Abstract
Women who experience intimate partner violence (IPV) are at heightened risk for drug use problems. While prevailing models of drug use suggest that IPV-exposed women use drugs in an effort to escape or avoid negative affect, a dearth of literature has examined the role of avoidance coping in drug use problems within this population. Given recent suggestions that flexible, situationally-appropriate use of avoidance coping may be adaptive, particularly when confronted with highly stressful situations, we hypothesized that avoidance coping and drug use problems would demonstrate a curvilinear, U-shaped dose-response relationship. Participants were 147 community-recruited women experiencing IPV. Consistent with our hypothesis, moderate levels of avoidance coping were associated with lower levels of drug use problems, whereas high and low levels of avoidance coping were associated with higher levels of drug use problems. Findings highlight the complex relationship between avoidance coping and drug use problems and suggest that avoidance coping, when used in moderation, may be an adaptive strategy for coping with relational conflict among women who experience IPV.
Keywords: Intimate partner violence, drug use problems, avoidance coping, emotion regulation, dose-response
Intimate partner violence (IPV) is a highly prevalent public health problem (Garcia-Moreno, Jansen, Ellsberg, Heise, & Watts, 2006; Schafer, Caetano, & Clark, 1998) associated with a range of deleterious physical, psychological, economic, and societal costs (Brown, Finkelstein, & Mercy, 2008; Golding, 1999; Walby, 2009). One well-established correlate of IPV is drug use problems. Among IPV-exposed women, prevalence rates of drug abuse or dependence are 2–7 times higher than women nationally (Substance Abuse and Mental Health Services Administration, 2009), with 7%–44% of IPV-exposed women reporting drug problems severe enough to be diagnosed with drug abuse or dependence (Golding, 1999). Further, extant research provides support for a significant positive association between women's IPV victimization and their drug use problems (Brewer, Fleming, Haggerty, & Catalano, 1998; Cottler, Compton, Mager, Spitznagel, & Janca, 1992; El-Bassel, Gilbert, Schilling, & Wada, 2000; El-Bassel, Gilbert, Wu, Go, & Hill, 2005). Prevailing models of drug use, such as negative reinforcement (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004) and self-medication (Khantzian, 1997), suggest that drug use problems often develop as a consequence of IPV (Kilpatrick, Acierno, Resnick, Saunders, & Best, 1997; Testa & Livingston, 2000; Testa, Livingston, & Leonard, 2003) because drugs facilitate avoidance of arousal and anxiety related to IPV-victimization (Stewart, 1996; Stewart, Pihl, Conrod, & Dongier, 1998). As such, these theories highlight the role of avoidance coping in drug use problems by implicating avoidance of negative affect as a central motive underlying the development, maintenance, and/or exacerbation of drug use problems among IPV-exposed women.
Consistent with this theoretical literature, avoidance coping is associated with a range of negative drug use outcomes within non-IPV populations, including greater drug use severity (Cooper, Russell, Skinner, Frone, & Mudar, 1992; Ouimette, Finney, & Moos, 1997), posttreatment drug use problems (Chung, Langenbucher, Labouvie, Pandina, & Moos, 2001), drug use cravings among individuals in recovery (Cleveland & Harris, 2010), and decreased likelihood of long-term abstinence (Moos & Moos, 2005). In contrast, Straight, Harper, and Arias (2003) found a non-significant relationship between avoidance coping and drug use problems among IPV-exposed women. While preliminary, this interesting finding suggests that the relationship between avoidance coping and drug use problems may be more complex than previously hypothesized – particularly among women who experience IPV.
The relationship between avoidance coping and drug use problems has historically been viewed and tested as linear, wherein avoidance coping is seen as maladaptive and is positively associated with drug use problems. However, an increasing number of theorists have emphasized the importance of considering the context in which coping strategies are used to determine whether the strategies are maladaptive or adaptive, rather than simply classifying strategies (Aldao, 2013; Calvete, Corral, & Estévez, 2008; Gratz & Roemer, 2004; Kocot & Goodman, 2003; Waldrop & Resick, 2004). Further, these theorists have noted the role of (in)flexible use of coping strategies in predicting outcomes, such that inflexible and rigid use of avoidance coping, whereby an individual relies on avoidance coping strategies without considering the situational demands or her goals, is the strongest predictor of psychopathology (Buss, 2011; Hayes, Strosahl, & Wilson, 1999; Rottenberg, Gross, & Gotlib, 2005). From this perspective, avoidance coping strategies may be considered adaptive within specific contexts.
