INTRODUCTION: Robert M. Sade, MD
A growing number of health care institutions are adopting a policy of denying employment to smokers, based on urine testing for the presence of nicotine and nicotine metabolites. Such institutions include the Cleveland Clinic, which pioneered this policy in 2007, the Geisinger Health System, the University of Pennsylvania Health System, and the Baylor Health Care System.[1]
These policies are controversial. Arguments favoring them include a social obligation of medical centers to promote healthy activities, an obligation to provide a healthy environment for employees, and not supporting a habit that is addictive and lethal. Moreover, smokers add considerable cost to the institution’s bottom line, because of their higher health care expenses and costs in lost productivity.
Arguments against denial of employment to tobacco users include the hypocrisy of banning smokers, while continuing to hire those who are obese, have a record of reckless driving, and use alcohol. Also, such policies are paternalistic: it’s none of the hospital's business what its employees do when they are not at work.
Thoracic surgeons as a group strongly oppose tobacco use, but a hiring ban changes the game: should surgeons oppose or support a hiring ban of smokers? To deliberate on this issue, a debate was held at the 60th Annual Meeting of the Southern Thoracic Surgical Association in 2013. The debate focused on the following vignette.
The Case of the Perplexed President
Dr. Nicholas Ateene is the president of University Physicians, the group practice that comprises all physicians who work in the University Hospital. The hospital's Executive Director has asked him to review a policy the hospital will implement in a few months. The hospital campus has been smoke-free for several years, and under the new policy, the hospital will not hire any job applicants who currently smoke tobacco products. The Executive Director is requesting that University Physicians adopt a similar policy for physician applicants. Dr. Ateene asks two of his colleagues, Dr. James Jones and Dr. William Novick, for their advice about how he should respond to this request.
PRO: James W. Jones, MD, PhD. MHA
I was surprised when I heard this topic was going to be debated because the ethical answer is so obviously clear. Next, I was saddened by such a deficiency of professional self-regulation that institutional regulation again was necessary. The ethics of the topic will be discussed on an ethical basis, a societal basis, an institutional basis, and on a professional basis.
Everyone knows smoking is harmful but to be a difference something needs to make a statistically significant difference. Smoking clearly qualifies as an major threat to health. According to the Centers for Disease Prevention (CDC) data, the top four causes of death in America (about one and a half million deaths combined)—heart disease, malignancy, chronic respiratory disease, cerebrovascular disease—are smoking related.[2] Lung cancer—one of the least desirable cancers, smoking’s signature sickness—is increased twenty fold in smokers.
Further CDC calculates 443,000 deaths in 2010 resulted from smoking related diseases. These are from protracted conditions requiring continuing sometimes debilitating therapies. Consider for a moment, the total amount of suffering of those dying and in those recovering from the scourges of smoking associated diseases.
The question is: Can smoking be considered a moral failure? Smoking violates the virtue of prudence which is the ability to personally self-govern and professionally to wisely advise others. Engelhardt defines prudence succinctly as: soundness of judgment to achieve a positive balance of benefits over harms.[3] This definition clearly echoes and emphasizes the most important concept in surgical therapeutic decision making—“the risk/benefit ratio.” Is a proposed benefit of an action worth the risk it entails? If not, the action violates prudence and is reckless at best and most likely foolish.
The benefits are meager indeed when compared to the risks. Nicotine is an acetylcholine receptor agonist which briefly enhances mood. It promotes alertness, calmness, and relaxation as it opens the door for the reaper. Smoking violates the virtue of prudence.
Rights include rights of three principals: the patient, the surgeon, and the institution. The patient has the right to be treated by a knowledgeable competent surgeon and to have his or her health valued more than the surgeon’s interests.[4]
The surgeon has the right to be rewarded financially for clinical work and has all other non-professional rights and duties of the public. Professional rights have strict limitations because of the assumption of a fiduciary role. Physician behavioral freedoms end where fiduciary obligations begin.
