Abstract
Tastes in humans provide a vital tool for screening soluble chemicals for food evaluation, selection, and avoidance of potentially toxic substances. Taste or gustatory dysfunctions are implicated in loss of appetite, unintended weight loss, malnutrition, and reduced quality of life. Dental practitioners are often the first clinicians to be presented with complaints about taste dysfunction. This brief review provides a summary of the common causes of taste disorders, problems associated with assessing taste function in a clinical setting and management options available to the dental practitioner.
KEY WORDS: Ageusia, dysgeusia, hypergeusia, hypogeusia, phantogeusia, taste disorders, taste disturbances
The chemosensory functions of taste and smell play a vital role in human physiology. They determine the flavor and palatability of foods and beverages, the selection of nutrients essential for life, and the warning of toxic vapors, fire, and spoiled foodstuffs. Chemosensory dysfunctions have serious implications for the preservation of oral and systemic health, with dramatic effects on quality-of-life.[1] Patients frequently report increased use of sugar and salt to compensate for diminished sense of taste, a practice that is detrimental to those with diabetes mellitus or hypertension.[2]
Anatomy and Physiology of Taste
The specialized sense organ for taste (gustation) consists of approximately 10,000 taste buds, which are ovoid bodies measuring 50-70 μm. There are four morphologically distinct types of cells within each taste bud: Basal cells, dark cells (Type I), light cells (Type II), and intermediate cells (Type III). Basal cells do not extend processes into the taste pore and are likely to be undifferentiated or immature taste cells. The later three cell types are sensory neurons that respond to taste stimuli or tastants. In humans, the taste buds are located in the mucosa of the epiglottis, palate, and pharynx and in the walls of the papillae of the tongue.[3] Each taste bud has receptors at the apical portion exposed to the oral cavity and a basolateral area separated by a tight junction.[1] Taste buds across the oral cavity serve similar functions. Although, there are subtle regional differences in sensitivity to different tastants, the concept of a “tongue map” defining distinct zones for sweet, bitter, salty, and sour has largely been discredited.[4] Taste sensation can be evoked by a diverse group of chemicals ranging from simple ions (H+, Na+) to inorganic molecules to carbohydrates and complex proteins.[5]
Taste modalities generally fall into five established basic tastes according to the receptor type most strongly activated: Sweet, sour, salty, bitter, and umami.[6] Accumulating evidence suggest a taste component for free fatty acids in humans as the sixth modality of taste.[7] The sensory nerve fibers from the taste receptors reach the gustatory nucleus of the medulla oblongata by VII, IX, and X cranial nerves. From there, the signals reach the ventral posteromedial nucleus of the thalamus through the axons of the second order neurons. From the thalamus, the third order neurons reach the gustatory cortex.[3]
Taste is also commonly confused with somatosensory sensations such as the cool of menthol or the heat of chili peppers perceived through trigeminal nerve. The capacity of cutaneous, including trigeminal, glossopharyngeal (IX cranial), and vagal (X cranial) nerve fiber endings, to detect chemicals is known as chemesthesis or cutaneous chemosensation. Oral chemesthesis explains the pungent or sharp feel of many different foods and spices such as chili peppers, horseradish, the coolness of peppermint, the tingle of carbonated drinks, and the irritation produced by substances such as raw garlic extracts.[8]
Terminologies
