Abstract
Background
The aim of this study was to evaluate the effects of topical ropivacaine anesthesia on hemodynamic responses during intubation and extubation of hypertensive patients.
Material/Methods
One hundred fifty patients with hypertension ASA II–III were scheduled for noncardiac operations. Patients were divided into 3 groups: a control group receiving 5 ml saline, and 2 groups receiving topical anesthesia with 100 mg lidocaine or 37.5 mg ropivacaine. Hemodynamic responses, including blood pressure and heart rate (HR), were recorded at baseline (T0), before intubation (T1), during tracheal intubation (T2), 2 min after intubation (T3), upon eye opening on verbal commands (T4), during tracheal extubation (T5), and 2 min after extubation (T6). Patients were injected with urapidil 5 mg during intubation and extubation if their systolic blood pressure (SBP) was ≥160 mmHg or diastolic blood pressure (DBP) was ≥90 mmHg, and esmolol 10 mg when HR was ≥90 bpm.
Results
During extubation, the total dosages of urapidil and esmolol were significantly higher in the saline than in the lidocaine or ropivacaine groups, and were significantly lower in the ropivacaine than in the lidocaine group. At T2, SBP, SBP, MAP, and HR were lower in the lidocaine and ropivacaine groups than in the saline group, but the differences were not significant. From T4 to T6, SBP, DBP, MAP, and HR were significantly lower in the ropivacaine group than in the other 2 groups (P<0.05 each).
Conclusions
Topical lidocaine and ropivacaine anesthesia can effectively reduce hemodynamic responses during intubation, with ropivacaine better at inhibiting hemodynamic changes at emergence in hypertensive patients.
MeSH Keywords: Adolescent Medicine, Anesthesia, Anesthesia and Analgesia
Background
Both intubation and extubation can increase the concentration of catecholamine in the blood by stimulating the sympathetic nervous system, resulting in severe hemodynamic changes [1,2]. However, during intubation, agents such as opioids and propofol can effectively inhibit airway stimulation by endotracheal tubes. During extubation, the withdrawal of anesthetics and the emergence of patients from anesthesia stimulate the sympathetic nervous system, increasing the release of catecholamine and resulting in cough and hemodynamic responses [3–7], including hypertension and tachycardia. Although hemodynamic changes in laryngeal and tracheal tissues during this period are normally well tolerated by healthy individuals, they may be detrimental in hypertensive patients, leading to life-threatening complications such as myocardial ischemia, cardiac arrhythmias, and cerebrovascular hemorrhage [8–11].
The topical anesthetic lidocaine is widely used to inhibit intubation and extubation responses [13–17]. During long operations, however, preoperatively administered lidocaine will no longer be present at the time of extubation. Ropivacaine is a long-acting local anesthetic, and topical anesthesia with ropivacaine has been reported to significantly attenuate histamine-induced bronchospasm [22]. We hypothesized that topical ropivacaine anesthesia can inhibit hemodynamic responses during intubation and extubation in hypertensive patients. The aim of this prospective double-blinded study was to test this hypothesis.
Material and Methods
Study design and patients
This study was approved by the Ethics Committee of Harbin Medical University (HMUIRB20130011) and registered in the Chinese Clinical Trial Registry (ChiCTR-TRC-13003525). All patients provided written informed consent. We enrolled a total of 150 patients aged 20–60 years, ASA II–III, with hypertension according to World Health Organization criteria (systolic blood pressure (SBP) ≥160 mmHg or diastolic blood pressure (DBP) ≥90 mmHg) [23], undergoing noncardiac surgery.
The 150 patients were randomly assigned to receive saline (n=50), lidocaine (n=50), or ropivacaine (n=50) using a random number table. The assignments were recorded and sealed within envelopes, with the anesthesiologists blinded to assignments. Topical anesthesia was administered by one anesthesiologist, and hemodynamic changes were recorded by a second anesthesiologist. The drugs for topical anesthesia were prepared by a third anesthesiologist not blinded to randomization. Patients were excluded if they had ASA grade IV or higher; gastro-esophageal reflux; obesity (body mass index >30 kg/m2); anticipated difficulty maintaining airways on the face mask or more than 1 attempt at intubation; myocardial infarction within 6 months); heart function grade III or higher; or congestive cardiac failure. Patients with a cardiac pacemaker, congenital heart disease, or heart block on ECG were also excluded.
