Abstract
Ameloblastic carcinoma is a rare odontogenic tumor exhibiting not only features of ameloblastoma, but also features of carcinoma. Clinical dissemination of this lesion is more aggressive and rapid than that of ameloblastoma and it can metastasize to the lung or regional lymph node. Histologically, there are features of both ameloblastoma and carcinoma. <50 cases have been reported until 2011. We report a series of six cases with our treatment modalities.
KEY WORDS: Ameloblastic carcinoma, ameloblastoma, malignant ameloblastoma, neck dissection
Ameloblastoma is a benign but locally aggressive neoplasm, which presents as a slowly growing painless swelling of the jaws. It is reported to constitute about 1-3% of all jaw tumors and cysts. The malignant variants are exceptionally rare and may arise de-novo or from transformation of a long-standing primarily benign lesion, which has undergone several surgical treatments. The terms malignant ameloblastoma and ameloblastic carcinoma have been used interchangeably for these variants in the past.[1] Malignant ameloblastoma and ameloblastic carcinoma are two distinct variants of ameloblastoma. Ameloblastic carcinoma is locally aggressive and may or may not undergo regional lymph node metastasis, whereas malignant ameloblastoma would definitely show metastasis.[2]
Choice of treatment also differs for all these three conditions. Malignant ameloblastoma exhibits metastatic spread, regional lymph node metastases, and hematogenous dissemination may occur. Surgical resection of the primary tumor with wide margins is the mainstay treatment of ameloblastic carcinoma.[3] Neck dissection is done only in cases with positive lymph node involvement. Recent reports also mention the benefits of radiotherapy after initial surgical intervention, especially with the use of megavoltage therapy.[4]
Case Report
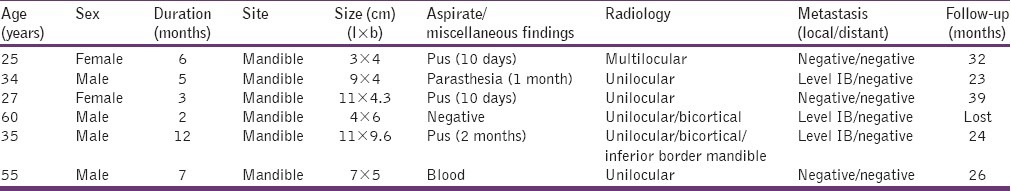
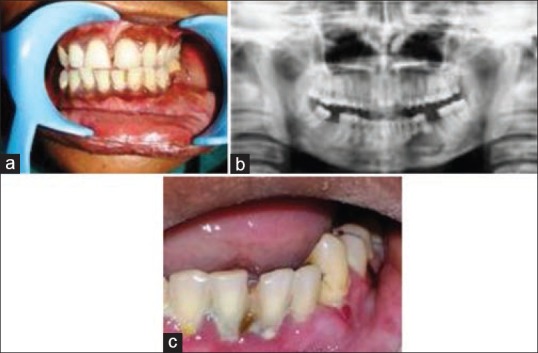
Six cases were reported from 2007 to 2012 to the Oral and Maxillofacial Unit of Annaswamy Mudaliar General Hospital, Bangalore, out of which four patients were males with the lesion occurring between the second decade of life and sixth decade of life [Figures 1a–3c]. In all cases, the mandible was involved with the greatest size of tumor seen being 11 cm × 9.6 cm [Figure 1a]. All cases exhibited enlargement of cortical plates with perforation, pain and tenderness with regional lymph node enlargement, with three cases showing fixed submandibular groups of lymph nodes (Level IB) and in one case parasthesia of inferior alveolar nerve. An orthopantomograph was taken for all patients. Five cases showed unilocular radiolucency and one case showed multilocular radiolucency with erosion of bone, including inferior border of mandible in one case [Figure 1c]. The duration of the tumor was from 2 to 12 months. Maximum follow-up was for 39 months with one patient being lost to the follow-up [Table 1]. All patients had a Chest X-ray and an abdomen ultrasound done to avoid missing distant metastasis as we were aware of the potential of this lesion to metastasize. We did not find evidence of distant metastasis in any of our patients. Incisional biopsy was done for diagnosis for all cases and was diagnosed as features suggestive of ameloblastoma with areas showing dysplastic changes in the epithelium suggestive of a neoplastic change.