The utility of avoidance coping may be particularly salient to women in relationships characterized by IPV. According to Lazarus and Folkman (1984), environmental constraints, personal constraints, and extreme threats are related to the effectiveness of coping strategies (e.g., avoidance coping). However, the vast majority of investigations of the relation between avoidance coping and negative outcomes within IPV-exposed populations have failed to consider these contextual constraints and their consequences (Kocot & Goodman, 2003). Nonetheless, there is some evidence to suggest that, when applied flexibly, avoidance coping may be particularly adaptive for IPV-exposed women. For example, Fine (1992) suggested that IPV-exposed women's use of avoidance coping may be more effective for managing relationship problems than problem-focused coping, as efforts to solve problems within their relationships may result in failure and a sense of hopelessness. Likewise, Lewis et al. (2006) argued that putatively adaptive modes of coping may actually be unsafe for IPV-exposed women, suggesting instead that some degree of avoidance coping in the context of physical threat may reduce conflict and buffer the impact of victimization experiences on psychological outcomes. In fact, extant literature suggests that avoidance coping may be functionally adaptive and protective among populations with exposure to repeated or prolonged stressors (Duncan, 1996; Gonzales & Kim, 1997), such as women who experience IPV (Cattaneo & Goodman, 2005). Specifically, whereas problem-solving coping confers greater beneficial psychological outcomes for individuals in environments perceived as controllable, emotion-focused coping (such as avoidance) is associated with adaptive outcomes within environments perceived as uncontrollable (Valentiner, Holahan, & Moos, 1994; Vitaliano, DeWolfe, Maiuro, Russo, & Katon, 1990), such as in the context of an abusive relationship (Walker, 2009). Likewise, greater reliance on putatively adaptive coping strategies such as problem-focused coping has been associated with greater mental health problems among IPV-exposed women (Kocot & Goodman, 2003).
Given evidence to suggest that some degree of avoidance coping may be adaptive, investigation of alternative models to describe the relationship between avoidance coping and drug use problems among IPV-exposed women is warranted. Consequently, the goal of the present study was to extend extant research by exploring whether the relation between levels of avoidance coping (i.e., dose) and drug use problems (i.e., response) is nonlinear. To ensure that any observed relationships between avoidance coping and drug use problems were not simply due to their shared variance with negative affect (Billings, Folkman, Acree, & Moskowitz, 2000; Wills, Sandy, Shinar, & Yaeger, 1999), a measure of negative affect was included in our analyses as a covariate. Given suggestions that flexible use of avoidance coping strategies may be adaptive (Aldao, 2013; Calvete et al., 2008; Kocot & Goodman, 2003; Waldrop & Resick, 2004), particularly when confronted with highly stressful situations (Linehan, 1993), we hypothesized that avoidance coping and drug use problems would demonstrate a U-shaped dose-response relationship, such that moderate levels of avoidance coping would be associated with the lowest levels of drug use problems, and high and low levels of avoidance coping would be associated with higher levels of drug use problems.
Methods
Participants
Participants were 147 women reporting experiences with at least one act of physical victimization by their current male intimate partner in the past 30 days, as measured via phone screen using selected items from the CTS-2 (Straus, Hamby, & Warren, 2003). Additional inclusion criteria were: (a) female gender, (b) age 18 or older, (c) the use of any amount of alcohol or drugs in the previous 30 days, (d) current involvement in a heterosexual intimate relationship of at least six months duration with current contact at least twice a week, and (e) residency in the greater-urban area. Exclusion criteria were (a) inpatient psychiatric hospitalization within the last year, and (b) current residence in a shelter/group home (determined a priori because structured living environments affect women's use of substances).
Women ranged in age from 18 to 57 (M = 38.2, SD = 10.6). In terms of racial/ethnic background, 80.3% of participants self-identified as Black/African American, 9.5% as White, 6.1% as Latina, 2% as Native American, and 2.1% as another or multiple racial/ethnic backgrounds. Most women were unemployed for over a month prior to the study (58.5%), with a mean level of education of 12 years (SD = 1.3) and a mean annual household income of $14,323 (SD = $12,832). Fourteen (9.5%) women were married although over half (59.2%) were living with their partner or saw him on a daily basis (M = 6.4 days a week, SD = 1.3). Mean years in the current relationship was 6.5 years (ranging from 6 months to 27 years; SD = 6 years) and 82.1% of women had children.
