Abstract
Burning mouth syndrome (BMS), a chronic and intractable orofacial pain syndrome is characterized by the presence of burning sensation of the oral mucosa in the absence of specific oral lesion. This condition affects chiefly of middle aged and elderly woman with hormonal changes or psychological disorders. In addition to burning sensation, patient with BMS also complains of oral mucosal pain, altered taste sensation, and dry mouth. This condition is probably of multifactorial origin, often idiopathic and its exact etiopathogenesis remains unclear. So far, there is no definitive cure for this condition and most of the treatment approaches, medications remains unsatisfactory. An interdisciplinary and systematic approach is required for better patient management. The purpose of this article is to present a review of epidemiology, clinical presentation, classification, etiopathogenesis, diagnosis and management of BMS.
KEY WORDS: Burning mouth syndrome, classification, dysgeusia, epidemiology, etiology and treatment, stomatodynia
“A doctor who cannot take good history and a patient who cannot give one are in danger of giving and receiving bad treatment.”
-Paul Dudley White
Patient complaining of burning sensation of the oral cavity present one of the difficult task to the oral health care professionals. This condition gets even worsened if it is accompanied by pain. Pain is the frequent cause of suffering and disability that seriously impairs the quality of a human life. Burning mouth syndrome (BMS), a chronic and intractable pain syndrome that chiefly affecting the middle or old age women is characterized by stinging or burning sensation of the oral mucosa in the absence of an apparent signs of an organic cause on physical examination. A universally accepted definition of this syndrome is still lacking because of their variations in their clinical manifestations. However, International Association for the Study of Pain[1] defines this condition as “burning pain in the tongue or other oral mucous membrane associated with normal signs and laboratory findings lasting at least 4-6 months.”[2]
In the past, this condition has been referred by variety of names that includes scalded mouth syndrome, stomatodynia, sore tongue, burning lips syndrome, glossodynia, glossalgia, stomatopyrosis, oral dysesthesia, burning mouth condition, glossopyrosis, sore mouth, and BMS (the most widely accepted).[3,4] The use of various terms in the past leads to the confusion and uncertainty in the clinical practice and scientific literature. Affected individuals often complains of burning pain of the oral mucosa preferably on the tongue accompanied by other sensory disorders such as dry mouth, altered taste sensation. This condition is often idiopathic in nature and its etiopathogenesis so far remains unclear.
Epidemiology
It is extremely hard to establish the true prevalence of BMS due to the lack of appropriate and consistent classification system, definitive diagnostic criteria and their awareness among the oral health care professionals. Many authors fail to distinguish between the syndrome and the symptom as such. The prevalence of BMS reported from various international studies ranges from 0.6% to 15%, respectively.[5] BMS is basically a disorder of middle-aged and elderly individuals with an age range of 38-78 years.[4] It seems that their prevalence increases with age in both males and females. BMS exhibits significant female predilection and the ratio between females and males varies from 3:1 to 16:1 in various literature studies.[6] Even though it is not yet defined, these gender differences were explained in the context of biological, psychological, and sociocultural factors. Epidemiological studies reveal that this condition is particularly common among peri- and post-menopausal women where their prevalence increases up to 12-18%.[7] This condition is extremely rare in patients under 30 years and never been reported in children and adolescence.[8]
Classification and Subtypes
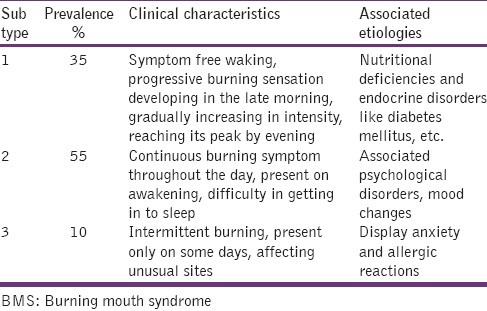
Different classification types have been proposed to illustrate the clinical course of the condition. Lamey and Lewis have suggested classifying BMS into three subtypes according to variations in pain intensity over 24 h [Table 1].[3,9]
Table 1.
