Abstract
We investigated the ability of using monoclonal antibodies (MAbs) against anthrax protective antigen (PA), an anthrax exotoxin component, to modulate exotoxin cytotoxic activity on target macrophage cell lines. Anthrax PA plays a critical role in the pathogenesis of Bacillus anthracis infection. PA is the cell-binding component of the two anthrax exotoxins: lethal toxin (LeTx) and edema toxin. Several MAbs that bind the PA component of LeTx are known to neutralize LeTx-mediated killing of target macrophages. Here we describe for the first time an overlooked population of anti-PA MAbs that, in contrast, function to increase the potency of LeTx against murine macrophage cell lines. The results support a possible mechanism of enhancement: binding of MAb to PA on the macrophage cell surface stabilizes the PA by interaction of MAb with macrophage Fcγ receptors. This results in an increase in the amount of PA bound to the cell surface, which in turn leads to an enhancement in cell killing, most likely due to increased internalization of LF. Blocking of PA-receptor binding eliminates enhancement by MAb, demonstrating the importance of this step for the observed enhancement. The additional significance of these results is that, at least in mice, immunization with PA appears to elicit a poly-clonal response that has a significant prevalence of MAbs that enhance LeTx-mediated killing in macrophages.
Anthrax protective antigen (PA) is a key molecule in the tripartite anthrax toxin that causes impairment of cellular activity and cell death during infection with Bacillus anthracis. PA plays a central role in the toxin-mediated pathogenesis of anthrax, interacting with other proteins to form two exotoxins: lethal toxin (LeTx) and edema toxin (EdTx) (29). PA is a well-characterized molecule, and its functional domains have been identified (29, 31). PA in association with edema factor comprises EdTx, which has been shown to impair cellular function (20, 21). LeTx, comprised of PA in association with lethal factor (LF), contributes to death from anthrax (2, 36). It has also been shown that LeTx causes lysis and the death of murine macrophages in vitro (8, 11-13), forming the basis of standard bioassays to measure LeTx activity (8, 24). EdTx has been shown to have additional deleterious effects in animal models when administered along with LeTx (32).
The various steps in LeTx intoxication of cells have been identified. Initially, PA (83 kDa) binds to ubiquitously expressed cell surface receptors (3, 6, 26). Binding is followed by cleavage of PA by cell-associated furin-like proteases, releasing a 20-kDa fragment to produce the activated form, PA63 (63 kDa) (19, 23). The next steps are formation of a heptamer of PA63 molecules and binding of LF to the PA63 (27, 31). The PA63:LF complexes are internalized and undergo acidification within the endosomal pathway, leading to translocation of LF into the cytoplasm (8, 28). LF is a zinc metalloprotease (10, 11, 18) that cleaves mitogen-activated protein kinase kinase (MAPKK) or mitogen-activated extracellularly regulated kinase-activating kinase (MEK) in the cytoplasm, thereby inhibiting the MAPK signal transduction pathway (5, 41).
Panels of hybridomas secreting monoclonal antibodies (MAbs) with specificity for PA have been generated from the splenic B cells of mice that were immunized with PA (25). Some of these MAbs have been shown to neutralize LeTx activity in vitro (25). Other MAbs have been shown to bind PA but not to exhibit any neutralizing effect on the toxin in vitro or in vivo (25). The binding sites of several anti-PA MAbs have been mapped to key domains on the PA molecule by competitive analysis and through the use of PA mutants (25, 34).
We describe a population of non-neutralizing MAbs generated by two different immunizing protocols that enhance LeTx-mediated killing of murine macrophage cell lines in a modified in vitro LeTx cytotoxicity assay. Although antibody-mediated enhancement of infectivity of virus particles in host cells has been reported (39), there are no reports to date of a similar phenomenon in the case of protein toxins. Furthermore, our results show that the enhancement of LeTx-mediated cytotoxicity in the presence of anti-PA MAbs requires interaction of the Fc domain of MAbs with their counterpart receptors and binding of PA to its receptor on the cell surface. The sensitivity of cells to the toxin and presence of Fc receptors on the cell surface are critical factors in enabling enhancement of killing in the presence of these anti-PA MAbs. The effect of the presence of these anti-PA MAbs on steps of LeTx intoxication, such as PA binding to the cell surface, acidification of intracellular compartments, and MEK cleavage, was also investigated. This is the first time that the enhanced potency of a toxin in the presence of an anti-toxin MAb has been reported.
MATERIALS AND METHODS
Cell lines.
Murine macrophage cell lines J774.1, RAW 264.7, and P388D1, human macrophage cell lines U937 and THP-1, and Chinese hamster ovary (CHO) cells were obtained from the American Type Culture Collection (ATCC) and were maintained according to ATCC protocols. The FcγR-transfected CHO cell line mRG1-1, a CHO cell line transfected with the binding chain of the mouse FcγRI (4), was a gift from Daniel Conrad, Virginia Commonwealth University. Early-passage cells were frozen down to create working cell banks. Murine macrophage cell lines J774A.1, RAW 264.7, and P388D1 were grown in Dulbecco’s modified Eagle medium containing 10% fetal bovine serum (FBS). Human macrophage cell lines U937 and THP-1 were grown in RPMI containing 10% FBS. CHO cells and mRG1-1 cells were grown in F12K containing 5% FBS. To ensure consistency in bioassay results, cells were discarded after 12 to 13 passages and a new working cell bank vial was thawed for use.
MAbs.
All MAbs used in the study are listed in Table 1. Some of the MAbs used for the present study have been described previously (25) and were purified from ascites (see below). Other MAbs were received from William Sutherland at the University of Virginia and had been generated under a Collaborative Research and Development Agreement between the University of Virginia and the U.S. Army Medical Research Institute of Infectious Diseases. These MAbs were the result of immunization of BALB/c mice with PA, along with CpG (ImmunEasy mouse adjuvant; Qiagen, Valencia, Calif.) as an adjuvant.
TABLE 1.
