Abstract
A Salmonella enterica serovar Typhimurium aroA-deficient delivery system was used to target the immunosuppressive protein Salp15 to antigen-presenting cells. In vitro and in vivo infections with Salp15-containing Salmonella resulted in an impaired CD4+-T-cell activation, suggesting that the protein was produced by antigen-presenting cells in a physiologically active form.
Immunosuppressive drugs are essential for the success of allogeneic transplantations. Drugs such as cyclosporine, FK506, and rapamycin have been a mainstay in heart, liver, kidney, and bone marrow transplantation due to their profound immunosuppressive properties (4). These fungal metabolites block activation of naïve T cells by inhibiting the transcription of genes encoding interleukin 2 (IL-2) and the high-affinity IL-2 receptor alpha, which are essential for T-cell activation (10). Despite impressive results obtained with these drugs in transplants, negative side effects do arise due to their systemic administration (2, 11, 21, 22), suggesting the need for alternative approaches to define and use molecules that are specific to T cells and that are targeted to the sites in which T-cell priming occurs.
We have recently cloned and characterized an immunomodulatory protein present in Ixodes scapularis saliva, Salp15, which is the first I. scapularis protein known to be associated with the immunosuppressive activity of tick saliva (1). Salp15 has been shown to impair proliferative responses of anti-CD3- plus anti-CD28-activated CD4+ T cells by inhibition of T-cell-receptor-mediated calcium mobilization (1). Furthermore, Salp15 does not affect other immune cells, namely B or dendritic cells, making it a specific T-cell inhibitor (1). Salp15 can thus be utilized in a number of pathological scenarios requiring immunosuppression. Therefore, it is a very attractive candidate for use in immunotherapy, because it can possibly reduce the toxicity associated with drugs while maintaining an effective degree of immunosuppression if it is delivered to T-cell priming sites.
The capacity to deliver biomolecules such as Salp15 to specific tissues, cells, or cellular compartments remains elusive. One approach consists of the use of plasmid-vector systems that allow professional antigen-presenting cells (APC) to efficiently produce and present protein antigens by using virulence-attenuated bacteria (7). Attenuated mutants have been obtained predominantly from strains of Salmonella enterica serovar Typhimurium. Inactivation of a number of different genes highly attenuates Salmonella virulence. Such genes include aroA, htrA, cya, crp, and phoP (19, 20). Attenuated strains of Salmonella do not require an active immune response for the resolution of infection (15). They have been successfully used as live vectors in many experimental systems (18) without impairing antigen processing and presentation by APC (12).
Genes cloned under the control of a eukaryotic promoter and delivered through bacterial systems can be efficiently expressed by eukaryotic cells (6). We therefore cloned salp15 into the eukaryotic expression vector pIRES2-eGFP (BD Biosciences Clontech, Palo Alto, Calif.) to target expression of the immunosuppressant to infected cells. This plasmid contains an internal ribosome-binding site (IRES) that allows simultaneous expression of Salp15 and green fluorescent protein (GFP) from the same mRNA transcript. salp15 was amplified with primers Salp15F (5′-AAG AGC TCA TGG AAT CTT TCG TCG CAA T-3′) and Salp15B (5′-AAG GAT CCC TAA CAT CCG GGA ATG TG-3′) and subcloned into the vector after digestion with SacI and BamHI (underlined in the above primer sequences). The subcloned fragment contained the leader sequence present in the original clone (1) to allow the protein to be secreted. S. enterica serovar Typhimurium SL7207 strain 2337-65 [WRAY] derivative hisG46 del407 [5]) was the recipient of the recombinant pIRES-eGFP plasmid containing the salp15 gene.