Procedures
All procedures were reviewed and approved by Yale University's Institutional Review Board. Data were collected as part of a larger study examining the efficacy and comparability of different methods of daily reporting among IPV-exposed women (T. P. Sullivan, Khondkaryan, Dos Santos, & Peters, 2011). Recruitment materials were posted in local businesses, selected state/public agencies, primary care clinics, and emergency departments, and eligibility was determined via a phone screen. Following informed consent, interviews were administered face-to-face by a trained master- or doctoral-level female research associate. All participants were remunerated $45.
Measures
The Drug Abuse Screening Test (DAST; Skinner, 1982) is a 10-item self-report questionnaire designed to assess drug problems experienced over the previous three months. Items assess the presence of problems related to participants' drug use, such as occupational or relational problems, illegal activities, or regret. Responses to each item have 1 (yes) 1 and 0 (no) options. A total drug use problems score was obtained by summing all items (α = .76).
The Coping Strategies Indicator (CSI; Amirkhan, 1990) is a 33-item self-report measure that assesses strategies for coping with conflict in a current intimate relationship. The CSI assesses individuals' typical levels of coping across three domains: avoidance (e.g., avoided being with people in general, daydreamed about better times), problem-solving (e.g., brainstormed all possible solutions before deciding what to do), and social support (e.g., confided fears and worries to a friend or a relative). Each subscale is composed of 11 items that are summed to create a subscale score. To orient participants to coping strategies they used to deal with recent conflict in their current intimate relationships, they were instructed to describe a conflict with their intimate partner in the past three months that was important to them and caused them to worry. Participants were then asked to rate each item using a 3-point Likert-type scale (1 = not at all, 3 = a lot). The CSI demonstrates adequate psychometric properties (Amirkhan, 1990, 1994), including convergent validity with Vitaliano, Russo, Carr, Maiuro, and Becker's (1985) Ways of Coping Checklist Wishful Thinking and Avoidance subscales (Amirkhan, 1994). For the purposes of the present study, only the avoidance coping domain was examined (α = .79).
The Multidimensional Anxiety Questionnaire (MAQ; Reynolds 1999) is a 40-item self-report questionnaire used to evaluate the severity of anxiety symptoms over the previous three months. The MAQ assesses individuals' anxiety severity across four factorially derived subscales: physiological-panic (e.g., shaky hands), social phobia (e.g., nervous with people), worry-fears (e.g., afraid of being alone), and negative affectivity (e.g., irritable). Given past findings of a strong relationship between negative affectivity and both avoidance coping (Billings et al., 2000) and drug use severity (Wills et al., 1999), the negative affectivity scale was included as a covariate in this study to ensure that any observed relationships between avoidance coping and drug use severity are not due simply to their shared variance with negative affectivity (α = .81).
Results
The mean avoidance coping score (M = 23.83, SD = 4.80, scores ranged from 11-32) was approximately one standard deviation higher than reported in Amirkhan's (1990) original community sample (i.e., M = 19.03, SD = 4.37). Drug use problems scores ranged from 0 to 10 (M = 3.20, SD = 2.71), and negative affect scores ranged from 9 to 34 (M = 20.39, SD = 4.96).
In analyzing the relationship between avoidance coping and drug use problems, we used hierarchical polynomial regression analyses to model the potential curvilinear nature of the relationship. Specifically, we utilized a quadratic regression model to test for a hypothesized U-shaped relation between avoidance coping and drug use problems where moderate levels of avoidance coping were expected to be associated with lower drug use problems. Prior to analysis, the predictor variables (avoidance coping and negative affect) were centered as recommended by Cohen, Cohen, West, and Aiken (2003).
The results of the regression analyses are presented in Table 1. The initial step of the model included the lower order terms for avoidance coping and negative affect and was statistically significant, F (2, 144) = 11.48, p < .001, R2 = 0.14. In this simple, rectilinear component of the model, avoidance coping was not related to drug use problems, b = 0.03, 95% CI [-0.06, 0.12] whereas negative affect predicted higher drug use problems, b = 0.19, 95% CI [0.10, 0.28]. The second step of the model included the lower order terms for avoidance coping and negative affect in addition to the squared avoidance variable to measure the curvilinear effects of avoidance coping on drug use problems. The second step (i.e., the quadratic component) was also statistically significant when compared to the null model, F (3, 143) = 10.07, p < .001, but more importantly, it provided a statistically significant improvement in fit (ΔR2 = 0.04) when compared to the simple linear component of the model (i.e., step 1), F = 6.39, p < .05. The quadratic term for avoidance coping (i.e., avoidance2) was statistically significant, b = 6.35, 95% CI [1.38, 11.32] and, as is apparent in Figure 1, represents a U-shaped relationship between avoidance coping and drug use problems where the lowest levels of drug use problems are observed at moderate levels of avoidance coping in contrast to the higher levels of drug use problems observed at both the high and low ends of the avoidance coping continuum.
