Abstract
Majority of patients with head and neck cancer are treated with combined treatment regimes such as surgery, radiation therapy, and chemotherapy. The loss of structural symmetry and imaging landmarks as a result of therapy makes post-treatment imaging a daunting task on conventional modalities like computed tomography (CT) scan and magnetic resonance imaging (MRI) as well as on 18 Fluorine-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography (18F FDG PET/CT). Combined multimodality treatment approach causes various tissue changes that give rise to a spectrum of findings on FDG PET/CT imaging, which are depicted in this atlas along with a few commonly encountered imaging pitfalls. The incremental value of FDG PET/CT in detecting locoregional recurrences in the neck as well as distant failures has also been demonstrated.
Keywords: Computed tomography, FDG PET flap, head and neck, infection, inflammation, radiation therapy
INTRODUCTION
The use of various imaging techniques in post-treatment assessment of head–neck cancer is gradually on the rise, though clinical examinations at periodic intervals still remains the mainstay of follow-up. 18F FDG PET/CT is increasingly used in the post-treatment setting to diagnose residual/recurrent disease early so that appropriate treatment can be initiated. The effects of multimodality treatment such as surgery, radiation, and chemotherapy can distort normal anatomical landmarks induce inflammation and infection, which can mask disease. It is important to understand the anatomical and functional effects as well as complications produced by these treatment modalities in order to diagnose the resultant imaging pitfalls on FDG PET/CT. Knowledge of the common and unusual patterns of loco-regional recurrent disease and distant metastases on FDG PET/CT is also crucial in the post-treatment assessment of head-neck cancer patients.
TISSUE CHANGES AFTER RADIATION THERAPY
Radiation therapy alone or in combination with chemotherapy is often used to treat head-neck cancer patients. There are several tissue changes, which are a result of early reaction to radiation. These include thickening of the skin and platysma, stranding of the subcutaneous fat, pharyngeal and laryngeal wall thickening and increased vascularity of the major and minor salivary glands.[1] Edema, inflammation, and increased vascularity in these structures lead to a pattern of FDG uptake which is low grade, diffuse, symmetrical, and restricted to the radiation field [Figure 1]. These findings are seen during the course or within 3 months of radiation therapy and are often reversible.[2] Several muscle groups within the radiation field also demonstrate an elevated FDG activity which can be potentially confused with neoplastic uptake.[3] Occasionally, uptake can be asymmetric and focal and can potentially mimic disease.[4] However, absence of a mass lesion on CT and reduction over time differentiate an inflammatory or physiological uptake from disease.
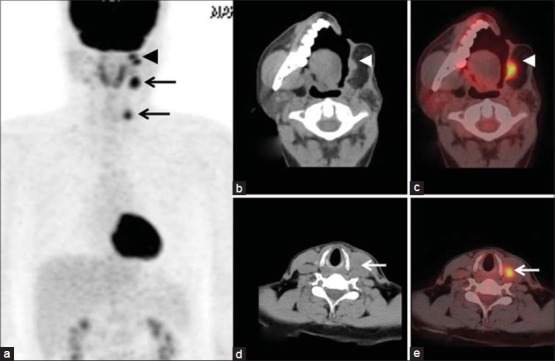
Figure 1.
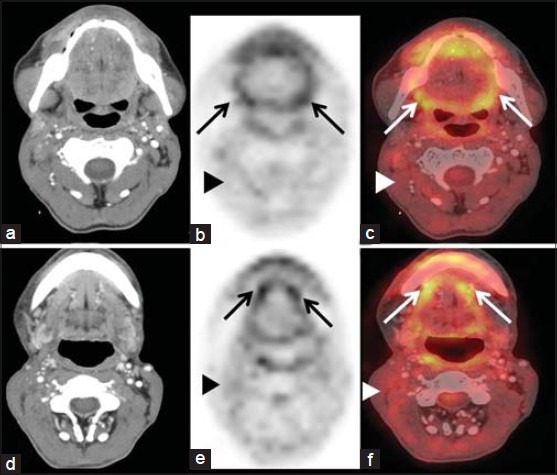
Tissue changes after radiation therapy. Axial PET and fused PET/CT images show diffuse symmetrical FDG uptake in the tongue and oropharynx (arrows in the b and c) and in the floor of mouth (arrows in e and f). Diffuse low intensity FDG uptake is also seen in the neck muscles (arrowheads in b,c,e,f). Diffuse uptake is seen within a few days of radiation and can last up to 8–10 weeks
Timing of PET/CT after radiation therapy is an important and often debated clinical issue. Performing PET/CT as early as possible to detect recurrent disease seems logical as salvage treatment can be initiated early enough to derive the best possible clinical benefit. However, studies performed too early may lead to false positive as well as false negative results. Post-treatment inflammation results in false positivity with resultant reduction in the specificity. Possible mechanism for false negative studies has been attributed to radiation induced vascular damage, which temporarily prevents concentration of radiotracer in the viable tumor cells.[5] Imaging after a further few weeks delay in such cases may allow accumulation of tracer in the viable cells leading to a true positive PET result. Waiting too long to image might result in a loss of therapeutic window and also a more complicated surgical procedure due to fibrosis setting in. In order to strike a balance between misleading PET results when study is performed early and the clinical drawbacks of imaging late, a time interval of 12 weeks after completion of radiation therapy is generally recommended.[6,7] Absence of FDG uptake at both the primary and nodal sites has a high negative predictive value in ruling out residual disease [Figure 2].[8,9] Studies have shown that a negative PET scan can potentially defer planned neck dissections after chemo-radiation therapy.[10]
Figure 2.