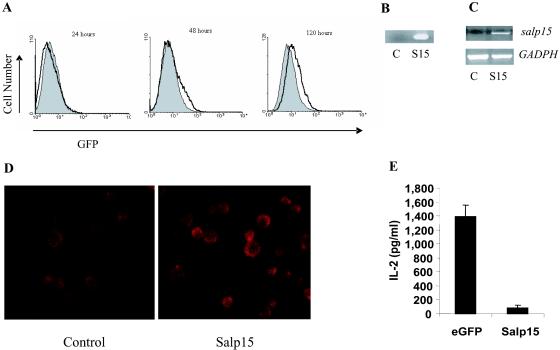
We infected MH-S cells (American Type Culture Collection, Manassas, Va.) with the salp15-containing Salmonella aroA mutant. Infected MH-S cells were assessed for enhanced GFP (eGFP) and Salp15 expression. eGFP was readily detected by flow cytometry 48 h postinfection, with increased expression that persisted for at least 120 h (Fig. 1A). Total RNA was extracted from 3 × 106 cells by using TRIZOL reagent (Gibco-BRL, Gaithersburg, Md.) and subjected to reverse transcription in the presence of random hexamers by using Superscript II reverse transcriptase (Invitrogen, Carlsbad, Calif.). PCR was performed with the primers and conditions described previously (1). PCR amplification of the glyceraldehyde-3-phosphate dehydrogenase housekeeping gene was performed with cDNA from each sample to ensure equal RNA input (1). DNA from infected MH-S cells was extracted with a QIAGEN (Valencia, Calif.) tissue kit, following the manufacturer's instructions. The PCR conditions used to amplify Salp15 were those described before (1). Infection of the macrophage cell line resulted in the presence of Salp15-encoding DNA (Fig. 1B) and salp15 gene transcripts (Fig. 1C) 5 days after infection. Infected MH-S cells were cytospun on slides and fixed in 3.7% formaldehyde for 30 min at room temperature. The cells were stained with polyclonal rabbit anti-Salp15 (1:100 dilution) (1), followed by a goat anti-rabbit immunoglobulin G (IgG) conjugated to Alexa Fluor 594 (1/1,000 dilution; Molecular Probes, Eugene, Oreg.), and examined with an Olympus Biological microscope equipped with a FLUOVIEW FV500 confocal laser scanning microscope system (Olympus, Melville, N.Y.). Confocal analysis of the infected cells demonstrated expression of Salp15 (Fig. 1D). These results indicated that delivery of the salp15 gene under a eukaryotic promoter results in expression of the Salp15 protein.
FIG. 1.
S. enterica serovar Typhimurium aroA mutant-based delivery of Salp15 in vitro. (A to D) MH-S cells were infected with mutant bacteria containing the salp15 gene (multiplicity of infection, 25) and analyzed after 5 days for eGFP expression (A), Salp15 DNA (B), and mRNA (C) by PCR and for Salp15 protein (D) by confocal microscopy. C, control; S15, Salp15. (E) Infected cells were also used as APC in an in vitro activation assay of splenic CD4+ T cells from BALB/c mice in response to 2.5 μg of concanavalin A/ml. At 40 h of activation, the supernatants were analyzed for IL-2 by ELISA. The data shown are from one of two experiments performed with similar results.
We next sought to determine whether Salp15 produced by infected MH-S cells was active in preventing CD4+-T-cell activation, as described for the recombinant protein (1). MH-S cells are an alveolar macrophage cell line that expresses major histocompatibility complex class II antigens on the surface (13) and, therefore, can be used as APC in in vitro T-cell activation assays. MH-S cells were seeded at 2.5 × 105 cells/well in a 24-well tissue culture plate and infected with cultures of S. enterica serovar Typhimurium containing the salp15 gene or the empty plasmid (eGFP) at a multiplicity of infection of 25. The mixture was incubated with the bacteria for 3 h to allow invasion and treated with 100 μg of gentamicin/ml to kill the remaining extracellular bacteria. Five days later, we used the cells as APC to activate CD4+ T cells purified by negative selection (1) from BALB/c mice (Charles River, Wilmington, Mass.) in the presence of 2.5 μg of concanavalin A/ml. At 40 h of incubation, the supernatants were analyzed for IL-2 by capture enzyme-linked immunosorbent assay (ELISA), as described previously (1). The Salp15-producing MH-S cells induced IL-2 production during CD4 T-cell activation that was impaired compared to that induced by the MH-S cells infected with Salmonella containing the empty plasmid, which were used as controls (Fig. 1E). Overall, our data indicated that in vitro delivery of the salp15 gene by aroA-deficient Salmonella results in the production of the protein and the suppression of CD4+-T-cell activation in vitro.
