Abstract
Objective
To describe children’s consumption of sugar-sweetened beverages (SSBs) and 100% fruit juice (FJ), and identify factors that may reduce excessive consumption
Design
830 Parents of young children completed a 36-item questionnaire at the pediatricians’ office.
Results
Children consumed soda (62.2%), other SSBs (61.6%), and fruit juice (88.2%): 26.9% exceeded the American Academy of Pediatrics’ recommended daily FJ intake. 157 (18.9%) children consumed excessive calories (>200kcal/day) from beverages (median 292.2 kcal/day , range 203.8 to 2177.0). Risk factors for excessive calorie consumption from beverages were exceeding recommendations for FJ (OR 119.7, 95%CI 52.2, 274.7), being 7- to 12-years-old (OR 4.3, 95%CI 1.9, 9.9), and having Medicaid insurance (OR 2.6, 95%CI 1.1, 6.0). Parents would likely reduce beverage consumption if recommended by the physician (65.6%).
Conclusions
About one in five children consume excessive calories from soda, other SSBs and FJ, with FJ the major contributor.
Keywords: sugar-sweetened beverages, practice-based research network, fruit juice, intervention strategies, obesity
INTRODUCTION
Excessive calories from beverages may be a modifiable driver of childhood obesity.3 Since 1977, consumption of sugar-sweetened beverages (SSBs, including non-diet soda, fruit drinks, sport drinks, and energy drinks) has doubled and the average portion size has increased by 46%.1 SSBs are energy dense and nutrient limited, and have been linked to an increased risk for obesity,2–8 insulin resistance,9 type 2 diabetes mellitus, 4, 10 and dental caries.11, 12 In addition, excessive consumption of SSBs can result in a poor diet with inadequate intake of micronutrients.13, 14 Consequently, U.S. Dietary Guidelines recommend avoidance of SSBs for all age groups.15, 16
Although often consumed as part of children’s total fruit intake,17 100% fruit juice (FJ) has similar caloric content to SSBs and is another source of additional calories. FJ consumption increases the risk for dental caries,18 and excessive consumption may contribute to obesity.19–21 22 Recommendations regarding FJ in children’s diets are controversial. U. S. Dietary Guidelines recommend FJ as a healthy alternative to SSB;16 however, some public health experts have advocated the elimination of FJ as a mechanism to reduce childhood obesity.23, 24 The American Academy of Pediatrics (AAP) encourages consumption of whole fruit, but suggests FJ can substitute for one daily serving of fruit defined as 4–6 ounces for children 1–6 years of age and 8–12 ounces for children 7–18 years of age.15, 25, 26
Seeking pragmatic options for treatment and prevention of obesity, pediatricians in our practice-based research network indicated that reduction of SSB and FJ consumption may be an effective target for intervention and feasible within the constraints of an office visit. The objectives for this study were to: 1) describe young children’s consumption of SSBs and FJ; 2) identify risk factors for excessive consumption; and 3) understand parents’ beliefs and behaviors regarding consumption of these beverages. This information would inform the development of an intervention to reduce consumption of excessive calories from beverages.
METHODS
Study Population
Pediatricians of the Washington University Pediatric and Adolescent Ambulatory Research Consortium (WU PAARC), a practice-based research network, were asked if they would permit a research assistant (RA) (RKR) to recruit patients for the survey in their waiting room. The study was approved by the Washington University Human Research Protection Office, requiring verbal consent for study enrollment.
Parents or legal guardians with a child between 6 months and 12 years of age were invited to participate in the study by the RA. The parent completed the survey regarding the beverage consumption of the child attending for the office appointment. If more than one child was seeing the doctor, the parent completed the survey on the youngest child in order to best inform an early intervention. Those who were not proficient in English or had already taken a survey were excluded. Parents were not approached by the RA if they were immediately called to see the physician, were preoccupied with an administrative task, or if the RA was busy with another parent.