Smell or olfaction is the perception of odor by the nose, whereas taste or gustation is the perception of salty, sweet, sour, or bitter by the tongue. Flavor is the combination of taste, smell, and trigeminal sensation. Trigeminal stimulation (pain, tactile, and temperature) contributes to flavor perception throughout the eating process.[1] Gustatory dysfunctions are classified as quantitative or qualitative disorders.[9] Quantitative taste disorder include ageusia, hypogeusia and hypergeusia, while qualitative disorders are dysgeusia and phantogeusia. Ageusia is an absence of the sense of taste; hypogeusia is a decreased sensitivity to all tastants.[10] Hyperguesia refers to enhanced gustatory sensitivity.[11] Dysgeusia or pargeusia is an unpleasant perception of a tastant and phantogeusia, is a perception of taste that occurs in the absence of a tastant.[3,10]
Etiology
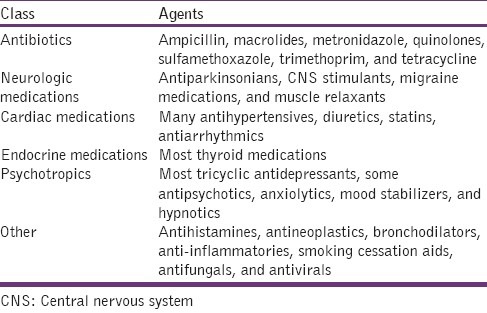
Majority of the gustatory dysfunctions are caused by impairment of smell rather than taste perception. The most common causes of olfactory dysfunction include allergic rhinitis, chronic rhinosinusitis and upper respiratory infection.[12] Any condition that results in a compromised environment for the mediators of chemosensation (e.g. tongue, saliva, oral mucosa, neural pathways, and neurotransmitters) results in altered taste perception at any age. The mechanistic cause of gustatory dysfunction can be of three types: Transport, sensory or neuronal problem [Table 1].[1] Drug-induced taste disorder was found to be the most common etiology among the patients visiting a taste clinic in Japan [Table 2].[13] The drug interactions and side-effects index lists over 200 drugs with chemosensory dysfunction. A partial list of these medications affecting taste is shown in Table 3.[14]
Table 1.
Mechanistic cause of gustatory dysfunction[1]
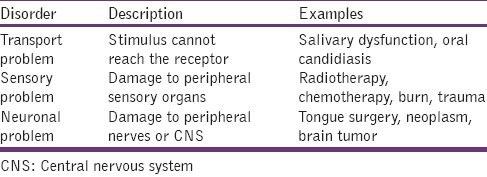
Table 2.
Etiology of gustatory dysfunction in 2,278 patients[13]
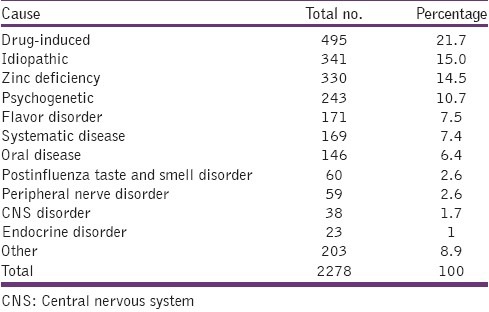
Table 3.
Drugs causing gustatory dysfunction[14]
Oral sources of altered taste function are common and can be evaluated by a dentist. Trauma (burns, lacerations, surgery, and local anesthesia), local antiplaque medicaments and drugs excreted into saliva, infections (dentoalveolar, periodontal, soft tissue), vesiculobullous conditions, removable prostheses, metallic dental restorations, and salivary dysfunction can directly or indirectly affect taste function.[1] Gastroesophageal reflux disease can produce apparent phantogeusia, which may be intermittent or persistent and are often described as sour.[15]
Systemic conditions such as diabetes mellitus, pernicious anemia, Sjogren syndrome and Crohn's disease are also known to cause gustatory dysfunction.[16] Radiation therapy can injure the taste buds, transmitting nerves, and salivary glands, resulting in gustatory dysfunction.[16] Zinc deficiency is responsible for taste perception abnormalities in otherwise healthy persons and in drug-induced taste disorders.[17] Finally, aging or factors associated with aging may render individuals more vulnerable to gustatory dysfunction.[15]
Occasionally, patients complain that the sweet orange juice turns sour and bitter, if consumed immediately after they brush their teeth. This effect on sweet taste is transient and can be explained by the action of the detergent sodium dodecyl sulfate, a common ingredient in toothpastes.[5]
Clinical Assessment and Diagnosis
A clinician evaluating a patient who has gustatory dysfunction must understand that “taste” complaints are usually symptoms of an olfactory dysfunction. The distinction between true gustatory loss (bitter, sweet, salty, sour, or umami) and olfactory loss, the inability to perceive complex flavors of food, will help clarify the patient's diagnosis.[18] Qualitative gustatory dysfunction is more frequent than the quantitative dysfunction.[9] The incidence of taste disorders is the same among men and women, but that women with milder symptoms are more likely to seek treatment.[13] Gustatory dysfunction is often associated with nausea, decreased appetite, and dry mouth, especially in patient undergoing chemotherapy.[19]