Lamey and Lewis classification of BMS
Scala et al. classified BMS into two categories: ‘Primary or essential/idiopathic’ BMS, in which local or systemic causes cannot be identified, and involving peripheral or central neuropathological pathways. “Secondary” BMS, resulting from local, systemic or psychological factors.[4]
Based on the level of pathology involved, Jääskeläinen categorized primary BMS into three subgroups with some overlapping in individual patients. The first subgroup is characterized by peripheral small diameter fiber neuropathy of oral mucosa, the second subgroup consist of pathology involving the lingual, mandibular or trigeminal system and the third subgroup, labeled as having central pain, that may involve the hypofunction of dopaminergic neurons in the basal ganglia.[10]
Clinical Features
The clinical manifestations of BMS are not constant and are always diverse and variable. Most of the time, patient found difficulty in describing the sensations they perceive. The term BMS implies to an individual who complains of variety of chronic oral symptoms (that includes oral mucosal pain, altered taste sensation, xerostomia, and others) that often increases in intensity at the end of each day that seldom interfere with sleep.[11]
Oral burning pain remains the chief symptom of BMS. Most individual describes this symptom as burning, tingling, scalding, annoying, tender, or numb feeling of the oral mucosa, most commonly involving the anterior 2/3rd of the tongue, followed by dorsum, lateral borders of tongue, anterior portion of hard palate, and labial mucosa. The onset of pain is spontaneous, bilateral with no identifiable precipitating factors. Pain may be felt deep within the mucosa, continuous for at least 4-6 months, with moderate to severe intensity that may vary during the day. The location of pain is not pathognomonic, often involving more than one site. Some may even experience burning sensation involving extra oral mucosa including the anogenital region. In some, pain alters the sleep pattern that leads to poor quality of life, anxiety, depression, decrease desire to socialize and/or somatization.[4]
More than 70% of individuals also experience taste disturbances that manifest as persistent alteration in the taste, most commonly bitter, metallic or both.[12] And this may be due to the disturbance of sensory modalities of small diameter afferent fibers. Approximately, 2/3rd of the patient complains of dry mouth. The feeling or evidence of dry mouth in these individuals is more likely due to the side-effects of anticholinergics, psychotropic drugs, antihistamines and or diuretics.[13] There have been several studies that have shown clear alterations in the quality and quantity of saliva in BMS affected individual.
Various literature studies proves that the patient with BMS have nonspecific health complaints that includes headaches, TMJ pain, dizziness, musculoskeletal disorders, irritable bowel syndrome, dermatological and psychiatric disorders.[14]
Etiopathogenesis
Because of the complex clinical behavior, the exact cause of BMS is currently unknown. The etiology is presumed to be multifactorial involving the interaction between neurophysiological mechanisms and psychological factors.[15]
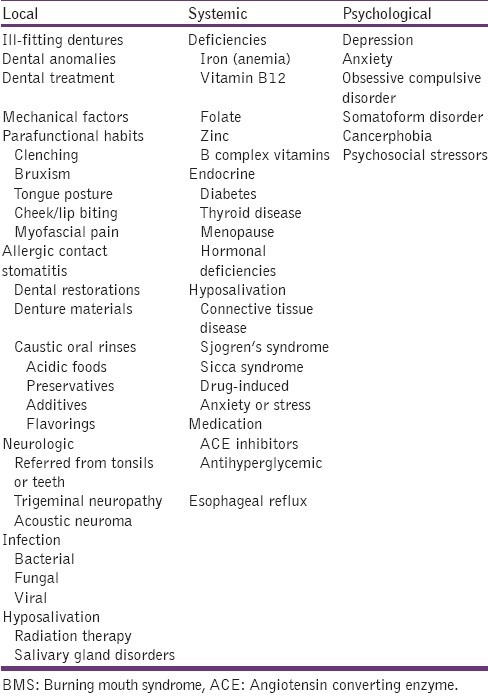
A considerable number of local, systemic, and psychological factors have been found related to BMS; however, several of these factors should be considered as conditions important to the differential diagnosis of oral burning rather than as an etiologic factor for BMS [Table 2].
Table 2.
