Abstract
Introduction:
Pain-free treatment to the patients is considered as an important treatment objective for orthodontic health care providers. However, many orthodontists underestimate the degree of pain experienced by the patients. Hence, this study was conducted as a randomized, double-blinded clinical trial with the following objectives.
Objective:
To study the pain characteristics after separator placement; to compare the efficacy of various commonly used analgesics in pain management and to determine the efficacy of pre- and post-operative analgesics in pain management.
Subjects and Methods:
Data were collected from 154 patients (77 males and 77 females, age group of 14-21 years, with mean age of 18.8 years) who reported to Department of Orthodontics. Patients were randomly divided in to four groups. Group 1: Paracetamol 650 mg, Group 2: Ibuprofen 400 mg, Group 3: Aspirin 300 mg, Group 4: Placebo and the study were conducted as a randomized, double-blinded clinical trial. The patients were instructed to take two tablets, one tablet 1 h before separator placement, and the other one after 6 h. The pain evaluations were made by the patients, when teeth not touching (TNT), biting back teeth together, chewing food (CF) using a 100-mm visual analogue scale for 7 days after separator placement. Patients were advised to record the severity of pain.
Results:
Group 3 (Aspirin 300 mg) showed lowest pain values, followed by Group 2 (ibuprofen 400 mg), and Group 1 (paracetamol 650 mg). All NSAID's achieved good pain control compared to Group 4 (placebo), where the intensity pain was maximum.
Conclusion:
Pre- and post-operative analgesics were found to be more effective in controlling orthodontic pain, after separator placement at all-time intervals.
KEY WORDS: Analgesics, orthodontic pain, pain management, separator placement, visual analogue scale
Pain is derived from a Greek word “Poine” which mean penalty or punishment. There is a reason to believe that it is inherent in any life linked with consciousness. Although, pain is of considerable significance to all health providers, many patients consider pain and orthodontic treatment to be synonymous and go hand in hand.
International Association for the Study of Pain describe pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”[1] Stedman's Medical Dictionary gives a more complete definition of pain as “an unpleasant sensation associated with actual or potential tissue damage and mediated by specific nerve fibers to the brain, where its conscious appreciation may be modified by various factors”.[2] This definition recognizes that pain may have a noxious transmission component, a psychological component and a very important modulatory component.
According to O’Connor's survey, pain is the greatest dislike during treatment and fourth among major fears and apprehensions prior to orthodontic treatment.[3] There is an increase in the expression of Calcitonin Gene-Related Peptide and Substance P during the first 2 days after application of an orthodontic force in the rat.[4,5] Similarly, clinical human studies show pain symptoms reach the peak approximately 1-2 days after force application.[6,7,8,9] Many factors like intensity and duration of forces applied, age, gender, the degree of crowding of the arch/arches, patient's psychological background and past experiences affect the extent of the symptoms. Therefore, orthodontic therapy with minimal patient discomfort is essential for an orthodontist to avoid noncompliance.
One would assume a large volume of research on the treatment related to pain, but unfortunately little is discussed by clinicians and orthodontist. Preoperative use of NSAIDs decrease the intensity of postoperative pain and swelling by inhibiting the “formation” of prostaglandins.[10]
Paracetamol, ibuprofen, and aspirin are first line analgesics which are generally available over the counter. Paracetamol (acetaminophen), which was first described by Von Mering (1893), is used commonly for its analgesic and antipyretic properties. Ibuprofen was the first member of propionic acid derivatives to be introduced in 1969. It is a nonselective inhibitor of cyclo-oxygenase-1 (COX-1) and COX-2 pathway.[11] Aspirin introduced in 1895 has been known to be an effective analgesic for many years and is commonly used throughout the world for many different pain conditions.
This randomized, double-blinded, prospective clinical trial aims at studying pain characteristics after separator placement; to compare the efficacy of various commonly used analgesics in pain management and to determine the efficacy of pre- and post-operative analgesics in pain management.
Subjects and Methods
Subjects
The proposed study was submitted for ethical committee approval and the same was approved based on ICMR guidelines. A total of 154 patients who attended Department of Orthodontics for fixed orthodontic appliance treatment were selected. Patients and their parents were informed about the procedure and informed consent was obtained for the same. A detailed case history which included past dental, past medical, allergic to any specific drugs was taken for all the patients.