Medical institutions operate more in accordance with duties than rights. Its rights are those of a business. Aside from meeting substantial regulatory compliance, a medical institution has the right to maintain its health-promoting image to secure the trust of patients. All institutions, medical and non-medical, have the right to “employer branding” their products and services. Since tobacco smoking is causal for the majority of diseases treated by the Cleveland Clinic and smokers carry a recognizable odor of their habit, why should they permit smokers to be caregivers?
Dr. Paul Terpeluk, director of Occupational Medicine at the Cleveland Clinic updated me about their employee non-smoking policy. The policy was initiated in 2007 by Dr. Delos Cosgrove, President and surgeon extraordinaire, and the policy is regarded as very successful for several reasons. Three thousand surgeons and forty thousand employees work there and none can smoke. The health-promoting image of the Clinic is not weakened which is vital to an important heath care institution. And the rate of smoking in the county where the clinic is located has declined double the average elsewhere. The basis legitimizing their right to institute the policy was the desire to have healthier employees for the business of medical care.
Physicians are overwhelmingly chosen as the source of information and encouragement for patients adopting healthier lifestyles.[5] This ethical obligation is at risk when physicians have adopted the unhealthy lifestyles they should be recommending that patients stop. The compromise occurs because our beliefs often adjust to defend our behavior.
The STOP study (Smoking: The Opinions of Physicians) examined the interactions of several thousand physicians with patients about smoking.[6] Physician smokers considered beneficial stress relief from smoking was a major barrier to cessation and were less likely to counsel against smoking. And, amazingly, one-third of physician smokers did not believe that smoking was a health hazard.
The harm principle has broad legal standing for limiting behavioral autonomy to prevent one from harming others. First articulated by John Stuart Mill: “…the sole end for which mankind are warranted, individually or collectively, in interfering with the liberty of action, of any of their number, is self-protection.”[7] Equally, one’s right to liberty ends when it imposes on another’s rights—especially when the imposition induces observable harm. As data showing harm to others accumulated from public smoking, it was banned.
American Medical Association in publication H-490-917 entitled “Physician Responsibilities for Tobacco Cessation” supports and advocates measures by physicians to: …quit smoking and to urge colleagues to quit; inquiring of all patients at each visit about their smoking habits; and at every visit, counseling those who smoke to quit using tobacco in any form. It supports the concept that hospitals, among others, be primary sites for educating the public about the harmful effects of tobacco.
According to the American Association of Thoracic Surgery’s and the Society of Thoracic Surgeon’s combined Code of Ethics, article 1.4: “Members should use their best efforts to protect patients from harm by recommending and providing care that maximizes anticipated benefits and minimizes potential harms.”[8]
Ethics are defined by logical examination of the societal mores in which we are immersed. Currently personal illness is a societal responsibility from medical insurance and obligations of medical institutions to provide care regardless of payment probability. Illness not physicians drives medical cost. Loss of heath drives illness and health is frequently behaviorally controlled.
In American society, cost of medical care is approaching a tipping point of no return. The Affordable Health Care Act is a financial tsunami which is fiscally unsound. The Office of the Actuary for the Centers for Medicare and Medicaid Services projects the 2014 National Medical Expenditures, after the Affordable healthcare act actualizes, are over $3.1 trillion. The government will pay half or $1.55 trillion. The 2012 total direct governmental revenue was 2.5 trillion.
Chronic disease is the deadly killer and there is no greater promoter of chronic disease than smoking. The answer to the ballooning cost of medical care is not to provide more medical treatments; it is to avoid needing expensive care; the only answer is prevention.
The arguments against refusing to hire smokers lack validity. “It is callous — and contradictory — for health care institutions devoted to caring for patients regardless of the causes of their illness to refuse to employ smokers.”[9] That argument erroneously equates the relationship of the institution with patients and employees; the ethics are very different: one is a fiduciary relationship and the other is an employer/employee relationship.
The claim that the policy of excluding smokers is discriminatory because more smokers are poor and minorities is not a legitimate claim because the demographics of health care employees differs from the general population; nurses commonly are smokers. Correlation is not always confirmation. Being qualified for employment at the Cleveland Clinic requires the same for all groups: They must give up smoking. Societies are improved by increasing top down standards and diminished by reducing bottom up standards.