Reported etiological factors for BMS[14]
The possible theories behind the cause of BMS are enlisted here:
Abnormal interaction between the sensory functions of facial and trigeminal nerves.[16] According to this theory, certain individuals labeled as supertasters (mainly females) due to the high density of fungiform papilla present on the anterior aspect of tongue, are at risk of developing burning pain.[17]
Sensory dysfunction associated with small and/or large fiber neuropathy.[18] Forssell et al. found that almost 90% of individuals with BMS had some form of altered sensory threshold and/or blink reflex reaction. Immunohistochemical and microscopic observations revealed axonal degeneration of epithelial and subpapillary nerve fibers in the affected epithelium of the oral mucosa.[19]
Centrally mediated alteration in the modulation of nociceptive processing. This theory explains the fact that there is a reduction in the nigrostriatal dopaminergic system resulting in reduced central pain suppression in BMS individuals.[20]
Disturbances in the autonomic innervation and oral blood flow.[21]
Chronic anxiety or stress results in the alteration of gonadal, adrenal and neuroactive steroid levels in skin and oral mucosa.[22]
Diagnosis
The following steps should be performed before arriving the diagnosis of BMS
Taking a thorough and comprehensive history to quntify the sensation of pain
Thorough clinical examination of the oral mucosa to rule out local and systemic causes
Information on previous or current psychosocial stressors and psychological well-being
Objective measurements of salivary flow rates and taste function
Neurological imaging and examination to rule out any pathology and degenerative disorders
Oral cultures to confirm suspected bacterial, viral, and fungal infections
Patch test for allergic individuals
Gastric reflux studies
Hematological test to rule out nutritional, hormonal, autoimmune conditions.
Treatment
The complex and multifactorial etiology of BMS necessitates systematic and interdisciplinary approach for the proper management of these patients. Although many drugs, treatment methods have been proposed for the management of BMS, none of them proves to be a gold standard one and are not satisfactory. Treatment planning should be custom made to each patient. Obtaining the correct clinical diagnosis of BMS is of paramount importance for the management.
Acquiring patient trust and reassurance is of paramount in the management of BMS, and it is crucial that the patient understands and accept the diagnosis and has a realistic understanding of the likelihood of being cured. These have a great impact on patient's attitude and may often results in long-term beneficial effects.[23] The investigator should have a detailed review of patient's personal/familiar/medical/dental/personal histories and a careful interpretation of data obtained from various physical and laboratory investigations. If any local, systemic or psychological factors are evident, attempt should be made to treat or eliminate these factors.
A thorough clinical examination of the oral mucosa is crucial in these patients. The lack of oral mucosal pathology is mandatory for the diagnosis of BMS. Details regarding the quality, onset, persistence, intensity, occurrence, duration, relieving factors, evolution, site(s) involved in pain symptoms are essential. This information will give a vital clue in differentiating the BMS from other chronic orofacial pain disorders. Because BMS is a multifactorial disease, none of a single drug or treatment procedure can result in complete remission of all symptoms.
Management of BMS can be broadly discussed under three topics namely topical medications, systemic medications and behavioral interactions. Medications used for BMS include antidepressants, analgesics, antiepileptics, antifungals, antibacterials, sialagogues, antihistamines, anxiolytics, antipsychotics and vitamin, mineral, and hormonal replacements.
Topical medications
Topical application of capsaicin (0.025% cream) has been used in BMS as a desensitizing agent and is thought to inhibit substance P. Reduced patient tolerance and increased toxicity limits its use in some patients.[24] Trials have also been made on rinsing with 0.15% benzydamine hydrochloride, 3 times a day, having an analgesic, anesthetic, and anti-inflammatory effect, but with inconsistent results.[25] Some other gets relieved from pain by using mouth rinse made of Tabasco sauce with water[26] or alternatively one made of hot pepper and water in a dilution between 1:2 and 1:1.[27] The topical application of clonazepam (by sucking a tablet of 1 mg), an agonist of gamma amino butyric acid receptors, 3 times a day for 14 days found some success in some.[28]
The most commonly used local anesthetic agent, lidocaine was tried by few and they have not been shown as an effective treatment due to their short duration of analgesic action. Topical application of 0.5 ml Aloe vera gel at 70%, 3 times a day combined with tongue protector is found to be effective for reducing the burning and pain sensation of tongue.[29] Topical lactoperoxidase (biotene mouthwash) and 5% doxepin were attempted and found to be ineffective.[30]
Systemic medications
Numerous studies have assessed systemic therapies for treating BMS with varied outcome. The use of tricyclic antidepressants such as amitriptyline, desipramine, imipramine, clomipramine and nortriptyline (starting dose of 5-10 mg/day and gradually increases to 50 mg/day) are useful in treating BMS. Some authors contraindicate these drugs in patient with dry mouth as they can worsen the condition.
