Abstract
Objective:
The study was designed to analyze the frequency and clinical features of multicystic ameloblastoma and its histological variants in South Indian sample population, as there is minute information available in the English literature.
Methodology:
The study source was the biopsy specimens retrieved from the archives of the Department of Oral and Maxillofacial Pathology, College of Dental Sciences, Davangere, Karnataka, India, during the past 13 years, from 2001 to 2013. Clinical data for the study were obtained from the case records of patients and the analyzed clinical variables were age, gender and anatomical location. Histologically, hematoxylin and eosin stained sections fitting the World Health Organization (2005) criteria for diagnosis of multicystic ameloblastoma were selectively included.
Results:
Of the 3026 biopsy reports analyzed, 103 cases were odontogenic tumors (3.4%) and 58 cases were ameloblastoma. 31 cases of multicystic ameloblastoma, including follicular ameloblastoma (54.8%), acanthomatous ameloblastoma (29%), plexiform ameloblastoma (6.5%), granular cell ameloblastoma (6.5%) and desmoplastic ameloblastoma (3.2%) were recorded. The age of the patients during the presentation of the lesion was ranging from 21 to 73 years, with a mean of 39.5 years. The most frequent clinical manifestation was swelling, followed by a combination of pain and swelling. In our study, ameloblastoma showed distinct anatomic predilections for occurrence in mandible (96.8%) rather than maxilla (3.2%). This study result also indicated that there is geographical variation in the frequency and distribution of ameloblastoma.
KEY WORDS: Ameloblastoma, clinicopathological correlation, histological subtypes, prevalence, South Indian Population
Odontogenic tumors (OT) encompass a group of heterogenous lesions arising from the odontogenic epithelium or its remnants, when these odontogenic cell rests get entrapped within the bone tissue or gingival tissue of the jaws.[1] These tumors have a broad range of clinical presentations from hamartomatous or nonneoplastic proliferations to benign or malignant neoplasms with varying degree of aggressiveness and metastatic potential.[2]
Ameloblastoma forms the most common of all OT[3,4] and can be conventional solid/multicystic (86%), unicystic (13%) or peripheral (1%)[5] in clinical presentation. Exclusively, solid/multicystic variant alone is analyzed in the present study and according to World Health Organization (WHO) 2005[6] solid/multicystic ameloblastoma is defined as “a slowly growing, locally invasive, epithelial OT of the jaws with a high rate of recurrence if not removed adequately, but with virtually no tendency to metastasize.”[6] Histopathologically, there are various subtypes of solid/multicystic ameloblastoma, of which follicular, plexiform, acanthomatous, desmoplastic, granular cell, and basal cell subtypes are most commonly studied.[5]
Regardless of the vast number of studies on odontogenic tumors and ameloblastoma in the literature, information regarding the demographic profile of multicystic ameloblastoma and its histological subtypes in different populations is inadequate, especially in the Indian population. Thus, the objective of this study is to determine the distribution and clinical features of solid/multicystic ameloblastoma and its individual histological variants diagnosed over a period of 13 years in Davangere and around the surrounding districts of Davangere, Karnataka, India.
Methodology
A retrospective study on ameloblastoma was conducted based on the availability of oral biopsy specimens retrieved from the archives of the Department of Oral and Maxillofacial Pathology, College of Dental Sciences, Davangere, India, from the year 2001 through December 2013. The age, gender, and anatomical location of all cases were compiled from the clinical data sent together with the biopsy records. Histopathology slides stained with hematoxylin and eosin were selected and re-evaluated according to the current concepts outlined by the WHO (2005).[6] Inclusion criteria involved the histological confirmation of subtypes of solid/multicystic ameloblastoma. Some clinical records that were sent with the biopsy material were with inadequate information and were excluded. Furthermore, unicystic and peripheral variant of ameloblastoma were excluded from the analysis. Clinicopathological correlation was done by analyzing the age, gender and site distribution in each histopathological subtype of multicystic ameloblastoma. For analytical convenience, site distribution in the maxilla and mandible were divided into anterior (from midline to distal surface of canine in each quadrant) and posterior (from mesial surface of first premolar to the tuberosity in the maxilla and ramus in the mandible in each quadrant) regions. The collected data were subjected to descriptive statistical analyses with the SPSS version 16.0 statistical software package (SPSS Inc., Chicago, USA).