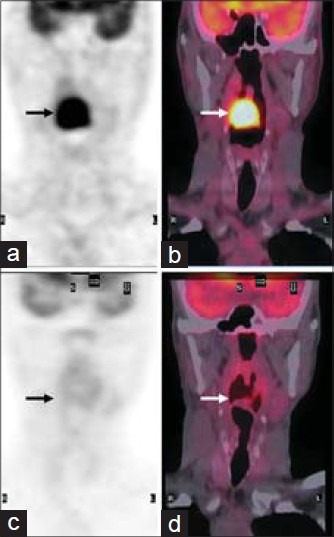
Response to chemo-radiation therapy. Pretreatment coronal fused PET/CT CT studies show FDG avid right sided hypopharyngeal mass (arrow in a and b). Study performed 8 weeks after completion of chemo-radiation therapy show complete metabolic and morphologic response (arrow in c and d) which rules out the possibility of residual disease
TISSUE CHANGES AFTER SURGERY
Curative resection involves complex surgical procedures, which result in loss of symmetry and anatomical landmarks. Various reconstructive techniques are used to close the surgical defects and restore function which produces characteristic well-recognizable imaging findings.
Procedures such as glossectomy, marginal or segmental mandibulectomy, maxillectomy leave large surgical defects, which are closed by flaps and grafts. Pectoralis myocutaneous flap is an example of a composite flap which is often used for reconstruction of large surgical defects in the face, tongue, and skull base.[11] They can be recognized by the well marginated soft tissue/muscle density at the site of the defect and is often accompanied by fat density [Figure 3a, b] produced by a denervation atrophy and fatty replacement of the muscle.[12,13] Normal symmetric pattern of tracer concentration is disturbed due to absence of physiological FDG uptake at the resected and reconstructed site [Figure 3b and d]. In patients undergoing total laryngo-pharyngectomy, a neopharynx is reconstructed which can be recognized as a simple tubular structure sans the accompanying complex anatomy of hypopharynx and larynx [Figure 4]. The neopharynx is often constructed by using a jejunal free flap, which is recognised recognized by the mesenteric fat along with its native vessels.
Figure 3.
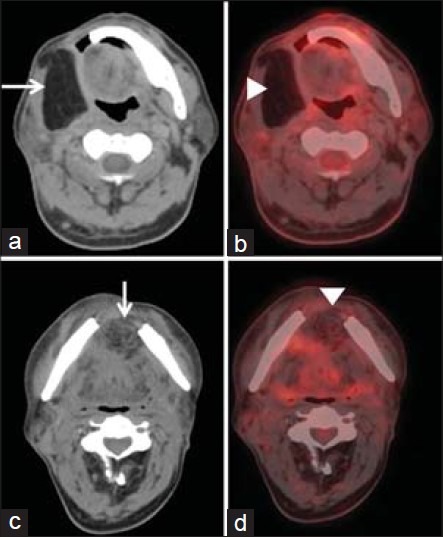
Tissue changes after surgery. Axial fused PET/CT images show myocutaneous flap with fat density used to reconstruct the defect after hemimandibulectomy (arrow in a) and mandibular symphysectomy (arrow in b) performed for buccal cancer absence of normal physiological FDG uptake in the reconstructed flap (arrowheads in a and b)
Figure 4.
Tissue changes after surgery. Axial CT shows a reconstructed neopharynx after a laryngopharyngectomy seen as a tubular structure (arrow in a). Diffuse low grade physiological uptake is seen around the neopharynx (arrow head in b)
PITFALLS
During or after the course of treatment pitfalls in image interpretation can occur due to several factors. Asymmetric nature of physiological uptake, inflammations/infective processes, and treatment-related complications are some of the common causes of false positive results leading to imaging pitfalls.