Survey Tool
The 36-item, self-report questionnaire was developed by the study team based on the literature, informal discussion with parents, and clinical experience, and was finalized after pilot testing with six parents. Questions enquired about the child’s consumption of soda containing sugar, which excludes diet soda; other SSBs (fruit drinks, energy drinks, sports drinks, and any drinks made at home and to which sugar was added); and FJ (100% fruit juice without any added sugars). For each beverage type, parents used a categorical scale to indicate their child’s frequency of consumption in the past month (never, once, 2–3 times, once/week, twice/week, 3–4 times/week, 5–6 times/week, once/day, 2–3 times/day, 4–5 times/ day, ≥ 6 times/day) and average portion size (“just a few sips”, 4 ounces or half a cup, 8 ounces or one cup, 12 ounces or typical can size, 16 ounces or McDonald’s™ small size, 32 ounces or McDonald’s™ large size). Parents selected options from a list to indicate their rationale for providing these beverages and to identify factors that might motivate them to reduce their child’s consumption. Additional questions asked about discussions with the child’s primary care provider (PCP) regarding SSB consumption and their likelihood to follow PCP advice to avoid these beverages. Each survey took approximately five minutes to complete and had a Flesch-Kincaid reading level of 4.9, indicating the survey should be understandable by an average individual with a 5th grade education or higher. Demographic information was also obtained.
For each child, intake in ounces/day for each beverage type were calculated based on the frequency of consumption and portion size; for responses with a range of frequencies (e.g. 3–4 times/week), the lesser frequency was used, and the categories “just a few sips” and “other” were excluded. Calories per ounce were estimated based on the Fat and Calorie Counter provided by the National Diabetes Education Program: 27 non-diet soda: 12.7 kcal/oz, FJ (average Calorie per ounce for orange and apple juice): 14.3 kcal/oz, and other SSBs (average for fruit punch, Gatorade™ and Kool-Aid™): 11.2 kcal/oz. Daily caloric intake for each beverage type was calculated and summed to provide total calories per day/child from beverages. We defined energy excess as > 200 kcal/day, a value estimated from mathematical models of dietary intake survey data from 1977/8 and 1994/6 that indicated a per capita increase of >200kcal/d was associated with pediatric obesity.28
Statistical Analysis
Summary statistics are reported as percentages for categorical variables and mean (standard deviation, sd) or median (range or interquartile range, IQR) for continuous variables. Child ages were split into two categories based on the AAP recommendation for FJ: ≤ 6 years of age, and 7–12 years of age.15, 26
Multivariable logistic regression was used to identify independent risk factors for excessive caloric intake from beverages for which odds ratios (OR) and 95% confidence intervals (CI) are reported. Factors included in the model were: race—African American vs. all other races; health insurance—Medicaid vs. other insurance; respondents’ educational attainment—college degree (Associate’s or higher) vs. no college degree; family income— <$30,000/year vs. ≥$30,000/year; exceeding the AAP recommendations for daily FJ consumption; age-group of the child; keeping track of the child’s beverage consumption – usually/always vs. never/rarely/sometimes; perceived control over what the child drinks – a lot vs. none/some; and concern about the child becoming overweight.