Make no mistake we are our profession’s keepers. There is no higher calling than our fiduciary role in providing exemplary medical care to our fellow human beings. Emotional, religious, legal, financial, and occupational problems take a backseat when the health of us or our loved ones is seriously threatened. To default, even minimally, from that calling is at best a moral error and we should thank Toby Cosgrove and the Cleveland Clinic.
CON: William M. Novick, MD
Is it ethical for a hospital to deny employment to a physician who smokes tobacco products? This is the essence of the current debate. We are not discussing the negative impact smoking has on the individual. The position of those in favor of such a ban regarding employment is based upon a number of assertions:
Tobacco usage contributes to 20% of all annual deaths in the United States
Physicians should be role models for our patients, and therefor practice a healthy life-style, which includes no use of tobacco products
Hospitals should practice what they preach, i.e., healthy life-styles in their employee’s
Health care systems and practitioners should strive to decrease health care expenditures, i.e., decreasing use of tobacco products would decrease costs
Companies in the US can set the standards for employment in their institution.
The reasons that these assertions are of no significance in this particular ethical dilemma are presented.
Other unhealthy life-styles that contribute to the annual deaths in the US
Obesity contributes to 15% of all annual deaths in the US and 35.7% of all adults in the US were considered obese in 2010 [10,11,12,13]. Smoking of tobacco products is estimated to occur in approximately 19% of the adult population in the US, just over half the number of obese individuals. The estimated contribution to the annual death rate in the US for alcohol consumption is 80,000 and in the United Kingdom alcohol related death has a bimodal distribution [14,15]. Fatalities from traffic accidents were estimated to cause 35,000 deaths in 2012 and the protective effects of seat-belts, driving at the speed limit and not having consumed significant amounts of alcohol, are all well known to decrease fatalities in traffic accidents[16]. Almost 16,000 people with HIV/AIDS died in 2009 and the life-span of Gay men is reported to be as much as 20 years less than heterosexual counterparts [17,18].
The debate over whether or not obesity actually contributes 400,000 deaths annually [19] is another political maneuver specifically designed to keep tobacco smoking at the top of the list of causative agents and to preserve funding. The historically stated benefits of smoking by doctors, athletes and media stars have long since been corrected by the studies and data of the effects of long-term smoking. However, the continued use of tobacco products by politicians, celebrities and the occasional model athlete make it difficult to severely stigmatize smoking.
Doctors should serve as role models for their patients by practicing healthy life-styles
While this is certainly a laudable goal, doctors are just as human as the next person. Smoking among physicians has decreased from 18.8% to just over 3% between the 70’s and 1991[20]. Recent Gallop and WebMD polls report a smoking rate of 1.3% to 4% in the last 2 years for physicians [21,22]. It would appear that the decrease in the percentage of physicians who smoke has leveled out over the last 20 years. However, when one examines other unhealthy life-styles among physicians, we find that 42% are overweight or obese, 35% exercise less than 30 minutes once per week (if at all) and alcohol intake up to 2 drinks per day is common [men 18.9%, women 11.3%] . Where do we stop with this idea of physicians being role models for healthy life-styles? Do we monitor their caffeine intake to know whether they are in withdrawal, with its consequent detrimental effects,[23] or make sure they have a cup of coffee before they take that late night bleeder back?[24] Do we assess how many double lattes, or fast food burgers one had this week? Do we examine their lives for jumping out of perfectly good airplanes, speeding or not wearing a seat-belt when driving [25]? Do we quiz them on their attendance to church, temples or mosques last week? After all, in many parts of the country, spiritual health is considered to be an integral part of one’s overall mental health. Given the shorter life-span of Gay men, do we look at their gender preferences? The list is endless and considering the small number of physicians who smoke compared to those who are obese and fail to exercise adequately it seems we are overly focused on a tiny minority of physicians.
