Abstract
Lymphoepithelial cysts are benign, slowly growing unilocular or multilocular lesions that appear in the head and neck. They are also called Branchial cyst. The head and neck sites are the salivary glands(more commonly parotid and rarely submandibular gland) and the oral cavity (usually the floor of the mouth). there are various methods of investigation available today, of which Fine needle aspiration cytology (FNAC) can be used to provide an immediate diagnosis of a lymphoepithelial cyst. The other investigations include, Ultrasonogram,and Computed tomography. It usually occurs due to the process of lymphocyte-induced cystic ductular dilatation and the confirmatory diagnosis is always made postoperatively by histopathological examination. The mainstay in the treatment of a lymphoepithelial cyst remains the surgical approach, which includes complete enucleation of the cyst along with total excision of the involved salivary gland. This is a report of a lymphoepithelial cyst involving the submandibular salivary gland and its management.
KEY WORDS: Lyphoepithelial cyst, sub-mandibular gland, benign neck lesion malignant transformation
Lymphoepithelial cysts are benign, slowly growing unilocular or multilocular lesions that appear in the head and neck. They are also called Branchial cyst. The head and neck sites are the salivary glands (more commonly parotid and rarely submandibular gland) and the oral cavity (usually the floor of the mouth). These cysts are usually seen in adults and only occasionally in children. They range in size from 0.5 to 5.0 cm, and they can cause considerable cosmetic deformity and physical discomfort. Sometimes, the lymphoepithelial cyst may occur without involving the salivary glands, most commonly in the anterior triangle of the neck. If not treated, there is a high chance of lymphoepithelial cysts transforming into malignant lesions such as malignant lymphomas, which has the capacity to involve the extranodal sides secondarily. This is a case report of lymphoepithelial cyst involving the submandibular gland.
Case Report
The case we present here is about a 32-year-old, female patient who reported to our hospital with the complaint of a painless swelling on the left side of the neck for past 8 months. The swelling was small initially and has progressed to the present size [Figure 1]. The swelling did not cause any functional restriction but was cosmetically evident, which was the patient's concern. On extraoral examination, there was a soft, fluctuant, compressible, nontender swelling of size 8-10 cm in the left submandibular region. The swelling extended anteriorly from the parasymphysis region of mandible, and extended posteriorly until the angle region of the mandible. Superiorly the swelling did not go beyond the lower border of mandible and inferiorly extended until the level of thyroid cartilage. On intraoral examination, there was no abnormal finding. The orifice of the left submandibular duct and the saliva flow was normal.
Figure 1.

Preoperative photo showing cyst on the left side sub-mandibular region
On intraoral examination, there were no abnormal finding and the patient did not complaint of any dryness of mouth or pain along the floor of the mouth or at the opening of the submandibular duct.
An aspiration was done from the swelling using a wide bore needle, which showed the presence of a Straw colored fluid. The aspirated fluid subjected for fine-needle aspiration cytology (FNAC), which revealed the presence of lymphocytes, few histiocytes, few plasma cells and squamous cells dispersed in a proteinaceous material. This almost proved that the lesion is a cyst from a lymphoepithelial origin.
A computed tomography (CT) scan was done to assess the size and extent of the swelling which revealed the presence of a well circumscribed and encapsulated lesion measuring about 10 cm × 6 cm. The lesion did not show any invasion into the mandible or major blood vessels, except it was pushing the facial artery and vein medially into the neck. The capsule of the lesion was slightly adherent to the superficial part of the left side submandibular gland [Figure 2]. A routine blood investigation was performed. The patient was tested for human immunodeficiency virus (HIV) both with enzyme linked immunosorbent assay and Western blot test, both of which were negative.
Figure 2.
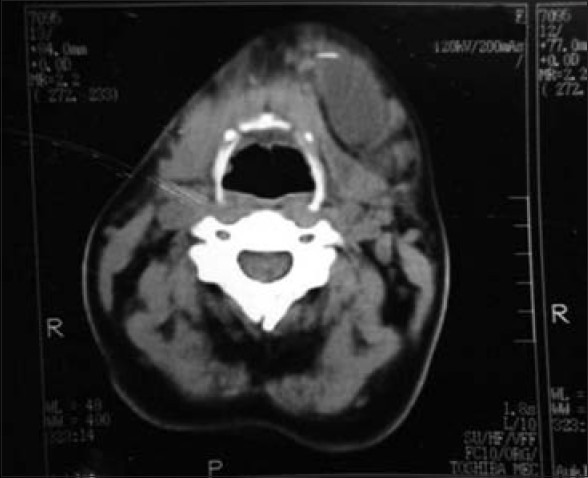
Computed tomography of the submandibular region shows a well encapsulated mass seen on the left submandibular region being attached to superficial part of left submandibular gland
The treatment was very definitive and the patient was planned for excision of the lesion under general anesthesia. The surgical approach was made with a horizontal neck incision along the neck crease. Facial artery and vein were seen adherent to the cystic wall and hence they were ligated. Marginal mandibular nerve was identified and preserved. The lesion was exposed and was completely enucleated along with the excision of the superficial part of the submandibular salivary gland. Hemostasis was achieved and closure was done. The specimen was sent for histopathological examination, which revealed the specimen consisting of cyst lined by glandular epithelium consisting of lymphoid follicles [Figure 3].
Figure 3.