All statistical analyses were performed using STATA 11 (StataCorp LP, College Station, TX). Pearson Chi-square tests were performed for between-group analyses. A probability of p < 0.05 (two-tailed) was used to determine statistical significance.
RESULTS
Study Participants
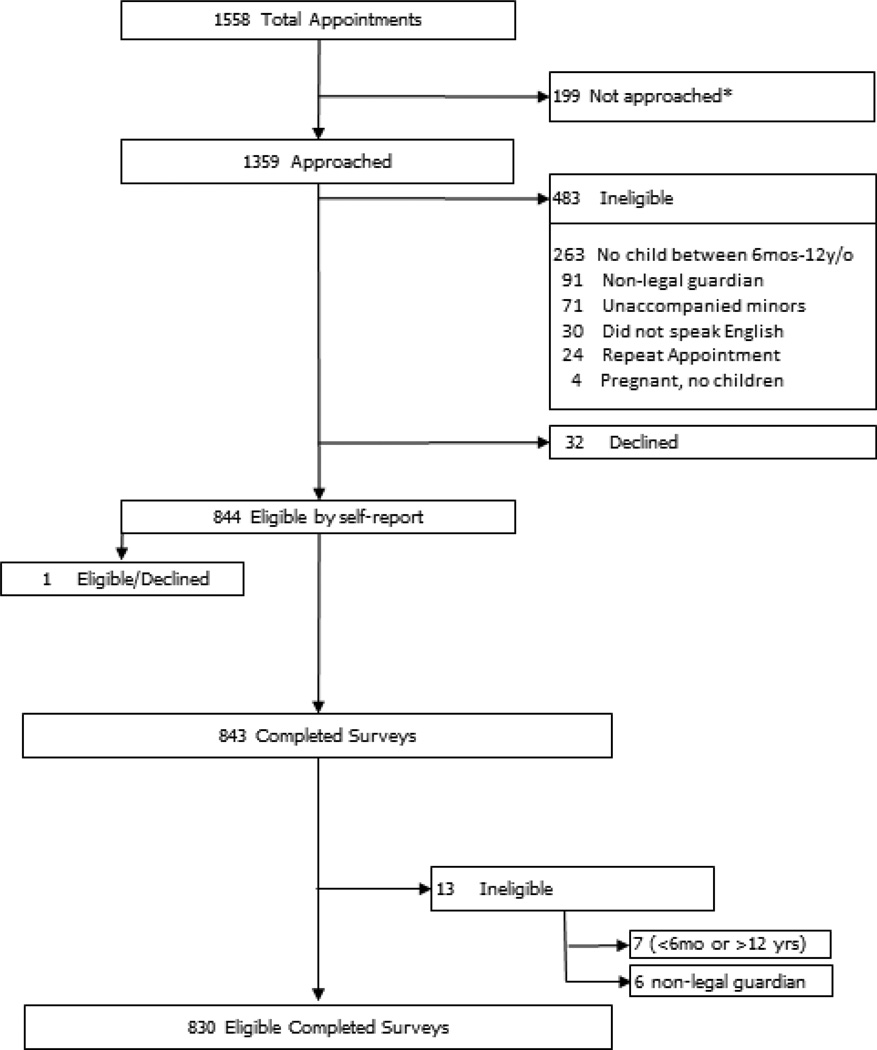
Fifteen of 34 (44.1%) WU PAARC practices agreed to participate in the study. Practices were located throughout the St. Louis metropolitan area (13 Missouri, 2 Illinois; 12 group practices, 3 solo practitioners). A total of 830 surveys were collected between December 4, 2012 and April 16, 2013 (median 58 surveys per practice, range 15 to 93). The RA was at each practice for a median of 3.5 days (range 2 – 4 days). Of the 1,359 individuals who were invited to participate, 496 were ineligible and 33 declined (participation rate: 96.2%) (Figure 1). Most (83.8%) respondents were the child’s mother, 20.5% were African American, 27.7% had Medicaid coverage, and 63% had attained an associate’s degree or higher (Table 1).
Figure 1. Eligibility flowchart.
*Parents were not approached by the research assistant (RA) if they were immediately called back to see the physician, were preoccupied with an administrative task, or if the RA was busy with another parent.
Table 1.
Characteristics of survey respondents (N = 830)
| Survey respondent | %† |
|---|---|
| Relationship to child | |
| Mother | 83.8% |
| Father | 15.4% |
| Other | 0.9% |
| Racial group | |
| White | 76.2% |
| Black | 20.5% |
| Asian | 1.2% |
| Other | 2.0% |
| Hispanic | 2.7% |
| Educational level | |
| Grade 1 through 8 | 0.6% |
| High school, no diploma | 3.5% |
| High school graduate or GED | 11.9% |
| College – no degree | 21.0% |
| Associate’s degree or equivalent | 16.3% |
| Bachelor’s degree | 25.5% |
| Graduate or professional degree | 21.2% |
| Family characteristics | %† |
| Child’s age in years (Median, Interquartile range) | 4.0 (2–8) |
| Age groups (n, %) | |
| 6 months of age to <7 years of age | 565 (68.1%) |
| 7–12 years of age | 265 (31.9%) |
| Child’s gender - Male | 55.4% |
| Two-parent family | 79.9% |
| Family income/year (n=784) | |
| < $30,000 | 23.9% |
| $30,000 to < $60,000 | 22.6% |
| $60,000 to < $100,000 | 26.7% |
| $100,000 or more | 26.9% |
| Health insurance | |
| Work-related insurance | 68.2% |
| Medicaid | 27.7% |
| Self-pay | 3.7% |
| Other | 0.4% |
When data are less than 95% of the total survey population, n is provided.
Percentages may not sum to 100% due to rounding.
Beverage Consumption
Consumption patterns for soda, other SSBs, and FJ are reported in Table 2. Within the past month, only 6.9% of children had not consumed at least one of these beverages (10.1% <6 years of age, 0% 7–12 year-olds, p<0.001): 37.8% had not consumed soda, 38.4% had not consumed other SSBs, and 11.8% had not consumed FJ. The most frequently consumed beverage was FJ. Of the 687 respondents who drank FJ and provided information to allow calculation of ounces consumed, 26.9% exceeded the AAP’s recommendations (34.0% ≤ 6 years of age; 13.5% 7–12 year-olds, p<0.001).