Hospitals should practice what they preach, healthy life-styles
Perhaps this is the most intriguing argument for denying employment to tobacco smokers. Hospitals in the US are institutions where the treatment of disease occurs. To suggest that they have somehow undergone a metamorphosis into preventative treatment centers alone is disingenuous at best. The hypocrisy of this position has been discussed [26]. Cleveland Clinic advertises on its web-page that it has a Wellness Institute, yet within the different options are those offering treatment plans for smoking cessation [27]. By offering of such a program, the clinic promulgates the hypocrisy of not allowing new employees to smoke. Why is it that they offer to help others stop smoking and yet are so callous to not help potential employees? Promoting healthy life-styles is certainly beneficial to potential patients, but when one considers the appearance of the workers I wonder what is more obvious: a smoker who cannot smoke on site or an obese physician? The answer is obvious.
A company in the United States has the right to set standards for hiring people
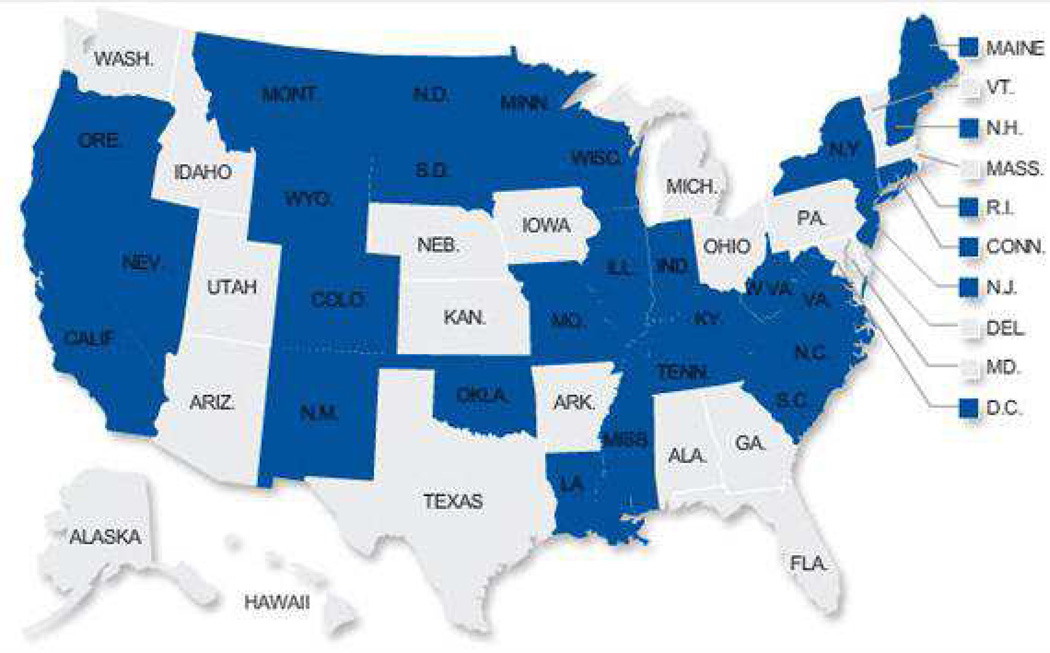
Although companies do have the right to set standards for individuals they hire, they must do so within the legal limits of State and Federal laws in the United States. Currently, there are 29 states which have enacted laws protecting smokers from what state legislators viewed as a form of workplace discrimination [28]. (Figure 1) The International Labor Organization states that “ Discrimination in employment and occupation takes many forms, and occurs in all kinds of work settings. It entails treating people differently because of certain characteristics, such as race, color or sex, which results in the impairment of equality of opportunity and treatment. In other words, discrimination results in and reinforces inequalities. The freedom of human beings to develop their capabilities and to choose and pursue their professional and personal aspirations is restricted, without regard for ability. Skills and competencies cannot be developed, rewards to work are denied and a sense of humiliation, frustration and powerlessness takes over”[29].
Figure 1.
Twenty-nine states and the District of Columbia (noted in blue) have passed laws that protect smokers rights by prohibiting hiring discrimination. (Adapted from: More workplaces don't allow employees to smoke at work, anywhere. Available at: http://www.digtriad.com/news/article/207243/8/Experimental%20Severe%20Weather%20Warnings%20To%20Motivate%20Response. Accessed December 3, 2013.)