Anesthesia and treatment
All patients received their usual antihypertensive drugs but were not otherwise preoperatively medicated. After transfer to the operating room, blood pressure, heart rate (HR), electrocardiography (ECG), and saturation of blood oxygen (SpO2) were continuously monitored. The radial artery was cannulated with a 22-g catheter under local anesthesia (1% lidocaine 1 ml) to monitor real-time mean arterial pressure (MAP). All patients received 5 ml/kg−1 Ringer lactate solution over a 10-min period before induction of anesthesia. Patients were preoxygenated for 5 min, followed by intravenous injection of 1 mg penehyclidine hydrochloride. Anesthesia was induced with midazolam 0.5 mg/kg−1, fentanyl 4 μg/kg−1, rocuronium 0.6 mg/kg−1 and propofol 1.5 mg/kg−1. Two min after induction, the patients were topically anesthetized with saline (5 ml) 1%, 2% lidocaine (100 mg), or ropivacaine (37.5 mg) using a laryngotracheal topical anesthesia kit (Tuoren Group, Xinxiang, Henan, China). One-third of the total dose of local anesthetic was sprayed onto the larynx, the epiglottic area, and the trachea.
Four min after topical anesthesia, endotracheal intubation was performed by the first anesthesiologist. Patients who required more than 1 attempt to intubate were withdrawn from the study. Successful endotracheal intubation was confirmed by auscultation and end-tidal capnography. Anesthesia was maintained with remifentanil 10 μg/h−1/kg−1 and sevoflurane 1.5–2%. Tidal volume was controlled at 7 ml/kg−1, the respiratory rate was set at 12 per minute, and the expiration/inspiration ratio was set at 1:2. During surgery, ephedrine or atropine was injected if MAP or HR decreased by 30% from baseline. TOF was continuously monitored with TOF-Watch S (Organon, Dublin, Ireland). After surgery and the withdrawal of anesthetics, 0.05 mg/kg−1 of neostigmine and 0.3 mg of atropine were administered to reverse neuromuscular blockade. Extubation was performed when the TOF ratio (T4/T1) was >70%. During intubation and extubation, urapidil 5 mg was intravenously injected if SBP was ≥160 mmHg or diastolic blood pressure (DBP) was ≥90 mmHg, and 10 mg esmolol was intravenously injected if HR was ≥90 bpm. After confirmation of the absence of respiratory failure, hemorrhage, or hypertensive crisis, the patients were transferred to the ward.
Evaluation
The primary outcome measures were the dosages of urapidil and esmolol during emergence. Secondary outcomes included MAP and HR recorded by the second anesthesiologist at baseline (T0), at laryngoscopy before intubation (T1), at tracheal intubation (T2), 2 min after intubation (T3), upon eye opening in response to verbal commands (T4), at tracheal extubation (T5), and 2 min after extubation (T6).
The volume of bleeding and infusion were recorded. Five minutes after extubation, patients were transferred to the post-anesthesia care unit, and possible adverse events, including respiratory depression, hypoxemia, hypertension crisis, and nausea/vomiting, were evaluated.
Statistical analysis
Data were analyzed with SPSS 11.5 for Windows (Chicago, Illinois, USA). All data are expressed as mean (SD) or number (proportion,%). MAP and HR were analyzed using repeated measures analysis and compared at different time-points using the t-test. Categorical data were analyzed using the chi-square test or Fisher’s exact test, where appropriate. P values <0.05 were considered statistically significant.
A power analysis of number of patients who needed urapidil during extubation in a pilot study of 10 patients indicated that a sample size of 42 patients per group would reach approximately 80% power to reject the null hypothesis. To allow for lack of eligibility and attrition, 150 patients were enrolled in this study.