Table 1.
Hierarchical quadratic regression analyses of avoidance and drug use problems.
| B | 95% CI | Bse | β | t value | p | VIF | |
|---|---|---|---|---|---|---|---|
| Step 1: R2 = 0.14, p < .001 | |||||||
| Intercept | 3.20 | [2.79, 3.62] | 0.209 | 15.35 | < .001 | ||
| Negative Affect | 0.19 | [0.10, 0.28] | 0.045 | 0.35 | 4.29 | < .001 | 1.12 |
| Avoidance Coping | 0.03 | [-0.06, 0.12] | 0.046 | 0.05 | 0.61 | 0.5403 | 1.12 |
| Step 2: ΔR2 = 0.04, p = .013 | |||||||
| Intercept | 3.20 | [2.79, 3.61] | 0.205 | 15.63 | < .001 | ||
| Negative Affect | 0.21 | [0.12, 0.30] | 0.044 | 0.38 | 4.70 | < .001 | 1.15 |
| Avoidance Coping | 1.31 | [-3.90, 6.52] | 2.634 | 0.48 | 0.50 | 0.620 | 1.19 |
| Avoidance Coping2 | 6.35 | [1.38, 11.32] | 2.514 | 2.35 | 2.53 | 0.013 | 1.13 |
Note. VIF = variance inflation factor.
Figure 1.
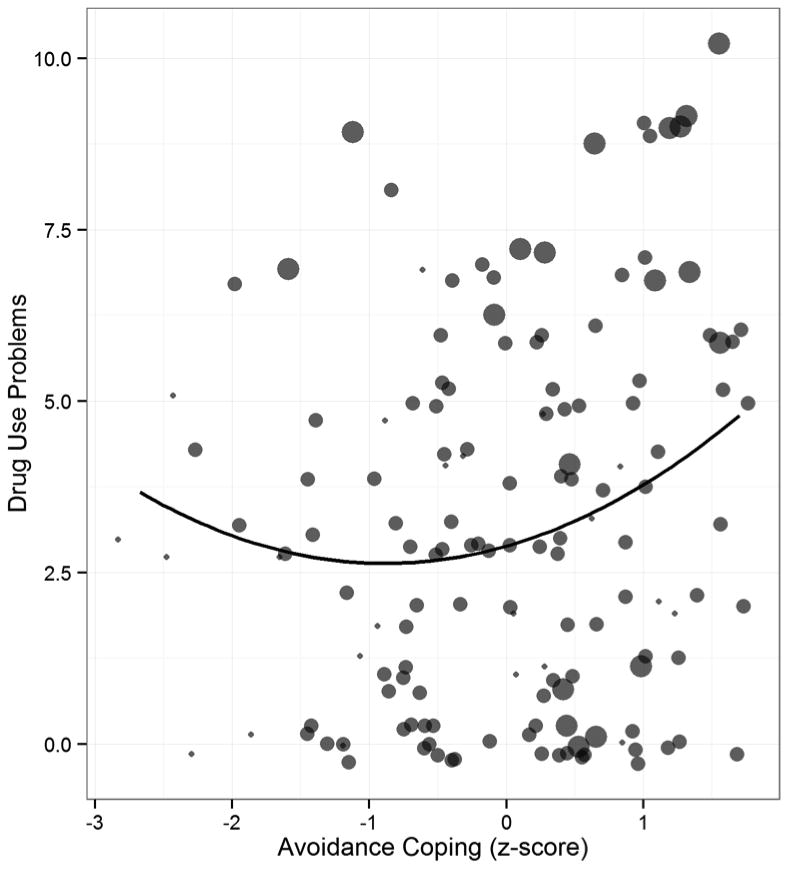
Scatter plot of drug use problems and avoidance coping scores (jittered) with the size of each point mapped onto negative affect levels superimposed with the curvilinear relation between avoidance and drug use severity.