Pitfalls due to physiological uptake
Sometimes, as a consequence of late effects of radiation therapy, there is a reduction of the normal physiological FDG uptake in structures such as the salivary glands and pharyngeal mucosal lining on the side of the therapy, leading to an appearance of asymmetric increased uptake in the normal tissues on the contralateral side [Figure 5].
Figure 5.
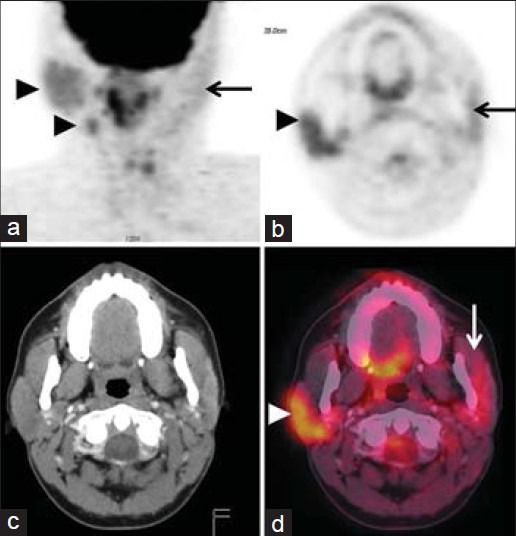
Pitfalls due to asymmetric physiological uptake. Coronal and axial (PET) and fused PET/CT images show reduction in physiological uptake (arrows in a,b,d) on the left side due to long term effects of radiation therapy. Note the relative increase in physiological uptake in the parotid and submandibular glands and the oropharynx on the contralateral normal side which can mimic pathology (arrowheads in a and d)
Absence of physiological FDG uptake in the region of the surgically removed part and persistence of physiological uptake in the normal contralateral side produces an appearance of asymmetric tracer concentration that can mimic disease [Figure 6].[14] Occasionally, after partial resection of an organ such as the tongue, the remnant portion retains its physiological uptake, which appears focal in nature mimicking disease [Figure 7]. After extensive jaw surgeries and reconstructive procedures, the altered mechanics of mastication can result in physiologically increased focal uptake in the adjacent masticator muscles that can be mistaken for disease [Figure 8].
Figure 6.
Pitfalls of due asymmetric physiological uptake. Axial CT shows changes of right hemiglossectomy with a myocutaneous flap containing fat (arrowhead in a). Axial PET and fusion PET/CT show physiological uptake in the remnant tongue which is focal and asymmetric in nature (arrows in b and c) and can potentially mimic disease
Figure 7.
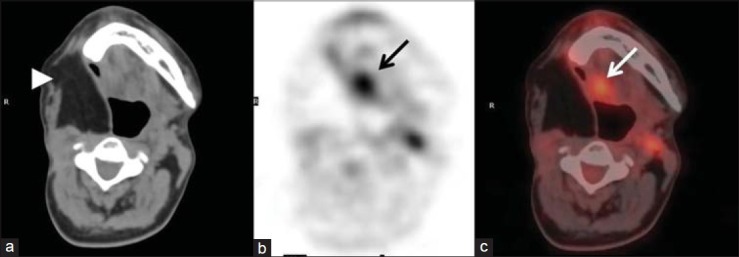
Pitfalls of due asymmetric physiological uptake. Surgery and radiation therapy on the left side of the oral cavity. Coronal PET and fusion PET/CT show physiological uptake along the right side of the oral cavity and the floor of mouth which is asymmetric in nature (arrows in b and c) and can potentially mimic disease. Note the absence of normal physiological uptake on the left side (arrowheads in b and c). This pattern was seen more than a year after treatment
Figure 8.

Pitfalls of due asymmetric physiological uptake. Axial PET and fusion PET/CT show focal asymmetric uptake in the left masseter which is physiological in nature (arrows in a and b) and is produced due to altered mechanics of mastication secondary to jaw surgery
Physiological uptake in the tongue tip and oral cavity arising due to close approximation of tongue and palate, buccal and gingival mucosae can be better resolved by performing certain maneuvers like puffing the cheek and placing a gauzegauze that can help mouth opening.