Results
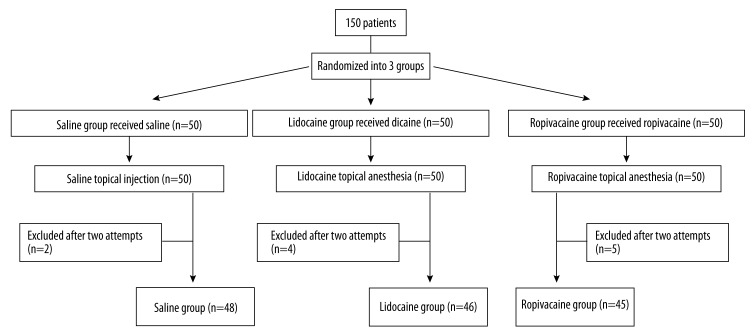
Of the 150 patients enrolled in this study, 11 (2 in the saline group, 4 in the lidocaine group, and 5 in the ropivacaine group) were excluded because they needed 2 attempts to intubate (Figure 1). There were no significant differences among the 3 groups in demographic data, duration of anesthesia and surgery, or volume of bleeding and infusion (P>0.05 each; Table 1). Moreover, there were no significant differences in preoperative dosages of antihypertensive drugs or perioperative ephedrine among the 3 groups (P>0.05; Table 2).
Figure 1.
CONSORT diagram of patient distribution.
Table 1.
Demographic data of the 2 groups.
| Saline group (n=48) | Lidocaine group (n=46) | Ropivacaine group (n=45) | P | |
|---|---|---|---|---|
| Sex (M) n (%) | 24.0 (50.0) | 26.0 (56.5) | 24.0 (53.3) | >0.05 |
| Age (year) | 60.3 (10.4) | 59.2 (10.8) | 61.4 (11.5) | >0.05 |
| Weight (kg) | 68.5 (7.4) | 67.2 (8.7) | 69.0 (5.8) | >0.05 |
| Duration of surgery (min) | 171.6 (19.1) | 169.0 (18.8) | 173.2 (18.5) | >0.05 |
| Duration of anesthesia (min) | 195.7 (22.1) | 196.3 (21.0) | 199.2 (21.8) | >0.05 |
| Volume of bleeding (ml) | 141.4 (27.5) | 133.9 (28.4) | 143.1 (26.7) | >0.05 |
| Volume of infusion (ml) | 659.8 (51.3) | 648.8 (49.1) | 665.2 (50.6) | >0.05 |
Table 2.
Antihypertensive medication in the 3 groups.
| Saline group (n=48) | Lidocaine group (n=46) | Ropivacaine group (n=45) | |
|---|---|---|---|
| Diuretic | 3 | 2 | 4 |
| Beta blocker | 4 | 5 | 3 |
| ACE inhibitor | 9 | 8 | 7 |
| Calcium channel blocker | 11 | 10 | 13 |
| Combination therapy | 21 | 21 | 18 |
The data are presented with number. There was no significant difference of use of antihypertensive medication in the 3 groups.
During emergence, 25 patients in saline group required urapidil to decrease blood pressure, with 5 patients each requiring 2 doses. In comparison, only 15 patients in the lidocaine group and only 7 in the ropivacaine group required urapidil to decrease blood pressure, with 4 and zero patients, respectively, requiring 2 doses. The total dosage of urapidil was significantly higher in the saline group (150 mg) than in either the lidocaine (95 mg) or ropivacaine (35 mg) group and was significantly higher in the lidocaine group than in the ropivacaine group (P<0.05 each; Table 3). Esmolol was required by 18 patients in the saline group, 12 in the lidocaine group, and 4 in the ropivacaine group. The total dosage of esmolol was significantly higher in the saline group than in either the lidocaine or ropivacaine group and was significantly higher in the lidocaine group than in the ropivacaine group (P<0.05 each; Table 3).
Table 3.
Comparison of dosage of urapidil and esmolol in the 3 groups.
| Saline group (n=48) | Lidocaine group (n=46) | Ropivacaine group (n=45) | |
|---|---|---|---|
| Urapidil (mg) | 195 | 95* | 35*,# |
| Esmolol (mg) | 180 | 120* | 40*,# |
P<0.05 compared with saline group.
P<0.05 compared with lidocaine group.