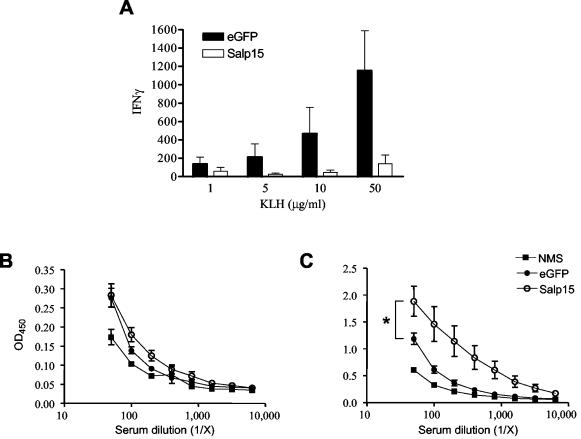
In order to assess whether the bacterium-based delivery system would target activating CD4+ T cells in vivo, we infected groups of BALB/c mice with Salmonella aroA mutant bacteria containing the salp15 gene or the empty plasmid (eGFP). Mice were infected intraperitoneally with 108 bacteria and 5 days later were immunized with 10 μg of keyhole limpet hemocyanin (KLH) in incomplete Freund's adjuvant. Oral administration of attenuated bacteria has been demonstrated to be the required route when mucosal immune responses are needed, such as for the delivery of vaccine candidates against mucosal pathogens (14). Both mucosal and parenteral administration of the carriers induce good systemic responses, however (16), so we delivered salp15-containing Salmonella by intraperitoneal injection to target T-cell priming sites. Ten days after immunization, KLH-specific CD4+-T-cell responses were assessed in in vitro restimulation assays using 106 purified CD11b+ CD11c+ cells from an uninfected control mouse as the APC. Splenic CD4+ T cells were purified by negative selection, as before, and restimulated in vitro with increasing concentrations of KLH. Supernatants were analyzed for gamma interferon (IFN-γ) and IL-4 at 40 h of incubation by capture ELISA. Control CD4+ T cells responded to the antigen in a dose-dependent manner (Fig. 2A). In contrast, CD4+ T cells from the mice infected with bacteria containing salp15 did not produce IFN-γ (Fig. 2A) or IL-4 (data not shown) in response to KLH. These data suggested that the Salmonella-delivered Salp15 inhibited the activation of T cells in vivo.
FIG. 2.
Salmonella aroA mutant-based delivery of Salp15 in vivo. BALB/c mice were infected with 108 salp15-containing S. enterica serovar Typhimurium aroA mutant bacteria or control bacteria with the empty plasmid (eGFP). Five days later, the mice were immunized with KLH in incomplete Freund's adjuvant. (A) The mice were analyzed for KLH-specific IFN-γ production by splenic CD4+ T cells in recall responses 10 days after immunization. (B and C) When the mice were sacrificed, KLH-specific IgM (B) and IgG (C) levels in the sera were also determined by ELISA. OD450, optical density at 450 nm; NMS, normal mouse serum; *, significant differences in results of the KLH-specific IgG titers between the Salp15 and eGFP groups, as determined by a two-way analysis of variance (P < 0.001). The data shown were obtained from four mice in two independent experiments.