The selection criteria were as follows:
Should be in the age group of 14-21 years
No previous orthodontic treatment
Should not be under any medication for systemic problems.
Should not be allergic to NSAID's
Should not have a history of asthma, gastritis, bleeding disorders
No teeth extraction at least 2 weeks before or after separator placement
Should not have any missing teeth.
Study design
Patients were randomly divided in to four groups.
Group 1: Paracetamol 650 mg
Group 2: Ibuprofen 400 mg
Group 3: Aspirin 300 mg
Group 4: Placebo.
The patients and the research assistant were blind to experimental groups. The patients were instructed to take two tablets, one tablet 1 h before separator placement and the other one after 6 h. Separators (AlastiK S-2 separator modules, 3M Unitek, Monrovia, Calif) were placed for first molars in all 4 quadrants preferably in the morning between 10 a.m. and 12 noon.
All patients were provided with a questionnaire which is in a form of seven page booklet that contained 100 mm horizontal visual analog scale (VAS). The patients were advised to mark the degree of pain as per the instructed time period in VAS. Pain intensity was recorded by the patients 2 h, 6 h after separator placement, bed time on the day of appointment, next day morning, and 2nd day morning, 3rd day, 7th day morning after separator placement. Patients were advised to record the severity of pain with teeth not touching (TNT), biting back teeth (BBT) together, and chewing food (CF). Patients were advised not to take any additional medication during the study period. The filled in questionnaire were collected in subsequent visit. Patients who did not take the given drug or who did not completely fill the questionnaire or who lost/removed the separators were excluded from the study.
Statistical analysis
The above data's were subjected to statistical analysis using SPSS IBM version 20 (Chicago, USA) systems. Descriptive measures like mean values and standard deviations for continuous variables and percentage for categorical variables were calculated. Tests of significance like independent t-test for comparing means were performed.
Results
Totally, 77 boys and 77 girls were included in the study. There were 11 dropouts in boys and 5 dropouts in girls. Finally, the study was carried out with 66 boys and 72 girls. There were 38 patients in Group 1 (Paracetamol 650 mg) with 18 boys and 20 girls and the dropouts were 3 and 1, respectively. Group 2 (Ibuprofen 400 mg) comprised 39 patients with 20 boys and 19 girls and the dropouts were 2 and 1, respectively. Group 3 (Aspirin 300 mg) comprised 36 patients with 18 boys and 18 girls and the dropouts were 2 and 0, respectively. Group 4 (placebo) comprised 41 patients with 21 boys and 20 girls and the dropouts were 4 and 3 respectively. The mean age of boys in Group 1, 2, 3, and 4 were 19.8, 19.5, 19.1, and 18.9 years, respectively. Similarly, mean age of girls in Group 1, 2, 3, and 4 were 19.5, 18.9, 18.6, and 18.0 years, respectively [Table 1].
Table 1.
VAS pain index scores recorded at different time intervals during TNT, BBT, and CF in four groups
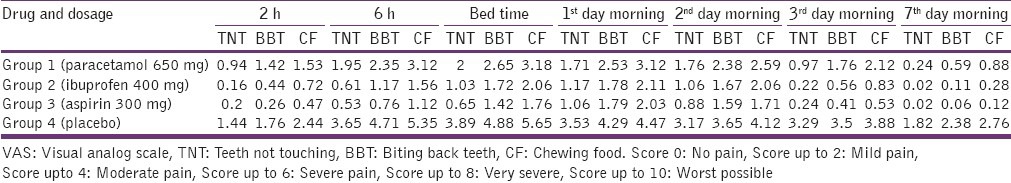
Pain experience of Group 1 (Patients taking paracetomol 650 mg one at 1 h before separator placement and another tablet 6 h after separator placement) [Figure 1]: When TNT, pain intensity gradually increased from mild pain after 2 h and 6 h to peak pain at bed time. The peak intensity at bedtime was found to be moderate pain. The pain then gradually decreased from next day morning to mild pain and was in decreasing intensity of mild pain thereafter. The pain intensity was nearing no pain on 7th day morning.
Figure 1.