MAbs used for this study
| MAb clone | Form | Isotypea | Concnb | Kd (nM)c | Adjuvant | Source or reference |
|---|---|---|---|---|---|---|
| Anti-PA 14B7d | Affinity purified from ascites | IgG1 | 3.3 mg/ml | 4.0 | Freund | Little et al (25) |
| Anti-PA 3F3d | Affinity purified from ascites | IgG1 | 1.3 mg/ml | 9.1 | Freund | Little et al. (25) |
| Anti-PA 3B6 | Affinity purified from ascites | IgG1 | 1.2 mg/ml | 10.3 | Freund | Little et al. (25) |
| Anti-PA 2F9 | Affinity purified from ascites | IgG1 | 0.5 mg/ml | ND | Freund | Little et al. (25) |
| Anti-PA 6C3 | Ascites | IgG1 | 7.7 mg/ml | ND | Freund | Little et al. (25) |
| Anti-PA 2A2 | Tissue culture supernatant | IgG2a | 16.8 μg/ml | ND | CPG | This study |
Isotype was determined by using a mouse isotyping kit (Bio-Rad).
The protein concentration was determined by using a modified Lowry assay kit (Sigma-Aldrich) for purified MAbs. The concentration of mouse IgG in ascites and hybridoma supernatant was determined by using a kit from Roche.
Dissociation constants were determined by using the BiaCore 3000 system.
MAbs 14B7 and 3F3 bind to different epitopes on PA (25).
Mouse immunoglobulin G (IgG) concentrations in each of the ascitic fluids or hybridoma supernatants were determined by using an ELISA kit (Roche Diagnostics, Inc., Indianapolis, Ind.). Isotype testing was performed with a kit from Bio-Rad (Hercules, Calif.). The endotoxin concentration in all MAb preparations was determined by using an LAL-Pyrochrome kit (Associates of Cape Cod, Cape Cod, Mass.) with pyrogen-free materials as recommended in the product insert. All MAbs were found to be low in endotoxin (<2 EU/ml at the highest concentration used, i.e., 10 μg of MAb/ml).
MAb 2.4G2 (FcBlock; BD Biosciences, San Jose, Calif.) was used to block Fc receptors on cell surfaces. This MAb binds to mouse FcγRII and FcγRIII via its Fab region. It also binds to FcγRI to some extent via its Fc (40).
Purification of MAb and preparation of Fab.
MAbs 3F3, 3B6, 2F9, and 14B7 were purified from ascites fluid by protein A affinity chromatography. Fab fragments were prepared from purified MAbs by using a papain digestion kit according to manufacturer's instructions (Pierce Biotechnology, Inc., Rockford, Ill.). The Fab fragments were analyzed by standard methods to determine concentration, molecular weight, and purity (by Lowry assay and sodium dodecyl sulfate-polyacrylamide gel electrophoresis).
Affinity measurements.
To determine affinity for some of the MAbs, kinetic measurements were made by using the BiaCore 3000 system (BiaCore, Inc., Piscataway, N.J.). Rabbit anti-mouse (RAM) polyclonal antibodies were covalently linked to a CM5 chip via amine coupling according to the manufacturer's instructions (Biacore). The anti-PA MAb (ligand) was captured on the RAM-coated CM5 chip, and PA (analyte) was flowed at various concentrations over the MAb. All MAbs and PA were diluted in BiaRunning buffer (BioCore). After each MAb:PA cycle, the chip was regenerated by using 20 mM HCl for 30 s. The generated sensograms were analyzed by using BIAevaluation software (BiaCore) to yield the dissociation constant (Kd).
LeTx neutralization assay.
Neutralization of LeTx cytotoxicity by anti-PA MAbs was performed as previously described (24) with a few modifications. Recombinant PA (7, 22) and purified LF (22) were produced as described above. Wells of 96-well microtiter plates were seeded with either 100,000 J774A.1 cells, 200,000 RAW 264.7 cells, or 30,000 U937, THP-1/P388D1, CHO, or mRG1-1 cells per well. Lethal toxin components (PA+LF) were added simultaneously to MAb(s), Fab, or medium alone, followed by incubation for 1 h at 37°C prior to addition to macrophages. The final concentrations of LeTx used for the experiments were determined to result in ca. 50% killing (final concentration of LeTx = 30 ng of PA/ml + 30 ng of LF/ml) or 100% killing (final concentration of LeTx = 80 ng of PA/ml + 80 ng of LF/ml) of J774A.1 and RAW 264.7 cells. For experiments in which MAb 2.4G2 was used to block FcγRII or FcγRIII, the MAb was preincubated with the cells for 1 h before samples and LeTx were added. The LeTx reaction mixture was added to the macrophages and, after a 4-h incubation with cells at 37°C, MTT [3-(4,5-dimethylthiazole-2-yl)-2,5-diphenyl tetrazolium bromide] was added and the cells were incubated for 1 h. Cells were lysed and solubilized by addition of lysing-solubilization buffer (14). After an overnight incubation at 37°C, the plates were read at 570 nm on a plate reader, and the data were analyzed by using SoftMaxPro software (Molecular Devices, Sunnyvale, Calif.).
For U937, THP-1, P388D1, or CHO cells and the FcγRI-transfected CHO cells (mRG1-1), LeTx and MAb mixtures were preincubated for 1 h and incubated with the cells for 48 h before addition of MTT.
For some experiments, LeTx neutralization samples were analyzed by flow cytometry. J774A.1 or RAW 264.7 cells were preincubated with LeTx and either MAb or medium in duplicate for 4 h at 37°C. LeTx was used at a concentration that yielded ca. 50% killing (100 to 120 ng of PA/ml and LF). The cells were washed once with phosphate-buffered saline (PBS)-bovine serum albumin (BSA) buffer (PBS containing 0.5% BSA) after the incubation and then stained with propidium iodide (PI) for 20 min at room temperature. The cells were then washed twice with PBS-BSA buffer and immediately analyzed on a flow cytometer (BD FACSCalibur; Becton Dickinson). Cells were gated based on the forward-scatter versus side-scatter profile. The PI-positive population was designated the dead cell population.
Effect of lysosomotropic agents on LeTx-mediated killing.