Pitfalls due to treatment related complications
Complications can arise after both surgery and radiation therapy. Surgical complications occur early and include serous collections, infections, abscess and fistula formation, flap necrosis. Benign serous collections are self-limiting and should be distinguished from infected abscesses that might need a drainage procedure. Benign serous collections also called seromas usually do not show any FDG avidity unless they get infected. On FDG PET/CT abscesses show a rim of tracer uptake in the periphery with a photopenic center which corresponds to a hypodense collection on CT with air pockets seen occasionally. Linear FDG uptake is seen along the fistulous communications associated with abscesses [Figure 9]. These complications occur at the site of surgical resection and reconstructed flaps in the head–neck region. Rarely, one can come across infections/inflammations at the site of the donor flap in the chest or the abdominal wall and focal tracer uptake in this region can potentially mimic metastatic disease [Figure 10].
Figure 9.
Pitfalls due to treatment related complications (surgery). Post surgery and radiation therapy for oral cavity cancer. Axial fused PET/CT shows an intense focus of FDG uptake in the infratemporal fossa mimicking disease recurrence (arrow in b). Corresponding contrast CT image shows a hypodense collection with an air pocket (arrow in a) suggestive of an abscess. Note the linear FDG uptake along the enhancing fistulous tract opening on the skin surface. (arrowheads in a and b)
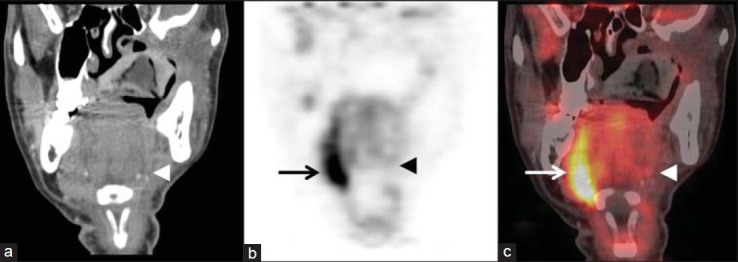
Figure 10.
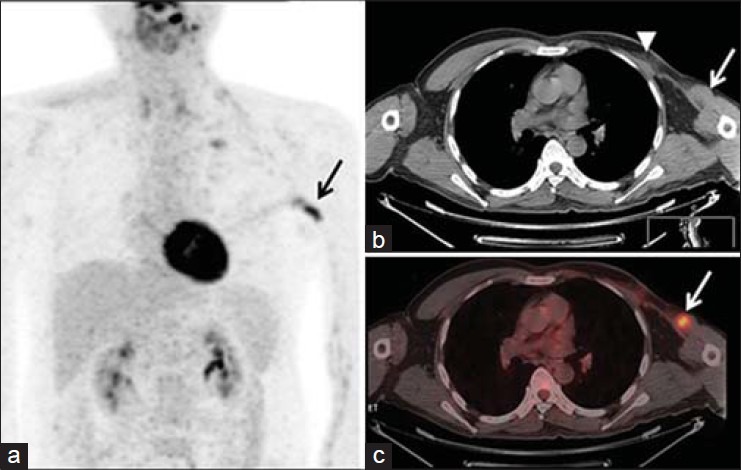
Pitfalls due to treatment related complications (surgery). Pectoralis major myocutaneous (PMMC) flap reconstruction for buccal cancer. Coronal MIP image shows an intense focus of FDG uptake in the left hemithorax (arrow in a) which appears to be metastatic disease. Fused PET/CT shows focal uptake in the anterior chest wall (arrow in c) which was the site for the PMMC flap. FDG uptake was seen due to flap donor site inflammation. Note the absent pectoralis major in the left chest wall. arrowhead in b)
Radiation toxicity can lead to intense inflammatory changes in the mucosal structures and the soft tissues of the neck that can cause intense FDG accumulation [Figure 11].
Figure 11.
Pitfalls due to treatment related complications (radiation). Post radiation therapy for oropharyngeal cancer. Coronal PET (b) and fused PET/CT (c) shows intense FDG uptake in the naso, oro, and hypopharyngeal structures and the soft tissue of the neck bilaterally, with associated ill-defined fat stranding (a – arrowhead). Such intense non-infective inflammation is seen on rare occasions after radiation and should not be confused with recurrence
Radiation induced necrosis can occur in bones (osteoradionecrosis [ORN]), cartilage (chondronecrosis/laryngeal necrosis) and even in irradiated soft tissues. Osteoradionecrosis (ORN) occurs due to devitalization of irradiated bone which gets exposed through the skin and mucosa and remains without healing for at least 3 months. Mandible is one of the commonly affected sites of ORN. The risk of ORN is greatest at 6-12 months after radiation therapy and it is uncommon to see ORN at radiation doses below 60 Gy. Lytic destruction, cortical erosion and fragmentation of the mandible with associated fistulae and soft tissue thickening are some of the features seen on CT scan[1,11] [Figure 12]. Increased FDG avidity is seen in areas affected by ORN [Figure 12], but its specificity in differentiating viable tumor from radionecrosis is not reported to be very high.[15] ORN can occur at rare sites such as the hyoid bone[16] and increased FDG avidity may lead to the erroneous diagnosis of viable disease unless the physician is aware of its occurrence [Figure 13]. Characteristics osseous changes of ORN and absence of associated soft tissue lesion make the diagnosis of radiation necrosis more likely.