Table 2.
Reported beverage consumption for the past month
| Reported beverage consumption frequency: |
Soda | Other SSBs |
FJ |
|---|---|---|---|
| N* | 828 | 820 | 824 |
| Never | 37.8% | 38.4% | 11.8% |
| 1–3 times per month | 37.8% | 28.7% | 18.5% |
| 1–4 times per week | 21.0% | 21.8% | 34.8% |
| 5 or more times per week | 3.3% | 12.2% | 34.9% |
| Average portion size: | |||
| N** | 511 | 505 | 725 |
| Just a few sips | 15.1% | 6.6% | 3.2% |
| 4 ounces | 27.2% | 28.5% | 39.0% |
| 8 ounces | 27.8% | 45.7% | 46.8% |
| 12 ounces | 20.6% | 13.4% | 6.3% |
| 16 ounces | 5.1% | 4.4% | 2.8% |
| 32 ounces | 0.6% | 0.8% | 0.4% |
| Other | 3.7% | 0.6% | 1.5% |
N less than 830 due to missing responses to sections of the survey
Portion size sample size excluded those who answered that their child had not consumed the beverage in the past month.
SSB = sugar-sweetened beverage
FJ=100% fruit juice
Caloric intake
On average, children who drank these beverages consumed an additional 116.98 kcal/day (sd 193.3) with no difference by age group (p=0.42). 157 (18.9%) consumed excessive calories (>200 kcal/day).28 Among these children, the average kcal/day due to soda, other SSBs and FJ were 44.3 kcal/day (sd 74.6), 122.5 kcal/d (sd 180.1), and 293.4 kcal/d (sd 228.5), respectively.
In the multivariable logistic regression model (pseudo R2 0.51), three factors increased the likelihood of excessive calorie consumption from beverages: drinking more than the recommended daily FJ servings for their age group (OR 119.7, 95%CI 52.2 to 274.7), being in the older age group (OR 4.3, 95%CI 1.9 to 9.9), and Medicaid insurance (OR 2.6, 95%CI 1.1 to 6.0). Two factors were protective: parental report of “usually” or “always” tracking their child’s caloric beverage consumption (OR 0.38, 95%CI 0.19 to 0.76) and maintaining “a lot” of control over their child’s beverage options (OR 0.38, 95%CI 0.15 to 0.97).
Context of beverage use
For children who drank soda, most did so at home (51.6%), in fast food restaurants (49.5%), or at other types of restaurants (31.7%). Twenty-one percent of parents reported they had soda available in the home all the time (58.8% “once in a while”, 20.2% never).
The majority (90.4%) of parents felt they had a lot of control over what their child drank (9.3% some control), but varied in the frequency they kept track of the child’s beverage consumption (55% always, 23.3% usually, 12.3% sometimes, 9.4% rarely or never). Few (4.1%) believed their child was overweight, with no difference by level of calorie consumption by beverages (excessive calories, 5.3%; others, 3.8%, p=0.49); the majority (58.7%) of parents were not concerned about their child becoming overweight (25.1% concerned; 16.2% very concerned). For soda, other SSBs, and FJ, the most common reasons parents indicated that their child consumed the beverage were as a treat and because the child requested it (Table 3). Many parents (33.4%) provided FJ because they thought it was good for their child.
Table 3.
Parental reasons for child’s beverage consumption
| All SSBsb | FJ | |
|---|---|---|
| Na | 644 | 727 |
| Reason the child drinks the beverage: | ||
| It’s a treat | 64.3% | 24.6% |
| It’s what they ask for | 37.7% | 45.4% |
| It’s good for the child | 2.2% | 33.4% |
| It’s what other people in the house drink | 14.6% | 13.2% |
| Taste is preferred by the child over water or milk | 13.7% | 14.6% |
| It’s what the parents drink | 16.8% | 11.7% |
| It’s convenient | 16.6% | 9.8% |
| It’s inexpensive | 8.1% | 2.8% |
| It’s what their friends drink | 6.2% | 2.2% |
| It’s able to keep the child quiet | 2.2% | 1.4% |
SSBs = sugar-sweetened beverages; FJ=100% fruit juice
Respondents whose children had not consumed the beverage in the past month were excluded.
Respondents who selected the item for either soda or other SSBs were counted as an affirmative response for all SSBs.