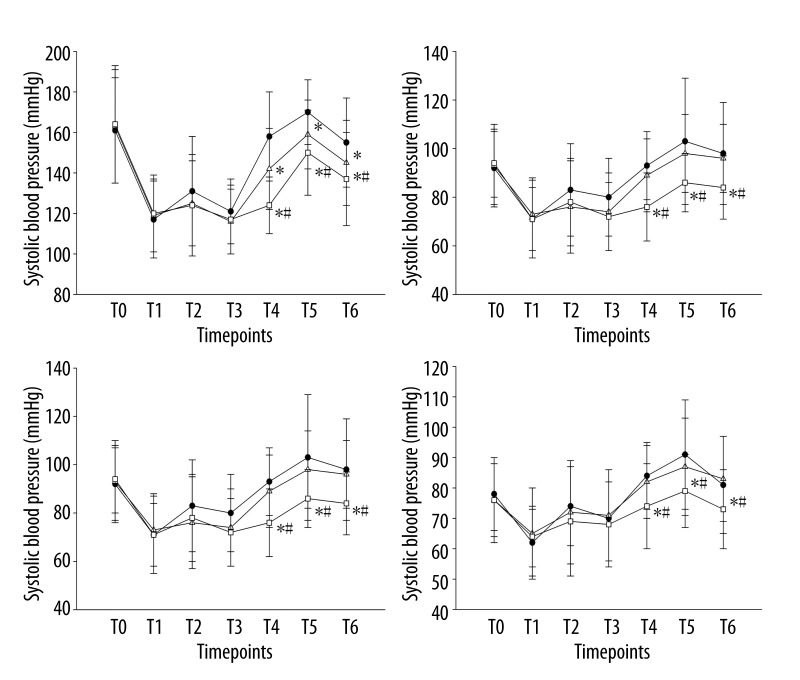
At T2, SBP, DBP, MAP, and HR were lower in the lidocaine and ropivacaine groups than in the saline group, but blood pressure and HR did not differ significantly between the lidocaine and ropivacaine groups. No patient required urapidil or esmolol during intubation. From T4 to T6, SBP, DBP, MAP, and HR were significantly higher in the saline group than in the lidocaine and ropivacaine groups and were significantly higher in the lidocaine than in the ropivacaine group (P<0.05 each) (Figure 2).
Figure 2.
Comparison of SBP, DBP, MAP, and HR in the 3 groups. The data are presented with mean ±SD. * P<0.05 compared with saline group. # P<0.05 compared with lidocaine group. There were no significant differences in SBP, DBP, MAP, and HR among the 3 groups from T0 to T3 (P>0.05 each). From T4 to T6, SBP, DBP, MAP, and HR were significantly lower in the lidocaine and ropivacaine groups than in the saline group (P<0.05 each) and were significantly lower in the ropivacaine group than in the lidocaine group (P<0.05 each).
Discussion
We found that both ropivacaine and lidocaine, when used for topical anesthesia before intubation, can inhibit hemodynamic responses during intubation. Compared with lidocaine, however, ropivacaine more effectively inhibited hemodynamic responses during extubation.
Insertion and withdrawal of a laryngoscope and endotracheal tube during intubation and extubation can irritate the sympathetic nervous system, leading to severe tachycardia, hypertension, or arrhythmia [26]. Although the hemodynamic changes induced by general anesthesia are transitory and not harmful for healthy individuals, in hypertensive patients they can lead to life-threatening complications, including myocardial ischemia and cardiac arrhythmias, and may even be fatal.
Opioids, α-blockers, β-blockers, and α2 agonists have been used to stabilize hemodynamic responses during intubation or extubation [36–38,43–50]. Care should be taken when using these agents, however, because of delays in postoperative awakening and the occurrence of complications associated with a decline in cardiac function. Lidocaine as an airway topical anesthetic is widely used to attenuate hemodynamic reflexes [3,17,18,25,27–31]. Godzieba et al. indicated that use high dose or high concentration of lidocaine (≤4 ampules) with epinephrine seems to be relatively safe for cardiovascularly compromised patients [51]. Due to its short half-life, however, lidocaine given prior to intubation cannot inhibit hemodynamic responses during extubation following a long operation. Moreover, endotracheal tube cuff lidocaine was not superior to intravenous lidocaine [19]. Laryngotracheal instillation of lidocaine for topical anesthesia during extubation may increase the risk of postoperative aspiration and costs to patients [16]. We therefore evaluated the effects of topical ropivacaine anesthesia on hemodynamic responses during intubation and extubation.
