Abstract
Background
Objective, subjective, and neighborhood socioeconomic status (SES) are associated with perceived health, morbidity, and mortality.
Purpose
We investigated whether perceived stress and health behaviors mediated the relation between the three types of SES and perceived health.
Methods
Participants (N = 508) attending a public clinic completed a computerized survey assessing objective SES (income, education, employment); health behaviors; perceived stress; and perceived health. They also indicated their social standing relative to others (subjective SES) and provided their current address to determine neighborhood SES.
Results
In a structural equation model including all three SES types, lower objective and subjective SES were related to poorer perceived health. When mediators were included in the model, there were significant indirect effects of: (a) SES on health through stress; and (b) SES on health through stress and health compromising behaviors.
Conclusions
Interventions to reduce the impact of stressors could improve the health of socioeconomically disadvantaged individuals.
Keywords: socioeconomic status, health behaviors, stress, perceived health
Introduction
Socioeconomic disadvantage is associated with numerous health disparities, including cardiovascular disease, diabetes, cancer, and mortality [1]. The relation between socioeconomic status (SES) and health exists at all levels of SES [2, 3], although the relation is stronger for individuals at the lower end of the SES spectrum [4]. Despite advances in medical care and improved health overall, socioeconomic disparities in health have increased over the past several decades [5, 6].
The association between objective measures of individual-level SES (e.g., income, education, occupation) and health has been well-studied [7]. Other measures of SES, including neighborhood SES (e.g., percentage living in poverty, median family income, percentage with a college degree) and subjective SES (i.e., perception of one’s SES relative to others) are also related to health. Neighborhood SES is positively correlated with subjective health, physical functioning, and negatively related to early mortality [8–11]. Further, neighborhood SES is associated with various indicators of health (e.g., number and prevalence of chronic conditions, body mass index, self-rated health, early mortality) above and beyond individual- and family-level SES measures [8–15], indicating that neighborhood SES is not merely a proxy for objective SES, but that the neighborhood context affects health above and beyond objective SES. Subjective SES is also related to health outcomes, including physical functioning, perceived health, and susceptibility to the common cold, even after controlling for individual-level, objective measures of SES [16–19].
Thus, research has found that objective SES, neighborhood SES, and subjective SES are all associated with health. However, these three types of SES are correlated [8], making it difficult to disentangle the effects of each type of SES on health. One purpose of the current study is to better understand the unique influence of these different types of SES on perceived health.
Mediators of the Association between SES and Health
Although the relation between SES and health is well-established, why and how these variables are related remains unclear. Numerous explanations for how objective SES leads to poor health have been proposed, including differential access to healthcare, health-related knowledge, stressors, psychological distress, poor health behaviors, hazardous environments, social support availability, and personal resources and coping strategies [1–3, 20–22]. It has been suggested that low neighborhood SES may lead to poor health through violence, low levels of social capital and less supportive social networks, different norms for health behaviors, constraints on physical activity and food availability, limited access to medical care, stressful environmental conditions, and higher levels of pollution and toxins [3, 8, 22–29]. Subjective SES, which may represent a composite of several objective SES variables [16], may lead to poor health through the same mechanisms as objective SES. Alternatively, subjective SES may represent an individual’s appraisal of their standing in the social hierarchy; perceived position in the social hierarchy may influence health. Although numerous potential pathways through which SES may lead to poor health have been proposed, little research has tested potential mediators and, to our knowledge, no research has tested mediators of the SES-health relation while simultaneously considering objective, neighborhood, and subjective SES effects on health. Thus, a second purpose of the current study is to test two plausible pathways through which these three types of SES may influence health: (a) stressors and (b) health behaviors.
SES and stressors
Individuals who are socioeconomically disadvantaged experience more stressful life events [30, 31] and, when stressful events do happen, individuals who are socioeconomically disadvantaged perceive these events as more stressful, perhaps due to limited interpersonal and intrapersonal resources to cope with stressors [2]. Neighborhood SES may lead to increased stress through factors such as overcrowding and high crime rates [3, 32]. There is an extensive animal literature that finds associations between being low on the social hierarchy and stress [33, 34], suggesting that subjective SES may also be associated with stress.
Several lines of research support the potential mediating role of stressors in the SES-health relation. First, research on the concept of allostatic load provides evidence of the mediating role of stressors in the SES-health relation. Allostatic load refers to the “wear and tear” on physiologic systems that occurs as a result of these systems adapting to severe or chronically stressful situations [35]. Lower SES is associated with higher allostatic load scores [36, 37]. Higher allostatic load scores are associated with decreased physical functioning, and increased risk of mortality [38–40].
Second, a small body of research provides direct empiric support for the mediating role of stressors in the SES-health relationship. Self-reported stress has been found to mediate the relation between objective SES and health, including physical health symptoms and self-rated health [31, 41]. Further, measures of neighborhood-related stressors (e.g., neighborhood strain, social integration, sense of control, and financial strain) mediated the relation between neighborhood SES and physical functioning [10].
SES and health behaviors
Health compromising behaviors (HCBs) such as smoking, poor diet, and lack of physical activity usually lead to poor health. Low objective SES is associated with higher rates of these health compromising behaviors [2, 42–45]. When health behaviors are assessed longitudinally, health behaviors explain 72% of the association between objective SES and all-cause mortality [42]. Low neighborhood SES [15, 24, 46] and low subjective SES [47] are also associated with HCBs.
Limited research has investigated health behaviors as mediators of the SES-health relation. Health behaviors have been found to mediate the association between objective SES and health [7, 21], as well as the association between neighborhood SES and health [48]. To our knowledge, no research has investigated HCBs as a mediator of the relation between subjective SES and health.
Health compromising behaviors may be used to cope with stressors and to reduce negative affect associated with stressful circumstances [3, 24, 49]. Thus, while health behaviors may mediate the association between SES and health, there may also be a more complex mediational chain in which low SES leads to increased exposure to stressors, which leads to health compromising behaviors to cope with the stressors, which, in turn, leads to poor health. Limited research has investigated such a complex mediation model of the effects of SES on health.