Postoperative photo after 2 weeks of excision
Discussion
Lymphoepithelial cysts or the branchial cysts are the benign, slow growing lesion that occurs mostly in adults with a predilection for gender with 60-80% being female. It occurs in the second and third decade of life and the swelling is usually diffuse, fluctuant and nontender. The lymphoepithelial cysts are usually associated with the salivary gland, especially the parotid gland and rarely the submandibular gland.[1] In this kind of lesion, as the glands are affected, the duct of the gland is also affected as in the above case, submandibular gland and duct.[2] The branchial cysts which do not involve the salivary component usually arise on the lateral cervical area including the lymphnode. They have been classically described to occur anterior to the upper third of the sternomastoid. Anyways, they have been known to occur in other areas of neck, oral cavity, salivary glands, thyroid, and mediastinum and even in pancreas. It occurs due to lymphocyte induced cystic ductular dilatation and it is always diagnosed postoperatively by histopathlogic examination.
There are various theories proposed as the cause for a branchial cyst. They can be broadly classified as congenital theories and lymph node theories. Of the two theories, the most accepted is the lymphnode theory suggested by kings. It proposed that cysts developed due to the cystic transformation of the lymphnodes. Lymphoepithelial cysts can arise with other condition like Sjogren's syndrome, mikulicz's disease and myoepithelial sialadinitis. In Sjogren's syndrome minor salivary glands are involved, but generally lack a lymphoepithelial component.[3]
The lymphoepiyheliail cyst has been associated with HIV infection as part of a diffuse infiltrative lymphocytosis syndrome. HIV-associated salivary gland disease is a lymphoid hyperplasia in the parotid and sometimes submandibular, gland with lymphoepithelial cyst and lymphoepithelial lesions in HIV positive patients. The incidence of HIV-associated salivary disease is about 3-10% among the HIV positive patient. Children and adults, males and females are affected. Salivary gland disease usually develops before AIDS and sometimes it is the first manifestation of HIV infection. It is usually bilateral and is accompanied by cervical lymphadenopathy.[4]
The investigation modalities include FNAC, which is usually therapeutic as well as a confirmatory test if performed accurately. The presence of proteinaceous background and a mixed population of lymphocytes, histiocytes, plasma cells, and metaplastic squamous cells in the cytologic findings on the fine-needle aspiration of a major salivary gland lesion, the diagnosis of lymphoepithelial cyst should be considered.[5] CT helps in determining the nature of cyst, if it is encapsulated or breaching and invading into other structures. The most important is that the CT reveals the extent of the lesion in all direction before planning for surgical excision. Magnetic resonance imaging (MRI) with contrast, which would clearly show thin rim enhancement. Ultrasonogram can be performed, which can very well-demonstrate a cystic lesion and a vascular lesion. Sialography can be done to detect any obstruction within the gland and duct. Both MRI and sialography was not done as the patient was unaffordable.
The lesions of salivary glands with a prominent lymphoid component are a heterogeneous group of diseases that include benign reactive lesions and malignant neoplasms. The differential diagnosis include lymphoepithelial sialadenitis, HIV-associated salivary gland disease, chronic sclerosing sialadenitis, Warthin tumor, and extranodal marginal zone B-cell lymphoma, salivary duct retention cyst (mucocele), dysgenetic polycystic disease of the salivary gland, mucosa associated lymphoid tissue lymphoma. Patients with salivary gland lymphoepithelial cyst are at the increased risk of developing lymphoma and that is reason such cyst should be treated as early as possible.
Treatment of the lyphoepithelial cyst includes both conservative as well as surgical approach. The conservative approach includes decompression the cyst by aspirating the fluid out thereby reducing the pressure. Such a procedure should be considered in an immudeficient patient like HIV positive in which the surgical management is clearly outweighed by the risk. Other conservative treatment includes external radiotherapy. The definitve treatment is the surgical management by complete enucleation of the cyst along with the excision of the involved gland. Most patients are completely cured by excision and never get a recurrence.[6]
Conclusion
It should kept in mind that the lymphoepithelial cysts are benign in nature and should be treated as early as possible as it can transform itself into a malignant lesion such as malignant lymphoma, adenocarcinoma, mucoepidermoid carcinoma and surgery remains the main-stay in the treatment of all lymphoepithelial and lateral cervical cyst.[4]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ioachim HL. Lymphoid hyperplasias and lymphomas of salivary glands. Pathol Case Rev. 2004;9:206–13. [Google Scholar]
- 2.Tiwari A, Kini H, Pai RR, Rau AR. HIV lymphadenitis of the salivary gland: A case with cytological and histological correlation. J Cytol. 2009;26:146–8. doi: 10.4103/0970-9371.62184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Panchbhai AS, Choudhary MS. Branchial cleft cyst at an unusual location: A rare case with a brief review. Dentomaxillofac Radiol. 2012;41:696–702. doi: 10.1259/dmfr/59515421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rojas R, Di Leo J, Palacios E, Rojas I, Restrepo S. Parotid gland lymphoepithelial cysts in HIV infection. Ear Nose Throat J. 2003;82:20–2. [PubMed] [Google Scholar]
- 5.Lester J, Gopez EV. Cystic lesions of the salivary glands: Cytologic features in fine-needle aspiration biopsies. (197-204).2002;27:4. doi: 10.1002/dc.10168. [DOI] [PubMed] [Google Scholar]
- 6.Habib S, Rahman MM, Chaudhury AA, Kamal M. Benign lymphoepithelial cyst. Bangladesh J Otorhinolaryngol. 2010:16. [Google Scholar]