LeTx was added to J774A.1 or RAW 264.7 cells (100 ng of PA/ml and 100 ng of LF/ml) in the presence or absence of MAb 2A2 or 3F3 at 2 μg/ml. NH4Cl or monensin was then added to the medium containing cells at concentrations between 0 and 250 μg/ml and 0 and 5 μg/ml, respectively (8). After a 4-h incubation at 37°C, the cells were washed once, stained with PI, and analyzed by flow cytometry.
Western blots and densitometry.
PA or LeTx preincubated with various MAbs was added to 6 × 106 J774A.1 or RAW 264.7 cells, and samples were obtained at various time points. The final concentration of toxin components (PA and LF) and MAb were 100 ng/ml and 1.5 μg/ml, respectively. For some experiments, cells were incubated with MAb 2.4G2 at 1 μg per 106 cells prior to the addition of the toxin-MAb reaction mixture. After they were washed with PBS, the cells were resuspended in radioimmunoprecipitation assay-phenylmethylsulfonyl fluoride buffer and homogenized on ice. The total protein of the cell lysate was quantified by using a modified Lowry assay according to the manufacturer's instructions (Sigma-Aldrich, St. Louis, Mo.). All reagents for Western blotting were purchased from Santa Cruz Biotechnology (Santa Cruz, Calif.) unless specified otherwise. Equal amounts of protein for each sample (20 to 25 μg per lane) were loaded onto a 4 to 12% Tris-glycine gel (Invitrogen) and electrophoretically transferred onto nitrocellulose membranes (Schleicher & Schuell, Keene, N.H.). Nonspecific binding was blocked with Blotto A in Tris-buffered saline (TBS), followed by incubation overnight at 4°C, followed by three washes with TBS with 0.05% Tween 20. The immunodetection of PA was performed with anti-PA MAb 2D3 (25) as the primary antibody and goat anti-mouse-horseradish peroxidase as the secondary antibody. The immunodetection of MEK-1 was done with rabbit polyclonal anti-MEK-1 as the primary antibody (Upstate Biotech, Waltham, Mass.) and goat anti-rabbit-horseradish peroxidase as the secondary antibody. Primary and secondary incubations were for 1 h at room temperature, followed by three washes with TBS-0.05% Tween 20. The specific target proteins were then visualized by applying Luminol reagents to the blot. Images were captured by using a BioChemi dark-room imaging system (UVP, Upland, Calif.) and analyzed with LabWorks software.
Statistical analysis.
Statistical significance was determined by using the two-tailed Student t test assuming unequal variances. A P value of <0.05 was considered significant.
RESULTS
Discovery of MAbs that enhance LeTx-mediated killing of macrophages.
MAbs raised against PA with either Freund or CpG adjuvants were tested in LeTx neutralization assays. Neutralizing activity was first determined by using a standard neutralization assay (LeTx concentration = 100% lethal concentration [LC100]). These results confirmed previous reports (25) that anti-PA MAb 14B7 neutralized LeTx cytotoxicity, whereas anti-PA MAbs 2F9, 3F3, and 6C3 did not (Fig. 1a). However, when LeTx concentration that yielded ca. 50% killing (i.e., the LC50) was used, thus increasing the sensitivity of the assay, MAbs that have been shown to be non-neutralizing (25) (Fig. 1a) now increased the cytotoxicity of LeTx, as shown by a decrease in viability of J774A.1 cells in the presence of the MAbs (Fig. 1b). To determine whether the increased cytotoxicity observed in the presence of the MAbs required LeTx, samples with MAb alone, MAb with PA, and MAb with LF were analyzed. None of these controls demonstrated significantly more killing than background (data not shown).
FIG. 1.
Toxin neutralization assays. (a) Standard assay performed with a LeTx concentration of LC100; (b) modified assay done with a LeTx concentration of LC50. The viability of J774A.1 cells incubated with increasing amounts of anti-PA MAbs, along with LeTx at a concentration of LC100 (PA at 80 ng/ml, LF at 80 ng/ml) or LC50 (PA at 30 ng/ml, LF at 30 ng/ml), was determined. The MAb-LeTx mixture was added to J774A.1 macrophages and incubated for 4 h at 37°C. The percent viability was determined with MTT.
Of 43 MAbs tested for their ability to neutralize at an LeTx concentration of LC50 (13 Freund and 30 CpG), 29 were found to increase LeTx-mediated killing in J774A.1 cells. Twenty-one of these were of IgG2a subclass (0 Freund and 21 CpG), and eight were IgG1 (7 Freund and 1 CpG). Interestingly, in the RAW 264.7 cell line, all 21 of the IgG2a MAbs mentioned above were observed to increase killing, whereas none of the IgG1 MAbs were able to cause an increase in killing. A similar finding was reported for antibody-dependent enhancement of feline infectious peritonitis virus infection of feline macrophages in which IgG2a MAbs but not IgG1 MAbs enhanced FIPV infection (15). MAb 3F3 (mouse IgG1) (25) and MAb 2A2 (mouse IgG2a) were chosen for further analysis. Some of the studies were restricted to MAb 3F3 since only limited quantities of MAb 2A2 were available due to poor immunoglobulin production by the hybridoma cell line. We did not observe significant killing of human macrophage cell lines U937 and THP-1 and murine macrophage cell line P388D1, even at very high doses of LeTx (up to 1 μg of PA and LF/ml incubated with cells for up to 48 h [data not shown]), with or without MAb 3F3.
Role of Fc in enhancement of LeTx-mediated killing.
We speculated that one of the possibilities for the observed MAb-mediated increase in LeTx cytotoxicity was the interaction of Fc of the MAb with Fc receptors on the cell surface, as has been shown to be the case with MAb-induced enhancement of viral particle internalization (39). To test this possibility, we designed experiments to eliminate the Fc region of the MAbs or block the Fc receptors on J774A.1 and RAW 264.7 macrophage cell lines with (i) MAb 3F3 (IgG1) Fabs that lacked the Fc, (ii) MAb 2.4G2 (anti-FcγRII/FcγRIII) to block Fc receptors on the macrophage surfaces, and (iii) protein A to block the Fc from interacting with the Fc receptors on the cell surface (15).