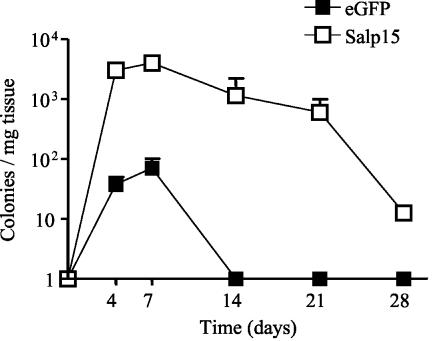
KLH-specific antibody titers in the sera of the infected, immunized mice were then determined by ELISA, as described previously (1). KLH-specific IgM responses were comparable for both groups of mice (Fig. 2B). However, salp15-containing Salmonella-infected mice developed a significantly increased IgG response to KLH compared to controls (two-way analysis of variance, P < 0.01) (Fig. 2C), suggesting that KLH-specific antibody responses had been affected by the immunosuppressive protein. This result is in striking contrast to the effect observed when the recombinant protein was used (1). Our results suggest that there is a T-cell-mediated modulatory action on B-cell activation in response to foreign antigens during Salmonella infection, since B cells are not affected by Salp15 (1). We hypothesize that this interaction is dependent on T-cell activation and, therefore, that its inhibition by Salp15 results in increased B-cell responses against the antigen. Alternatively, the inhibition of T-cell responses by Salp15 might impair the clearance of the bacteria and allow a persistent interaction with B cells. Indeed, B-cell mitogenic activities have been described in Salmonella spp. (9, 23, 24). In order to assess whether the presence of the gene encoding Salp15 in the aroA mutant resulted in an impaired ability to clear infection, we infected mice with SL7207 containing the salp15 gene or the empty plasmid (eGFP) and monitored infection over time by plating a small sample from the spleen on Luria-Bertani plates containing 50 μg of kanamycin/ml. Mice infected with the aroA mutant harboring the salp15 gene showed increased bacterial burdens in the spleen throughout the experiment, although the infection eventually abated (Fig. 3). This finding correlates with increased splenomegaly in these mice, resulting from a prominent infiltration of CD11b+ cells (data not shown). Our results agree with those of previous studies indicating increased mutant Salmonella burdens in mice that are unable to mount T-cell responses (17).
FIG. 3.
Salp15 increases the bacterial burden and delays resolution of infection with the S. enterica serovar Typhimurium aroA mutant. Mice were infected with 108 aroA-deficient bacteria harboring either the salp15 gene (Salp15) or the empty plasmid (eGFP). Bacterial burdens in the spleens of the infected animals were assessed over the course of infection by plating a section of the spleens in Luria-Bertani medium containing 50 μg of kanamycin/ml. The data represent numbers of CFU per milligram of tissue. The data at each time point represent the average of results for two mice.
The use of live bacterial carriers constitutes a powerful tool to achieve efficient delivery of DNA constructs (3, 8). There are several applications of this system, such as in immunotherapy and immunoprophylaxis of chronic processes (16). Many different attenuated mutants and expression systems have been tested for the transfer of eukaryotic expression plasmids into host cells. aroA-deficient strains of S. enterica serovar Typhimurium have been widely used for the delivery of antigenic polypeptides for vaccine purposes (20). However, this is the first instance to our knowledge in which this delivery system has been used to attempt to provide APC with immunomodulatory antigens.
Our results show that the delivery of Salp15 through the use of Salmonella mutants provides an efficient means to target activating CD4+ T cells. The use of a eukaryotic promoter ensures that the expression of the gene is restricted to phagocytic cells that are able to acquire the plasmid contained in the bacteria and express it. Thus, a limited expression of the antigen is ensured and permits the delivery of the protein to CD4+ T cells that are being activated. The data presented here also indicate that the delivery system provided a physiologically relevant form of the immunosuppressive protein. However, caution must be exercised in the use of live bacterial systems to deliver immunosuppressive antigens such as Salp15. The lack of T-cell-mediated responses results in increased bacterial burdens with prominent splenomegaly and delayed resolution of the infection. Our results indicate that the delivery of immunomodulatory molecules may require the use of noninfectious delivery methods to avoid unwanted secondary effects.