Potential opportunities to reduce use
Across all SSBs and FJ, the factors parents selected as potential motivators to reduce caloric beverage consumption by their child were similar (Table 4). Most commonly selected items were if a PCP recommended limiting consumption of the beverage, and if consumption of the beverage was not healthy, made the child overweight, or damaged their teeth. Almost all respondents said they would follow SSB consumption advice from a doctor (82.5% very likely, 16.4% likely) or a nurse (68.8% very likely, 27.6% likely). Most parents (90.7%) would prefer to get information regarding their child’s diet from their physician versus a health educator (29.8%) or a brochure (22.7%). However, only 59% stated their pediatrician had discussed SSB consumption during an office visit.
Table 4.
Reasons parent may reduce their child’s beverage consumption by beverage type
| All SSBsb | FJ | |
|---|---|---|
| Na | 644 | 727 |
| Reasons for reducing beverage consumption | ||
| If it was not healthy for children | 57.9% | 64.4% |
| If the doctor recommended limiting intake | 50.9% | 54.9% |
| If it made their child overweight | 49.7% | 50.2% |
| If it damaged their child’s teeth | 47.7% | 51.0% |
| If the parent stopped buying it | 38.4% | 25.5% |
| If there was a warning label on the packaging | 30.4% | 30.3% |
| If the parent stopped drinking it | 27.3% | 10.9% |
| If the price went up | 17.2% | 10.2% |
| If it was not available in school | 9.5% | 8.3% |
| If the child’s friends stopped drinking it | 10.6% | 4.7% |
SSBs = sugar-sweetened beverages; FJ=100% fruit juice
Respondents whose children had not consumed that particular beverage in the past month were excluded.
Respondents who selected the item for either soda or other SSBs were counted as an affirmative response for all SSBs.
DISCUSSION
Our findings suggest that interventions to reduce excessive calorie intake from beverages are needed. They also provide insight into intervention development that can be incorporated at the PCP level. In the study population, one in five children consumed excessive calories, ranging from 200–2200 kcal/day, from soda, other SSBs (such as sports drinks), and 100% FJ. As children do not compensate for additional liquid calories with reduced dietary intake,29 it is reasonable to suggest excessive consumption of these beverages will increase the risk of obesity. Interventions to address excessive beverage consumption should be broad in scope. In addition to targeting soda, they should address consumption of other SSBs, such as sports drinks and 100% FJ. Of the three beverage types evaluated, FJ was the largest provider of excess calories, particularly for younger children. In contrast to soda and other SSBs typically provided infrequently as a treat, parents believed FJ to be a healthy beverage choice and often provided more than the recommended daily serving. Interventions that increase parents’ awareness of the recommended limited use of FJ and the potential health risks for their child associated with excessive FJ consumption may be effective, whereas interventions focusing exclusively on SSBs may miss key caloric contributors. Interventions targeting younger children are warranted, as childhood obesity is most likely to occur among children who are overweight on entry to kindergarten.30 Also, acclimating young children to sweet tasting beverages may lead to poor long-term eating behaviors.31–33 Finally, encouraging parents to control and monitor their child’s consumption of SSBs and FJ may protect against excessive calorie consumption and be more acceptable to parents than complete elimination.
PCPs have the potential to play a large role in the reduction of excessive calories from beverages. While almost all parents in the study population indicated they would follow the advice of their child’s physician regarding the consumption of these drinks, a third reported their pediatrician had not discussed SSB consumption with them. Observational studies suggest that substituting water for SSB and FJ would reduce total energy intake in children,29 and reducing FJ consumption with fresh fruit may provide additional health benefits from improved dietary fiber.17 Yet, few interventions have targeted reduction of excessive calorie consumption from beverages. Although the effects were modest, two school-based programs reduced SSB consumption in healthy 7- to 11-year-olds with an associated reduction in the number of overweight and obese children.34, 35 One program was an educational intervention34 and the other used beverage replacement.35 A 12-month home-based program to replace excessive SSB consumption with water or diet soda for overweight adolescents resulted in reduced weight gain.36 Primary care-based interventions to prevent or reduce childhood obesity usually use a comprehensive approach targeting multiple behaviors. 37 38–40 However, addressing obesity may be a daunting prospect for the PCP due to perceived ineffectiveness of current obesity treatments,41–44 parental resistance,43, 45 and concern about reimbursement.41, 43, 45 Future studies will evaluate if targeted messages that focus on consumption of excessive calories from beverages are effective and feasible in a busy practice setting.