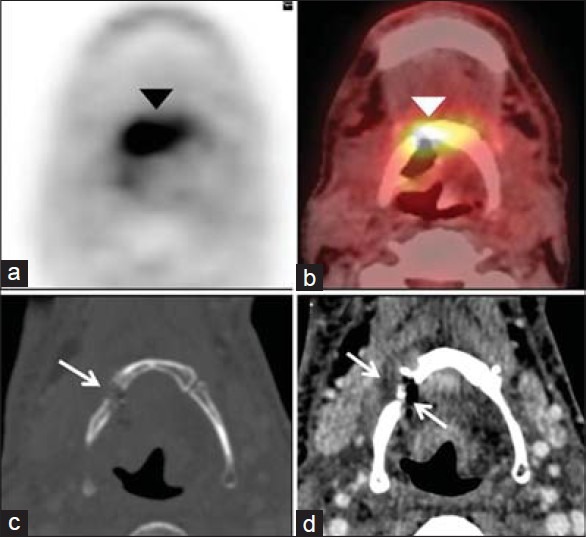
Figure 12.
Pitfalls due to treatment related complications - osteoradionecrosis [ORN]. Post radiation therapy for oral cavity cancer. Axial CT in soft tissue (a) and bone window settings (b) show soft tissue thickening, erosion and fragmentation of the mandible (arrows). Coronal fused PET/CT shows intense FDG uptake restricted to right hemimandible (arrowhead in c and d). Findings suggest the diagnosis of ORN
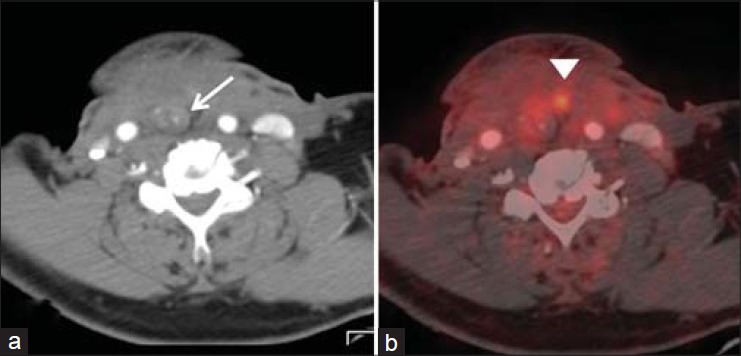
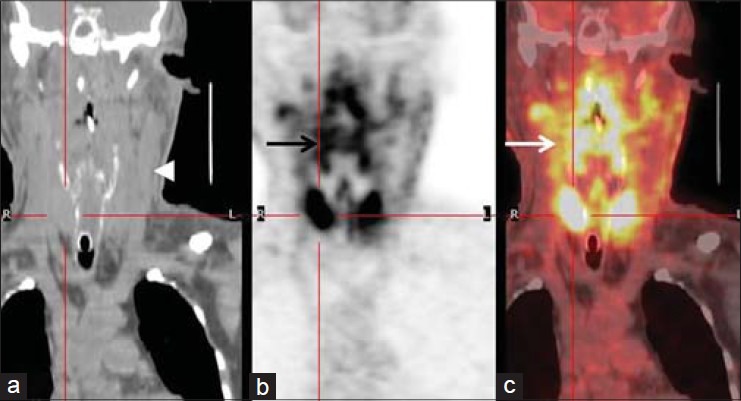
Figure 13.