Acknowledgments
This work was supported by a Junior Faculty Research Program grant from the University of North Carolina at Charlotte and by NIH grant AI 053064 to J.A.
We thank B. A. D. Stocker for generously providing the S. enterica serovar Typhimurium aroA mutant used in these studies and Rafal Persinski for technical support.
Editor: F. C. Fang
REFERENCES
- 1.Anguita, J., N. Ramamoorthi, J. W. Hovius, S. Das, V. Thomas, R. Persinski, D. Conze, P. W. Askenase, M. Rincon, F. S. Kantor, and E. Fikrig. 2002. Salp15, an Ixodes scapularis salivary protein, inhibits CD4+ T cell activation. Immunity 16:849-859. [DOI] [PubMed] [Google Scholar]
- 2.Attur, M. G., R. Patel, G. Thakker, P. Vyas, D. Levartovsky, P. Patel, S. Naqvi, R. Raza, K. Patel, D. Abramson, G. Bruno, S. B. Abramson, and A. R. Amin. 2000. Differential anti-inflammatory effects of immunosuppressive drugs: cyclosporin, rapamycin and FK-506 on inducible nitric oxide synthase, nitric oxide, cyclooxygenase-2 and PGE2 production. Inflamm. Res. 49:20-26. [DOI] [PubMed] [Google Scholar]
- 3.Beyer, T., M. Herrmann, C. Reiser, W. Bertling, and J. Hess. 2001. Bacterial carriers and virus-like-particles as antigen delivery devices: role of dendritic cells in antigen presentation. Curr. Drug Targets Infect. Disord. 1:287-302. [DOI] [PubMed] [Google Scholar]
- 4.Burkhardt, H., and J. R. Kalden. 1997. Xenobiotic immunosuppressive agents: therapeutic effects in animal models of autoimmune diseases. Rheumatol. Int. 17:85-90. [DOI] [PubMed] [Google Scholar]
- 5.Chomczynski, P., and N. Sacchi. 1987. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal. Biochem. 162:156-159. [DOI] [PubMed] [Google Scholar]
- 6.Darji, A., S. zur Lage, A. I. Garbe, T. Chakraborty, and S. Weiss. 2000. Oral delivery of DNA vaccines using attenuated Salmonella typhimurium as carrier. FEMS Immunol. Med. Microbiol. 27:341-349. [DOI] [PubMed] [Google Scholar]
- 7.Gentschev, I., G. Dietrich, S. Spreng, A. Kolb-Maurer, J. Daniels, J. Hess, S. H. Kaufmann, and W. Goebel. 2000. Delivery of protein antigens and DNA by virulence-attenuated strains of Salmonella typhimurium and Listeria monocytogenes. J. Biotechnol. 83:19-26. [DOI] [PubMed] [Google Scholar]
- 8.Gentschev, I., G. Dietrich, S. Spreng, S. Pilgrim, J. Stritzker, A. Kolb-Maurer, and W. Goebel. 2002. Delivery of protein antigens and DNA by attenuated intracellular bacteria. Int. J. Med. Microbiol. 291:577-582. [DOI] [PubMed] [Google Scholar]
- 9.Johnson, R. B., S. Köhl, and W. G. Bessler. 1983. Polyclonal activation of B-lymphocytes in vivo by Salmonella typhimurium lipoprotein. Infect. Immun. 39:1481-1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kruger, M., M. Schwaninger, R. Blume, E. Oetjen, and W. Knepel. 1997. Inhibition of CREB- and cAMP response element-mediated gene transcription by the immunosuppressive drugs cyclosporin A and FK506 in T cells. Naunyn Schmiedeberg's Arch. Pharmacol. 356:433-440. [DOI] [PubMed] [Google Scholar]
- 11.Lindholm, A. 1991. Therapeutic monitoring of cyclosporin—an update. Eur. J. Clin. Pharmacol. 41:273-283. [DOI] [PubMed] [Google Scholar]