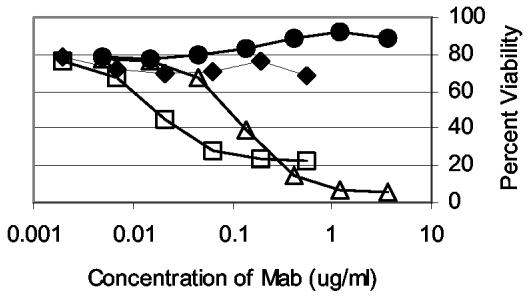
The modified LeTx cytotoxicity assay (LeTx concentration = LC50) was performed with MAb 3F3, 3F3 Fabs, and MAb 14B7. Fab fragments from MAb 3F3 neutralized cytotoxic activity (Fig. 2), whereas MAb 3F3 enhanced cytotoxic activity. This result suggests that the Fc of the MAb was involved in the increase in LeTx activity. MAb 14B7 neutralized toxin as previously shown.
FIG. 2.
Comparison of MAb versus Fab in modulating LeTx activity. The viability of J774A.1 cells incubated with increasing amounts of anti-PA MAb 3F3 (□), MAb 14B7 (⧫), and 3F3 Fabs (▵), along with LeTx at a concentration of LC50 (PA at 30 ng/ml, LF at 30 ng/ml), was determined. The MAb (or Fab)-LeTx mixture was added to J774A.1 macrophages and incubated for 4 h at 37°C. The percent viability was determined with MTT.
To further investigate the role of Fc interaction with its cell surface receptors, MAb 2.4G2 was used to block the Fc receptors on the macrophage. This MAb is known to block FcγRII and FcγRIII via its Fab region and binds to FcγRI via its Fc portion (40), but it does not completely inhibit interaction of mouse IgG2a with FcγRI (35). Both J774A.1 and RAW 264.7 cells were used for these experiments. MAb 2.4G2 completely prevented the enhancement of LeTx-mediated killing in the presence of MAbs 2A2 and 3F3 in J774A.1 cells (Fig. 3). In the case of RAW 264.7 cells, however, MAb 2.4G2 was observed to have no effect (data not shown).
FIG. 3.
Effect of blocking Fc receptors on macrophages with MAb 2.4G2 on enhancement of LeTx activity. A toxin neutralization assay in J774A.1 macrophages with anti-PA MAb 2A2 with (♦) or without (□) preincubation of cells with MAb 2.4G2 or with anti-PA MAb 3F3 with (•) or without (▵) preincubation of cells with MAb 2.4G2 was carried out. LeTx was incubated with MAb 2A2 or 3F3 at various concentrations. Macrophages were preincubated with MAb 2.4G2 at 0.5 μg/ml prior to addition of the above reaction mixture. The macrophages were incubated with the MAb-LeTx mixture for 4 h at 37°C. The percent viability was determined with MTT.
Irrelevant mouse IgG2a used at a very high concentration (100 μg/ml) complexed with its cognate antigen was also unable to prevent enhancement of killing in RAW 264.7 cell line, perhaps because all Fc receptors were not blocked (data not shown). Since MAb 2A2 has γ2a heavy chains, which have high affinity for FcγRI (16, 43), the enhancement in RAW 264.7 cells may be FcRγI dependent. Since enhancement in J774A.1 cells was blocked by MAb 2.4G2 (Fig. 3), it can be concluded that it was not entirely FcγRI mediated. In an attempt to block Fc interaction with all three FcγRs, we incubated the MAbs with protein A at a high concentration (50 μg/ml) prior to the addition to the RAW 264.7 macrophages, as previously reported with viral studies (15). However, this had no effect on the MAbs' ability to interact with Fc receptors, as determined by flow cytometry (data not shown), and did not lead to the elimination of enhancement of LeTx-mediated killing, consistent with previous reports on incomplete blocking by others (15). This may be due to the fact that FcγRI and FcγRIIa receptors bind to a region in the mouse IgG2a Fc that is distinct from that recognized by protein A (44).
Effect of blocking PA-receptor binding on MAb-mediated enhancement.
To determine whether PA-receptor binding was critical for the observed enhancement, we incubated PA in the presence of MAb 14B7 and MAb 2A2 or 3F3. Previous studies showed that 14B7 blocks receptor binding by PA (25, 34) and recognizes a different epitope on PA compared to MAb 3F3 (25). PA was incubated with 14B7 (at 1.5 μg/ml) and 3F3 or 2A2 (at 1.5 μg/ml) for 1 h prior to addition to macrophages in the presence of LF. Figure 4 shows the effect of blocking receptor binding by 14B7 on the enhancement of cytotoxicity caused by 3F3 and 2A2 in the presence of LeTx. As can be noted, blocking receptor binding by 14B7 reverses the enhancement caused by both enhancing MAbs. These results show the importance of PA-receptor binding in effecting the observed enhancement of LeTx cytotoxicity.
FIG. 4.
Effect of blocking PA-receptor binding on enhancement of LeTx-mediated killing by MAbs 2A2 and 3F3. PA was incubated with a mixture of MAbs 14B7 and 2A2 (both at 1.5 μg/ml) or a mixture of MAbs 14B7 and 3F3 (both at 1.5 μg/ml) for 1 h at 37°C. The mixture was added to macrophages, along with LF, followed by incubation for 4 h at 37°C. The percent viability was determined with MTT.
Effect of anti-PA MAb on binding of PA to the cell surface.
To determine the total amount of PA associated with the macrophages (surface associated plus endocytosed), Western blot analysis was performed on lysates of RAW 264.7 cells that had been incubated for various lengths of time with PA and MAb 2A2. Two bands were observed in the Western blot between 90 and 55 kDa based on molecular mass markers (Fig. 5, top) and represent whole PA and PA63. At all of the time points evaluated, the bands were darker when PA was incubated in the presence of MAb 2A2. There was an ∼2-fold increase in cell-associated PA/PA63 in the presence of the MAb 2A2 with PA compared to PA alone, as determined by densitometry (Fig. 5). Based on these results, we conclude that, in the presence of the anti-PA MAb, there is an increase in the amount of PA recruited to the cell.