Current Study
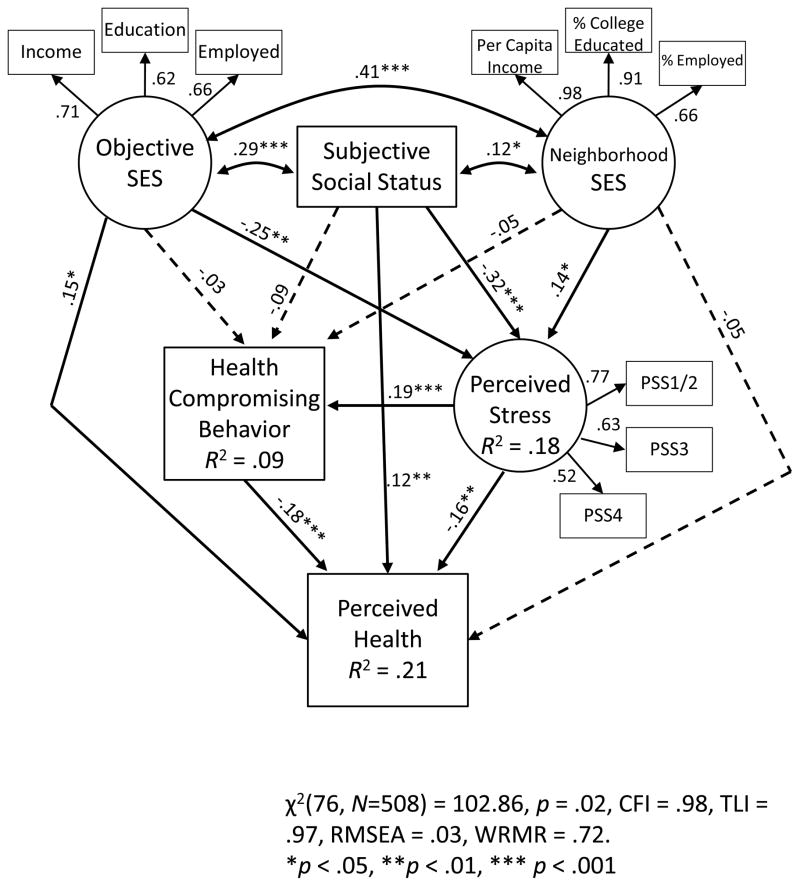
In this study, we investigate the relations between objective, subjective, and neighborhood SES; perceived stress; health behaviors; and perceived health (see Figure 1). We hypothesized that all three types of SES would be negatively associated with perceived stress and perceived health, and positively associated with health compromising behaviors. Further, we hypothesized a mediational chain in which low SES leads to greater perceived stress, which leads both directly and indirectly (through increased health compromising behaviors) to poorer perceived health. This is one of the first studies to simultaneously investigate the direct and indirect effects of these three different types of SES on perceived health. In addition, our consideration of HCBs as a potential step on the causal chain from SES to poor health represents an advance over prior research that has frequently viewed health behaviors as an outcome or controlled for the influence of health behaviors on health; because SES may influence HCBs (as a way to cope with the stressors associated with socioeconomic disadvantage), studies that control for health behaviors may underestimate the true impact of SES on health [50]. We employ a structural equation modeling approach to allow for multiple, correlated measures of each type of SES.
Figure 1.
Structural equation model showing associations between SES constructs, perceived stress, health compromising behaviors, and perceived health. Standardized regression coefficients are reported. Control variables included age, sex, and race. Dashed lines represent non-significant paths.
Methods
Participants
Participants were patients attending a publicly-funded sexually transmitted disease (STD) clinic who were recruited into a randomized controlled trial (RCT) to evaluate a sexual risk reduction intervention [51]. Inclusion criteria for the trial were: (a) age 16 or older; and (b) engaged in sexual risk behavior (> 1 sex partner or a non-monogamous sex partner in the past 3 months and inconsistent condom use). Exclusion criteria were: (a) severe mental impairment; (b) inpatient substance use treatment; (c) HIV infection; and (d) planning to move out of the area in the next year. Patients were recruited into the trial from August, 2010 through September, 2012. Of the 2766 patients approached, 2677 (97%) agreed to be screened, 1322 (49%) were eligible, and 1010 (76%) consented and completed the baseline survey. Participants were randomly assigned to complete a general-health focused (n = 508) or a sexual health focused (n = 502) survey. Data for the current study come from the 508 participants who completed the general health survey. Participants were 46% female (n = 236), 68% African American (n = 345), 18% Caucasian (n = 92), and 8% mixed race (n = 41). The average age was 28 years (SD = 9 years).
Procedures
Patients waiting to be seen at the clinic were called by clinic number and escorted to a private exam room. A trained Research Assistant (RA) obtained verbal consent for screening and screened patients for eligibility. The study was explained to eligible patients; those who were interested in participating provided written, informed consent.
Participants completed a baseline Audio Computer-Assisted Self-Interview (ACASI) in the private exam room. With this technology, questions and response options are read aloud, allowing individuals of all literacy levels to participate while also allowing participants to respond privately to sensitive questions. After completing the ACASI, participants completed a paper-and-pencil measure of subjective SES. Participants viewed one of two intervention videos as part of the main RCT, and were reimbursed $30 for their time. All procedures were approved by the Institutional Review Boards of the participating institutions.
Measures
Demographic information
We obtained information on participants’ age, sex, and race; dummy variables were created indicating White (vs. Black) and mixed (vs. Black) races.
Socioeconomic status
Measures of income, education, and employment status served as indicators of objective SES. Participants were asked to report their annual yearly family income (<$15,000; $15,000 to <$30,000; $30,000 to $45,000; >$45,000), the highest grade they completed in school (8th grade or less; > 8th grade but < 12th grade; GED; graduated high school; started college; graduated college), and their employment status (employed full or part time; unemployed). These categorical variables served as indicators of a latent objective SES construct.