Pitfalls due to treatment related complications - osteoradionecrosis [ORN]. Post radiation therapy for hypopharyngeal cancer. Axial fused PET/CT shows intense FDG uptake along the hyoid bone (arrowhead in a and b). Axial CT shows subtle erosion of the hyoid bone along with a small collection and air pockets (arrows in c and d). Findings suggest the diagnosis of ORN of the hyoid bone
RECURRENT DISEASE
FDG PET/CT has been used to detect recurrent disease in the head and neck cancer patients.[17,18,19] It can confirm the site of clinically suspected local recurrence and determine its true extent. It has also shown a good accuracy in diagnosing asymptomatic and subclinical recurrences.[20] Recurrences at the site of the treated primary disease, subtle disease in the reconstructed flaps and nodal/soft tissue recurrence in the irradiated neck, the clinical assessment of which is difficult can be seen on PET/CT as enhancing lesions with intense FDG avidity [Figures 14 and 15]. At the same time, it can pick up distant failures with a good accuracy and thus is performed before salvage surgery can potentially change the intended treatment plan.[21] In addition to common sites of distant metastases like the lungs and bones, PET/CT has the potential to unmask second primaries as well as certain unusual and rare metastatic sites such as the subcutaneous tissue, muscles, and feeding stomies [Figures 16 and 17].
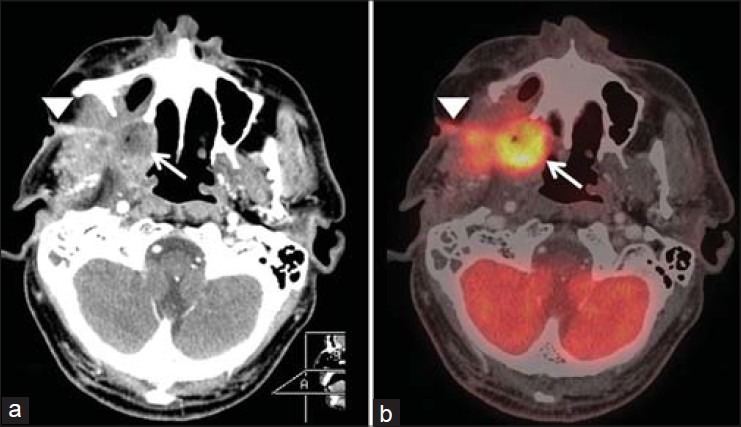
Figure 14.
Recurrent disease. Operated case of buccal cancer. Coronal MIP shows intense foci of FDG uptake on the left side of the face and neck (arrowhead and arrows in a). Axial fused PET/CT shows FDG avid recurrent nodule in the PMMC flap (arrowhead in b and c) and a metastatic cervical lymph node (arrow in d and e)
Figure 15.
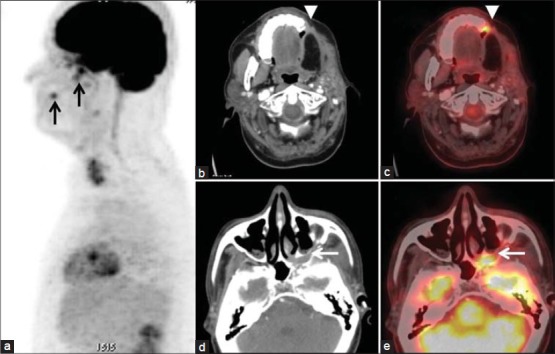
Recurrent disease. Operated case of buccal cancer. Sagittal MIP shows foci of FDG uptake in the face (arrows in a). Axial fused PET/CT (arrowhead in b and c) shows subtle uptake at the cut margin of the mandible due to local recurrence as well as metastatic deposit in the pterygopalatine fossa (arrows in d and e)
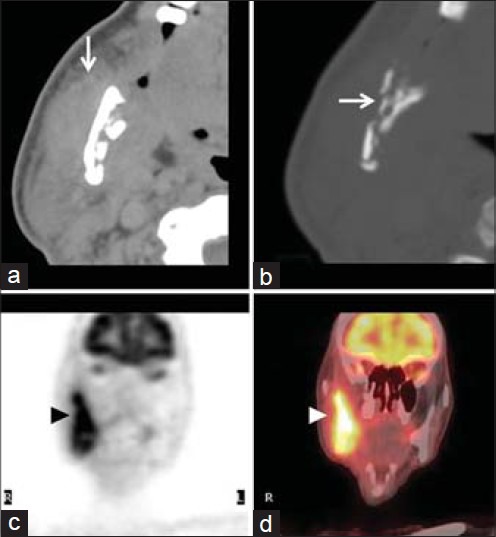
Figure 16.
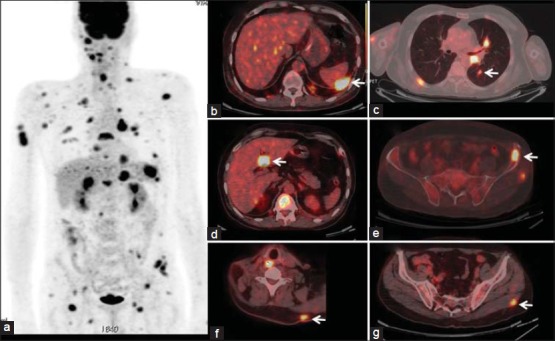
Distant metastases. Treated case of base tongue cancer. MIP image (a) shows multiple FDG avid foci scattered throughout the body. Fusion PET/CT images show metastatic deposits in spleen (b), lungs (c), liver (d), bone (e), subcutaneous region (f) and muscle (g)
Figure 17.