Selective serotonin reuptake inhibitor antidepressants like sertraline (50 mg/day), paroxetine (20 mg/day) for 8 weeks, duloxetine at a dose of 30-60 mg/day, a dual action antidepressants that inhibit both serotonin and noradrenaline result in a significant improvement of oral burning sensation.[31] Antipsychotics such as amisulpride, levosulpiride at a dose of 50 mg/day for 24 weeks proved to be effective and shows a better patient compliance when used in short duration.
Alpha-lipoic acid (ALA) at a dose of 600 mg/day, either alone or in combination for 2 months, acts as an antioxidant and a powerful neuroprotective agent that prevents nerve damage by free radicals, regenerating other antioxidants such as vitamin C and E, able to increase the intracellular levels of glutathione, thereby significantly reduces the symptoms in patients with idiopathic dysgeusia.[32] Patients undergoing ALA therapy must be advised concomitant gastric protection medication.[33]
Systemic capsaicin (0.25% capsules, 3 times a day, for 1 month) proves to be effective in reducing pain intensity. However, it should be used cautiously as it results in gastric pain in some individuals. Benzodiazepines at low doses are useful in patients with anxiety disorders. Clonazepam (0.5 mg/day) and alprazolam (0.25 mg to 2 mg/day) are commonly used in the treatment of BMS pain and it acts by probably disrupting the underlying neuropathologic mechanism.[34]
Supplementation with vitamin BC capsules, B12, folic acid and minerals like iron, zinc can significantly lower the mean serum homocysteine level and boost up the blood hemoglobin level with reported complete remission of oral symptoms.[35]
Hormone replacement therapy (conjugated estrogens like premarin, 0.625 mg/day for 21 days and medroxyprogesterone acetate like farlutal, 10 mg/day from day 12 through day 21, for three consecutive cycles) can relieve oral burning symptoms and improved cytologic features, especially in peri- and post-menopausal women.[36]
Cognitive behavior therapy has been beneficiary in some individuals.[37] Successful treatment of BMS patients with combined psychotherapy and psychopharmacotherapy has also been reported.[31]
Conclusion
Burning mouth syndrome is a painful and often frustrating condition to the patients. The exact cause of BMS often is difficult to pinpoint and is probably of multifactorial origin and may be idiopathic. The etiopathogenesis of BMS seems to be complex. Diagnosis and management of BMS is not an easy task for oral health care professionals. A thorough understanding of the etiology and psychological impact of this disorder, combined with novel pharmacological interventions is required for better management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Merskey H, Bogduk N. Classification of Chronic Pain. 2nd ed. Seattle, WA: IASP Press; 1994. Descriptions of chronic pain syndromes and definitions of pain terms; p. 74. [Google Scholar]
- 2.Grinspan D, Fernández Blanco G, Allevato MA, Stengel FM. Burning mouth syndrome. Int J Dermatol. 1995;34:483–7. doi: 10.1111/j.1365-4362.1995.tb00617.x. [DOI] [PubMed] [Google Scholar]
- 3.Lamey PJ. Burning mouth syndrome. Dermatol Clin. 1996;14:339–54. doi: 10.1016/s0733-8635(05)70361-2. [DOI] [PubMed] [Google Scholar]
- 4.Scala A, Checchi L, Montevecchi M, Marini I, Giamberardino MA. Update on burning mouth syndrome: Overview and patient management. Crit Rev Oral Biol Med. 2003;14:275–91. doi: 10.1177/154411130301400405. [DOI] [PubMed] [Google Scholar]