There are study limitations that should be noted. This survey has not been validated, although the questions posed in this survey are similar to those used in National surveys that also use a 30-day recall.46 The data are self-reported and the only guidance for parents for determining portion size was reference to well-known serving sizes. Thus, measures of beverage consumption may be prone to social desirability bias and may be either under- or over-reported.47, 48 Parents might have misconstrued the difference between fruit drinks and FJ, leading to an overestimation of FJ consumption. Exclusion of calories consumed from “just a few sips” reported as the serving size for any of the beverages may have underestimated average calorie consumption. While the study population was large, it was localized to the St. Louis metropolitan area; therefore, study findings may not be generalizable to other communities.
CONCLUSIONS
Excessive consumption of calories from beverages is common in children, with FJ the main contributor. A PCP-based intervention with the goal to reduce consumption of FJ and SSBs in younger children by discussing broad health-related effects of excessive consumption and emphasizing the potential benefits of drinking solely milk and water would be merited.
ACKNOWLEDGMENTS
We are indebted to the physicians and office staff at Caryn Garriga General & Developmental Pediatrics, Children’s Clinic, Esse Health – Creve Coeur Pediatrics, Esse Health – Florissant Pediatrics, Esse Health – Pediatric and Adolescent Medicine at Watson Road, Forest Park Pediatrics, Heartland Pediatrics – Collinsville, Johnson Pediatrics, Nagireddi Pediatrics, Patients First: Pediatrics - Washington, Pediatric Healthcare Unlimited, Southwest Pediatrics, Strashun Pediatrics, St. Louis Pediatrics Practitioners, Tots Thru Teens Pediatrics, for agreeing to participate in this study. We thank Elizabeth Winright, MA, Washington University School of Medicine, for her assistance in data collection, entry and verification.
Study data were collected and managed using REDCap electronic data capture tools hosted at Washington University. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing: 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.
This study was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and the Children’s Discovery Institute (grant LI-2012-200).
Role of the Sponsors: This study’s contents are solely the responsibility of the author and do not necessarily represent the official view of NCATS, or NIH. The sponsors had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Mr. Rader wrote the first draft of the manuscript and no honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
Abbreviations
- AAP
American Academy of Pediatrics
- CI
confidence interval
- NCATS
National Center for Advancing Translational Sciences
- NIH
National Institutes of Health
- OR
odds ratio
- PCP
primary care provider
- RA
research assistant
- SD
standard deviation
- SSB
sugar-sweetened beverage
- WU PAARC
Washington University Pediatric and Adolescent Ambulatory Research Consortium
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
Author Contributions: Study concept and design: Garbutt, Strunk, Sterkel. Acquisition of data: Rader. Analysis and interpretation of data: Garbutt, Mullen, Rader, Strunk, Sterkel. Drafting of the manuscript: Rader, Garbutt. Critical revision of the manuscript for important intellectual content: Garbutt, Strunk, Sterkel, Mullen, Rader. Statistical analysis: Garbutt, Mullen, Rader. Obtained funding: Garbutt. Administrative, technical, and material support: Mullen. Study supervision: Garbutt, Strunk.
Dr. Garbutt and Ms. Mullen had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Nielsen SJ, Popkin BM. Changes in beverage intake between 1977 and 2001. Am J Prev Med. 2004;27:205–210. doi: 10.1016/j.amepre.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 2.Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiol Behav. 2010;100:47–54. doi: 10.1016/j.physbeh.2010.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tam CS, Garnett SP, Cowell CT, Campbell K, Cabrera G, Baur LA. Soft drink consumption and excess weight gain in Australian school students: results from the Nepean study. Int J Obes (Lond) 2006;30:1091–1093. doi: 10.1038/sj.ijo.0803328. [DOI] [PubMed] [Google Scholar]
- 4.Malik VS, Popkin BM, Bray GA, Despres JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–1364. doi: 10.1161/CIRCULATIONAHA.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health. 2007;97:667–675. doi: 10.2105/AJPH.2005.083782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grimes CA, Riddell LJ, Campbell KJ, Nowson CA. Dietary salt intake, sugar-sweetened beverage consumption, and obesity risk. Pediatrics. 2013;131:14–21. doi: 10.1542/peds.2012-1628. [DOI] [PubMed] [Google Scholar]