Discrimination in the work place is not a new concept in the US. The Equal Employment Opportunity Act was signed into law by President R.M. Nixon in 1972. At the signing ceremony, Nixon stated “One of the basic principles in our way of life in America has always been that individuals would be free to pursue the work of their own choice, and to advance in that work subject only to consideration of their individual qualifications, talents and energies”[30]. Where in this statement or in this law does it allow for discrimination against individuals who smoke in the privacy of their own homes, cigar lounges or golf games? What exactly is the point of this highly discriminating action by a few hospitals? Physician smoking is at an all-time low, yet by self-admission, over 40% of physicians are overweight or obese. What is more evident to casual observers: a doctor who smokes, but they never see smoking or an obese physician that is clearly seen by all? The economics of a few smokers (2% or less) regarding health care expenditures compared to the economics of overweight physicians clearly is not the issue. The issue is one of marketing. Those hospitals that can claim a 100% smoker free staff stand to gain in the eyes of the public, which is constantly deluged by marketing and public relations firms to “buy” their product.
Ethical? Is it legal?
The United States was founded upon the principles of individual rights and, over the years since our founding, we have consistently reviewed our society and added laws to protect those who are discriminated against, regardless of the issue. The three pieces of paper that make the foundation of our government; the Declaration of Independence, the Constitution and the Bill of Rights, all uphold our rights to independent choice and decision without the fear of discrimination. The requirement for blood and urine tests for legal products used in the privacy of our own homes, which do not impact one’s ability to practice their specialty, is very close to violating the Fourth Amendment as an illegal search and seizure; “The right of the people to be secure in their persons, houses, papers, and effects, against unreasonable searches and seizures, shall not be violated…” [31]. Currently, 29 States have enacted laws specifically preventing discrimination on the basis of an individual being a smoker. It is important that the other 21 follow suit before this act of discrimination gains any more ground. The overt paternalism in this edict is not that different from the “nannystate” of New York City where Mayor Bloomberg recently pushed a plan to prevent the purchase of “Big Sized” soda beverages [32]. Are we as Americans now incapable of deciding what we want to do with our lives to the extent that the government needs to decide how we live our lives? We are not a culture or society that responds well to having our choices made for us by the government, as exemplified by the 60% of New York City residents who opposed Bloomberg’s proposal.[33]
The guiding principles by which we as a society make decisions regarding whether an action is ethical or not depends mostly on the perception by the majority of the people. When a majority of people see an action as wrong the act itself is perceived as unethical. Considering the principles of ethics being beneficence, non-maleficence, autonomy and justice one can see how denying physicians who smoke the opportunity to practice medicine in an institution blatantly violates each of these pillars.
Summary
Smoking among physicians is at an all-time low, indicating that we as health-care providers for the most part, practice what we preach. The hypocrisy of preventing those remaining physicians who smoke from practicing at a particular health care institution that provides care for individuals who suffer the consequences of smoking is obvious. We should accept these colleagues who continue to smoke and provide them with the necessary support to quit. The hard paternalistic position of some institutions seems in principle to violate the very ideals on which this country was founded and is actually against the law in the majority of states. Let us embrace our roles as physicians and help our colleagues who smoke rather than discriminate against them and ostracize them from our society.
CONCLUDING REMARKS: Robert M. Sade, MD
Both essayists were asked to advise the hypothetical Dr. Ateene on how he should respond to a request to adopt a policy of not hiring any physician applicant who smokes tobacco products. Jones is clear in advising him to adopt such a policy, while Novick is similarly clear in advising him not to do so. Each makes a strong case in support of his position.
In arguing their viewpoints, however, both also are blowing smoke at their audience in the form of irrelevant or misleading discussions. For example, Jones goes to some length in describing smoking as a moral failure of individuals, but the issue was not the morality of individuals’ smoking, rather, it was the ethics of institutional policy making. Novick mistakenly equates coercive law with corporate policy making by comparing New York Mayor Bloomberg's plan to prohibit sales of large-size soft drinks by force of law with a health care institution's development of a hiring policy — public law and private policy have very different ethical implications.