When examining patients with gustatory dysfunction, comprehensive subjective assessment of the chief complaint, objective head, neck, oral evaluation, and review of the patient's medical, dental, medication, and social history is necessary.[1] Examinations using imaging techniques to rule out or prove the presence of damage to central nervous structures, and in particular to the brain stem, thalamus and pons, may be necessary. If bacterial or mycological diseases are suspected, swab tests may be carried out.[11]
Assessment of taste sensation can be done in an outpatient clinic by electro- or chemo-gustometry. In electrogustometry, weak electrical currents are applied to the various taste bud fields in the oral cavity. In chemogustometry, specific taste solutions are used to examine the taste sensitivity. A whole-mouth taste test is used to assess the patient's ability to detect, identify, and evaluate the intensity of different concentrations of sweet, salty, sour, and bitter taste solutions.[16] A spatial test is used to assess the different areas of the oral mucosa since localized areas of impairment can be undetected. A cotton swab dipped in a special taste solution is applied in different areas of the oral mucosa. The throat is evaluated by having a patient swallow part of each taste solution. The individual is requested to assess the quality and intensity of the taste.[16] Other test methods are based on presenting the stimuli in the form of a tastant-saturated filter paper or so-called taste strips with the dried tastants – the task of the patient is to identify the taste. When compared to taste solution, taste strips have the advantage of a long shelf life.[11]
For evaluation of a gustatory dysfunction, one can apply a topical anesthetic such as unflavored 2% lidocaine to the dorsal surface of the tongue. The anesthetic is applied starting from the left anterior 2/3, progressing toward the posterior 1/3, followed by the contralateral side in the same fashion. If the complaint is eliminated, then the source of taste disorder may be local. If the complaint persists and is unchanged, then the cause may be systemic or may originate from the central nervous system.[5]
Management
The success of treatment for gustatory dysfunction depends upon the etiology. An orofacial cause can usually be traced, treated and followed by the dental surgeon.[1] Many patients become concerned about the seriousness of their disorder and also develop depression. The thought of an untreatable, but not life-threatening disease, as most chemosensory disorders are, is often more acceptable for a patient than an undiagnosed one. Some taste disorders do not need any treatment, since they may resolve spontaneously.[5]
Zinc supplementation has been shown to be effective in the treatment of patients with taste disorders, especially patients undergoing radiotherapy or chemotherapy.[17] In cases of dysgeusia and burning mouth disorder (prevalent in postmenopausal women), tricyclic antidepressants and clonazepam can be helpful.[16] In case of severe dysgeusia topical anesthetics like lidocaine gel is indicated.[9] In case of trauma or surgery, no specific therapy is available, only time will tell whether the condition will improve.[16] Drug-related dysgeusia can be reversed with cessation of the offending agent. An artificial saliva may be helpful in patients with xerostomia.[2]
In the absence of specific treatment for a diagnosed gustatory dysfunction, the most important aspect of treatment is teaching the patient to cope with the disorder.[5] Some of the common self-care strategies used by patients with gustatory dysfunction include eating smaller and more frequent meals, using more condiments, using more fats and sauces, eating blander foods, adding something sweet to meats, sucking on hard candy, eating more boiled foods, using more salt, oral care before eating, eating cold foods, avoiding beef, and spicy foods.[19]
The clinician should be sensitive to the patient's psychological state. Depression may be the result of a taste disorder or contribute to a taste complaint. In either case, referral for psychological counseling may be considered, although not as a first step.[15] Furthermore, if a cause cannot be established, patients should be referred to a multidisciplinary taste and smell center.[1]