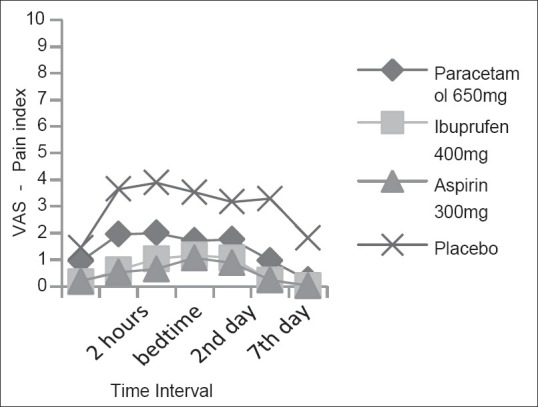
Mean pain scores at teeth not touching
When BBT [Figure 2], pain gradually increased from mild pain after 2 h to moderate pain until 2nd day morning and then decreased to mild pain on 3rd - and 7th - day morning. Peak intensity of pain was felt at bedtime, which was of moderate intensity.
Figure 2.
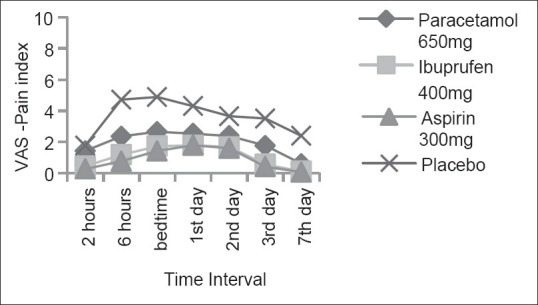
Mean pain scores at biting back teeth together
When CF [Figure 3], pain gradually increased from mild pain after 2 h to moderate pain which peaked at bed time. The pain was perceived as moderate until 3rd day morning and then decreased to mild pain on 7th day morning.
Figure 3.
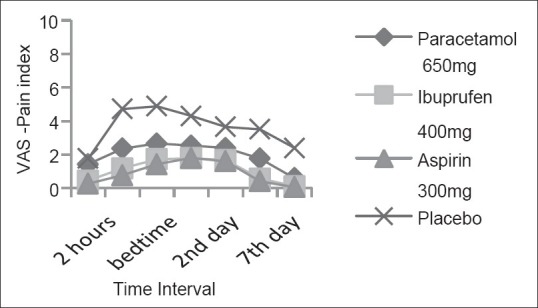
Mean pain scores at chewing foo
Pain experience of Group 2 (patients taking Ibuprofen 400 mg one at 1 h before separator placement and another tablet 6 h after separator placement) [Figure 1]: When TNT, pain intensity was mild throughout the time intervals. The pain intensity showed a gradual increase and peaked at next day morning after which there was a gradual decrease in pain intensity till 7th day morning. Pain intensity was nearing no pain from 3rd day morning.
When BBT pain perceived was mild pain thorough out the time interval [Figure 2]. There was a gradual increase in pain, which peaked at next day morning and then gradually reduced at 7th day morning and was nearing no pain on the 7th day morning [Figure 3].
When CF [Figure 3], pain gradually increased from mild pain after 2 h and 6 h to moderate pain which peaked at next day morning. The pain then decreased to mild pain on the 3rd day morning and was nearing no pain on the 7th day morning.
Pain experience of Group 3 (patients taking Aspirin 300 mg one at 1 h before separator placement and another tablet 6 h after separator placement) [Figure 1]: When TNT and back teeth biting, the pain perceived was mild throughout the time interval. There was a gradual increase in discomfort which peaked at next day morning and then gradually reduced thereafter nearing no pain from 3rd - and 7th - day morning when TNT and when back teeth biting respectively [Figure 2].
When CF [Figure 3], pain gradually increased from mild discomfort after 2 h to moderate pain at next day morning and then gradually decreased to mild discomfort on 2nd, 3rd day and was nearing no pain on 7th day morning.
Pain experience of Group 4 (patients taking placebo one at 1 h before separator placement and another tablet 6 h after separator placement) [Figure 1]: When TNT, the pain perceived was mild after 2 h and then gradually increased to moderate pain and peaked at bedtime. There was a gradual decrease in pain thereafter and reduced to mild pain on 7th day morning.