Results
Prevalence rate
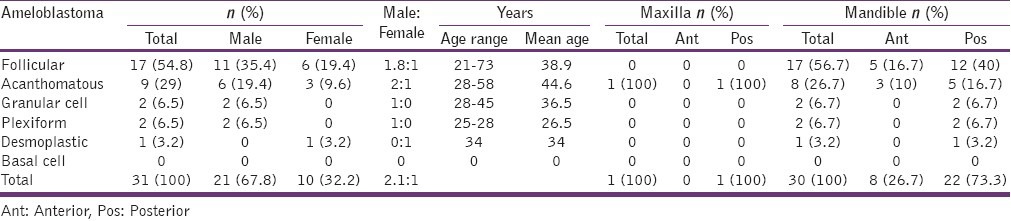
A total of 3026 biopsy specimens were reported during the period of 13 years (2001–2013) and 103 odontogenic tumors (3.4%) were observed, of which 58 cases (56.3%) were ameloblastoma [Table 1]. Among the 58 ameloblastomas, 31 cases (53.4%) were diagnosed as solid variant of ameloblastoma and 27 cases (46.5%) were unicystic variant. These 31 cases of multicystic ameloblastomas were histopathologically revealing the following subtypes, follicular ameloblastoma – 17 cases (54.8%), acanthomatous ameloblastoma – 9 cases (29%), plexiform and granular cell ameloblastoma – 2 cases each (6.5%) and desmoplastic ameloblastoma – 1 case (3.2%) [Table 2].
Table 1.
Prevalence rate and age distribution in patients with ameloblastoma
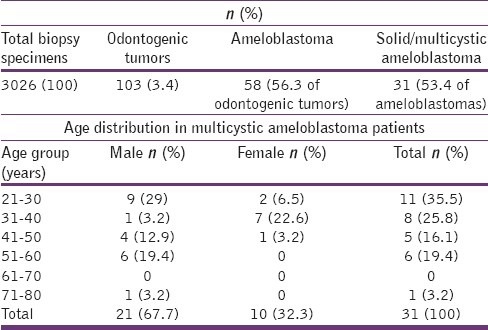
Table 2.
Gender and site distribution in multicystic ameloblastoma patients according to individual histological subtypes
Gender and age
Of all the ameloblastomas, 21 (67.8%) cases were observed in men and 10 (32.2%) cases were seen in women, with a male:female ratio of 2.1:1. The mean age of the patients was 39.5 years, with a wide range (21-73 years) of age distribution, and of these, 11 (35.5%) cases and 8 (25.8%) cases were diagnosed in the third and fourth decades of life, respectively [Table 1]. The gender and age range distribution in individual subtypes is elaborated in Table 2.
Site
Ameloblastoma lesions were seen predominantly in the mandible (30 cases [96.8%]), sparing a single lesion at maxilla (3.2%). Posterior mandible was most commonly affected (22 cases [73.3%]) followed by anterior region (8 cases [26.7%]). The single case in maxilla also favored posterior region [Table 2]. Among the four quadrants, left posterior body-ramus-angular region was most frequently involved than the right side.
Discussion
Prevalence rate
In our study, odontogenic tumors constituted about 3.4% of all the biopsy lesions recorded from 2001 to 2013. Odontogenic tumors show variation in distribution depending on ethnicity and geographical location.[3] Thus, on comparison with other studies from various regions, it is less than that of African series (9.6%),[7] but higher than that of North American (1.55%),[8,9] South American (1.82%)[10,11,12,13] and European series (0.74%).[14,15] A hospital-based study on South Indian population, (Tamil linguistic Dravidians) showed frequency of 4.13%[3] and 3.75%[4] was seen in Srilankan population.