In this study, 13 patients underwent craniotomies for aneurysms. The stability of perioperative hemodynamics is very important for these hypertensive patients. An increase or decrease in blood pressure may cause bleeding or edema, or predispose the patient to cerebral ischemia. Tachycardia caused by irritation of sympathetic nervous system can result in increased oxygen consumption by the myocardium, and may even result in myocardial ischemia. To stabilize hemodynamics, intravenous urapidil and esmolol may be administered to decrease blood pressure and HR, respectively. However, administration of α- or β-blockers may lead to hypotension or bradycardia. In this study, we compared the dosages of urapidil and esmolol in 3 groups to determine whether topical ropivacaine could reduce the consumption of urapidil and esmolol, and stabilize hemodynamic changes.
We found that, compared with saline or lidocaine, topical ropivacaine significantly reduced the consumption of urapidil and esmolol during emergence from anesthesia and extubation by stabilizing hemodynamic responses. Ropivacaine significantly reduced SPB, DBP, MAP, and HR when compared with patients in the saline and lidocaine groups.
The effect of ropivacaine is due in large part to its blockade of sympathetic nerves distributed in the upper parts of the airway. Insertion of a laryngoscope and/or intake tube into the upper airways may directly produce pressure stimulation on laryngeal tissue. This causes marked cardiovascular responses by irritating the deep sensory receptors of the larynx. Topical anesthesia applied to the larynx or trachea is effective in suppressing intubation-induced increases in blood pressure [39,40], as well as blocking cardiovascular responses to airway irritation [41,42]. Topical ropivacaine was found to significantly attenuate the reactivity of the airways and to block the conduction of sympathetic nerves [22].
In conclusion, topical ropivacaine before intubation can effectively inhibit the intubation response, as well as decreasing the incidence and grade of cough and attenuating hemodynamic changes during the extubation period in hypertensive patients.
Conclusions
Topical ropivacaine before intubation can effectively inhibit the intubation response, as well as decreasing the incidence and grade of cough and attenuating hemodynamic changes during the extubation period in hypertensive patients.
Footnotes
Source of support: Departmental sources
References
- 1.Mazzone SB. An overview of the sensory receptors regulating cough. Cough. 2005;1:2. doi: 10.1186/1745-9974-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh S, Smith JE. Cardiovascular changes after the three stages of nasotracheal intubation. Br J Anaesth. 2003;91:667–71. doi: 10.1093/bja/aeg240. [DOI] [PubMed] [Google Scholar]
- 3.Minogue SC, Ralph J, Lampa MJ. Laryngotracheal topicalization with lidocaine before intubation decreases the incidence of coughing on emergence from general anesthesia. Anesth Analg. 2004;99:1253–57. doi: 10.1213/01.ANE.0000132779.27085.52. [DOI] [PubMed] [Google Scholar]
- 4.Estebe JP, Dollo G, Le Corre P, et al. Alkalinization of intracuff lidocaine improves endotracheal tube-induced emergence phenomena. Anesth Analg. 2002;94:227–30. doi: 10.1097/00000539-200201000-00044. [DOI] [PubMed] [Google Scholar]
- 5.Estebe JP, Delahaye S, Le Corre P, et al. Alkalinization of intracuff lidocaine and use of gel lubrication protect against tracheal tube-induced emergence phenomena. Br J Anaesth. 2004;92:361–66. doi: 10.1093/bja/aeh078. [DOI] [PubMed] [Google Scholar]
- 6.Estebe JP, Gentili M, Le Corre P, et al. Alkalinization of intracuff lidocaine: efficacy and safety. Anesth Analg. 2005;101:1536–41. doi: 10.1213/01.ANE.0000180995.24211.89. [DOI] [PubMed] [Google Scholar]