Neighborhood SES variables were derived from 2010 U.S. Census data. The census tract in which each participant lived was determined from his/her current address. Measures of neighborhood SES included: (a) per capita income in the census tract; (b) percentage of individuals with a college education in the census tract; and (c) percent employed in the census tract. These variables served as indicators of a latent neighborhood SES construct.
Subjective SES was assessed with a paper-and-pencil measure. Participants were shown a ladder with 10 rungs and asked to indicate, with an X, where they fell on the ladder from people who are the worst off in their community (1) to people who are the best off in their community (10) [52].
Perceived stress
Participants completed the 4-item Perceived Stress Scale [53]. This measure assesses perceived stress in the past month (e.g., “How often have you felt you were unable to control the important things in your life?”) on a scale from never (0) to very often (4). This scale has adequate internal consistency and test-retest reliability, and evidence of validity in community samples, as well as among adolescents/young adults and urban populations [53–55]. In the present study, internal consistency reliability was .68. Scale items served as indicators of a latent perceived stress construct [with items 1 and 2 parceled to yield three total indicators; 56].
Health compromising behaviors
We created an index of health compromising behaviors (HCBs), informed by prior research on multiple health compromising behaviors [45, 57, 58], which included substance use behavior, sexual behavior, physical activity, diet, and sleep. Each HCB was dichotomized, and items were summed to form a single index of HCBs, ranging from 0 to 12.
Binge drinking was defined as having had four or more drinks for women (five or more drinks for men) in a single day in the past 3 months [59]. Smoking was defined as ever using cigarettes or other tobacco products in the past 3 months. Illegal drug use was defined as using marijuana, crack, or cocaine during the past 3 months; in prior research at the clinic, these substances were the only ones used by a substantial percentage of patients [60, 61]. Sexual risk behavior was defined as having sex without a condom with a non-primary partner in the past 3 months. Participants who reported engaging never or rarely in vigorous physical activity (for 20 minutes or more at a time) or moderate physical activity (for 30 minutes or more at a time) in the past 3 months were considered to be physically inactive. Because sitting for > 8 hours/day may compromise health [62], participants who reported sitting for > 8 hours/day were coded as engaging in excessive sitting. Irregular breakfast consumption was defined as eating breakfast on 5 or fewer days during the past week. Participants who reported eating fast food at least once per week were considered to be frequent fast food consumers. Participants who reported consuming both fruits and vegetables less than daily in the past month were coded as infrequent fruit and vegetable consumers. Those who reported drinking soda at least daily in the past month were coded as frequent soda consumers. Those who reported consuming red meat, processed meat, or fried food daily in the past month were coded as having a high-fat diet. Participants who slept fewer than 7 hours or more than 9 hours per night were coded as having poor sleep.
Consistent with prior research [10, 45, 63, 64], we created summed the number of dichotomous indicators of HCBs to form a single indicator of HCB. The index of HCBs ranged from 0 to 12.
Perceived health status
Participants were asked to report their self-rated health with a single item from the Medical Outcomes Study General Health Survey [65]. Participants were asked to rate their health on a 5-point scale from poor (1) to excellent (5). Single items assessing self-rated health are associated with mortality [66].
Data Analysis
The primary study analyses were conducted using structural equation modeling, allowing us to test both direct and indirect associations of objective, neighborhood, and subjective SES with perceived health. Objective SES, neighborhood SES, and perceived stress were represented as latent constructs with three indicators each, while subjective SES, HCBs, and perceived health were represented as manifest variables. Latent constructs were identified by fixing variance at 1 [67]; to increase the interpretability of coefficients, we also standardized the manifest variables in our model.
In our structural model, the three types of SES were allowed to correlate. Directional paths led from all three SES constructs to stress, HCBs, and perceived health; from stress to HCBs and perceived health; and from HCBs to perceived health, in line with our hypotheses. Additionally, directional paths led from demographic variables (including age, male sex, White race, and mixed race) to all constructs in the model in order to control for these variables.
Models were fit with the robust weighted least squares (WLSMV) estimator in Mplus 7 [68]. Model fit was assessed using traditional fit indices, including the comparative fit index [CFI; 69]; the Tucker-Lewis index [TLI; 70]; and the misfit measure known as the root-mean-square error of approximation [RMSEA; 56]. Good fit is indicated by CFI and TLI values greater than .95 and RMSEA values less than .05 [56, 71].
When testing indirect effects, we utilized bias-corrected bootstrapped 95% confidence intervals based on 5,000 iterations, as is recommended given the non-normal distribution of these effects [72]. We report standardized coefficients and 95% confidence intervals throughout.
Levels of missing data were modest; 8% of participants (n = 43) were missing information on neighborhood-level SES, and less than 4% of data was missing for all other variables. Participants with some missing data (n = 65) did not significantly differ from those with complete data (n = 443) on any key study variables (objective SES, subjective SES, neighborhood SES, perceived stress, health compromising behaviors, or perceived health) or in terms of demographic characteristics (sex, race/ethnicity, and age). (See Asparouhov and Muthen [73] for an explanation of how missing data are handled using the WLSMV estimator.)
Results
Sample Characteristics
The sample was predominantly socioeconomically disadvantaged, with at least half of participants reporting an income <$15,000/year (53%, n = 258), a high school or less education (63%, n = 322), and current unemployment (50%, n = 253). Participants also lived in socioeconomically disadvantaged neighborhoods, with a median per capita income of $14,267 per year. The median percentage of college graduates in these census tracts was 13%, and the median employment rate was 89%. Compared to others in their community, participants rated their social status as average (M = 5.8 on the 10 point scale, SD = 1.9).