Discussion
The goal of the present study was to examine whether the relationship between avoidance coping and drug use problems among IPV-exposed women is best characterized as nonlinear. Specifically, given evidence to suggest that flexible use of avoidance coping may be adaptive among women whose relationships are characterized by IPV (Fine, 1992; Kocot & Goodman, 2003; Lewis et al., 2006), we examined whether there was a U-shaped dose-response effect of avoidance coping on drug use problems. Consistent with study hypotheses, moderate levels of avoidance coping were associated with lower levels of drug use problems, whereas high and low levels of avoidance coping predicted higher levels of drug use problems. While preliminary, this finding highlights the role of contextual factors in the relationship between avoidance coping and drug use problems, and suggests that avoidance coping strategies, when used in moderation, may be an adaptive strategy for coping with distress stemming from relational conflict among IPV-exposed women.
Given evidence of a significant positive association between avoidance coping and drug use problems in other trauma-exposed samples (Ouimette, Finney, & Moos, 1999; Ullman, Filipas, Townsend, & Starzynski, 2006), it is possible that the results of this study reflect the unique experiences of IPV-exposed women (versus individuals with traumatic exposure more broadly). Upwards of 93% of IPV-exposed women report repeated victimization by their intimate partners (Cattaneo & Goodman, 2005). Further, attempts to leave abusive relationships are often unsuccessful (Campbell, Miller, Cardwell, & Belknap, 1994; Herbert, Silver, & Ellard, 1991), and, when successful, may result in continued threats, physical assault, and stalking (C. M. Sullivan, Campbell, Angelique, Eby, & Davidson, 1994; Wilson, Johnson, & Daly, 1995) . Thus, IPV-exposed women may experience relational conflict as particularly unpredictable and uncontrollable (Walker, 2009). Importantly, use of avoidance coping strategies in contexts perceived as unpredictable or uncontrollable has been shown to confer greater adaptive psychological outcomes (Valentiner et al., 1994; Vitaliano et al., 1990). For example, because women who experience IPV are not able to control their partner's behavior, use of avoidance coping strategies may redirect attention toward pleasurable activities, subsequently increasing positive affect and decreasing risk for depression or posttraumatic stress. Under these circumstances, avoidance coping could be viewed as functionally adaptive and protective (Gonzales & Kim, 1997). Future research is needed to elucidate specific situational contexts in which avoidance coping may be adaptive for IPV-exposed women.
Interestingly, and consistent with our hypotheses, lower levels of avoidance coping were associated with higher levels of drug use problems. This finding provides support for the utility of avoidance coping, when used in moderation, in IPV-exposed populations (Fine, 1992; Kocot & Goodman, 2003; Lewis et al., 2006). Further, it highlights one potential strategy for intervening with IPV-exposed women who exhibit drug use problems. In fact, several empirically-supported treatments incorporate avoidance coping strategies. For example, in Dialectical Behavioral Therapy (Linehan, 1993), distraction, which entails noticing aversive emotions and then temporarily redirecting one's attention toward something other than the emotion, is recommended when the patient's goal is to tolerate or survive a highly stressful situation, such as IPV victimization. Likewise, Emotion Regulation Group Therapy (Gratz & Gunderson, 2006; Gratz & Tull, 2011; Gratz, Tull, & Levy, 2013) teaches women how to use distraction in a flexible and situationally-appropriate manner to modulate the intensity and/or duration of their emotions. Notably, although treatments that teach effective use of distraction have been found to reduce substance use (Axelrod, Perepletchikova, Holtzman, & Sinha, 2011; Gratz & Tull, 2011), few studies have examined the effects of these treatments outside the context of borderline personality pathology. Future investigations are needed to examine the utility of these treatments in reducing substance use within other populations, such as women who experience IPV.
In evaluating the implications of our findings, it is important to take into account study limitations. First, the cross-sectional and correlational nature of the data precludes determination of the precise nature and direction of the relationships examined. For example, it is possible that this association is bidirectional and that drug use problems may lead to or exacerbate avoidance coping. Future research should investigate the nature and direction of this relationship through prospective, longitudinal investigations. Second, while drawn from a well-established and empirically-validated assessment (Amirkhan, 1990), our measure of avoidance coping does not differentiate between the various functions avoidance behaviors may serve (i.e., permanent or temporary redirection away from emotions). Thus, it is unclear whether or not we were assessing more adaptive forms of avoidance coping, such as distraction, which is theorized to reduce the intensity and/or duration of aversive emotions or behavioral urges (e.g., drug use; Linehan, 1993). Third, avoidance coping is associated with mental disorders prevalent among IPV-exposed women, such as depression (Amirkhan, 1994). As such, future research would benefit from examination of the role of mental disorders in avoidance coping and drug use problems. Fourth, future studies would benefit from examination of whether the relation between levels of avoidance coping and drug use problems is nonlinear when controlling for positive affect (which is associated with substance use outcomes; Cooper, Frone, Russell, & Mudar, 1995). Fifth, although our focus on community-recruited substance using women who experience IPV may be considered a strength of this study, findings may not generalize to other IPV populations (including men who experience IPV and women recruited from IPV shelters) or non-IPV populations. For example, women were only eligible for this study if they reported past 30 day alcohol or drugs use; thus, future research is needed to examine whether our findings vary as a function of current substance use status (present vs. absent). Lastly, replication and extension of the curvilinear dose-response effect of avoidance coping on other clinically-relevant behaviors (e.g., risky sexual behavior, deliberate self-harm) is warranted.