- 5.Zakrzewska JM, Hamlyn PJ. Facial pain. In: Crombie IK, editor. Epidemiology of Pain. Seattle, WA: IASP Press; 1999. pp. 175–82. [Google Scholar]
- 6.Grushka M. Clinical features of burning mouth syndrome. Oral Surg Oral Med Oral Pathol. 1987;63:30–6. doi: 10.1016/0030-4220(87)90336-7. [DOI] [PubMed] [Google Scholar]
- 7.Sun A, Wu KM, Wang YP, Lin HP, Chen HM, Chiang CP. Burning mouth syndrome: A review and update. J Oral Pathol Med. 2013;42:649–55. doi: 10.1111/jop.12101. [DOI] [PubMed] [Google Scholar]
- 8.López-Jornet P, Camacho-Alonso F, Andujar-Mateos P, Sánchez-Siles M, Gómez-Garcia F. Burning mouth syndrome: An update. Med Oral Patol Oral Cir Bucal. 2010;15:e562–8. doi: 10.4317/medoral.15.e562. [DOI] [PubMed] [Google Scholar]
- 9.Lamey PJ, Lewis MA. Oral medicine in practice: Orofacial pain. Br Dent J. 1989;167:384–9. doi: 10.1038/sj.bdj.4807050. [DOI] [PubMed] [Google Scholar]
- 10.Jääskeläinen SK. Pathophysiology of primary burning mouth syndrome. Clin Neurophysiol. 2012;123:71–7. doi: 10.1016/j.clinph.2011.07.054. [DOI] [PubMed] [Google Scholar]
- 11.Gorsky M, Silverman S, Jr, Chinn H. Clinical characteristics and management outcome in the burning mouth syndrome. An open study of 130 patients. Oral Surg Oral Med Oral Pathol. 1991;72:192–5. doi: 10.1016/0030-4220(91)90162-6. [DOI] [PubMed] [Google Scholar]
- 12.Ship JA, Grushka M, Lipton JA, Mott AE, Sessle BJ, Dionne RA. Burning mouth syndrome: An update. J Am Dent Assoc. 1995;126:842–53. doi: 10.14219/jada.archive.1995.0305. [DOI] [PubMed] [Google Scholar]
- 13.Astor FC, Hanft KL, Ciocon JO. Xerostomia: A prevalent condition in the elderly. Ear Nose Throat J. 1999;78:476–9. [PubMed] [Google Scholar]
- 14.Klasser GD, Fischer DJ, Epstein JB. Burning mouth syndrome: Recognition, understanding, and management. Oral Maxillofac Surg Clin North Am. 2008;20:255–71. doi: 10.1016/j.coms.2007.12.012. vii. [DOI] [PubMed] [Google Scholar]
- 15.Zakrzewska JM. The burning mouth syndrome remains an enigma. Pain. 1995;62:253–7. doi: 10.1016/0304-3959(95)00089-B. [DOI] [PubMed] [Google Scholar]
- 16.Grushka M, Epstein JB, Gorsky M. Burning mouth syndrome and other oral sensory disorders: A unifying hypothesis. Pain Res Manag. 2003;8:133–5. doi: 10.1155/2003/654735. [DOI] [PubMed] [Google Scholar]
- 17.Bartoshuk LM, Snyder DJ, Grushka M, Berger AM, Duffy VB, Kveton JF. Taste damage: Previously unsuspected consequences. Chem Senses. 2005;30(Suppl 1):i218–9. doi: 10.1093/chemse/bjh192. [DOI] [PubMed] [Google Scholar]
- 18.Forssell H, Jääskeläinen S, Tenovuo O, Hinkka S. Sensory dysfunction in burning mouth syndrome. Pain. 2002;99:41–7. doi: 10.1016/s0304-3959(02)00052-0. [DOI] [PubMed] [Google Scholar]
- 19.Lauria G, Majorana A, Borgna M, Lombardi R, Penza P, Padovani A, et al. Trigeminal small-fiber sensory neuropathy causes burning mouth syndrome. Pain. 2005;115:332–7. doi: 10.1016/j.pain.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 20.Jääskeläinen SK, Rinne JO, Forssell H, Tenovuo O, Kaasinen V, Sonninen P, et al. Role of the dopaminergic system in chronic pain – A fluorodopa-PET study. Pain. 2001;90:257–60. doi: 10.1016/S0304-3959(00)00409-7. [DOI] [PubMed] [Google Scholar]