Figure 1.

(a) Patient exhibiting large extra oral tumor with draining sinus, (b) Intra oral view of tumor: (c) Orthopantomogram showing bicortical involvement of mandible
Table 1.
Patient data
Surgical Management
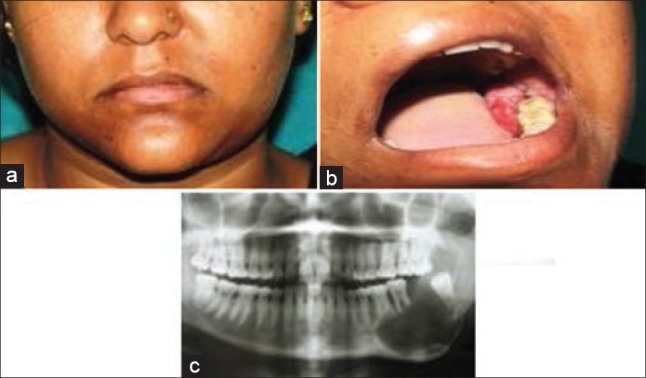
In one patient, wide excision was done as the lesion was small and the patient being young did not wish aggressive measures that may have had postsurgical cosmetic deformity [Figure 2a–c]. He chose the “wait and watch” policy and there is no evidence of disease after 32 months.
Figure 2.
(a) Preoperative view showing tumor involving left mandible and sulcus, (b) Preoperative orthopantomogram, (c) Intra oral view of tumor being excised
Two patients underwent hemimandibulectomy and neck dissection because of increased involvement of mandible with palpable Level IB nodes where fine-needle aspiration cytology showed positive for carcinoma, as also one more patient who had underwent a wide excision with hemimandibulectomy and neck dissection due to skin involvement and palpable fixed nodes at IB Level [Figure 1a–c].
One patient had a segmental resection of the mandible
All the resected specimens were sent for histological examination.
Figure 3.
(a) Preoperative view of tumor involving left mandible, (b) Intra oral view of tumor, (c) Orthopantomogram showing involvement of left mandible
Histopathology
The largest diameter of the tumors was 10 cm × 9 cm [Figure 1a] showing increased vascularity with numerous cystic spaces and areas of necrosis. Typical features found were multiple pieces of tissue with predominant tumor islands within connective tissue seen under scanner. Under higher magnification tumor islands appearing epithelial odontogenic in origin showed infiltrative pattern with each island showing peripheral columnar cells with central stellate reticulum exhibiting feature of ameloblastoma, but with atypical features such as bizarre mitosis, altered nuclear chromatin ratio, hyperchromatisim, and mild pleomorphism. Central stellate reticulum appears to be condensed and hypercellular presenting a less orderly fashion. Individual cell keratinization with keratin pearl formation with stroma showed predominant inflammatory component and endothelial lined blood vessels [Figure 4]. Immunohistochemical findings showed that ameloblastic carcinomas reacted strongly with antibodies directed against cytokeratin CHM and AEI and AE3. The tumor was negative for carcinoembryonic antigen.
Figure 4.