Despite these limitations, results of this study contribute to the extant literature examining the role of avoidance coping in drug use problems among women who experience IPV. Specifically, moderate levels of avoidance coping were associated with lower levels of drug use problems, whereas high and low levels of avoidance coping were associated with higher levels of drug use problems. As such, our results suggest the potential utility of teaching women who experience IPV how to effectively reduce the intensity of emotional arousal through adaptive forms of avoidance coping, such as distraction.
Acknowledgments
Funding: This work was supported by the National Institutes of Health under Grant (K23 DA019561); the National Institutes of Health under Grant (T32DA019426); and the University of Connecticut General Clinical Research Center under Grant (M01 RR06192).
Contributor Information
Nicole H. Weiss, Email: nhweiss7@gmail.com, Department of Psychiatry, Yale University School of Medicine, 389 Whitney Avenue, New Haven, CT 06511, Phone: (203)789-7645.
Aaron A. Duke, Email: aaron.duke@yale.edu, Department of Psychiatry, Yale University School of Medicine, 389 Whitney Avenue, New Haven, CT 06511, Phone: (203)789-7645.
Tami P. Sullivan, Email: tami.sullivan@yale.edu, Department of Psychiatry, Yale University School of Medicine, 389 Whitney Avenue, New Haven, CT 06511, Phone: (203)789-7645.
References
- Aldao A. The future of emotion regulation research capturing context. Perspectives on Psychological Science. 2013;8:155–172. doi: 10.1177/1745691612459518. [DOI] [PubMed] [Google Scholar]
- Amirkhan JH. A factor analytically derived measure of coping: The Coping Strategy Indicator. Journal of Personality and Social Psychology. 1990;59:1066–1074. doi. [Google Scholar]
- Amirkhan JH. Criterion validity of a coping measure. Journal of Personality Assessment. 1994;62:242–261. doi: 10.1207/s15327752jpa6202_6. [DOI] [PubMed] [Google Scholar]
- Axelrod SR, Perepletchikova F, Holtzman K, Sinha R. Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. The American Journal of Drug and Alcohol Abuse. 2011;37:37–42. doi: 10.3109/00952990.2010.535582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Billings DW, Folkman S, Acree M, Moskowitz JT. Coping and physical health during caregiving: The roles of positive and negative affect. Journal of Personality and Social Psychology. 2000;79:131–142. doi: 10.1037//0022-3514.79.1.131. [DOI] [PubMed] [Google Scholar]
- Brewer DD, Fleming CB, Haggerty KP, Catalano RF. Drug use predictors of partner violence in opiate-dependent women. Violence and Victims. 1998;13:107–115. [PubMed] [Google Scholar]
- Brown DS, Finkelstein EA, Mercy JA. Methods for estimating medical expenditures attributable to intimate partner violence. Journal of Interpersonal Violence. 2008;23:1747–1766. doi: 10.1177/0886260508314338. [DOI] [PubMed] [Google Scholar]
- Buss KA. Which fearful toddlers should we worry about? Context, fear regulation, and anxiety risk. Developmental Psychology. 2011;47:804–819. doi: 10.1037/a0023227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvete E, Corral S, Estévez A. Coping as a mediator and moderator between intimate partner violence and symptoms of anxiety and depression. Violence Against Women. 2008;14:886–904. doi: 10.1177/1077801208320907. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Miller P, Cardwell MM, Belknap RA. Relationship status of battered women over time. Journal of Family Violence. 1994;9:99–111. doi: 10.1007/BF01531957. [DOI] [Google Scholar]
- Cattaneo LB, Goodman LA. Risk factors for reabuse in intimate partner violence a cross-disciplinary critical review. Trauma, Violence, & Abuse. 2005;6:141–175. doi: 10.1177/1524838005275088. [DOI] [PubMed] [Google Scholar]
- Chung T, Langenbucher J, Labouvie E, Pandina RJ, Moos RH. Changes in alcoholic patients' coping responses predict 12-month treatment outcomes. Journal of Consulting and Clinical Psychology. 2001;69:92–100. doi: 10.1037/0022-006X.69.1.92. [DOI] [PubMed] [Google Scholar]