- 21.Heckmann SM, Heckmann JG, HiIz MJ, Popp M, Marthol H, Neundörfer B, et al. Oral mucosal blood flow in patients with burning mouth syndrome. Pain. 2001;90:281–6. doi: 10.1016/S0304-3959(00)00410-3. [DOI] [PubMed] [Google Scholar]
- 22.Woda A, Dao T, Gremeau-Richard C. Steroid dysregulation and stomatodynia (burning mouth syndrome) J Orofac Pain. 2009;23:202–10. [PubMed] [Google Scholar]
- 23.Bergdahl J, Anneroth G, Perris H. Cognitive therapy in the treatment of patients with resistant burning mouth syndrome: A controlled study. J Oral Pathol Med. 1995;24:213–5. doi: 10.1111/j.1600-0714.1995.tb01169.x. [DOI] [PubMed] [Google Scholar]
- 24.Grushka M, Epstein JB, Gorsky M. Burning mouth syndrome. Am Fam Physician. 2002;65:615–20. [PubMed] [Google Scholar]
- 25.Buchanan J, Zakrzewska J. Burning mouth syndrome. Clin Evid. 2004;12:1899–905. [PubMed] [Google Scholar]
- 26.Moreno Gimenez J. Glosodynia before and after diagnosis. Piel. 2005;20:524–9. [Google Scholar]
- 27.Brufau-Redondo C, Martín-Brufau R, Corbalán-Velez R, de Concepción-Salesa A. Burning mouth syndrome. Actas Dermosifiliogr. 2008;99:431–40. [PubMed] [Google Scholar]
- 28.Gremeau-Richard C, Woda A, Navez ML, Attal N, Bouhassira D, Gagnieu MC, et al. Topical clonazepam in stomatodynia: A randomised placebo-controlled study. Pain. 2004;108:51–7. doi: 10.1016/j.pain.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 29.López-Jornet P, Camacho-Alonso F, Molino-Pagan D. Prospective, randomized, double-blind, clinical evaluation of Aloe vera Barbadensis, applied in combination with a tongue protector to treat burning mouth syndrome. J Oral Pathol Med. 2013;42:295–301. doi: 10.1111/jop.12002. [DOI] [PubMed] [Google Scholar]
- 30.Femiano F. Burning mouth syndrome (BMS): An open trial of comparative efficacy of alpha-lipoic acid (thioctic acid) with other therapies. Minerva Stomatol. 2002;51:405–9. [PubMed] [Google Scholar]
- 31.Van Houdenhove B, Joostens P. Burning mouth syndrome. Successful treatment with combined psychotherapy and psychopharmacotherapy. Gen Hosp Psychiatry. 1995;17:385–8. doi: 10.1016/0163-8343(95)00061-u. [DOI] [PubMed] [Google Scholar]
- 32.Granot M, Nagler RM. Association between regional idiopathic neuropathy and salivary involvement as the possible mechanism for oral sensory complaints. J Pain. 2005;6:581–7. doi: 10.1016/j.jpain.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 33.Buchanan J, Zakrzewska J. Burning mouth syndrome. Clin Evid. 2005;14:1685–90. [PubMed] [Google Scholar]
- 34.Nagler RM, Hershkovich O. Sialochemical and gustatory analysis in patients with oral sensory complaints. J Pain. 2004;5:56–63. doi: 10.1016/j.jpain.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 35.Sun A, Lin HP, Wang YP, Chen HM, Cheng SJ, Chiang CP. Significant reduction of serum homocysteine level and oral symptoms after different vitamin-supplement treatments in patients with burning mouth syndrome. J Oral Pathol Med. 2013;42:474–9. doi: 10.1111/jop.12043. [DOI] [PubMed] [Google Scholar]
- 36.Forabosco A, Criscuolo M, Coukos G, Uccelli E, Weinstein R, Spinato S, et al. Efficacy of hormone replacement therapy in postmenopausal women with oral discomfort. Oral Surg Oral Med Oral Pathol. 1992;73:570–4. doi: 10.1016/0030-4220(92)90100-5. [DOI] [PubMed] [Google Scholar]
- 37.Bergdahl J, Anneroth G, Perris H. Personality characteristics of patients with resistant burning mouth syndrome. Acta Odontol Scand. 1995;53:7–11. doi: 10.3109/00016359509005936. [DOI] [PubMed] [Google Scholar]