- 7.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr. 2006;84:274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeBoer MD, Scharf RJ, Demmer RT. Sugar-sweetened beverages and weight gain in 2- to 5-year-old children. Pediatrics. 2013;132:413–420. doi: 10.1542/peds.2013-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kondaki K, Grammatikaki E, Jimenez-Pavon D, et al. Daily sugar-sweetened beverage consumption and insulin resistance in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr. 2013;16:479–486. doi: 10.1017/S1368980012002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malik VS, Hu FB. Sweeteners and Risk of Obesity and Type 2 Diabetes: The Role of Sugar-Sweetened Beverages. Curr Diab Rep. 2012 doi: 10.1007/s11892-012-0259-6. [DOI] [PubMed] [Google Scholar]
- 11.Armfield JM, Spencer AJ, Roberts-Thomson KF, Plastow K. Water fluoridation and the association of sugar-sweetened beverage consumption and dental caries in Australian children. Am J Public Health. 2013;103:494–500. doi: 10.2105/AJPH.2012.300889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lim S, Sohn W, Burt BA, et al. Cariogenicity of soft drinks, milk and fruit juice in low-income african-american children: a longitudinal study. J Am Dent Assoc. 2008;139:959–967. doi: 10.14219/jada.archive.2008.0283. quiz 95. [DOI] [PubMed] [Google Scholar]
- 13.Harnack L, Stang J, Story M. Soft drink consumption among US children and adolescents: nutritional consequences. J Am Diet Assoc. 1999;99:436–441. doi: 10.1016/S0002-8223(99)00106-6. [DOI] [PubMed] [Google Scholar]
- 14.Frary CD, Johnson RK, Wang MQ. Children and adolescents' choices of foods and beverages high in added sugars are associated with intakes of key nutrients and food groups. J Adolesc Health. 2004;34:56–63. doi: 10.1016/s1054-139x(03)00248-9. [DOI] [PubMed] [Google Scholar]
- 15.Gidding SS, Dennison BA, Birch LL, et al. Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006;117:544–559. doi: 10.1542/peds.2005-2374. [DOI] [PubMed] [Google Scholar]
- 16.Dietary Guidelines for Americans, 2010. Services. 7th ed. Washington, D.C.: U.S. Government Printing Office; 2010. USDoAaUSDoHaH, ed. [Google Scholar]
- 17.Monsivais P, Rehm CD. Potential nutritional and economic effects of replacing juice with fruit in the diets of children in the United States. Arch Pediatr Adolesc Med. 2012;166:459–464. doi: 10.1001/archpediatrics.2011.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marshall TA, Levy SM, Broffitt B, et al. Dental caries and beverage consumption in young children. Pediatrics. 2003;112:e184–e191. doi: 10.1542/peds.112.3.e184. [DOI] [PubMed] [Google Scholar]
- 19.Dennison BA, Rockwell HL, Baker SL. Excess fruit juice consumption by preschool-aged children is associated with short stature and obesity. Pediatrics. 1997;99:15–22. [PubMed] [Google Scholar]
- 20.Faith MS, Dennison BA, Edmunds LS, Stratton HH. Fruit juice intake predicts increased adiposity gain in children from low-income families: weight status-by-environment interaction. Pediatrics. 2006;118:2066–2075. doi: 10.1542/peds.2006-1117. [DOI] [PubMed] [Google Scholar]
- 21.Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA. 2004;292:927–934. doi: 10.1001/jama.292.8.927. [DOI] [PubMed] [Google Scholar]
- 22.O'Neil CE, Nicklas TA, Rampersaud GC, Fulgoni VL., 3rd 100% orange juice consumption is associated with better diet quality, improved nutrient adequacy, decreased risk for obesity, and improved biomarkers of health in adults: National Health and Nutrition Examination Survey, 2003–2006. Nutr J. 2012;11:107. doi: 10.1186/1475-2891-11-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wojcicki JM, Heyman MB. Reducing childhood obesity by eliminating 100% fruit juice. Am J Public Health. 2012;102:1630–1633. doi: 10.2105/AJPH.2012.300719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nicklas T, Kleinman RE, O'Neil CE. Taking into account scientific evidence showing the benefits of 100% fruit juice. Am J Public Health. 2012;102:e4. doi: 10.2105/AJPH.2012.301059. author reply e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stallings VA, Yaktine AL Institute of Medicine (U.S.) Nutrition standards for foods in schools : leading the way toward healthier youth. Washington, D.C.: National Academies Press; 2007. Committee on Nutrition Standards for Foods in Schools. [Google Scholar]