FIG. 5.
Effect of MAb 2A2 on PA binding and internalization in macrophages. Densitometry was performed on a Western blot (shown at the top of the figure) for immunodetection of PA and PA63 in RAW 264.7 cell lysates after incubation with PA ± MAb 2A2. Lane 1, PA at 10 min; lane 2, PA at 30 min; lane 3, PA at 60 min; lane 4, PA plus MAb 2A2 at 10 min; lane 5, PA plus MAb 2A2 at 30 min; lane 6, PA plus MAb 2A2 at 60 min.
Effect of lysosomotropic agents on LeTx cytotoxicity in the presence or absence of MAb.
To begin to investigate whether there was a difference in the intracellular trafficking of LeTx in the presence or absence of the anti-PA MAb, we used lysosomotropic agents that have been shown to eliminate LeTx-mediated cytotoxicity (8). A lysosomotropic amine, NH4Cl, as well as an ionophore, monensin, eliminated the cell killing ability of LeTx even in the presence of anti-PA MAb 2A2 (Fig. 6) in RAW 264.7 cells. Similar results were obtained when J774A.1 cells were used with either MAb 2A2 or MAb 3F3 (data not shown). These results support the model that LeTx traffics through intracellular compartments that require acidification for the LeTx to be effective in the presence of MAbs.
FIG. 6.
Effect of lysosomotropic agents on LeTx mediated killing in the presence of enhancing MAb 2A2. LeTx at 100 ng/ml was mixed with MAb 2A2 at 2 μg/ml or medium, and the reaction mixture was added to RAW 264.7 cells, along with either medium (░⃞), monensin at 1.25 μg/ml (□), or NH4Cl at 125 μg/ml (▪). After a 4-h incubation, the percent viability was determined by using flow cytometry after the cells were stained with PI.
Cleavage of MAPKKs or MEKs by LeTx in the presence of the anti-PA MAbs.
Once LF is internalized, it acts as a zinc metalloprotease and is responsible for the cleavage of MEKs (1, 5, 41). To determine whether LF internalized in the presence of the anti-PA MAb led to MEK cleavage, the amount of MEK-1 found in lysates of cells after various treatments was measured by Western blot analysis. The band representing MEK-1 was weaker in lysates from J774A.1 cells incubated in the presence of LeTx and anti-PA MAb 3F3 than it was in lysates from cells incubated in the presence of LeTx alone (Fig. 7, top, lanes 5 and 3). Also, incubation of the cells with MAb 2.4G2 prior to the addition of the MAb-LeTx mixture led to an increase in the intensity of the MEK-1 band (Fig. 7, top, lane 6), indicating a decrease in MEK-1 cleavage when FcγR was blocked. Viability was measured on the same cell samples by using flow cytometry. The decrease in MEK-1 coincided with a decrease in cell viability (Fig. 7). Experiments done with anti-PA MAb 2A2 with RAW 264.7 cells yielded similar results (data not shown). These results show that anti-PA MAb in the presence of LeTx led to additional MEK-1 cleavage that correlated with an increase in cell killing.
FIG. 7.
Effect of MAb 3F3 on MEK cleavage and viability in the presence of LeTx. The viability of J774A.1 cells with various treatments was determined. A Western blot for the immunodetection of MEK in J774A.1 cell lysates after incubation for 4 h with no toxin (lane 1), MAb 2.4G2 (lane 2), LeTx only (lane 3), MAb 2.4G2 with LeTx (lane 4), LeTx plus MAb 3F3 (lane 5), or LeTx plus MAb 3F3 plus MAb 2.4G2 (lane 6) is shown at the top of the figure.
Increased cytotoxicity in FcγRI-transfected CHO cells.
The anthrax PA receptors are ubiquitously expressed (3, 6, 26). CHO cells, which are epithelial cell-like cells, are slightly sensitive to LeTx (Fig. 8). They do not express FcγR under normal culture conditions. A CHO cell line expressing the human FcγRI has been created (4). To determine whether the MAbs described above were able to increase killing in FcγR-negative cells, experiments were performed with this cell line and CHO cells. The anti-PA MAbs 3F3 and 2A2 did not cause any increase in killing of parental CHO cells in the presence of LeTx. However, when mRG1-1 cells (CHO cells transfected with only the binding portion of mouse FcγRI) were used, an increase in killing by ca. 20% in the presence of anti-PA MAb 2A2 and LeTx compared to LeTx alone was observed (Fig. 8). This increase was statistically significant (P = 0.015).
FIG. 8.
Toxin neutralization assay using a CHO cell line and mRG1-1 cell line (CHO/FcγRI) with MAb 2A2. LeTx was incubated with MAb 2A2, followed by the addition of the mixture to mRG1-1 cells (▪) or CHO cells (□). After a 48-h incubation at 37°C, the percent viability was determined with MTT.
DISCUSSION
We report here that certain antibodies generated against PA, the cell-binding component of the two-component anthrax LeTx, are capable of increasing the cellular cytotoxicity caused by LeTx. Antibody-mediated enhancement of viral infection of cells is well known (39), but no previous reports of a similar phenomenon with a protein toxin have been published. We tested MAbs from mice immunized with PA, and a significant subset of MAbs that were identified as high affinity were found to enhance LeTx-mediated killing of J774A.1 (29 of 43 overall [67%]) and RAW 264.7 (21 of 43 overall [49%]) murine macrophages. Another murine macrophage cell line, P388D1, and human macrophage cell lines U937 and THP-1 were found to be insensitive to LeTx, and none of the anti-PA MAbs were able to effect LeTx mediated cytotoxicity in these cells.