- 7.Tazeh-Kand NF, Eslami B, Mohammadian K. Inhaled fluticasone propionate reduces postoperative sore throat, cough, and hoarseness. Anesth Analg. 2010;111:895–98. doi: 10.1213/ANE.0b013e3181c8a5a2. [DOI] [PubMed] [Google Scholar]
- 8.Aouad MT, Al-Alami AA, Nasr VG, et al. The effect of low-dose remifentanil on responses to the endotracheal tube during emergence from general anesthesia. Anesth Analg. 2009;108:1157–60. doi: 10.1213/ane.0b013e31819b03d8. [DOI] [PubMed] [Google Scholar]
- 9.Irwin RS. Complications of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:54s–58s. doi: 10.1378/chest.129.1_suppl.54S. [DOI] [PubMed] [Google Scholar]
- 10.Saghaei M, Reisinejad A, Soltani H. Prophylactic versus therapeutic administration of intravenous lidocaine for suppression of post-extubation cough following cataract surgery: a randomized double blind placebo controlled clinical trial. Acta Anaesthesiol Taiwan. 2005;43:205–9. [PubMed] [Google Scholar]
- 11.Wetzel LE, Ancona AL, Cooper AS, et al. The effectiveness of 4% intracuff lidocaine in reducing coughing during emergence from general anesthesia in smokers undergoing procedures lasting less than 1.5 hours. AANA J. 2008;76:105–8. [PubMed] [Google Scholar]
- 12.Prys-Roberts C, Greene LT, Meloche R, Foex P. Studies of anaesthesia in relation to hypertension. II. Haemodynamic consequences of induction and endotracheal intubation. Br J Anaesth. 1971;43(6):531–47. doi: 10.1093/bja/43.6.531. [DOI] [PubMed] [Google Scholar]
- 13.Fujii Y, Saitoh Y, Takahashi S, Toyooka H. Combined diltiazem and lidocaine reduces cardiovascular responses to tracheal extubation and anesthesia emergence in hypertensive patients. Can J Anaesth. 1999;46:952–56. doi: 10.1007/BF03013130. [DOI] [PubMed] [Google Scholar]
- 14.Qi DY, Wang K, Zhang H, et al. The Efficacy of Intravenous Lidocaine versus Placebo on Attenuating Cardiovascular Response to Laryngoscopy and Tracheal Intubation: A Systematic Review of Randomized Controlled Trials. Minerva Anestesiol. 2013;79(12):1423–35. [PubMed] [Google Scholar]
- 15.Estebe JP, Dollo G, Le Corre P, et al. Alkalinization of intracuff lidocaine improves endotracheal tube-induced emergence phenomena. Anesth Analg. 2002;94:227–30. doi: 10.1097/00000539-200201000-00044. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez RM, Bjerke RJ, Drobycki T, et al. Prevention of endotracheal tube-induced coughing during emergence from general anesthesia. Anesth Analg. 1994;79:792–95. doi: 10.1213/00000539-199410000-00030. [DOI] [PubMed] [Google Scholar]
- 17.Denlinger JK, Ellison N, Ominsky AJ. Effects of Intratracheal Lidocaine on Circulatory Responses to Tracheal Intubation. Anesthesiology. 1974;41:409–12. doi: 10.1097/00000542-197410000-00024. [DOI] [PubMed] [Google Scholar]
- 18.Jee D, Park SY. Lidocaine Sprayed Down the Endotracheal Tube Attenuates the Airway-Circulatory Reflexes by Local Anesthesia During Emergence and Extubation. Anesth Analg. 2003;96:293–97. doi: 10.1097/00000539-200301000-00058. [DOI] [PubMed] [Google Scholar]
- 19.Behzadi M, Hajimohamadi F, Alagha AE, et al. Endotracheal tube cuff lidocaine is not superior to intravenous lidocaine in short pediatric surgeries. Int J Pediatr Otorhinolaryngol. 2010;74(5):486–88. doi: 10.1016/j.ijporl.2010.01.025. [DOI] [PubMed] [Google Scholar]
- 20.Stewart J, Kellett N, Castro D. The central nervous system and cardiovascular effects of levobupivacaine and ropivacaine in healthy volunteers. Anesth Analg. 2003;97:412–16. doi: 10.1213/01.ANE.0000069506.68137.F2. [DOI] [PubMed] [Google Scholar]
- 21.Zink W, Graf BM. The toxicity of local anesthetics: the place of ropivacaine and levobupivacaine. Curr Opin Anaesthesiol. 2008;21:645–50. doi: 10.1097/ACO.0b013e32830c214c. [DOI] [PubMed] [Google Scholar]