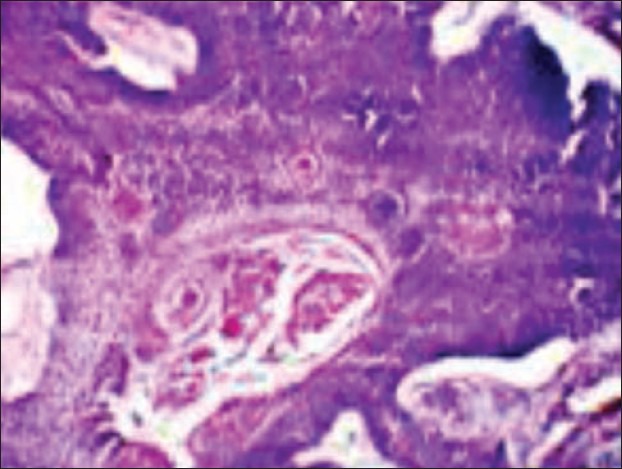
Histopathological picture showing bizarre mitosis, altered nuclear chromatin ratio, hyperchromatisim, mild pleomorphism, and central stellate reticulum confirming ameloblastic carcinoma
No evidence of disease or metastasis was seen postsurgery in any of the patients.
It is interesting to note that up to date of completion of this study 71 cases of ameloblastoma had reported to our department between February 2007 and May 2012. In this series, six cases proved to be that of ameloblastic carcinoma.
Discussion
Ameloblastic carcinoma is a lesion with histologic behavior that dictates a more aggressive surgical approach than that of a simple ameloblastoma.[5] Mean age for occurrence is 30.5 years, male: female ratio is 1.5:1, and 80% are located in the mandible posterior region.[6] These findings coincided with our case series where mean age was 39.33 years. There is no apparent sex predilection.[7] All our cases also had mandibular involvement and no involvement of maxilla was seen. Involvement of the maxilla is less frequent than that of the mandible.[6,8]
The clinical symptoms of ameloblastic carcinoma are more aggressive than conventional ameloblastoma, with swelling, pain, rapid growth, trismus, dysphonia, expansion of the jaws, and frequently perforation of the cortex.[6] These were mirrored in our series also.
Radiographic appearance of ameloblastic carcinoma is consistent with that of ameloblastoma except for occasional presence of some focal radiopacities, reflecting dystrophic calcification.[6] Histologically, ameloblastic carcinoma does not show uniform proliferation, and has pleomorphic and hyperchromatic cells arranged in the form of sheets and chords with reversed polarity.[8] Spindling of the cells is recognized in some solid proliferating areas.[7]
Differential diagnosis included odontogenic keratocyst, squamous cell carcinoma and ameloblastoma. An additional consideration in the differential diagnosis is the squamous cell carcinoma arising in the lining of an odontogenic cyst. Histologically, this lesion tends to more closely resemble oral squamous cell carcinoma ameloblastic carcinoma. It is of interest that ameloblastic carcinoma can apparently arise from a cystic lining. The squamous odontogenic tumor may also be mistaken for ameloblastic carcinoma, being composed of islands of squamous epithelium that lack stellate reticulum like zones, peripheral palisading, microcystic changes and dystrophic calcifications. However, the epithelium of the squamous odontogenic tumor lacks any cytologic evidence of malignant disease.
Thus, the term ameloblastic carcinoma can be applied to our series, where all showed evidence of malignant disease including cytologic atypia and mitoses with indisputable features of classic ameloblastoma.
Whether ameloblastoma may transform biologically and histologically from a classic ameloblastoma to a malignant lesion is controversial. Many authors have shown that metastasizing ameloblastomas are histologically indistinguishable from classic ameloblastomas and others have identified malignant features in the tumor, usually after repeated surgical excisions. The high rate of recurrence maybe due to the mode of growth and surgical mismanagement rather that any inherent malignant properties and metastases are “exceedingly rare.”[9]
Wide local excision is the treatment of choice as most investigators have recommended,[9,10] which we had followed in all our cases. Regional lymph node dissection should be performed selectively as we did in three of our cases where in the regional lymph node was palpable. The efficacy of adjuvant radiation or chemotherapy as a postsurgical treatment is not clear and seems to have a limited value.[3] Data regarding chemotherapy is sparse. Lanham treated a patient with doxorubicin, cisplatin, cyclophosphamide, dacarbazine, and 5 FU; but, the tumor failed to respond.[9] Yoon et al. have reported distant metastasis as early as 4 months and as late as 47 months after surgery.[8] None of our patients showed recurrence, but one patient was lost to follow-up. None of our patients were sent for radiotherapy or chemotherapy. In our case series, least follow-up until date is 22 months and maximum follow-up being 39 months.