- 26.Committee on Nutrition. American Academy of Pediatrics: The use and misuse of fruit juice in pediatrics. Pediatrics. 2001;107:1210–1213. doi: 10.1542/peds.107.5.1210. [DOI] [PubMed] [Google Scholar]
- 27.Wing RR. In: Fat and Calorie Counter. Gillis B, editor. University of Pittsburgh; 1996. [Google Scholar]
- 28.Hall KD, Butte NF, Swinburn BA, Chow CC. Dynamics of childhood growth and obesity: development and validation of a quantitative mathematical model. The lancet Diabetes & endocrinology. 2013;1:97–105. doi: 10.1016/s2213-8587(13)70051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang YC, Ludwig DS, Sonneville K, Gortmaker SL. Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Arch Pediatr Adolesc Med. 2009;163:336–343. doi: 10.1001/archpediatrics.2009.23. [DOI] [PubMed] [Google Scholar]
- 30.Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. The New England journal of medicine. 2014;370:403–411. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ford CN, Slining MM, Popkin BM. Trends in dietary intake among US 2- to 6-year-old children, 1989-2008. J Acad Nutr Diet. 2013;113:35–42. doi: 10.1016/j.jand.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Birch L, Savage JS, Ventura A. Influences on the Development of Children's Eating Behaviours: From Infancy to Adolescence. Can J Diet Pract Res. 2007;68:s1–s56. [PMC free article] [PubMed] [Google Scholar]
- 33.Beauchamp GK, Moran M. Dietary experience and sweet taste preference in human infants. Appetite. 1982;3:139–152. doi: 10.1016/s0195-6663(82)80007-x. [DOI] [PubMed] [Google Scholar]
- 34.James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. Bmj. 2004;328:1237. doi: 10.1136/bmj.38077.458438.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. The New England journal of medicine. 2012;367:1397–1406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 36.Ebbeling CB, Feldman HA, Chomitz VR, et al. A randomized trial of sugar-sweetened beverages and adolescent body weight. The New England journal of medicine. 2012;367:1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Resnicow K, McMaster F, Woolford S, et al. Study design and baseline description of the BMI2 trial: reducing paediatric obesity in primary care practices. Pediatr Obes. 2012;7:3–15. doi: 10.1111/j.2047-6310.2011.00001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity: a feasibility study. Arch Pediatr Adolesc Med. 2007;161:495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 39.Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA. 2007;297:2697–2704. doi: 10.1001/jama.297.24.2697. [DOI] [PubMed] [Google Scholar]
- 40.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch Pediatr Adolesc Med. 2011;165:714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Silberberg M, Carter-Edwards L, Murphy G, et al. Treating pediatric obesity in the primary care setting to prevent chronic disease: perceptions and knowledge of providers and staff. N C Med J. 2012;73:9–14. [PMC free article] [PubMed] [Google Scholar]
- 42.Jelalian E, Boergers J, Alday CS, Frank R. Survey of physician attitudes and practices related to pediatric obesity. Clin Pediatr (Phila) 2003;42:235–245. doi: 10.1177/000992280304200307. [DOI] [PubMed] [Google Scholar]
- 43.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110:210–214. [PubMed] [Google Scholar]
- 44.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. J Am Diet Assoc. 2006;106:2024–2033. doi: 10.1016/j.jada.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 45.Boyle M, Lawrence S, Schwarte L, Samuels S, McCarthy WJ. Health care providers' perceived role in changing environments to promote healthy eating and physical activity: baseline findings from health care providers participating in the healthy eating, active communities program. Pediatrics. 2009;123(Suppl 5):S293–S300. doi: 10.1542/peds.2008-2780H. [DOI] [PubMed] [Google Scholar]
- 46.The National Health and Nutrition Examination Survey (NHANES) [Accessed February 3, 2014];Centers for Disease Control and Prevention. 2014 (at http://www.cdc.gov/nchs/nhanes.htm.)
- 47.Champagne CM, Baker NB, DeLany JP, Harsha DW, Bray GA. Assessment of energy intake underreporting by doubly labeled water and observations on reported nutrient intakes in children. J Am Diet Assoc. 1998;98:426–433. doi: 10.1016/S0002-8223(98)00097-2. [DOI] [PubMed] [Google Scholar]
- 48.Krebs-Smith SM, Graubard BI, Kahle LL, Subar AF, Cleveland LE, Ballard-Barbash R. Low energy reporters vs others: a comparison of reported food intakes. Eur J Clin Nutr. 2000;54:281–287. doi: 10.1038/sj.ejcn.1600936. [DOI] [PubMed] [Google Scholar]