We tested the hypothesis that MAb enhancement of LeTx cytotoxicity is mediated by Fc receptors. Enhancement of host cell infection by anti-virus MAbs, for example, is mediated by interaction of MAb Fc with its receptors on the surface of the host cell (39). Fabs generated from an enhancing MAb (3F3, mouse IgG1) no longer enhanced cytotoxicity but neutralized toxin activity (Fig. 2), suggesting a role for the Fc portion of the MAb. Blocking FcγRs on the macrophage with a MAb (MAb 2.4G2) also eliminated MAb 3F3-mediated enhancement of LeTx cytotoxicity in the J774A.1 cell line (Fig. 3). The fact that Fabs were unable to cause any enhancement shows that binding to its cognate antigen was necessary but not sufficient for the observed enhancement, thereby ruling out the possibility of other mechanisms such as inhibition of proteolysis of PA at the macrophage cell surface. It remains unclear why the Fab fragment neutralized the LeTx, whereas MAb 3F3 in the presence of MAb 2.4G2 did not neutralize the LeTx. One possibility is that MAb 2.4G2 may not completely block Fc receptors (35, 40). Thus, any neutralization caused by binding of PA by MAb 3F3 may have been offset by enhancement effected via available FcRs. One way in which interaction of the Fc portion of a LeTx enhancing MAb with FcγR on the macrophage surface might mediate increased cell killing is by helping to stabilize the PA on the cell surface, thereby increasing the PA bound to the cell. This would lead to additional internalization of LF into the cell. Western blot results indicate that the MAbs indeed increased the amount of PA and activated PA (PA63) that was bound and/or internalized by macrophages (Fig. 5). Blocking of PA from binding its receptor prevented increased cytotoxicity by the anti-PA MAbs, suggesting the importance of this step in the enhancement phenomenon (Fig. 4). The dual interaction of PA with its receptor and the MAb may lead to stabilization of the PA on the surface, thereby decreasing the off-rate of the PA bound to the cell surface. A model for the proposed mode of stabilization is shown in Fig. 9. The observed increase in killing in the presence of the anti-PA MAbs correlates with levels of MAPKKs or MEKs in the cells (Fig. 7). Our results indicate greater cleavage of MEK in the presence of LeTx and enhancing MAb compared to LeTx alone. Our data also suggest that trafficking of the toxin in the presence of the MAbs is similar to that reported in the literature for LeTx alone (8). Lysosomotropic agents were able to completely eliminate LeTx-mediated killing irrespective of the presence or absence of enhancing MAb (Fig. 6).
FIG. 9.
Proposed model for stabilization of PA on the cell surface.
The enhancement of LeTx-mediated killing was observed in LeTx-sensitive cell lines that express Fc binding receptors on their cell surface. We also found that in mRG1-1 cells, which are CHO cells that express only the Fc binding portion of mouse FcγRI molecule (4), there was enhancement of LeTx-mediated killing in the presence of anti-PA MAb 2A2 (mouse IgG2a) (Fig. 8). This result suggests that the cytoplasmic effector domain of the FcγR was not required, and only Fc binding and physical stabilization of PA-MAb complexes was needed for the observed enhancement.
The reported enhancement of LeTx-mediated killing by MAbs may not be limited to murine macrophages. The role of macrophages in the pathophysiology of anthrax in mice and other animals is not entirely clear. Additional LeTx-sensitive cell types may exist. Some of these may also express Fc receptors on the cell surface, particularly in the presence of bacterial cell wall products and cytokines, as would be the case during infection with B. anthracis (10, 11, 12, 30). A recent report has shown that LeTx induces apoptosis in human umbilical vein endothelial cells (17). Although human umbilical vein endothelial cells do not express Fc receptors, other endothelial cells are known to express these receptors (9). LeTx has been shown to severely impair dendritic cell function (1), and dendritic cells are known to express FcγRs (33, 45). Anti-PA MAbs similar to the ones described here may be able to enhance LeTx-mediated killing in cell types that are LeTx sensitive and express Fc receptors such as the ones described above.
Although the results from the current study are not predictive of the situation in vivo, several studies have recently shown the occurrence of antibody-dependent enhancement of virus infection in vivo. The presence of enhancing antibodies has been demonstrated in serum samples of humans infected with the Ebola virus (37). A recent publication demonstrated that passive immunization of mice with subneutralizing concentrations of Japanese encephalitis virus antiserum, followed by challenge with wild-type Murray Valley encephalitis virus, resulted in an increase in viremia titers and mortality (42). Enhancement of West Nile virus infection of mice by a subneutralizing dose of a MAb has also been observed (Peter Mason, unpublished data).
One significant implication of our findings is that in a polyclonal response to PA there may be a prevalence of enhancing antibodies, which may result in a decrease in the neutralizing capability of polyclonal antibodies. This may be the case with immune responses elicited against a PA-based vaccine. The proportion of neutralizing and enhancing antibodies could depend on a variety of factors, including genetic predisposition of the immunized host, type of adjuvant, and administered dose of vaccine. It is possible that some individuals may even develop more enhancing antibodies than neutralizing antibodies. It is unclear from our study whether the use of adjuvants alters the prevalence of enhancing antibodies. That immunization can induce generation of enhancing antibodies was demonstrated by a previous study. DNA immunization of mice with a plasmid encoding the surface glycoprotein of the Zaire strain of Ebola virus enhanced the infectivity of vesicular stomatitis virus pseudotyped with the Ebola glycoprotein (38).
Another implication of our study is that it is possible that certain epitopes on PA are responsible for the generation of enhancing MAbs. Studies with the Ebola virus have shown that distinct epitopes are responsible for the generation of neutralizing and enhancing antibodies (38). Some of the MAbs described in the present study are known to bind the same antigenic determinant on PA, as shown by competitive enzyme-linked immunosorbent assay (25). One can speculate that a subunit vaccine that does not contain epitopes that lead to generation of enhancing MAbs might be a better alternative to a vaccine that is based upon whole PA. Further in vitro and in vivo studies need to be carried out to completely understand the significance of these cytotoxicity enhancing anti-PA antibodies and their involvement, if any, in the pathophysiology of disease that might develop in vaccinated individuals.
Acknowledgments
This study was funded by the U.S. Army Medical Research and Material Command (grant DAMD-02-1-0701) and by Elusys Therapeutics, Inc.
We thank William M. Sutherland, University of Virginia, for the gift of anti-PA MAb 2A2, and Stephen H. Leppla (National Institutes of Health) for the gifts of the 14B7 hybridoma cell line and the anti-PA rabbit polyclonal antibodies. We also thank Daniel H. Conrad, Virginia Commonwealth University, for the mRG1-1 cell line and Steven Pincus and Steven Jones, Elusys Therapeutics, Inc., for helpful discussions.