When BBT [Figure 2], pain gradually increased from mild pain after 2 h to severe pain until next day morning and then decreased to moderate pain from 2nd day morning onwards. Peak intensity of pain was felt at bedtime, which was of severe intensity.
When CF [Figure 3], pain gradually increased from moderate pain after 2 h to severe pain after 6 h to 2nd day morning. Then pain gradually decreased to moderate pain on 3rd day and 7th day morning.
In Group 4, on 7th day pain intensity was mild when TNT and moderate pain when BBT and CF. Whereas in Group 1 pain was nearing no pain on 7th day morning when TNT. In Group 2 and 3, pain was nearing no pain on the 3rd day morning when TNT and on the 7th day morning when BBT and CF. It was observed that pain peaked at bedtime in all groups and pain intensity was maximum while CF.
In Group 4, pain was severe at bedtime on the day of separator placement, whereas pain was perceived as moderate pain in Group 1 and 2 and as mild pain in Group 3.
Overall results showed Group 3 (Aspirin 300 mg) patients experienced very less pain in terms of mild discomfort, closely followed by Group 2 (Ibuprofen 400 mg). Group 1 (Paracetamol 650 mg) patients experienced mild to moderate pain on bed time and next day morning, after which gradually reduced to no pain from 3rd day morning. However, Group 4 (Placebo) patients had a bitter experience of moderate to severe pain at all-time intervals.
Discussion
Orthodontic tooth movement cause varying pain and discomfort to patients. Maximum pain is perceived on the 1st and 2nd day of orthodontic movement and decrease to minor levels after 5 days.[7,8,9] The sources for the pain in connection with orthodontic treatment are primarily due to the periodontal inflammatory reactions and consequent inflammatory reaction in pulpal tissues. The pulp circulation and tissue metabolism and even vitality may be affected or compromised by the applied forces.[12]
During orthodontic separator placement, the collagen fibers of periodontal ligament are disrupted. Initial healing of wounds in the periodontal ligament begins with blood clot and granulation tissue formation subsequent to necrosis regardless of the type of the periodontal challenge.[13] During organization of granulation tissue, vascular, and nervous components[14] as well as new periodontal connective tissue[15,16] enter the area. Nociceptive nerve fibers of periodontal ligament transmit pain impulses centrally and also release neuropeptides peripherally.[17] Nerve sprouting within the pulp in response to orthodontic forces, affect the functional properties of the intradental nerves and might potentiate dental pain sensitivity by multiplying the receptor sites.[18] All these factors induce pain, which peaks in 1 or 2 days of tooth movement. Hence, it would be appropriate to control pain with NSAIDS.
Measurement of pain
The VAS is a direct pain intensity scaling method in which the subjects evaluate the level of pain by making a mark on a continuous line. One end of the line means “no pain” and the other end “worst pain.” The advantages of using the VAS over observational, self-report, behavioral, physiological, or verbal rating scales, are the higher sensitivity, reproducibility, and reliability of the direct scaling techniques.[19] It also allows the use of parametric statistical tests.[20] On the other hand, the limitation of VAS is that the recorded values are mostly related to the intensity component of pain.
In this study, pain started 2 h after separator placement reached to peak level at the bed time and next day morning, approximately 24 h after separator placement. This is in agreement with the results of several other studies. Omur Polat and Karaman[21] have reported that pain intensity reached the maximum peak value 24 h after archwire placement.
Since any orthodontic procedure creates periodontal vasodilatation,[22] injury, pain and inflammation, analgesics should be prescribed for the effective control of pain. Preoperative analgesics reduces inflammatory response by effectively controlling prostaglandin production.[23,24] In this study, the analgesics taken both pre- (1 h before) and post-operatively (6 h after) created significant reduction in pain intensity compared to the placebo group.
2 h after separator placement, the patients taking Paracetamol, Ibuprofen, Aspirin showed low pain values at TNT, BBT together and CF. This is because of the preoperative analgesic effect, whereas the placebo group felt moderate pain.
6 h after, analgesics had a good control of pain. Aspirin and ibuprofen group felt mild pain during CF and BBT together, whereas in paracetamol group, the pain was moderate. Placebo started experiencing severe pain. Patients were advised to take postoperative analgesics at this time.