Participants reported moderate levels of stress (M = 1.7, SD = 0.8). They reported, on average, engaging in 6.1 of the 12 possible HCBs. Participants perceived themselves to be in good to very good health, with an average perceived health score of 3.5 (SD = 1.0).
Relations among SES Variables
The three SES variables were correlated. Objective SES was correlated with both neighborhood SES (r = 0.51, p < .001) and subjective SES (r = 0.27, p < .001). Neighborhood SES and subjective SES were also correlated (r = 0.11, p < .05).
Relations between SES, Health Compromising Behaviors, Perceived Stress, and Perceived Health
SES and perceived stress
We first explored independent associations between the different forms of SES and perceived stress. Controlling for demographics, objective SES had a significant negative association with stress, b = −.27, 95% CI = [−.42, −.12]. Subjective SES was also negatively associated with stress, b = −.34, 95% CI = [−.45, −.22]. Neighborhood SES was not associated with stress (Table 1).
Table 1.
Univariate and multivariate associations between SES and perceived stress, health compromising behaviors, and perceived health
| Univariatea | Multivariateb | |
|---|---|---|
| Perceived Stress | ||
| Objective SES | −0.27*** [−0.42, −0.12] | −0.25** [−0.43, −0.07] |
| Neighborhood SES | 0.01 [−0.08,0.11] | 0.14* [0.003,0.28] |
| Subjective SES | −0.34*** [−0.45, −0.22] | −0.32*** [−0.42, −0.21] |
| Health Compromising Behaviors | ||
| Objective SES | −0.13* [−0.24, −0.02] | −0.08 [−0.22,0.05] |
| Neighborhood SES | −0.07 [−0.17, 0.02] | −0.02 [−0.14,0.10] |
| Subjective SES | −0.17*** [−0.26, −0.10] | −0.15** [−0.24, −0.21] |
| Perceived Health | ||
| Objective SES | 0.22*** [0.12,0.31] | 0.20** [0.08,0.33] |
| Neighborhood SES | 0.06 [−0.02,0.14] | −0.07 [−0.17,0.04] |
| Subjective SES | 0.25*** [0.17,0.34] | 0.20*** [0.12,0.28] |
Individual associations between socioeconomic status (SES) and stress, HCBs, and perceived health, controlling for demographic variables.
Multivariate associations between the three measures of SES and stress, health compromising behaviors, and perceived health, controlling for demographic variables.
p < .05,
p < .01,
p < .001.
When all three forms of SES were considered simultaneously, both objective SES and subjective SES remained negatively associated with stress, b = −.25, 95% CI = [−.43, −.07] and b = −.32, 95% CI = [−.42, −.21], respectively. Additionally, after considering objective and subjective SES, neighborhood SES was positively associated with stress, b = .14, 95% CI = [.003, .28].
SES and health compromising behaviors
We also explored independent associations between the different forms of SES and HCBs. Controlling for demographics, objective SES was significantly associated with HCBs, b = −0.13, 95% CI = [−0.24, −0.02]. Subjective SES was also associated with HCBs, b = −0.17, 95% CI = [−0.26, −0.10]. Neighborhood SES was not associated with HCBs. When all three forms of SES were considered simultaneously, only subjective SES was significantly associated with HCBs, b = −0.15, 95% CI = [−0.24, −0.06].
SES and perceived health
We explored independent associations between the different forms of SES and perceived health. Controlling for demographics, objective SES was significantly associated with perceived health, b = 0.22, 95% CI = [0.12,0.31]. Subjective SES was also associated with perceived health, b = 0.25, 95% CI = [0.17,0.34]. Neighborhood SES was not associated with perceived health. When all three forms of SES were considered simultaneously, both objective and subjective SES remained associated with perceived health, b = 0.20, 95% CI = [0.08,0.33] and b = 0.20, 95% CI = [0.12,0.28], respectively.
Mediation Model
Measurement model
A measurement model containing latent constructs (objective SES, neighborhood SES, and perceived stress); manifest variables (subjective SES, HCBs, and perceived health); and all correlations among constructs fit the data well, χ2(42, N = 508) = 63.64, p < .05, CFI = 0.98, TLI = 0.97, RMSEA = 0.03, allowing us to proceed with our structural model.
Full model
The full model (Figure 1) fit the data well, χ2 (76, N = 508) = 102.86, p < .05, CFI = 0.98, TLI = 0.97, RMSEA = 0.03. This model explained 18% of the variance in perceived stress, 9% of the variance in HCBs, and 21% of the variance in perceived health. Although the chi-square test was significant (potentially indicating poor model fit), the chi-square test is not a good indicator of model fit because it is nearly always significant with large sample sizes [56]. For this reason, alternative fit indices such as the CFI, TLI, and RMSEA have been developed. These alternative fit indices all indicate a good model fit.
Direct effects of SES on perceived stress, health compromising behaviors, and perceived health
In the full model, objective SES and subjective SES were both negatively associated with perceived stress, while neighborhood SES was positively associated with perceived stress. Those with higher objective SES and those who perceived themselves as better off reported lower levels of stress, whereas those who lived in higher SES neighborhoods reported higher levels of stress. After accounting for perceived stress, there were no significant direct associations between SES and HCBs. However, even after accounting for perceived stress and HCBs, objective SES and subjective SES remained directly associated with perceived health; lower objective and subjective SES were associated with perceiving oneself to be in poorer health.
Indirect effects of SES on perceived health through perceived stress
There was an indirect effect of objective SES on perceived health through perceived stress, b = 0.04, 95% CI = [0.01,0.09]. In addition, there was an indirect effect of subjective SES on perceived health through perceived stress, b = 0.05, 95% CI = [0.02, 0.10]. Lower objective and subjective SES were associated with greater perceived stress; greater perceived stress, in turn, was associated with poorer perceived health. In contrast, there was a negative indirect effect of neighborhood SES on perceived health through perceived stress, b = −0.02, 95% CI = [−0.06, −0.003]; higher neighborhood SES was associated with greater perceived stress, which was in turn associated with poorer perceived health.