- 22.Groeben H, Grosswendt T, Silvanus MT, et al. Airway Anesthesia Alone Does Not Explain Attenuation of Histamine-induced Bronchospasm by Local Anesthetics. Anesthesiology. 2001;94:423–28. doi: 10.1097/00000542-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Denlinger JK, Ellison N, Ominsky AJ. World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens. 1999;17(2):151–83. [PubMed] [Google Scholar]
- 24.Pandey CK, Raza M, Ranjan R, et al. Intravenous Lidocaine Suppresses Fentanyl-Induced Coughing: A Double-Blind, Prospective, Randomized Placebo-Controlled Study. Anesth Analg. 2004;99(6):1696–98. doi: 10.1213/01.ANE.0000136967.82197.82. [DOI] [PubMed] [Google Scholar]
- 25.D’Aragon F, Beaudet N, Gagnon V, et al. The effects of lidocaine spray and intracuff alkalinized lidocaine on the occurrence of cough at extubation: a double-blind randomized controlled trial. Can J Anesth. 2013;60:370–76. doi: 10.1007/s12630-013-9896-8. [DOI] [PubMed] [Google Scholar]
- 26.Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59:295–99. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 27.Woodruff C, Wieczorek PM, Schricker T, et al. Atomised lidocaine for airway topical anaesthesia in the morbidly obese: 1% compared with 2% Anaesthesia. 2010;65(1):12–17. doi: 10.1111/j.1365-2044.2009.06126.x. [DOI] [PubMed] [Google Scholar]
- 28.Wieczorek PM, Schricker T, Vinet B, Backman SB. Airway topicalisation in morbidly obese patients using atomized lidocaine: 2% compared with 4% Anaesthesia. 2007;62:984–88. doi: 10.1111/j.1365-2044.2007.05179.x. [DOI] [PubMed] [Google Scholar]
- 29.Xue FS, Liu HP, He N, et al. Spray-as-you-go airway topical anesthesia in patients with a difficult airway: a randomized double-blind comparison of 2% and 4% lidocaine. Anesth Analg. 2009;108:536–43. doi: 10.1213/ane.0b013e31818f1665. [DOI] [PubMed] [Google Scholar]
- 30.Williams KA, Barker GL, Harwood RJ, Woodall NM. Combined nebulization and spray-as-you-go topical local anaesthesia of the airway. Br J Anaesth. 2005;95:549–53. doi: 10.1093/bja/aei202. [DOI] [PubMed] [Google Scholar]
- 31.Simmons ST, Schleich AR. Airway regional anesthesia for awake fibreoptic intubation. Reg Anesth Pain Med. 2002;27:180–92. doi: 10.1053/rapm.2002.30659. [DOI] [PubMed] [Google Scholar]
- 32.Wetzel LE, Ancona AL, Cooper AS, et al. The effectiveness of 4% intracuff lidocaine in reducing coughing during emergence from general anesthesia in smokers undergoing procedures lasting less than 1.5 hours. AANA J. 2008;76:105–8. [PubMed] [Google Scholar]
- 33.Aouad MT, Al-Alami AA, Nasr VG, et al. The effect of low-dose remifentanil on responses to the endotracheal tube during emergence from general anesthesia. Anesth Analg. 2009;108:1157–60. doi: 10.1213/ane.0b013e31819b03d8. [DOI] [PubMed] [Google Scholar]
- 34.Asai T, Koga K, Vaughan RS. Respiratory complications associated with tracheal intubation and extubation. Br J Anaesth. 1998;80:767–75. doi: 10.1093/bja/80.6.767. [DOI] [PubMed] [Google Scholar]
- 35.Adcock JJ, Douglas GJ, Garabette M, et al. RSD931, a novel anti-tussive agent acting on airway sensory nerves. Br J Pharmacol. 2003;138:407–16. doi: 10.1038/sj.bjp.0705056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pandazi AK, Louizos AA, Davilis DJ, et al. Inhalational anesthetic technique in microlaryngeal surgery: a comparison between sevoflurane-remifentanil and sevofluranealfentanil anesthesia. Ann Otol Rhinol Laryngol. 2003;112:373–78. doi: 10.1177/000348940311200414. [DOI] [PubMed] [Google Scholar]
- 37.Ayuso A, Luis M, Sala X, et al. Effects of anesthetic technique on the hemodynamic response to microlaryngeal surgery. Ann Otol Rhinol Laryngol. 1997;106:863–68. doi: 10.1177/000348949710601010. [DOI] [PubMed] [Google Scholar]