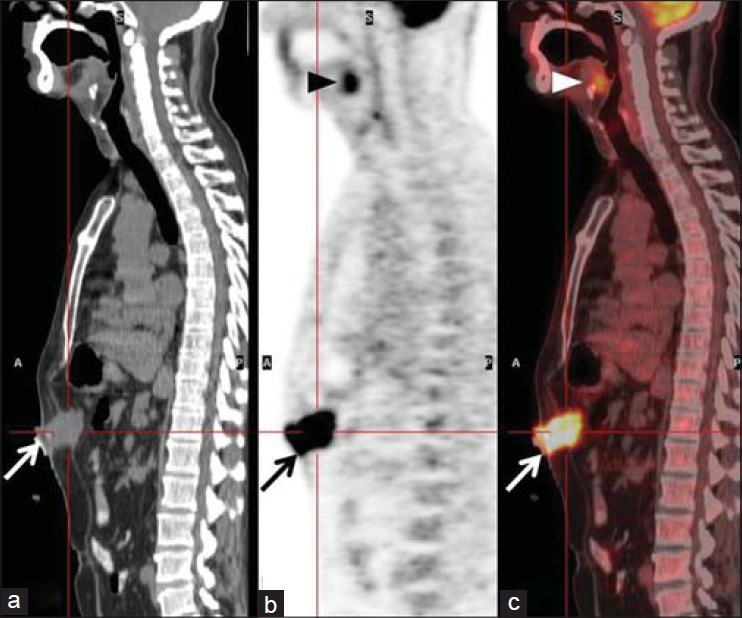
Distant metastases (unusual sites). Operated case of base tongue cancer with feeding gastrostomy. Sagittal PET and PET/CT images show a FDG avid mass in the anterior abdominal wall at the site of the gastrostomy (arrows in a-b) s/o metastatic deposit. Local recurrence in the tongue base is also noted (arrowheads in b and c)
CONCLUSION
FDG PET/CT is a useful modality in the post-treatment setting of head and neck cancers. Knowledge of certain characteristic imaging appearances and a few commonly encountered treatment related complications is important to avoid pitfalls in post-treatment imaging. Understanding the role of FDG PET/CT in detecting local recurrence and distant metastases plays a crucial role in deciding salvage treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Hermans R. Posttreatment imaging in head and neck cancer. Eur J Radiol. 2008;66:501–11. doi: 10.1016/j.ejrad.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 2.Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: Consequences and mechanisms. Lancet Oncol. 2003;4:529–36. doi: 10.1016/s1470-2045(03)01191-4. [DOI] [PubMed] [Google Scholar]
- 3.Matthews R, Shrestha P, Franceschi D, Relan N, Kaloudis E. Head and neck cancers: Post-therapy changes in muscles with FDG PET-CT. Clin Nucl Med. 2010;35:494–8. doi: 10.1097/RLU.0b013e3181e05d94. [DOI] [PubMed] [Google Scholar]
- 4.Bhargava P, Rahman S, Wendt J. Atlas of confounding factors in head and neck PET/CT imaging. Clin Nucl Med. 2011;36:e20–9. doi: 10.1097/RLU.0b013e318212c872. [DOI] [PubMed] [Google Scholar]
- 5.Greven KM, Williams DW, 3rd, McGuirt WF, Sr, Harkness BA, D’Agostino RB, Jr, Keyes JW, Jr, et al. Serial positron emission tomography scans following radiation therapy of patients with head and neck cancer. Head Neck. 2001;23:942–6. doi: 10.1002/hed.1136. [DOI] [PubMed] [Google Scholar]
- 6.Tan A, Adelstein DJ, Rybicki LA, Saxton JP, Esclamado RM, Wood BG, et al. Ability of positron emission tomography to detect residual neck node disease in patients with head and neck squamous cell carcinoma after definitive chemoradiotherapy. Arch Otolaryngol Head Neck Surg. 2007;133:435–40. doi: 10.1001/archotol.133.5.435. [DOI] [PubMed] [Google Scholar]
- 7.Martin RC, Fulham M, Shannon KF, Hughes C, Gao K, Milross C, et al. Accuracy of positron emission tomography in the evaluation of patients treated with chemoradiotherapy for mucosal head and neck cancer. Head Neck. 2009;31:244–50. doi: 10.1002/hed.20962. [DOI] [PubMed] [Google Scholar]
- 8.Wong RJ. Current status of FDG-PET for head and neck cancer. J Surg Oncol. 2008;97:649–52. doi: 10.1002/jso.21018. [DOI] [PubMed] [Google Scholar]
- 9.Gupta T, Jain S, Agarwal JP, Rangarajan V, Purandare N, Ghosh-Laskar S, et al. Diagnostic performance of response assessment FDG-PET/CT in patients with head and neck squamous cell carcinoma treated with high-precision definitive (chemo) radiation. Radiother Oncol. 2010;97:194–9. doi: 10.1016/j.radonc.2010.04.028. [DOI] [PubMed] [Google Scholar]
