. The unified model is seen as an approach that maximizes the combined strengths and resources that CBOs and FBOs can bring to the research project. Our work also suggests that there can often be clear differences in the level of FBO engagement and experience in evidence-based research, which in turn impacts their ability to participate in the research experience and to ensure benefits to their community. Samoan FBOs seemed to have more experience and familiarity with community-based research compared with that seen among the Tongan FBOs. Similarly, the number and focus of CBO's varied widely across the primary sampling units, with a particularly limited number of active CBO's associated with the Samoan sample population to choose from. Because of these differences in experience, the PIA-HS chose to employ the direct model for the Samoan and Tongan sample and the unified model for the Tongan sample. Initially, the investigators experimented with the restricted model approach in the Samoan case, collaborating with a Samoan CBO to pretest interviewer training and questionnaire readability. Shared concerns with the CBO over the research protocol, data quality checks, and handling of incentives ultimately made them ineligible to perform the actual interviews. Still, the process proved to be a valuable learning experience, allowing us to improve and refine our interviewer training to meet the needs of less experienced Samoan interviewers. Similarly, we constantly refined our approach for engaging the community through the direct and ongoing engagement of FBO leaders by the study's principle investigator. Because of their high-ranking status within the community and immediate responsibilities to church members, they could and did offer invaluable guidance and important advocates for the study when meeting with their congregations and communities. Additionally, focus group meetings with FBO elders were conducted with each participating community to discuss the study and receive approval to access their church rosters for the sample design. Community partners reviewed and provided feedback on the questionnaire and supporting materials, as well as helping to recruit interviewers.
Figure 1.
CBPR models applied in PI communities.
Pacific Islander Community-Based and Faith-Based Organizations
CBOs and FBOs within PI communities are unique and address different goals. Table 1 highlights some of the unique characteristics between organizations. The majority of PI CBOs are organized around the needs of a particular ethnic group. The same holds true for FBOs, some explicitly with ethnicity-based congregations and others implicitly because of the composition of the neighborhood. CBOs are typically defined by their specific mission such as health, education, and cultural preservation, and their work is often limited to the local area. This allows them to address critical needs, but the total number of CBOs found within PI populations remains small, narrowing their impact across communities. CBOs often act as an entry point for researchers, offering a means to interact with PI stakeholders, and working with the researcher to approach the FBOs to gain broad access and acceptance within PI communities. In contrast, FBOs saturate PI communities, each FBO belonging to a specific neighborhood or representing multiple faith groups within the neighborhood. FBOs also maintain relationships with other FBOs through the formal Church Connection or Conference, as well as through informal networks that connect churches serving other congregations. The very purpose and cultural construction of the PI FBO requires it to exist in areas of high PI concentrations who share similar needs, expectations, and interpretations of doctrine. This special role of faith provision and cultural reinforcement provides them direct access to community members but, more important, a respected role of influence over community decisions.
Table 1. Comparison of PI CBOs and FBOs in California.
| Characteristics | PI CBOs | PI FBOs |
|---|---|---|
| Status | Nonprofit organization | Nonprofit organization |
| Mission | Defined by specific function(s) such as health, education or policy targeting the local community | Generally all encompassing of issues relevant to the congregation in the local community as well as out-of-state and global communities |
| Relationship | Independent | Member of the Connectional (e.g., Conference of United Methodist Churches, Conference of Congregational Churches, as well as Catholic and Mormon Churches) |
| Membership | None | PI households, families and individuals; congregation sizes can vary from very small (e.g., <20 households to very large (e.g., >100 households). |
| Ethnic based | Majority of the CBOs are organized around a specific ethnic group (e.g., Guam Communications Network, Office of Samoan Affairs, Samoan National Nurses Association, Samoan Solutions, Taulama for Tongans and Tongan Social Services; only a small number outreach to all Native Hawaiian and Pacific groups (e.g., The Pacific Islander Health Partnership and Native Hawaiian and Pacific Islander Alliance) | Majority of the PI congregations are organized by ethnicity and belong to a larger church connection (e.g., The United Methodists, London Missionary Society, Congregationalists, Assembly of God, and Seventh-Day Adventists) with the exception of those who a part of a mixed congregation (e.g.; Catholics and Mormons); only a very small number of congregations operate independently (e.g., Siasi Uesiliana Tau'ataina ‘o Amelika) |
| Number of PI organizations/congregations in California | Fewer than 15 organizations are devoted to health. This total does not include API health organizations | Estimate >300 PI church congregations |
| Funding sources | External through grants, donations and fund-raising activities | Church membership contributions, Church Connection, fund-raising activities, and external grants and donations |
Challenges Encountered and Lessons Learned
Past experiences have often left PI communities distrustful of outside researchers and labels such as “helicopter researcher” or “mosquito researcher” reflect their feeling that researchers collect data from the community, but then leave after providing little or no benefit for the community's effort. As part of discussions with community members, specific issues were identified that made them less likely to be part of external research designs. Core concerns included “participant burden,” researchers assuming ownership of the data and not sharing with the community, failure to present results to community stakeholders, not engaging the community to better understand results, and the inadequate investment in capacity building. Taking this information to heart, the PIA-HS carefully invested the time needed to build trust. Initially, the PIA-HS fielded several focus group meetings with each of the community leadership groups to identify core concerns and establish a partnership between the community and the study. The principal investigator travelled to California repeatedly to meet with community members, conduct interviewer training, and supervise fieldwork; between trips, communication was conducted via telephone meetings and group emails. The recruitment of PI interviewers took considerable planning and time investment because of our need to identify potential interviewers who not only had the required language skills and ethnic background, but who were also unlikely to personally know respondents eligible for the survey within specific neighborhoods. Ensuring that interviewer and respondent were unlikely to know each other was seen as an essential step in providing our respondent with the level of confidentiality promised in our informed consent. Having PI interviewers was essential because they brought in the cultural competencies needed to encourage accurate responses to the questionnaire. Conversely, the insular nature of PI communities also required additional vigilance in the selection of neutral interviewers to minimize bias in the collection of information.