Interestingly, both essayists claim that the no-smokers policy is aimed at the public image of the health care institution, but each sees its purpose in an entirely different light. Jones describes this aspect of the policy as the institution maintaining "its health-promoting image to secure the trust of patients," an altogether praiseworthy objective. Novick understands this facet of the policy completely differently, seeing it as merely another sales pitch aimed at the public "which is constantly deluged by marketing and public relations firms to ‘buy’ their product."
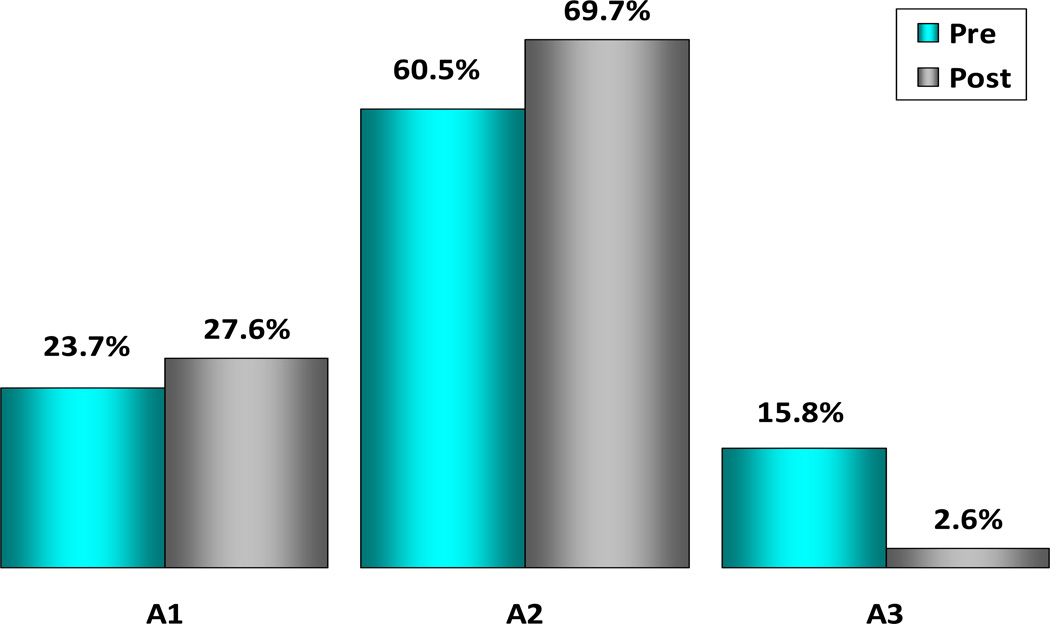
As part of the presentation of this debate, an Audience Response System was used, allowing attendees to use "clickers" to express their views on the topic being presented. The audience response to one of the questions was noteworthy because of a shift from pre- to post-debate. (Figure 2) Asked whether denying employment to tobacco smokers is ethically and morally justified, initially, 15.8% were not sure of their position, but by the end of the debate, only 2.6% remained uncertain. Most of the 13.2% initially undecided who made up their minds by the end of the debate came down on the negative side: the “No” answer increased from 60.5% to 69.7%. These numbers suggest that Novick presented the more persuasive arguments, and the data are consistent with a national Harris poll in 2012, which found that 65% of people surveyed oppose such hiring practices[34].
Figure 2.
The following choices were offered for audience response to the statement: Denying employment to tobacco smokers is ethically and morally justified.
A1. Yes
A2. No
A3. Not sure
The number of companies, including many health-related companies, that have adopted a no-hiring-of-smokers policy is said to be over 6,000 and increasing.[35] Contradicting this trend are the facts that 65% oppose policies banning the hiring of smokers and 29 states have already passed laws prohibiting such policies[36]. These conflicting trends suggest that the contest between supporters and opponents of smoker hiring bans is likely to continue for the foreseeable future.