Of these odontogenic tumors, ameloblastoma was the most common one in our study (56.3%), coinciding with that of (67.69%) Gupta and Ponniah[3] and Siriwardena et al.[4] (48.7%), whereas odontomes are more common in the western countries.[4] Multicystic ameloblastoma was about 53.4% and unicystic ameloblastoma was about 46.5% in distribution with no peripheral variant. This distribution is quite varying from that of Neville et al.,[5] where 86% of ameloblastoma lesions are attributed to multicystic variant, but Gupta and Ponniah[3] have reported the occurrence of only 42.33% of solid variant in their study. The similar study population (Dravidians) in both this study and that of Gupta and Ponniah[3] could explain the similarities in study results.
Among the histological subtypes of multicystic ameloblastoma, follicular subtype (54.8%) was the most commonly encountered variant followed by acanthomatous (29%) ameloblastoma. From other scientific resources,[5,16] plexiform is the second most common next to follicular subtype and the variation could be due to the difference in the ethnicity of the study population. Desmoplastic variant constituted 3.2% in the present study, while it was 1.4% in the study by Reichart et al.[16] Plexiform and granular cell subtypes were distributed equally (6.5%) and basal cell ameloblastoma, the least common subtype[5] had not been observed in any of the lesions.
Age
In this study, the average age of patients at the time of initial diagnosis was 39.5 years (Range: 21-73 years) similar to the findings of Small and Waldron[17] (38.9 years), while Reichart et al.[16] have reported it to be 35.9 years. Each subtype was showing slight variation in the mean age of presentation, with acanthomatous subtype showing maximum value of 44.6 years (eldest) and plexiform presenting with youngest mean age of 26.5 years. Interestingly, follicular ameloblastoma was seen at both extremes of age range that is, as young as 21 years and also at 73 years [Table 2].
Gender
Regarding gender predilection, of 31 cases, 21 cases (67.8%) were observed in men and 10 cases (32.2%) were seen in women, with a male:female ratio of 2.1:1. Comparing to the study results of Reichart et al.,[16] where the male:female ratio is 1.13:1, the observed ratio in the present study is slightly higher, which could be due to our comparatively smaller sample size. Considering individual subtypes, again male predominance was noted in all of them, except in desmoplastic variant, where only a single case was reported and it was in female.
Location
Favoring most of the literature source,[3,5,17,18] mandibular molar-ramus region was the most frequently involved site in the study. All histological subtypes of ameloblastoma involved posterior mandible most commonly. The single case occurring in maxilla was of acanthomatous subtype and desmoplastic ameloblastoma, which has predilection to occur in maxillary anterior region[5] had occurred in the mandibular posterior region.
The most frequent clinical manifestation was swelling, followed by a combination of pain and swelling. However, there is no correlation between histological subtypes and clinical symptoms, similar to the findings of Regezi et al.[19] and Kramer.[20] All the lesions are unilateral in occurrence and radiographically, most of them were presenting with multilocularity (soap bubble or honeycomb appearance) and a single case was showing unilocularity. As few cases were with insufficient radiographic details, complete analysis is not provided.
Conclusion
Clinical details with respect to each histological subtypes of ameloblastoma are very minimal in the literature and our analysis over more than a decade is valuable epidemiological data available for the future vision and comparison. The study results are showing similarities as well as variations with other ethnic groups in various clinical presentations of multicystic ameloblastoma. Pertaining to the details on prevalence rate and distribution, the study results are much similar with other Dravidian population studies, proving that the prevalence of odontogenic tumors vary with ethnical and geographical effect.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Regezi JA, Sciubba JJ, Jordan RC. 5th ed. St. Louis: Saunders; 2008. Oral Pathology: Clinical Pathologic Correlation; pp. 261–75. [Google Scholar]