- 10.Yao M, Smith RB, Graham MM, Hoffman HT, Tan H, Funk GF, et al. The role of FDG PET in management of neck metastasis from head-and-neck cancer after definitive radiation treatment. Int J Radiat Oncol Biol Phys. 2005;63:991–9. doi: 10.1016/j.ijrobp.2005.03.066. [DOI] [PubMed] [Google Scholar]
- 11.Offiah C, Hall E. Post-treatment imaging appearances in head and neck cancer patients. Clin Radiol. 2011;66:13–24. doi: 10.1016/j.crad.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Naidich MJ, Weissman JL. Reconstructive myofascial skull-base flaps: Normal appearance on CT and MR imaging studies. AJR Am J Roentgenol. 1996;167:611–4. doi: 10.2214/ajr.167.3.8751661. [DOI] [PubMed] [Google Scholar]
- 13.Hudgins PA. Flap reconstruction in the head and neck: Expected appearance, complications, and recurrent disease. Eur J Radiol. 2002;44:130–8. doi: 10.1016/s0720-048x(02)00067-0. [DOI] [PubMed] [Google Scholar]
- 14.King KG, Kositwattanarerk A, Genden E, Kao J, Som PM, Kostakoglu L. Cancers of the oral cavity and oropharynx: FDG PET with contrast-enhanced CT in the posttreatment setting. Radiographics. 2011;31:355–73. doi: 10.1148/rg.312095765. [DOI] [PubMed] [Google Scholar]
- 15.Ricci PE, Karis JP, Heiserman JE, Fram EK, Bice AN, Drayer BP. Differentiating recurrent tumor from radiation necrosis: Time for re-evaluation of positron emission tomography? AJNR Am J Neuroradiol. 1998;19:407–13. [PMC free article] [PubMed] [Google Scholar]
- 16.Yoo JS, Rosenthal DI, Mitchell K, Ginsberg LE. Osteoradionecrosis of the hyoid bone: Imaging findings. AJNR Am J Neuroradiol. 2010;31:761–6. doi: 10.3174/ajnr.A1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Subramaniam RM, Truong M, Peller P, Sakai O, Mercier G. Fluorodeoxyglucose-positron-emission tomography imaging of head and neck squamous cell cancer. AJNR Am J Neuroradiol. 2010;31:598–604. doi: 10.3174/ajnr.A1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abgral R, Querellou S, Potard G, Le Roux PY, Le Duc-Pennec A, Marianovski R, et al. Does 18F-FDG PET/CT improve the detection of posttreatment recurrence of head and neck squamous cell carcinoma in patients negative for disease on clinical follow-up? J Nucl Med. 2009;50:24–9. doi: 10.2967/jnumed.108.055806. [DOI] [PubMed] [Google Scholar]
- 19.Kao J, Vu HL, Genden EM, Mocherla B, Park EE, Packer S, et al. The diagnostic and prognostic utility of positron emission tomography/computed tomography-based follow-up after radiotherapy for head and neck cancer. Cancer. 2009;115:4586–94. doi: 10.1002/cncr.24493. [DOI] [PubMed] [Google Scholar]
- 20.Beswick DM, Gooding WE, Johnson JT, Branstetter BF., 4th Temporal patterns of head and neck squamous cell carcinoma recurrence with positron-emission tomography/computed tomography monitoring. Laryngoscope. 2012;122:1512–7. doi: 10.1002/lary.23341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yi JS, Kim JS, Lee JH, Choi SH, Nam SY, Kim SY, et al. 18F-FDG PET/CT for detecting distant metastases in patients with recurrent head and neck squamous cell carcinoma. J Surg Oncol. 2012;106:708–12. doi: 10.1002/jso.23185. [DOI] [PubMed] [Google Scholar]