- Cleveland HH, Harris KS. The role of coping in moderating within-day associations between negative triggers and substance use cravings: A daily diary investigation. Addictive Behaviors. 2010;35:60–63. doi: 10.1016/j.addbeh.2009.08.010. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West S, Aiken L. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037/0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101:139–152. doi: 10.1037/0021-843X.101.1.139. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Compton WM, Mager D, Spitznagel EL, Janca A. Posttraumatic stress disorder among substance users from the general population. American Journal of Psychiatry. 1992;149:664–670. doi: 10.1176/ajp.149.5.664. [DOI] [PubMed] [Google Scholar]
- Duncan DF. Growing up under the gun: Children and adolescents coping with violent neighborhoods. Journal of Primary Prevention. 1996;16:343–356. doi: 10.1007/BF02411740. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Schilling R, Wada T. Drug abuse and partner violence among women in methadone treatment. Journal of Family Violence. 2000;15:209–228. doi: 10.1023/A:1007532917759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Go H, Hill J. Relationship between drug abuse and intimate partner violence: A longitudinal study among women receiving methadone. American Journal of Public Health. 2005;95:465–470. doi: 10.2105/AJPH.2003.023200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine M. Disruptive voices: The possibility of feminist research. Ann Arbor, MI: University of Michigan Press; 1992. [Google Scholar]
- Garcia-Moreno C, Jansen HAFM, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: Findings from the WHO multi-country study on women's health and domestic violence. The Lancet. 2006;368:1260–1269. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14:99–132. doi: 10.1023/A:1022079418229. [DOI] [Google Scholar]
- Gonzales NA, Kim LS. Stress and coping in an ethnic minority context. In: Wolchik SA, Sandler IN, editors. Handbook of Children's Coping. Springer; 1997. pp. 481–511. [Google Scholar]
- Gratz KL, Gunderson JG. Preliminary data on an acceptance-based emotion regulation group intervention for deliberate self-harm among women with borderline personality disorder. Behavior Therapy. 2006;37:25–35. doi: 10.1016/j.beth.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Gratz KL, Tull MT. Extending research on the utility of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality pathology. Personality Disorders: Theory, Research, and Treatment. 2011;2:316–326. doi: 10.1037/a0022144. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Tull MT, Levy R. Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychological Medicine. 2013:1–14. doi: 10.1017/S0033291713002134. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press; 1999. [Google Scholar]
- Herbert TB, Silver RC, Ellard JH. Coping with an abusive relationship: I. How and why do women stay? Journal of Marriage and the Family. 1991;53:311–325. doi: 10.2307/352901. [DOI] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology. 1997;65:834–847. doi: 10.1037/0022-006X.65.5.834. [DOI] [PubMed] [Google Scholar]
- Kocot T, Goodman L. The roles of coping and social support in battered women's mental health. Violence Against Women. 2003;9:323–346. doi: 10.1177/1077801202250075. [DOI] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY: Springer; 1984. [Google Scholar]
- Lewis CS, Griffing S, Chu M, Jospitre T, Sage RE, Madry L, Primm BJ. Coping and violence exposure as predictors of psychological functioning in domestic violence survivors. Violence Against Women. 2006;12:340–354. doi: 10.1177/1077801206287285. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Moos RH, Moos BS. Paths of entry into Alcoholics Anonymous: Consequences for participation and remission. Alcoholism: Clinical and Experimental Research. 2005;29:1858–1868. doi: 10.1097/01.alc.0000183006.76551.5a. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Finney JW, Moos RH. Twelve-step and cognitive-behavioral treatment for substance abuse: A comparison of treatment effectiveness. Journal of Consulting and Clinical Psychology. 1997;65:230–240. doi: 10.1037/0022-006X.65.2.230. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Finney JW, Moos RH. Two-year posttreatment functioning and coping of substance abuse patients with posttraumatic stress disorder. Psychology of Addictive Behaviors. 1999;13:105–114. doi: 10.1037/0893-164X.13.2.105. [DOI] [Google Scholar]