- 2.Mosqueda-Taylor A. New findings and controversies in odontogenic tumors. Med Oral Patol Oral Cir Bucal. 2008;13:E555–8. [PubMed] [Google Scholar]
- 3.Gupta B, Ponniah I. The pattern of odontogenic tumors in a government teaching hospital in the southern Indian state of Tamil Nadu. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e32–9. doi: 10.1016/j.tripleo.2010.02.035. [DOI] [PubMed] [Google Scholar]
- 4.Siriwardena BS, Tennakoon TM, Tilakaratne WM. Relative frequency of odontogenic tumors in Sri Lanka: Analysis of 1677 cases. Pathol Res Pract. 2012;208:225–30. doi: 10.1016/j.prp.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 5.Neville BW, Damm DD, Allen CM, Bouquot JE. 2nd ed. Philadelphia: W.B. Saunders Company; 2002. Oral and Maxillofacial Pathology; pp. 611–8. [Google Scholar]
- 6.Barnes L, Eveson JW, Reichart P, Sidransky D. Lyon: IARC Press; 2005. Pathology and Genetics of Head and Neck Tumors; pp. 284–327. [Google Scholar]
- 7.Ladeinde AL, Ajayi OF, Ogunlewe MO, Adeyemo WL, Arotiba GT, Bamgbose BO, et al. Odontogenic tumors: A review of 319 cases in a Nigerian teaching hospital. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:191–5. doi: 10.1016/j.tripleo.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 8.Mosqueda-Taylor A, Ledesma-Montes C, Caballero-Sandoval S, Portilla-Robertson J, Ruíz-Godoy Rivera LM, Meneses-García A. Odontogenic tumors in Mexico: A collaborative retrospective study of 349 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:672–5. doi: 10.1016/s1079-2104(97)90371-1. [DOI] [PubMed] [Google Scholar]
- 9.Buchner A, Merrell PW, Carpenter WM. Relative frequency of central odontogenic tumors: A study of 1,088 cases from Northern California and comparison to studies from other parts of the world. J Oral Maxillofac Surg. 2006;64:1343–52. doi: 10.1016/j.joms.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 10.Ochsenius G, Ortega A, Godoy L, Peñafiel C, Escobar E. Odontogenic tumors in Chile: A study of 362 cases. J Oral Pathol Med. 2002;31:415–20. doi: 10.1034/j.1600-0714.2002.00073.x. [DOI] [PubMed] [Google Scholar]
- 11.Fernandes AM, Duarte EC, Pimenta FJ, Souza LN, Santos VR, Mesquita RA, et al. Odontogenic tumors: A study of 340 cases in a Brazilian population. J Oral Pathol Med. 2005;34:583–7. doi: 10.1111/j.1600-0714.2005.00357.x. [DOI] [PubMed] [Google Scholar]
- 12.Santos JN, Pinto LP, de Figueredo CR, de Souza LB. Odontogenic tumors: Analysis of 127 cases. Pesqui Odontol Bras. 2001;15:308–13. doi: 10.1590/s1517-74912001000400007. [DOI] [PubMed] [Google Scholar]
- 13.Avelar RL, Antunes AA, Santos Tde S, Andrade ES, Dourado E. Odontogenic tumors: Clinical and pathology study of 238 cases. Braz J Otorhinolaryngol. 2008;74:668–73. doi: 10.1016/S1808-8694(15)31375-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olgac V, Koseoglu BG, Aksakalli N. Odontogenic tumours in Istanbul: 527 cases. Br J Oral Maxillofac Surg. 2006;44:386–8. doi: 10.1016/j.bjoms.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Tamme T, Soots M, Kulla A, Karu K, Hanstein SM, Sokk A, et al. Odontogenic tumours, a collaborative retrospective study of 75 cases covering more than 25 years from Estonia. J Craniomaxillofac Surg. 2004;32:161–5. doi: 10.1016/j.jcms.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: Biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31B:86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 17.Small IA, Waldron CA. Ameloblastomas of the jaws. Oral Surg Oral Med Oral Pathol. 1955;8:281–97. doi: 10.1016/0030-4220(55)90350-9. [DOI] [PubMed] [Google Scholar]
- 18.Sriram G, Shetty RP. Odontogenic tumors: A study of 250 cases in an Indian teaching hospital. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e14–21. doi: 10.1016/j.tripleo.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 19.Regezi JA, Kerr DA, Courtney RM. Odontogenic tumors: Analysis of 706 cases. J Oral Surg. 1978;36:771–8. [PubMed] [Google Scholar]
- 20.Kramer IR. Ameloblastoma: A clinicopathological appraisal. Br J Oral Surg. 1963;1:13–28. doi: 10.1016/s0007-117x(63)80044-x. [DOI] [PubMed] [Google Scholar]