Visual analog scale scores measured at bed time and next day morning showed good pain control by analgesics. Paracetamol group again had moderate pain on next day morning, particularly during BBT together and CF. This is because of mechanism of action of paracetamol. It inhibits prostaglandin synthesis within the central nervous system and has little influence on peripheral prostaglandin synthesis, especially within inflamed tissues.[25] Placebo group continued with higher pain index at this time interval.
From 3rd day onwards, there was no pain in analgesic groups, whereas the pain slowly reduced in intensity in placebo group.
Throughout the course, NSAID's (Aspirin and Ibuprofen) elicited good control of pain followed by paracetamol (acetaminophen).
An analgesic with less side-effects should always be advised for pain management. NSAIDs are contraindicated for patients who have a current history of nephropathy, erosive or ulcerative conditions of the gastrointestinal mucosa, anticoagulant therapy, hemorrhagic disorders, or intolerance or allergy to any NSAID. They also should be avoided during pregnancy because prostaglandins maintain patency of the ductus arteriosus during fetal development. In all cases, where NSAIDs are contraindicated, paracetamol is the conventional nonopioid alternative and it can be given for orthodontic pain management, since it has analgesic efficiency comparable with other NSAIDs.[26]
Conclusion
The present study was performed to assess the experienced pain as reported by the patients at different times after the placement of separators. The following conclusions were arrived.
Pre- and post-operative analgesics were found to be more effective in controlling orthodontic pain, after separator placement at all-time intervals
Aspirin 300 mg effectively controls pain than 400 mg ibuprofen, followed by 650 mg paracetamol
The safety of analgesics should be considered while choosing an analgesic.
Only intensity of pain was considered in this study. Further studies are required to evaluate and access the duration of pain to determine the dosage of drug, which is equally important.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Okeson JP. 6th ed. Chicago: Quintessence; 2005. Bell's Orofacial Pains: The Clinical Management of Orofacial Pain; p. 6. [Google Scholar]
- 2.Stedman TL. 27th ed. Baltimore: Lippincott Williams and Wilkins; 2000. Stedman's Medical Dictionary; p. 1297. [Google Scholar]
- 3.O’Connor PJ. Patients’ perceptions before, during, and after orthodontic treatment. J Clin Orthod. 2000;34:591–2. [PubMed] [Google Scholar]
- 4.Kvinnsland I, Kvinnsland S. Changes in CGRP-immunoreactive nerve fibres during experimental tooth movement in rats. Eur J Orthod. 1990;12:320–9. doi: 10.1093/ejo/12.3.320. [DOI] [PubMed] [Google Scholar]
- 5.Norevall LI, Forsgren S, Matsson L. Expression of neuropeptides (CGRP, substance P) during and after orthodontic tooth movement in the rat. Eur J Orthod. 1995;17:311–25. doi: 10.1093/ejo/17.4.311. [DOI] [PubMed] [Google Scholar]
- 6.Furstman L, Bernick S. Clinical considerations of the periodontium. Am J Orthod. 1972;61:138–55. doi: 10.1016/0002-9416(72)90092-9. [DOI] [PubMed] [Google Scholar]
- 7.Wilson S, Ngan P, Kess B. Time course of the discomfort in young patients undergoing orthodontic treatment. Pediatr Dent. 1989;11:107–10. [PubMed] [Google Scholar]
- 8.Ngan P, Wilson S, Shanfeld J, Amini H. The effect of ibuprofen on the level of discomfort in patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1994;106:88–95. doi: 10.1016/S0889-5406(94)70025-7. [DOI] [PubMed] [Google Scholar]
- 9.Jones M, Chan C. The pain and discomfort experienced during orthodontic treatment: A randomized controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofacial Orthop. 1992;102:373–81. doi: 10.1016/0889-5406(92)70054-e. [DOI] [PubMed] [Google Scholar]