Editor: J. T. Barbieri
REFERENCES
- 1.Agrawal, A., J. Lingappa, S. H. Leppla, S. Agrawal, A. Jabbar, C. Quinn, and B. Pulendran. 2003. Impairment of dendritic cells and adaptive immunity by anthrax lethal toxin. Nature 424:329-334. [DOI] [PubMed] [Google Scholar]
- 2.Beall, F. A., M. J. Taylor, and C. B. Thorne. 1962. Rapid lethal effect in rats of a third component found upon fractionating the toxin of Bacillus anthracis. J. Bacteriol. 83:1274-1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradley, K. A., J. Mogridge, M. Mourez, R. J. Collier, and J. A. Young. 2001. Identification of the cellular receptor for anthrax toxin. Nature 414:225-229. [DOI] [PubMed] [Google Scholar]
- 4.Cho, S., and D. H. Conrad. 1997. A new multivalent B-cell activation model—anti-IgD bound to Fc gamma RI: properties and comparison with CD40L-mediated activation. Int. Immunol. 9:239-248. [DOI] [PubMed] [Google Scholar]
- 5.Duesbery, N. S., C. P. Webb, S. H. Leppla, V. M. Gordon, K. R. Klimpel, T. D. Copeland, N. G. Ahn, M. K. Oskarsson, K. Fukasawa, K. D. Paull, and G. F. Vande Woude. 1998. Proteolytic inactivation of MAP-kinase-kinase by anthrax lethal factor. Science 280:734-737. [DOI] [PubMed] [Google Scholar]
- 6.Escuyer, V., and R. J. Collier. 1991. Anthrax protective antigen interacts with a specific receptor on the surface of CHO-K1 cells. Infect. Immun. 59:3381-3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farchaus, J. W., W. J. Ribot, S. Jendrek, and S. F. Little. 1998. Fermentation, purification, and characterization of protective antigen from a recombinant, avirulent strain of Bacillus anthracis. Appl. Environ. Microbiol. 64:982-991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friedlander, A. M. 1986. Macrophages are sensitive to anthrax lethal toxin through an acid-dependent process. J. Biol. Chem. 261:7123-7124. [PubMed] [Google Scholar]
- 9.Groger, M., G. Sarmay, E. Fiebiger, K. Wolff, and P. Petzelbauer. 1996. Dermal microvascular endothelial cells express CD32 receptors in vivo and in vitro. J. Immunol. 156:1549-1556. [PubMed] [Google Scholar]
- 10.Hammond, S. E., and P. C. Hanna. 1998. Lethal factor active-site mutations affect catalytic activity in vitro. Infect. Immun. 66:2374-2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hanna, P. C., B. A. Kruskal, R. A. Ezekowitz, B. R. Bloom, and R. J. Collier. 1994. Role of macrophage oxidative burst in the action of anthrax lethal toxin. Mol. Med. 1:7-18. [PMC free article] [PubMed] [Google Scholar]
- 12.Hanna, P. C., D. Acosta, and R. J. Collier. 1993. On the role of macrophages in anthrax. Proc. Natl. Acad. Sci. USA 90:10198-10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanna, P. C., S. Kochi, and R. J. Collier. 1992. Biochemical and physiological changes induced by anthrax lethal toxin in J774 macrophage-like cells. Mol. Biol. Cell 3:1269-1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen, M. B., S. E. Nielsen, and K. Berg. 1989. Re-examination and further development of a precise and rapid dye method for measuring cell growth/cell kill. J. Immunol. Methods 119:203-210. [DOI] [PubMed] [Google Scholar]
- 15.Hohdatsu, T., J. Tokunaga, and H. Koyama. 1994. The role of IgG subclass of mouse monoclonal antibodies in antibody-dependent enhancement of feline infectious peritonitis virus infection of feline macrophages. Arch. Virol. 139:273-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kimberly R. P., J. E. Salmon, and J. C. Edberg. 1995. Receptors for immunoglobulin G: molecular diversity and implications for disease. Arthritis Rheum. 38:306-314. [DOI] [PubMed] [Google Scholar]
- 17.Kirby, J. E. 2004. Anthrax lethal toxin induces human endothelial cell apoptosis. Infect. Immun. 72:430-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klimpel, K. R., N. Arora, and S. H. Leppla. 1994. Anthrax toxin lethal factor contains a zinc metalloprotease consensus sequence which is required for lethal toxin activity. Mol. Microbiol. 13:1093-1100. [DOI] [PubMed] [Google Scholar]
- 19.Klimpel, K. R., S. S. Molloy, G. Thomas, and S. H. Leppla. 1992. Anthrax toxin protective antigen is activated by a cell surface protease with the sequence specificity and catalytic properties of furin. Proc. Natl. Acad. Sci. USA 89:10277-10281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leppla, S. H. 1982. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclic AMP concentrations of eukaryotic cells. Proc. Natl. Acad. Sci. USA 79:3162-3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leppla, S. H. 1984. Bacillus anthracis calmodulin-dependent adenylate cyclase: chemical and enzymatic properties and interactions with eucaryotic cells. Adv. Cyclic Nucleotide Protein Phosphorylation Res. 17:189-198. [PubMed] [Google Scholar]
- 22.Leppla, S. H. 1988. Production and purification of anthrax toxin. Methods Enzymol. 165:103-116. [DOI] [PubMed] [Google Scholar]
- 23.Leppla, S. H., A. M. Friedlander, and E. M. Cora. 1988. Proteolytic activation of anthrax toxin bound to cellular receptors, p. 111-112. In F. J. Fehenbach, J. E. Alouf, P. Falmagne, W. Goebel, J. Jeljaszewicz, D. Jurgens, and R. Rappuoli, (ed.), Bacterial protein toxins. Gustav Fischer, New York, N.Y.