ACKNOWLEDGEMENTS
Partial funding for Dr. Novick’s contribution was provided by the University Tennessee Health Sciences Centers Paul Nemir, Jr., MD, Chair for International Child Health and the International Children’s Heart Foundation. He thanks Ms. Aspen Mueller who was invaluable in the preparation of this manuscript and in managing his schedule from Iraq to Phoenix in time to make this presentation.
Dr. Sade’s role in this publication was supported by the South Carolina Clinical & Translational Research Institute, Medical University of South Carolina’s Clinical and Translational Science Award Number UL1RR029882. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Asch DA, Muller RW, Volpp KG. Conflicts and Compromises in Not Hiring Smokers. N Engl J Med. 2013;368:1371–1373. doi: 10.1056/NEJMp1303632. [DOI] [PubMed] [Google Scholar]
- 2.Ten Leading Causes of Death and Injury. [Accessed December 3, 2013];Injury Prevention and Control: Data and Statistics. Available at: http://www.cdc.gov/injury/wisqars/leadingcauses.html.
- 3.Englehardt H. The Foundations of Bioethics. New York: Oxford University Press; 1986. [Google Scholar]
- 4.McCullough L, Jones J, Brody B. Principles and Practice of Surgical Ethics. In: McCullough L, Jones J, Brody B, editors. Surgical Ethics. New York: Oxford University Press; 1998. [Google Scholar]
- 5.Llewellyn DJ, Lang IA, Langa KM, et al. Exposure to secondhand smoke and cognitive impairment in non-smokers: national cross sectional study with cotinine measurement. BMJ. 2009;338:b462. doi: 10.1136/bmj.b462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pipe A, Sorensen M, Reid R. Physician smoking status, attitudes toward smoking, and cessation advice to patients: an international survey. Patient Educ Couns. 2009;74:118–123. doi: 10.1016/j.pec.2008.07.042. [DOI] [PubMed] [Google Scholar]
- 7.Mill J. On Liberty. London: John W. Parker and Son; 1859. p. 34. [Google Scholar]
- 8.Code of Ethics. [Accessed December 3, 2013];Society of Thoracic Surgeons. 2009 Available at: http://www.sts.org/about-sts/policies/code-ethics.
- 9.Schmidt H, Voigt K, Emanuel EJ. The ethics of not hiring smokers. N Engl J Med. 2013;368:1369–1371. doi: 10.1056/NEJMp1301951. [DOI] [PubMed] [Google Scholar]
- 10.Satcher D. Surgeon general’s column. Commissioned Corps Bull. 2002;16(2):1–2. [Google Scholar]
- 11.Johannes L, Stecklow S. Dire warnings about obesity rely on slippery statistic. Wall Street Journal. 1998 Feb 9;B1 [Google Scholar]
- 12.Allison DB, Fontaine KR, Manson JE, et al. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–1538. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 13.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of Obesity in the United States, 2009–2010. NCHS Data Brief, No 82. 2012 Jan; [PubMed] [Google Scholar]
- 14.Fact sheets- alcohol use and health. [Accessed December 3, 2013];Alcohol and Public Health. Available at: http://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm.
- 15.White IR, Altmann DR, Nanchahal K. Alcohol consumption and mortality: modeling risks for men and women at different ages. BMJ. 2002;325:191–198. doi: 10.1136/bmj.325.7357.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.United States Census. [Accessed December 3, 2013];Transportation: motor vehicle accidents and fatalities. Available at: http://www.census.gov/compendia/statab/cats/transportation/motor_vehicle_accidents_and_fatalities.html.
- 17.HIV in the United States: at a glance. [Accessed December 3, 2013];HIV/AIDS. Available at: http://www.cdc.gov/hiv/statistics/basics/ataglance.html.
- 18.Hogg RS, Strathdee SA, Craib KJP, et al. Modelling the impact of HIV disease on mortality in gay and bisexual men. International J Epidem. 1997;26:657–661. doi: 10.1093/ije/26.3.657. [DOI] [PubMed] [Google Scholar]
- 19.Kolata G. [Accessed December 3, 2013];Data on deaths from obesity is inflated, U.S. agency says. Available at: http://www.nytimes.com/2004/11/24/health/24obese.html.