- 10.Jackson DL, Moore PA, Hargreaves KM. Preoperative nonsteroidal anti-inflammatory medication for the prevention of postoperative dental pain. J Am Dent Assoc. 1989;119:641–7. doi: 10.1016/s0002-8177(89)95018-6. [DOI] [PubMed] [Google Scholar]
- 11.Tripathi KD. Essentials of Medical Pharmacology. 5th ed. New Delhi: Jaypee Brothers; 2002. Non steroidal anti inflammatory drugs and anti pyretic analgesics. [Google Scholar]
- 12.Biesterfeld RC, Taintor JF, Marsh CL. The significance of alterations of pulpal respiration. A review of literature. J Oral Pathol. 1979;8:129–39. doi: 10.1111/j.1600-0714.1979.tb01819.x. [DOI] [PubMed] [Google Scholar]
- 13.Sismanidou C, Hilliges M, Lindskog S. Healing of the root surface-associated periodontium: An immunohistochemical study of orthodontic root resorption in man. Eur J Orthod. 1996;18:435–44. doi: 10.1093/ejo/18.5.435. [DOI] [PubMed] [Google Scholar]
- 14.Parlange LM, Sims MR. A T.E.M. stereological analysis of blood vessels and nerves in marmoset periodontal ligament following endodontics and magnetic incisor extrusion. Eur J Orthod. 1993;15:33–44. doi: 10.1093/ejo/15.1.33. [DOI] [PubMed] [Google Scholar]
- 15.Melcher AH. On the repair potential of periodontal tissues. J Periodontol. 1976;47:256–60. doi: 10.1902/jop.1976.47.5.256. [DOI] [PubMed] [Google Scholar]
- 16.Wikesjö UM, Nilvéus RE, Selvig KA. Significance of early healing events on periodontal repair: A review. J Periodontol. 1992;63:158–65. doi: 10.1902/jop.1992.63.3.158. [DOI] [PubMed] [Google Scholar]
- 17.Davidovitch Z. Tooth movement. Crit Rev Oral Biol Med. 1991;2:411–50. doi: 10.1177/10454411910020040101. [DOI] [PubMed] [Google Scholar]
- 18.Khayat BG, Byers MR, Taylor PE, Mecifi K, Kimberly CL. Responses of nerve fibers to pulpal inflammation and periapical lesions in rat molars demonstrated by calcitonin gene-related peptide immunocytochemistry. J Endod. 1988;14:577–87. doi: 10.1016/S0099-2399(88)80054-2. [DOI] [PubMed] [Google Scholar]
- 19.Duncan GH, Bushnell MC, Lavigne GJ. Comparison of verbal and visual analogue scales for measuring the intensity and unpleasantness of experimental pain. Pain. 1989;37:295–303. doi: 10.1016/0304-3959(89)90194-2. [DOI] [PubMed] [Google Scholar]
- 20.Bhat M. Statistical analysis and design characteristics of studies on dentinal sensitivity. Endod Dent Traumatol. 1986;2:165–71. doi: 10.1111/j.1600-9657.1986.tb00605.x. [DOI] [PubMed] [Google Scholar]
- 21.Polat O, Karaman AI. Pain control during fixed orthodontic appliance therapy. Angle Orthod. 2005;75:214–9. doi: 10.1043/0003-3219(2005)075<0210:PCDFOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Stanfeld J, Jones J, Laster L, Davidovitch Z. Biochemical aspects of orthodontic tooth movement. I. Cyclic nucleotide and prostaglandin concentrations in tissues surrounding orthodontically treated teeth in vivo. Am J Orthod Dentofacial Orthop. 1986;90:139–48. doi: 10.1016/0889-5406(86)90046-6. [DOI] [PubMed] [Google Scholar]
- 23.Steen Law SL, Southard KA, Law AS, Logan HL, Jakobsen JR. An evaluation of preoperative ibuprofen for treatment of pain associated with orthodontic separator placement. Am J Orthod Dentofacial Orthop. 2000;118:629–35. doi: 10.1067/mod.2000.110638. [DOI] [PubMed] [Google Scholar]
- 24.Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, Jakobsen JR. The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofacial Orthop. 2001;120:20–7. doi: 10.1067/mod.2001.115616. [DOI] [PubMed] [Google Scholar]
- 25.Kimmey MB. Cardioprotective effects and gastrointestinal risks of aspirin: Maintaining the delicate balance. Am J Med. 2004;117(Suppl 5A):72S–8. doi: 10.1016/j.amjmed.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 26.Cooper SA. Comparative analgesic efficacies of aspirin and acetaminophen. Arch Intern Med. 1981;141:282–5. doi: 10.1001/archinte.141.3.282. [DOI] [PubMed] [Google Scholar]