Conclusion
Gustatory dysfunctions present a number of difficulties to the clinicians like obscure etiology and inability to objectively assess the nature and degree of dysfunction. Future research is needed for a better understanding of chemosensory mechanisms and establishing improved diagnostic procedures. However, clinicians should be prepared to make appropriate evaluations, treatment or referrals.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ship JA, Chavez EM. Special senses: Disorders of smell and taste. In: Silverman S, Eversole LR, Truelove ED, editors. Essentials of Oral Medicine. Hamilton: BC Decker Inc; 2002. [Google Scholar]
- 2.Bromley SM. Smell and taste disorders: A primary care approach. Am Fam Physician. 2000;61:427–36. 438. [PubMed] [Google Scholar]
- 3.Barret KE, Barman SM, Boitano A, Brooks HL. 23rd ed. New Delhi: Tata McGraw Hill; 2010. Ganong's Review of Medical Physiology. [Google Scholar]
- 4.Lindemann B. Receptor seeks ligand: On the way to cloning the molecular receptors for sweet and bitter taste. Nat Med. 1999;5:381–2. doi: 10.1038/7377. [DOI] [PubMed] [Google Scholar]
- 5.Spielman AI. Chemosensory function and dysfunction. Crit Rev Oral Biol Med. 1998;9:267–91. doi: 10.1177/10454411980090030201. [DOI] [PubMed] [Google Scholar]
- 6.Widmaier EP, Raff H, Strang KT. 12th ed. New York: McGraw Hill; 2011. Vander's Human Physiology. [Google Scholar]
- 7.Mattes RD. Accumulating evidence supports a taste component for free fatty acids in humans. Physiol Behav. 2011;104:624–31. doi: 10.1016/j.physbeh.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viana F. Chemosensory properties of the trigeminal system. ACS Chem Neurosci. 2011;2:38–50. doi: 10.1021/cn100102c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welge-Lüssen A. Re-establishment of olfactory and taste functions. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2005;4:Doc06. [PMC free article] [PubMed] [Google Scholar]
- 10.Welge-Lüssen A, Gudziol H. Etiology, diagnostic and therapeutic management of taste disorders. Ther Umsch. 2004;61:302–7. doi: 10.1024/0040-5930.61.5.302. [DOI] [PubMed] [Google Scholar]
- 11.Hummel T, Landis BN, Hüttenbrink KB. Smell and taste disorders. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2011;10:Doc04. doi: 10.3205/cto000077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malaty J, Malaty IA. Smell and taste disorders in primary care. Am Fam Physician. 2013;88:852–9. [PubMed] [Google Scholar]
- 13.Hamada N, Endo S, Tomita H. Characteristics of 2278 patients visiting the Nihon University Hospital Taste Clinic over a 10-year period with special reference to age and sex distributions. Acta Otolaryngol Suppl. 2002;546:7–15. doi: 10.1080/00016480260046373. [DOI] [PubMed] [Google Scholar]
- 14.Doty RL, Shah M, Bromley SM. Drug-induced taste disorders. Drug Saf. 2008;31:199–215. doi: 10.2165/00002018-200831030-00002. [DOI] [PubMed] [Google Scholar]
- 15.Cowart BJ. Taste dysfunction: A practical guide for oral medicine. Oral Dis. 2011;17:2–6. doi: 10.1111/j.1601-0825.2010.01719.x. [DOI] [PubMed] [Google Scholar]
- 16.Mann NM. Management of smell and taste problems. Cleve Clin J Med. 2002;69:329–36. doi: 10.3949/ccjm.69.4.329. [DOI] [PubMed] [Google Scholar]
- 17.Najafizade N, Hemati S, Gookizade A, Berjis N, Hashemi M, Vejdani S, et al. Preventive effects of zinc sulfate on taste alterations in patients under irradiation for head and neck cancers: A randomized placebo-controlled trial. J Res Med Sci. 2013;18:123–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Wrobel BB, Leopold DA. Clinical assessment of patients with smell and taste disorders. Otolaryngol Clin North Am. 2004;37:1127–42. doi: 10.1016/j.otc.2004.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rehwaldt M, Wickham R, Purl S, Tariman J, Blendowski C, Shott S, et al. Self-care strategies to cope with taste changes after chemotherapy. Oncol Nurs Forum. 2009;36:E47–56. doi: 10.1188/09.onf.e47-e56. [DOI] [PMC free article] [PubMed] [Google Scholar]