- 20.Nelson DE, Giovino GA, Emont SL, et al. Trends in cigarette smoking among US physicians and nurses. JAMA. 1994;271(16):1273–1275. [PubMed] [Google Scholar]
- 21.Bass K, McGeeney K. [Accessed December 3, 2013];U.S. physicians set good health example. 2012 Oct 3; Available at: http://www.gallup.com/poll/157859/physicians-set-good-health-example.aspx.
- 22. [Accessed December 3, 2013];Medscape Physician Lifestyle Report: 2012 Results. Available at: http://www.medscape.com/features/slideshow/lifestyle/2012/public.
- 23.Griffiths R. [Accessed March 2, 2014];Caffeine withdrawal recognized as a disorder. Johns Hopkins Medicine. Available at: http://www.hopkinsmedicine.org/press_releases/2004/09_29_04.html. [Google Scholar]
- 24. [Accessed March 2, 2014];Tired doctors told to drink more coffee. Available at: http://www.news.com.au/national/tired-doctors-told-to-drink-more-coffee/story-e6frfkwr-1225770409106.
- 25.Sulzberger AG. Hospitals Shift Smoking Bans to Smoker Ban. New York Times; 2011. Feb 10, [Google Scholar]
- 26.Schmidt H, Voight K, Emanuel EJ. The Ethics of Not Hiring Smokers. N Engl J Med. 2013;15:1369–1371. doi: 10.1056/NEJMp1301951. [DOI] [PubMed] [Google Scholar]
- 27. [Accessed December 3, 2013];Tobacco Treatment Center. Available at: http://my.clevelandclinic.org/tobacco/default.aspx.
- 28. [Accessed December 3, 2013];Editorial: Not hiring smokers crosses privacy line. Available at: http://usatoday30.usatoday.com/news/opinion/editorials/story/2012-01-29/not-hiring-smokers-privacy/52874348/1.
- 29.International Labor Organization. [Accessed December 3, 2013];Workplace Discrimination. Available at: http://www.ilo.org/global/topics/equality-and-discrimination/workplace-discrimination/lang--en/index.htm.
- 30.The American Presidency Project. [Accessed December 3, 2013];Richard Nixon. Statement about signing the Equal Employment Opportunity Act of 1972. Available at: http://www.presidency.ucsb.edu/ws/?pid=3358.
- 31. [Accessed December 3, 2013];United States Bill of Rights, Fourth Amendment. Available at: http://www.archives.gov/exhibits/charters/bill_of_rights_transcript.html.
- 32.Grynbaum MM. [Accessed December 3, 2013];New York soda ban to go before state’s top court. Available at: http://www.nytimes.com/2013/10/18/nyregion/new-york-soda-ban-to-go-before-states-top-court.html?_r=0.
- 33.Grynbaum MM, Connelly M. [Accessed December 3, 2013];60% in city oppose Bloomberg’s soda ban, poll finds. Available at: http://www.nytimes.com/2012/08/23/nyregion/most-new-yorkers-oppose-bloombergs-soda-ban.html.
- 34.Harris Interactive. [Accessed December 3, 2013];Many Americans ambivalent over laws aimed at healthy living: poll. Available at: http://www.harrisinteractive.com/NewsRoom/PressReleases/tabid/446/mid/1506/articleId/986/ctl/ReadCustom%20Default/Default.aspx.
- 35.Homans MD. Banning smokers may harm your company’s health. [Accessed December 3, 2013];The Legal Intelligencer. 2012 245(92) Available at: http://www.flastergreenberg.com/media/article/383_Michael%20Homans%20Byline%20Article_May%202012.pdf. [Google Scholar]
- 36. [Accessed December 3, 2013];More workplaces don't allow employees to smoke at work, anywhere. USA Today. Available at: http://www.digtriad.com/news/article/207243/8/Experimental%20Severe%20Weather%20Warnings%20To%20Motivate%20Response.