Indirect effects of SES on perceived health through health compromising behaviors
There were no indirect effects of SES on perceived health through HCBs.
Indirect effects of SES on perceived health through perceived stress and health compromising behaviors
There was a significant positive indirect effect of objective SES on perceived health through perceived stress and HCBs, b = 0.01, 95% CI = [0.002, 0.03], as well as a significant positive indirect effect of subjective SES on perceived health through perceived stress and HCBs, b = 0.01, 95% CI = [0.004, 0.02]. Lower objective and subjective SES were associated with greater perceived stress; greater perceived stress, in turn, was associated with more HCBs; more HCBs, in turn, were associated with poorer perceived health. In contrast, there was a significant negative indirect effect of neighborhood SES on perceived health through perceived stress and HCBs, b = −0.01, 95% CI = [−0.02, −0.001]. Higher neighborhood SES was associated with greater perceived stress, greater perceived stress was associated with more HCBs, and more HCBs were associated with poorer perceived health.
Total effects of SES on perceived health
The total effect of objective SES on perceived health was significant, b = 0.21, 95% CI = [0.07, 0.34], as was the total effect of subjective SES on perceived health, b = 0.20, 95% CI = [0.10, 0.30]. The total effect of neighborhood SES on perceived health was not significant, b = −0.06, 95% CI = [−0.17, 0.05].
Discussion
Consistent with prior research, we found that objective, neighborhood, and subjective SES variables were correlated [8]. Correlations among the SES variables in our study ranged from r = .11 to .51. These correlations between SES variables are consistent with findings from other studies [8], and indicate that objective, subjective, and neighborhood SES are distinct constructs. In addition, in the full model both objective and subjective SES were associated directly and indirectly with perceived health, indicating that these variables are tapping different dimensions of socioeconomic disadvantage, each of which are uniquely important in predicting health.
We found support for the hypothesized indirect effects of SES on health through perceived stress, as well as through perceived stress and HCBs. As expected, lower objective and subjective SES were associated with greater stress; greater stress, in turn, was associated with poorer perceived health. Further, we found evidence of an additional indirect path whereby lower objective and subjective SES were associated with greater stress, which was associated with more HCBs, which, in turn, predicted poorer perceived health. This set of findings is consistent with the suggestion that HCBs are used to cope with stressors or to manage negative affect associated with stressors [3, 24, 45, 49]. In addition, stressors may lead to neurologic changes associated with poor self-control and future discounting (i.e., favoring smaller, immediate rewards of engaging in a pleasurable activity over longer-term, larger rewards of good health), which may make it difficult for individuals in stressful circumstances to refrain from engaging in highly reinforcing and pleasurable HCBs [74]. Additional research is needed to better understand the mechanisms through which stressors leads to HCBs. Regardless of the specific mechanism(s), our findings suggest that HCBs should be investigated as part of the pathway from socioeconomic disadvantage to stressors to poor health, rather than treated as a confound.
Both objective SES and subjective SES remained directly associated with perceived health after accounting for the mediating effects of perceived stress and HCBs, and the indirect effects through stress and HCBs were small. This suggests there may be additional pathways—not assessed in the current study—through which SES leads to poor health. Pathways to evaluate in future research include mediators such as healthcare access, social support, coping, social capital, norms, and pollutions and toxins [1, 3, 20, 23]. In addition, the full model explained 21% of the variance in perceived health. There are numerous determinants of actual health that were not assessed in the present study, including genetic influences, healthcare access and quality (which may partially be reflected in SES), and early life experiences and behaviors [75]. In addition, perceived health may be influenced by personality and mental health factors (e.g., mood, psychiatric disorder), independent of actual health status [76, 77].
In contrast to the expected findings for objective and subjective SES, the effects of neighborhood SES were not consistent with our hypotheses. Neighborhood SES had no direct associations with either HCBs or perceived health and was not independently associated with perceived stress. This contrasts with prior research findings that, even after controlling for other types of SES, neighborhood SES is associated with health [8, 10, 11, 15], including perceived health [9, 12]. After accounting for objective and subjective SES, neighborhood SES was positively associated with perceived stress, in contrast to our predictions. However, given the lack of association between neighborhood SES and perceived stress and health when neighborhood SES was considered independently, this unexpected relationship in the full model may be a statistical artifact reflecting that the multivariate analyses assess the relation between perceived health and the portion of the neighborhood SES construct that did not overlap with the objective and subjective SES constructs.
This study had several strengths, including a large sample that allowed for testing multiple mediators and complex meditational paths. In addition, the study had several methodological strengths, including the use of a computerized survey, which is associated with higher rates of reporting of socially sensitive behaviors relative to other assessment methods [78, 79]. In addition, the use of structural equation modeling allowed for multiple, correlated measures of the objective and neighborhood-level SES variables. SES has multiple components, including income, education, and occupation; constructing latent constructs representing objective and neighborhood SES allowed us to account for this. Use of structural equation modeling also allows for sensitive tests of indirect pathways [80].
This study also had several limitations. The sample was predominantly low-income and lived in low-income neighborhoods; thus, results may not generalize to less socioeconomically disadvantaged populations. However, because the relation between SES and health is strongest at the bottom end of the socioeconomic spectrum [4], it is important to study the pathways through which socioeconomic disadvantage leads to poor health among socioeconomically disadvantaged individuals. In addition, the sample was recruited from an STD clinic. Individuals seeking treatment for STDs may differ from other low income populations in several ways: these individuals are more likely to be engaging in sexual risk behavior (one of the HCBs assessed in the current study); they may be more likely to perceive themselves to be in poor health and to be currently experiencing distress because they believe they are infected with an STD. Thus, results may not generalize to individuals who are not STD clinic patients. The measures relied on patients’ perceptions of their social standing (i.e., subjective SES), stress, and health. Psychological factors, such as depression, could influence responses on all of these measures, and may account for some of the relations observed in this study. In addition, health behaviors were self-reported; objective measures confirming the accuracy of these self-reported behaviors (e.g., cotinine for smoking, accelerometer or pedometer data for physical activity and sitting) were not collected. Future research should investigate whether there are similar mediational paths between SES and health when using objective measures of health (e.g., body mass index, blood pressure, chronic disease status), rather than perceived health. Finally, this study was cross-sectional; therefore, we cannot be certain about the direction of effects. Although it is possible that poor health may lead to low SES [the social drift hypothesis; 81], data from longitudinal studies suggest that the SES-health association is driven primarily by low SES leading to poor health [the social causation hypothesis; 1, 7], supporting our hypothesized direction of effects.