- 12.Lo-Man, R., J. P. Langeveld, E. Dériaud, M. Jehanno, M. Rojas, J.-M. Clément, R. H. Meloen, M. Hofnung, and C. Leclerc. 2000. Extending the CD4+ T-cell epitope specificity of the Th1 immune response to an antigen using a Salmonella enterica serovar Typhimurium delivery vehicle. Infect. Immun. 68:3079-3089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mbawuike, I. N., and H. B. Herscowitz. 1989. MH-S, a murine alveolar macrophage cell line: morphological, cytochemical, and functional characteristics. J. Leukoc. Biol. 46:119-127. [DOI] [PubMed] [Google Scholar]
- 14.McGhee, J. R., and H. Kiyono. 1992. Mucosal immunity to vaccines: current concepts for vaccine development and immune response analysis. Adv. Exp. Med. Biol. 327:3-12. [DOI] [PubMed] [Google Scholar]
- 15.McSorley, S. J., and M. K. Jenkins. 2000. Antibody is required for protection against virulent but not attenuated Salmonella enterica serovar Typhimurium. Infect. Immun. 68:3344-3348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Medina, E., and C. A. Guzman. 2001. Use of live bacterial vaccine vectors for antigen delivery: potential and limitations. Vaccine 19:1573-1580. [DOI] [PubMed] [Google Scholar]
- 17.Mittrucker, H. W., A. Kohler, T. W. Mak, and S. H. Kaufmann. 1999. Critical role of CD28 in protective immunity against Salmonella typhimurium. J. Immunol. 163:6769-6776. [PubMed] [Google Scholar]
- 18.Paglia, P., E. Medina, I. Arioli, C. A. Guzman, and M. P. Colombo. 1998. Gene transfer in dendritic cells, induced by oral DNA vaccination with Salmonella typhimurium, results in protective immunity against a murine fibrosarcoma. Blood 92:3172-3176. [PubMed] [Google Scholar]
- 19.Roberts, M., S. Chatfield, D. Pickard, J. Li, and A. Bacon. 2000. Comparison of abilities of Salmonella enterica serovar Typhimurium aroA aroD and aroA htrA mutants to act as live vectors. Infect. Immun. 68:6041-6043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stocker, B. A. 2000. Aromatic-dependent Salmonella as anti-bacterial vaccines and as presenters of heterologous antigens or of DNA encoding them. J. Biotechnol. 83:45-50. [DOI] [PubMed] [Google Scholar]
- 21.Trevillyan, J. M., X. G. Chiou, Y. W. Chen, S. J. Ballaron, M. P. Sheets, M. L. Smith, P. E. Wiedeman, U. Warrior, J. Wilkins, E. J. Gubbins, G. D. Gagne, J. Fagerland, G. W. Carter, J. R. Luly, K. W. Mollison, and S. W. Djuric. 2001. Potent inhibition of NFAT activation and T cell cytokine production by novel low molecular weight pyrazole compounds. J. Biol. Chem. 276:48118-48126. [DOI] [PubMed] [Google Scholar]
- 22.Unsal, M., R. Gurunluoglu, O. Babuccu, K. Carnevale, and M. Siemionow. 2002. Effect of long-term cyclosporine administration on muscle flap hemodynamics. Ann. Plast. Surg. 48:305-311. [DOI] [PubMed] [Google Scholar]
- 23.Vordermeier, H. M., and W. G. Bessler. 1987. Polyclonal activation of murine B lymphocytes in vitro by Salmonella typhimurium porins. Immunobiology 175:245-251. [DOI] [PubMed] [Google Scholar]
- 24.Vordermeier, H. M., H. Drexler, and W. G. Bessler. 1987. Polyclonal activation of human peripheral blood lymphocytes by bacterial porins and defined porin fragments. Immunol. Lett. 15:121-126. [DOI] [PubMed] [Google Scholar]