- Rottenberg J, Gross JJ, Gotlib IH. Emotion context insensitivity in major depressive disorder. Journal of Abnormal Psychology. 2005;114:627–639. doi: 10.1037/0021-843X.114.4.627. [DOI] [PubMed] [Google Scholar]
- Schafer J, Caetano R, Clark CL. Rates of intimate partner violence in the United States. American Journal of Public Health. 1998;88:1702–1704. doi: 10.2105/AJPH.88.11.1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA. The drug abuse screening test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Stewart SH. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;120:83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Pihl RO, Conrod PJ, Dongier M. Functional associations among trauma, PTSD, and substance-related disorders. Addictive Behaviors. 1998;23:797–812. doi: 10.1016/S0306-4603(98)00070-7. [DOI] [PubMed] [Google Scholar]
- Straight ES, Harper FWK, Arias I. The impact of partner psychological abuse on health behaviors and health status in college women. Journal of Interpersonal Violence. 2003;18:1035–1054. doi: 10.1177/0886260503254512. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Warren WL. The conflict tactics scales handbook. Los Angeles, CA: Western Psychological Services; 2003. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Reults from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies; 2009. [Google Scholar]
- Sullivan CM, Campbell R, Angelique H, Eby KK, Davidson WS. An advocacy intervention program for women with abusive partners: Six-month follow-up. American Journal of Community Psychology. 1994;22:101–122. doi: 10.1007/BF02506819. [DOI] [PubMed] [Google Scholar]
- Sullivan TP, Khondkaryan E, Dos Santos NP, Peters EN. Applying experience sampling methods to partner violence research: Safety and feasibility in a 90-day study of community women. Violence Against Women. 2011;17:251–266. doi: 10.1177/1077801210397756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Livingston JA. Alcohol and sexual aggression reciprocal relationships over time in a sample of high-risk women. Journal of Interpersonal Violence. 2000;15:413–427. doi: 10.1177/088626000015004005. [DOI] [Google Scholar]
- Testa M, Livingston JA, Leonard KE. Women's substance use and experiences of intimate partner violence: A longitudinal investigation among a community sample. Addictive Behaviors. 2003;28:1649–1664. doi: 10.1016/j.addbeh.2003.08.040. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, Starzynski LL. Correlates of comorbid PTSD and drinking problems among sexual assault survivors. Addictive Behaviors. 2006;31:128–132. doi: 10.1016/j.addbeh.2005.04.002. [DOI] [PubMed] [Google Scholar]
- Valentiner DP, Holahan CJ, Moos RH. Social support, appraisals of event controllability, and coping: An integrative model. Journal of Personality and Social Psychology. 1994;66:1094–1102. doi: 10.1037/0022-3514.66.6.1094. [DOI] [Google Scholar]
- Vitaliano PP, DeWolfe DJ, Maiuro RD, Russo J, Katon W. Appraised changeability of a stressor as a modifier of the relationship between coping and depression: A test of the hypothesis of fit. Journal of Personality and Social Psychology. 1990;59:582–592. doi: 10.1037/0022-3514.59.3.582. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Russo J, Carr JE, Maiuro RD, Becker's J. The ways of coping checklist: Revision and psychometric properties. Multivariate Behavioral Research. 1985;20:3–26. doi: 10.1207/s15327906mbr2001_1. [DOI] [PubMed] [Google Scholar]
- Walby S. The cost of domestic violence: Up-date 2009. Lancaster University; Lancaster: 2009. [Google Scholar]
- Waldrop AE, Resick PA. Coping among adult female victims of domestic violence. Journal of Family Violence. 2004;19:291–302. doi: 10.1023/B:JOFV.0000042079.91846.68. [DOI] [Google Scholar]
- Walker LE. The battered woman syndrome. 3rd. New York, NY: Springer Publishing Company; 2009. [Google Scholar]
- Wills TA, Sandy JM, Shinar O, Yaeger A. Contributions of positive and negative affect to adolescent substance use: Test of a bidimensional model in a longitudinal study. Psychology of Addictive Behaviors. 1999;13:327–338. doi: 10.1037/0893-164X.13.4.327. [DOI] [Google Scholar]
- Wilson M, Johnson H, Daly M. Lethal and nonlethal violence against wives. Canadian Journal of Criminology. 1995;37:331–361. doi: 10.4135/9781452243306.n8. [DOI] [Google Scholar]