Discussion
The PIA-HS represents a useful model for overcoming challenges in the collection of robust data for small understudied populations. In PI communities, FBOs represent the “village” and play a central role in the lives of PIs. Similarly, in PI cultures the FBO leader is highly revered and is a “trusted voice” within the community. There are far more PI FBOs in the local community and comparatively fewer CBOs. Furthermore, the existence of FBOs requires formal PI membership and participation in FBO activities compared with CBOs that operate like a small business with no formal membership of community members. The study methodology can be replicated for other racial/ethnic groups that share high levels of religiosity combined with high levels of residential clustering.13-15 FBOs represent a valuable resource for offering services to eliminate health disparities; many FBOs offer ministries for the poor, and on health and well-being. In addition, FBO leaders represent the “trusted voices” within the community and their complex administrative connections to other church communities nationwide amplifies their impact and offers tremendous opportunities for engaging them in community action to eliminate health disparities.
Acknowledgments
This research was supported by the Asian Pacific Islander American Health Forum, W. K. Kellogg Foundation and the DHHS, Office of Minority Health. Additional support for this research was provided by a grant from the National Institute on Child and Human Development (Award #1-R21-HD-063074-01-A1).
References
- 1.Israel BA, Eng E, Schulz AJ, Parker EA. Introduction to methods in community-based participatory research for health. In: Israel BA, Eng E, Schultz AJ, Parker EA, editors. Methods in community-based participatory research for health. San Francisco: Jossey-Bass; 2005. [Google Scholar]
- 2.Israel BA, Shulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 3.Minkler M, Wallenstein N. Community based participatory research for health. San Francisco: Jossey-Bass; 2003. p. xxxiii. [Google Scholar]
- 4.Panapasa SV, Williams DR. National Leadership Summit on Eliminating Racial and Ethnic Disparities in Health. The Office of Minority Health; Washington (DC): Jan, 2006. Measuring US Pacific Islander health: Opportunities and challenges with existing data resources. [Google Scholar]
- 5.Srinivasan S, Guillermo T. Toward improved health: Disaggregating Asian American and Native Hawaiian/Pacific Islander Data. Am J Public Health. 2000;90:1731–4. doi: 10.2105/ajph.90.11.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moy E, Arispe IE, Holmes JS, Andrews RM. Preparing the National Healthcare Disparities Report: Gaps in data for accessing racial, ethnic, and socioeconomic disparities in health care. Med Care. 2004;43:I9–16. [PubMed] [Google Scholar]
- 7.Finau S, Finau E, Ofanoa M. Research imperialism in Pacific health: The case of Tonga (1966-1997) Pacific Health Dialog. 2000;7:109–14. [PubMed] [Google Scholar]
- 8.Asian & Pacific Islander American Health Forum. Health Brain Trust on data & research: A call to action—More data collection and reporting on Native Hawaiian and Pacific Islander Health to Eliminate Health Disparities [cited 2009] Available from: http://www.apiahf.org/sites/default/files/NHPI_Report12_2009.pdf.
- 9.Spickard PR, Fong R. Pacific Islander Americans and multi-ethnicity: A vision of America's future. Social Forces. 1995;73:1365–83. [Google Scholar]
- 10.Panapasa SV. Social, demographic, and cultural characteristics of Pacific Islanders. In: Trinh-Shevrin C, Rey MJ, editors. Health issues in the Asian American community. San Francisco: Jossey Bass; NYU School of Medicine Center for the Study of Asian American Health; 2009. pp. 50–72. [Google Scholar]
- 11.Fernandez EW. Comparison of selected social and economic characteristics between Asians, Hawaiians, Pacific Islanders and Asian Indians (Including Alaskan Natives) Washington (DC): Population Division, U.S. Bureau of the Census; 1996. [Google Scholar]
- 12.Office of Management and Budget. Revisions of the standards for the classification of federal data on race and ethnicity. Fed Reg. 1996;632:587–90. [Google Scholar]
- 13.Goldmon M, Roberson JT, Jr, Carey T, Godley P, Howard DL, Boyd C, et al. The Data collection/data distribution center: Building a sustainable African-American church-based research network. Prog Community Health Partnersh. 2008;2:205–24. doi: 10.1353/cpr.0.0023. [DOI] [PubMed] [Google Scholar]
- 14.Horowitz CR, Brenner BL, Lachapelle S, Amara DA, Arniella G. Effective recruitment of minority populations through community-led strategies. Am J Prev Med. 2009;37(6):1. doi: 10.1016/j.amepre.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ma GX, Toubbeh JI, Su X, Edwards RL. TECAR: An Asian American community-based participatory research model on tobacco and cancer control. Health Promot Pract. 2004;5:382–94. doi: 10.1177/1524839903260146. [DOI] [PubMed] [Google Scholar]