Interventions aimed at reducing the impact of stressors and improving HCBs could help to improve the health of socioeconomically disadvantaged individuals. Helping socioeconomically disadvantaged individuals to cope with stressors may be a particularly important intervention target, because stress reduction can have both direct and indirect effects on health through reductions in HCBs. For example, mindfulness-based stress reduction has significant benefits for mental health, well-being, and perceived stress [82, 83] and is associated with improved physiologic stress markers [84, 85]. Further, there is emerging evidence that mindfulness techniques may improve health behaviors [86]. Limited research has examined the benefits of these techniques specifically among socioeconomically disadvantaged individuals, but emerging evidence suggests these techniques may be effective at reducing stress and improving health in low-income populations [87].
In conclusion, when considering only direct effects of SES on perceived health, objective SES and subjective SES, but not neighborhood SES, predicted perceived health. In a mediation model including direct and indirect effects, effects of SES on perceived health were mediated by perceived stress and HCBs. Future research should investigate the effects of stress reduction techniques on the health of socioeconomically disadvantaged individuals.
Acknowledgments
This work was supported by grant #R01MH068171 from the National Institute of Mental Health.
Footnotes
Authors Statement of Conflict of Interest and Adherence to Ethical Standards: Author Senn, Author Walsh, and Author Carey declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committees on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
References
- 1.Adler NE, Rehkoph DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 2.Adler NE, Boyce T, Chesney MA, et al. Socioeconomic status and health: The challenge of the gradient. Am Psychol. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- 3.Taylor SE, Repetti RL. Health psychology: What is an unhealthy environment and how does it get under the skin? Annu Rev Psychol. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- 4.House JS, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Hofrichter R, editor. Health and social justice: Politics, ideology, and inequity in the distribution of disease. San Francisco: Jossey-Bass; 2003. pp. 89–131. [Google Scholar]
- 5.Preston SH, Elo IT. Are educational differentials in adult mortality increasing in the United States? J Aging Health. 1995;7:476–496. doi: 10.1177/089826439500700402. [DOI] [PubMed] [Google Scholar]
- 6.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1993;329:103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- 7.Mulatu MS, Schooler C. Casual connections between socio-economic status and health: Reciprocal effects and mediating mechanisms. J Health Soc Behav. 2002;43:22–41. [PubMed] [Google Scholar]
- 8.Chen E, Paterson LQ. Neighborhood, family, and subjective socioeconomic status: How do they relate to adolescent health? Health Psychol. 2006;25:704–714. doi: 10.1037/0278-6133.25.6.704. [DOI] [PubMed] [Google Scholar]
- 9.Malmstrom M, Sundquist J, Johansson S. Neighborhood environment and self-reported health status: A multilevel analysis. Am J Public Health. 1999;89:1181–1186. doi: 10.2105/ajph.89.8.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: The roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Ann Behav Med. 2004;27:91–99. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- 11.Jaffe DH, Eisenbach Z, Neumark YD, Manor O. Individual, household and neighborhood socioeconomic status and mortality: A study of absolute and relative deprivation. Soc Sci Med. 2005;60:989–997. doi: 10.1016/j.socscimed.2004.06.047. [DOI] [PubMed] [Google Scholar]
- 12.Robert SA. Community-level socioeconomic status effects on adult health. J Health Soc Behav. 1998;39:18–37. [PubMed] [Google Scholar]
- 13.Malmstrom M, Johansson S, Sundquist J. A hierarchical analysis of long-term illness and mortality in socially deprived areas. Soc Sci Med. 2001;53:265–275. doi: 10.1016/s0277-9536(00)00291-4. [DOI] [PubMed] [Google Scholar]
- 14.Jones K, Duncan C. Individuals and their ecologies: Analysing the geography of chronic illness within a multilevel modelling framework. Health Place. 1995;1:27–40. [Google Scholar]
- 15.Bosma H, van de Mheen HD, Borsboom GJJM, Mackenbach JP. Neighborhood socioeconomic status and all-cause mortality. Am J Epidemiol. 2001;153:363–371. doi: 10.1093/aje/153.4.363. [DOI] [PubMed] [Google Scholar]
- 16.Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Soc Sci Med. 2003;56:1321–1333. doi: 10.1016/s0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- 17.Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosom Med. 2005;67:855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- 18.Cohen S, Adler N, Alper CM, et al. Objective and subjective socioeconomic status and susceptibility to the common cold. Health Psychol. 2008;27:268–274. doi: 10.1037/0278-6133.27.2.268. [DOI] [PubMed] [Google Scholar]
- 19.Demakakos P, Nazroo J, Breeze E, Marmot M. Socioeconomic status and health: The role of subjective social status. Soc Sci Med. 2008;67:330–340. doi: 10.1016/j.socscimed.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldman N. Social inequalities in health: Disentangling the underlying mechanisms. Ann N Y Acad Sci. 2001;954:118–139. [PubMed] [Google Scholar]
- 21.Chandola T, Clarke P, Morris JN, Blane D. Pathways between education and health: A casual modelling approach. J Roy Stat Soc A. 2006;169:337–359. [Google Scholar]
- 22.Anderson NB, Armstead CA. Toward Understanding the association of socioeconomic status and health: A new challenge for the biopsychosocial approach. Psychosom Med. 1995;57 :213–225. doi: 10.1097/00006842-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Chen E, Miller GE. Socioeconomic status and health: Mediating and moderating factors. Annu Rev Clin Psycho. 2013;9:8.1–8.28. doi: 10.1146/annurev-clinpsy-050212-185634. [DOI] [PubMed] [Google Scholar]