Conclusion
This small series of cases illustrates the malignant portion in the spectrum of ameloblastomas and it is possible that ameloblastoma may show a wide variety of histologic and biologic behavior ranging from benignity to frank malignancy. Cases of ameloblastoma should be studied carefully, correlating their histologic pattern with biologic behavior to detect changes in histology that may predict aggressive behavior. When a case is diagnosed as ameloblastic carcinoma, assessment of nodal metastasis and evidence of distant metastasis should be evaluated. Treatment of ameloblastic carcinoma is wide surgical resection and if evidence of nodal metastasis is present, neck dissection should also be considered. Role of radiotherapy and chemotherapy is as yet conclusive.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ram H, Mohammad S, Husain N, Gupta PN. Ameloblastic carcinoma. J Maxillofac Oral Surg. 2010;9:415–9. doi: 10.1007/s12663-010-0169-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akrish S, Buchner A, Shoshani Y, Vered M, Dayan D. Ameloblastic carcinoma: Report of a new case, literature review, and comparison to ameloblastoma. J Oral Maxillofac Surg. 2007;65:777–83. doi: 10.1016/j.joms.2005.11.116. [DOI] [PubMed] [Google Scholar]
- 3.Ram H, Mohammad S, Husain N, Gupta PN. Ameloblastic carcinoma. J Maxillofac Oral Surg. 2010;9:415–9. doi: 10.1007/s12663-010-0169-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suomalainen A, Hietanen J, Robinson S, Peltola JS. Ameloblastic carcinoma of the mandible resembling odontogenic cyst in a panoramic radiograph. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:638–42. doi: 10.1016/j.tripleo.2005.07.033. [DOI] [PubMed] [Google Scholar]
- 5.Sharma S, Misra K, Dev G. Malignant ameloblastoma. A case report. Acta Cytol. 1993;37:543–6. [PubMed] [Google Scholar]
- 6.Datta R, Winston JS, Diaz-Reyes G, Loree TR, Myers L, Kuriakose MA, et al. Ameloblastic carcinoma: Report of an aggressive case with multiple bony metastases. Am J Otolaryngol. 2003;24:64–9. doi: 10.1053/ajot.2003.15. [DOI] [PubMed] [Google Scholar]
- 7.Bruce RA, Jackson IT. Ameloblastic carcinoma. Report of an aggressive case and review of the literature. J Craniomaxillofac Surg. 1991;19:267–71. doi: 10.1016/s1010-5182(05)80068-x. [DOI] [PubMed] [Google Scholar]
- 8.Yoon HJ, Hong SP, Lee JI, Lee SS, Hong SD. Ameloblastic carcinoma: An analysis of 6 cases with review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:904–13. doi: 10.1016/j.tripleo.2009.06.045. [DOI] [PubMed] [Google Scholar]
- 9.Corio RL, Goldblatt LI, Edwards PA, Hartman KS. Ameloblastic carcinoma: A clinicopathologic study and assessment of eight cases. Oral Surg Oral Med Oral Pathol. 1987;64:570–6. doi: 10.1016/0030-4220(87)90063-6. [DOI] [PubMed] [Google Scholar]
- 10.Newman L, Howells GL, Coghlan KM, DiBiase A, Williams DM. Malignant ameloblastoma revisited. Br J Oral Maxillofac Surg. 1995;33:47–50. doi: 10.1016/0266-4356(95)90087-x. [DOI] [PubMed] [Google Scholar]