- 24.Little, S. F., S. H. Leppla, and A. M. Friedlander. 1990. Production and characterization of monoclonal antibodies against the lethal factor component of Bacillus anthracis lethal toxin. Infect. Immun. 58:1606-1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Little, S. F., S. H. Leppla, and E. Cora. 1988. Production and characterization of monoclonal antibodies to the protective antigen component of Bacillus anthracis toxin. Infect. Immun. 56:1807-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu, S., S. H. Leppla. 2003. Cell surface tumor endothelium marker 8 cytoplasmic tail-independent anthrax toxin binding, proteolytic processing, oligomer formation, and internalization. J. Biol. Chem. 278:5227-5234. [DOI] [PubMed] [Google Scholar]
- 27.Milne, J. C., D. Furlong, P. C. Hanna, J. S. Wall, and R. J. Collier. 1994. Anthrax protective antigen forms oligomers during intoxication of mammalian cells. J. Biol. Chem. 269:20607-20612. [PubMed] [Google Scholar]
- 28.Milne, J. C., S. R. Blanke, P. C. Hanna, and R. J. Collier. 1995. Protective antigen-binding domain of anthrax lethal factor mediates translocation of a heterologous protein fused to its amino- or carboxy terminus. Mol. Microbiol. 15:661-666. [DOI] [PubMed] [Google Scholar]
- 29.Mock, M., and A. Fouet. 2001. Anthrax. Annu. Rev. Microbiol. 55:647-671. [DOI] [PubMed] [Google Scholar]
- 30.Park, J. M., F. R. Greten, Z. W. Li, and M. Karin. 2002. Macrophage apoptosis by anthrax lethal factor through p38 MAP kinase inhibition. Science 297:2048-2051. [DOI] [PubMed] [Google Scholar]
- 31.Petosa, C., R. J. Collier, K. R. Klimpel, S. H. Leppla, and R. C. Liddington. 1997. Crystal structure of the anthrax toxin protective antigen. Nature 385:833-838. [DOI] [PubMed] [Google Scholar]
- 32.Pezard, C., P. Berche, and M. Mock. 1991. Contribution of individual toxin components to virulence of Bacillus anthracis. Infect. Immun. 59:3472-3477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qin, D., J. Wu, K. A. Vora, J. V. Ravetch, A. K. Szakal, T. Manser, and J. G. Tew. 2000. Fc gamma receptor IIB on follicular dendritic cells regulates the B-cell recall response. J. Immunol. 164:6268-6275. [DOI] [PubMed] [Google Scholar]
- 34.Rosovitz, M. J., P. Schuck, M. Varughese, A. P. Chopra, V. Mehra, Y. Singh, L. M. McGinnis, and S. H. Leppla. 2003. Alanine scanning mutations in domain 4 of anthrax toxin protective antigen reveal residues important for binding to the cellular receptor and to a neutralizing monoclonal antibody. J. Biol. Chem. 278:30936-30944. [DOI] [PubMed] [Google Scholar]
- 35.Smith, K. G., J. M. Austyn, G. Hariri, P. C. Beverley, and P. J. Morris. 1986. T-cell activation by anti-T3 antibodies: comparison of IgG1 and IgG2b switch variants and direct evidence for accessory function of macrophage Fc receptors. Eur. J. Immunol. 16:478-486. [DOI] [PubMed] [Google Scholar]
- 36.Stanley, J. L., and H. Smith. 1961. Purification of factor I and recognition of a third factor of the anthrax toxin. J. Gen. Microbiol. 26:49-66. [DOI] [PubMed] [Google Scholar]
- 37.Takada, A., H. Feldman, T. G. Ksiazek, and Y. Kawaoka. 2003. Antibody-dependent enhancement of Ebola virus infection. J. Virol. 77:7539-7544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Takada, A., S. Watanabe, K. Okazaki, H. Kida, and Y. Kawaoka. 2001. Infectivity-enhancing antibodies to Ebola virus glycoprotein. J. Virol. 75:2324-2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tirado, S. M., and K. L. Yoon. 2003. Antibody-dependent enhancement of virus infection and disease. Viral Immunol. 16:69-86. [DOI] [PubMed] [Google Scholar]
- 40.Unkeless, J. C. 1979. Characterization of a monoclonal antibody directed against mouse macrophage and lymphocyte Fc receptors. J. Exp. Med. 150:580-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vitale, G., R. Pellizzari, C. Recchi, G. Napolitani, M. Mock, and C. Montecucco. 1999. Anthrax lethal factor cleaves the N terminus of MAPKKs and induces tyrosine/threonine phosphorylation of MAPKs in cultured macrophages. J. Appl. Microbiol. 87:288. [DOI] [PubMed] [Google Scholar]
- 42.Wallace, M. J., D. W. Smith, A. K. Broom, J. S. Mackenzie, R. A. Hall, G. R. Shellam, and P. C. McMinn. 2003. Antibody-dependent enhancement of Murray Valley encephalitis virus virulence in mice. J. Gen. Virol. 84:1723-1728. [DOI] [PubMed] [Google Scholar]
- 43.Wallace, P. K., F. H. Valone, and M. W. Fabger. 1995. Myeloid cell-targeted cytotoxicity of tumor cells, p. 43. In M. W. Fanger (ed.), Bispecific antibodies. R. G. Landis Co. Austin, Tex.
- 44.Wines, B. D., M. S. Powell, P. W. Parren, N. Barnes, and P. M. Hogarth. 2000. The IgG Fc contains distinct Fc receptor (FcR) binding sites: the leukocyte receptors FcγRI and FcγRIIa bind to a region in the Fc distinct from that recognized by neonatal FcR and protein A. J. Immunol. 164:5313-5318. [DOI] [PubMed] [Google Scholar]
- 45.Zhu, X., G. Meng, B. L. Dickinson, X. Li, E. Mizoguchi, L. Miao, Y. Wang, C. Robert, B. Wu, P. D. Smith, W. I. Lencer, and R. S. Blumberg. 2001. MHC class I-related neonatal Fc receptor for IgG is functionally expressed in monocytes, intestinal macrophages, and dendritic cells. J. Immuno1. 66:3266-3276. [DOI] [PMC free article] [PubMed] [Google Scholar]