- 24.Ellen IG, Mijanovich T, Dillman K. Neighborhood effects on health: Exploring the links and assessing the evidence. J Urban Aff. 2001;23:391–408. [Google Scholar]
- 25.Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann Behav Med. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- 26.Wen M, Hawkley LC, Cacioppo JT. Objective and perceived neighborhood environment, individual SES and psychosocial factors, and self-rated health: An analysis of older adults in Cook County, Illinois. Soc Sci Med. 2006;63:2575–2590. doi: 10.1016/j.socscimed.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 27.Evans GW, Kantrowitz E. Socioeconomic status and health: The potential role of environmental risk exposure. Annu Rev Public Health. 2002;23:301–331. doi: 10.1146/annurev.publhealth.23.112001.112349. [DOI] [PubMed] [Google Scholar]
- 28.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 29.Estabrooks PA, Lee RE, Gyuresik NC. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Ann Behav Med. 2003;25:100–104. doi: 10.1207/S15324796ABM2502_05. [DOI] [PubMed] [Google Scholar]
- 30.Brady SS, Matthews KA. The influence of socioeconomic status and ethnicity on adolescents’ exposure to stressful life events. J Pediatr Psychol. 2002;27:575–583. doi: 10.1093/jpepsy/27.7.575. [DOI] [PubMed] [Google Scholar]
- 31.Almeida DM, Shevaun DN, Banks SR, Serido J. Do daily stress processes account for socioeconomic health disparities? J Gerentol. 2005;60B:34–39. doi: 10.1093/geronb/60.special_issue_2.s34. [DOI] [PubMed] [Google Scholar]
- 32.Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress: Does stress account for SES effects on health? Ann N Y Acad Sci. 1999;896:131–144. doi: 10.1111/j.1749-6632.1999.tb08111.x. [DOI] [PubMed] [Google Scholar]
- 33.Sapolsky RM. The influence of social hierarchy on primate health. Science. 2005;308:648–652. doi: 10.1126/science.1106477. [DOI] [PubMed] [Google Scholar]
- 34.Tamashiro KLK, Nguyen MMN, Sakai RR. Social stress: From rodents to primates. Front Neuroendocrinol. 2005;26:27–40. doi: 10.1016/j.yfrne.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 35.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 36.Kubzansky LD, Kawachi I, Sparrow D. Socioeconomic status, hostility, and risk factor clustering in the normative aging study: Any help from the concept of allostatic load? Ann Behav Med. 1999;21:330–338. doi: 10.1007/BF02895966. [DOI] [PubMed] [Google Scholar]
- 37.Evans GW, Kim P. Childhood poverty and young adults’ allostatic load: The mediating role of childhood cumulative risk exposure. Psychol Sci. 2012;23:979–983. doi: 10.1177/0956797612441218. [DOI] [PubMed] [Google Scholar]
- 38.Karlamangla AS, Singer BS, Seeman TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom Med. 2006;68:500–507. doi: 10.1097/01.psy.0000221270.93985.82. [DOI] [PubMed] [Google Scholar]
- 39.Seeman TE, McEwen BS, Rowe JW, Singer BS. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci U S A. 2001;98:4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Crimmins EM, Johnston ML, Hayward M, Seeman T. Age differences in allostatic load: An index of frailty. In: Yi Z, Crimmins EM, Carriere Y, Robine JM, editors. Longer life and healthy aging. Netherlands: Springer; 2006. pp. 111–126. [Google Scholar]
- 41.Orpana HM, Lemyre L, Kelly S. Do stressors explain the association between income and declines in self-rated health? A longitudinal analysis of the national population health survey. Int J Behav Med. 2007;14:40–47. doi: 10.1007/BF02999226. [DOI] [PubMed] [Google Scholar]
- 42.Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. J Am Med Assoc. 2010;303:1159–1166. doi: 10.1001/jama.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviors and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med. 1997;44:809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- 44.Hanson MD, Chen E. Socioeconomic status and health behaviors in adolescence: A review of the literature. J Behav Med. 2007;30:263–285. doi: 10.1007/s10865-007-9098-3. [DOI] [PubMed] [Google Scholar]
- 45.Walsh JL, Senn TE, Carey MP. Longitudinal associations between health behaviors and mental health in low-income adults. Transl Behav Med. 2013;3:104–113. doi: 10.1007/s13142-012-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee RE, Cubbin C. Neighborhood context and youth cardiovascular health behaviors. Am J Public Health. 2002;92:428–436. doi: 10.2105/ajph.92.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ghaed SG, Gallo LC. Subjective social status, objective socioeconomic status, and cardiovascular risk in women. Health Psychol. 2007;26:668–674. doi: 10.1037/0278-6133.26.6.668. [DOI] [PubMed] [Google Scholar]
- 48.Robert SA. Neighborhood socioeconomic context and adult health: The mediating role of individual health behaviors and psychosocial factors. Ann N Y Acad Sci. 1999;896:465–468. doi: 10.1111/j.1749-6632.1999.tb08171.x. [DOI] [PubMed] [Google Scholar]
- 49.Rheingold AA, Acierno R, Resnick HS. Trauma, posttraumatic stress disorder, and health risk behaviors. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington: American Psychological Association; 2005. pp. 217–243. [Google Scholar]
- 50.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychol Bull. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 51.Carey MP, Senn TE, Coury-Doniger P, et al. Optimizing the scientific yield from a randomized controlled trial (RCT): Evaluating two behavioral interventions and assessment reactivity with a single trial. Contemp Clin Trials. 2013;36:135–146. doi: 10.1016/j.cct.2013.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- 53.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 54.Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the Perceived Stress Scale. Journal of College Counseling. 2006;9:135–147. [Google Scholar]