- 38.Matot I, Sichel JY, Yofe V, Gozal Y. The effect of clonidine premedication on hemodynamic responses to microlaryngoscopy and rigid bronchoscopy. Anesth Analg. 2000;91:828–33. doi: 10.1097/00000539-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Takita K, Morimoto Y, Kemmotsu O. Tracheal lidocaine attenuates the cardiovascular response to endotracheal intubation. Can J Anaesth. 2001;48:732–36. doi: 10.1007/BF03016686. [DOI] [PubMed] [Google Scholar]
- 40.Park YO, Bang KS, Choi EM, et al. Plasma Lidocaine Concentration and Hemodynamic Effect after 10% Lidocaine Spray on Laryngopharyngeal and Intratracheal Site during the Endotracheal Intubation. Korean J Anesthesiol. 2005;49:152–56. [Google Scholar]
- 41.Minogue SC, Ralph J, Lampa MJ. Laryngotracheal topicalization with lidocaine before intubation decreases the incidence of coughing on emergence from general anesthesia. Anesth Analg. 2004;99:1253–57. doi: 10.1213/01.ANE.0000132779.27085.52. [DOI] [PubMed] [Google Scholar]
- 42.Hamaya Y, Dohi S. Differences in cardiovascular response to airway stimulation at different sites and blockade of the responses by lidocaine. Anesthesiology. 2000;93:95–103. doi: 10.1097/00000542-200007000-00018. [DOI] [PubMed] [Google Scholar]
- 43.Hernandez-Palazon J, Tortosa Serrano JA, Garcia-Palenciano C, et al. Cardiovascular response to tracheal intubation in patients with intracranial tumor. Comparative study between urapidil and lidocaine. Rev Esp Anestesiol Reanim. 2000;47:146–50. [PubMed] [Google Scholar]
- 44.Cheng YC, Li Y, Xu CT, et al. Effects of propofol versus urapidil on perioperative hemodynamics and intraocular pressure during anesthesia and extubation in ophthalmic patients. Int J Ophthalmol. 2011;4:170–74. doi: 10.3980/j.issn.2222-3959.2011.02.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Santiveri X, Ledesma M, Delas F, et al. Comparison of lidocaine and urapidil for prevention of hemodynamic response to tracheal intubation in patients in general good health. Rev Esp Anestesiol Reanim. 1998;45:46–49. [PubMed] [Google Scholar]
- 46.Sharma S, Mitra S, Grover VK, Kalra R. Esmolol blunts the haemodynamic responses to tracheal intubation in treated hypertensive patients. Can J Anaesth. 1996;43:778–82. doi: 10.1007/BF03013028. [DOI] [PubMed] [Google Scholar]
- 47.Tan PH, Yang LC, Shih HC, et al. Combined use of esmolol and nicardipine to blunt the haemodynamic changes following laryngoscopy and tracheal intubation. Anaesthesia. 2002;57:1207–12. doi: 10.1046/j.1365-2044.2002.02624_4.x. [DOI] [PubMed] [Google Scholar]
- 48.Ugur B, Ogurlu M, Gezer E, et al. Effects of esmolol, lidocaine and fentanyl on haemodynamic responses to endotracheal intubation: a comparative study. Clin Drug Investig. 2007;27:269–77. doi: 10.2165/00044011-200727040-00006. [DOI] [PubMed] [Google Scholar]
- 49.Lim SH, Chin NM, Tai HY, et al. Prophylactic esmolol infusion for the control of cardiovascular responses to extubation after intracranial surgery. Ann Acad Med Singapore. 2000;29:447–51. [PubMed] [Google Scholar]
- 50.Kovac AL, Masiongale A. Comparison of nicardipine versus esmolol in attenuating the hemodynamic responses to anesthesia emergence and extubation. J Cardiothorac Vasc Anesth. 2007;21:45–50. doi: 10.1053/j.jvca.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 51.Godzieba A, Smektała T, Jędrzejewski M, Sporniak-Tutak K. Clinical assessment of the safe use local anaesthesia with vasoconstrictor agents in cardiovascular compromised patients: A systematic review. Med Sci Monit. 2014;20:393–98. doi: 10.12659/MSM.889984. [DOI] [PMC free article] [PubMed] [Google Scholar]