- 55.Sharp LK, Kimmel LG, Kee R, Saltoun C, Chang C. Assessing the Perceived Stress Scale for African American adults with asthma and low literacy. Journal of Asthma. 2007;44 :311–316. doi: 10.1080/02770900701344165. [DOI] [PubMed] [Google Scholar]
- 56.Kline RB. Principles and practice of structural equation modeling. New York: Guilford; 2011. [Google Scholar]
- 57.Heinrich KM, Maddock J. Multiple health behaviors in an ethnically diverse sample of adults with risk factors for cardiovascular disease. Perm J. 2011;15:12–18. doi: 10.7812/tpp/10.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.De Vries H, van’t Reit J, Spigt M, et al. Clusters of lifestyle behaviors: Results from the Dutch SMILE study. Prev Med. 2008;46:203–208. doi: 10.1016/j.ypmed.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 59.Dufour MC. What is moderate drinking? Defining “drinks” and drinking levels. Alc Res Hlth. 1999;1999:5–14. [PMC free article] [PubMed] [Google Scholar]
- 60.Carey MP, Senn TE, Vanable PA, Coury-Doniger P, Urban MA. Brief and intensive behavioral interventions to promote sexual risk reduction among STD clinic patients: Results from a randomized controlled trial. AIDS Behav. 2010;14:504–517. doi: 10.1007/s10461-009-9587-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Carey MP, Vanable PA, Senn TE, Coury-Doniger P, Urban MA. Evaluating a two-step approach to sexual risk reduction in a publicly-funded STI clinic: Rationale, design, and baseline data from the Health Improvement Project-Rochester (HIP-R) Contemp Clin Trials. 2008;29 :569–586. doi: 10.1016/j.cct.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222,497 Australian adults. Arch Intern Med. 2012;172:494–500. doi: 10.1001/archinternmed.2011.2174. [DOI] [PubMed] [Google Scholar]
- 63.Donovan JE, Jessor R, Costa FM. Adolescent health behavior and conventionality-unconventionality: An extension of problem-behavior therapy. Health Psychol. 1991;10:52–61. [PubMed] [Google Scholar]
- 64.Gallant MP, Connell CM. Neuroticism and depressive symptoms among spouse caregivers: Do health behaviors mediate this relationship? Psychol Aging. 2003;18:587–592. doi: 10.1037/0882-7974.18.3.587. [DOI] [PubMed] [Google Scholar]
- 65.Stewart AL, Hays RD, Ware JE. The MOS Short-Form General Health Survey. Med Care. 1988;26:724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 66.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 67.Little TD. Longitudinal structural equation modeling. New York: Guilford; 2013. [Google Scholar]
- 68.Muthén LK, Muthén BO. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2013. [Google Scholar]
- 69.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 70.Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- 71.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 72.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 73.Asparouhov T, Muthen B. Weighted least squares estimation with missing data. from http://www.statmodel.com/download/GstrucMissingRevision.pdf.
- 74.Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137:959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Woolf SH, Aron L, editors. US Health in international perspective: Shorter lives, poorer health. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 76.Roysamb E, Tambs K, Reichborn-Kjennerud T, Neale MC, Harris JR. Happiness and health: Environmental and genetic contributions to the relationship between subjective well-being, perceived health, and somatic illness. Journal of Personality and Social Psychology. 2003;85:1136–1146. doi: 10.1037/0022-3514.85.6.1136. [DOI] [PubMed] [Google Scholar]
- 77.Barsky AJ, Cleary PD, Klerman GL. Determinants of perceived health status of medical outpatients. Soc Sci Med. 1992;34:1147–1154. doi: 10.1016/0277-9536(92)90288-2. [DOI] [PubMed] [Google Scholar]
- 78.Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behavior for HIV among injecting drug users: A quasi-randomised trial. Lancet. 1999;353:1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 79.Perlis TE, Des Jarlais DC, Friedman SR, Arasteh K, Turner CF. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004;99:885–896. doi: 10.1111/j.1360-0443.2004.00740.x. [DOI] [PubMed] [Google Scholar]
- 80.Fairchild AJ, MacKinnon DP. A general model for testing mediation and moderation effects. Prev Sci. 2009;10:87–99. doi: 10.1007/s11121-008-0109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fox JW. Social class, mental illness, and social mobility: The social selection-drift hypothesis for serious mental illness. J Health Soc Behav. 1990;31:344–353. [PubMed] [Google Scholar]
- 82.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. J Psychosom Res. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 83.Smith BW, Shelley BM, Dalen J, et al. A pilot study comparing the effects of mindfulness-based and cognitive-behavioral stress reduction. J Alternative Compl Med. 2008;14 :251–258. doi: 10.1089/acm.2007.0641. [DOI] [PubMed] [Google Scholar]
- 84.Regehr C, Glancy D, Pitts A. Interventions to reduce stress in university students: A review and meta-analysis. J Affect Disord. 2013;148:1–11. doi: 10.1016/j.jad.2012.11.026. [DOI] [PubMed] [Google Scholar]
- 85.Nyklicek I, Mommersteeg PMC, Van Beugen S, Ramakers C. Mindfulness-based stress reduction and physiological activity during acute stress: A randomized controlled trial. Health Psychol. doi: 10.1037/a0032200. in press. [DOI] [PubMed] [Google Scholar]
- 86.Greeson JM. Mindfulness research update: 2008. Compl Health Pract Rev. 2009;14:10–18. doi: 10.1177/1533210108329862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Palta P, Page G, Piferi RL, et al. Evaluation of a mindfulness-based intervention program to decrease blood pressure in low-income AfricanfAmerican older adults. Journal of Urban Health. 2012;89:308–316. doi: 10.1007/s11524-011-9654-6. [DOI] [PMC free article] [PubMed] [Google Scholar]