Abstract
Introduction:
The bonding of orthodontic brackets and their failure rates by both direct and in-direct procedures are well-documented in orthodontic literature. Over the years different adhesive materials and various indirect bonding transfer procedures have been compared and evaluated for bond failure rates. The aim of our study is to highlight the use of a simple, inexpensive and ease of manipulation of a single thermo-plastic transfer tray and the use the of a single light cure adhesive to evaluate the bond failure rates in clinical situations.
Materials and Methods:
A total of 30 patients were randomly divided into two groups (Group A and Group B). A split-mouth study design was used, for, both the groups so that they were distributed equally with-out bias. After initial prophylaxis, both the procedures were done as per manufactures instructions. All patients were initially motivated and reviewed for bond failures rates for 6 months.
Results:
Bond failure rates were assessed for over-all direct and indirect procedures, anterior and posterior arches, and for individual tooth. Z-test was used for statistically analyzing, the normal distribution of the sample in a spilt mouth study. The results of the two groups were compared and P value was calculated using Z-proportion test to assess the significance of the bond failure.
Conclusion:
Over-all bond failure was more for direct bonding. Anterior bracket failure was more in-direct bonding than indirect procedure, which showed more posterior bracket failures. In individual tooth bond failure, mandibular incisor, and premolar brackets showed more failure, followed by maxillary premolars and canines.
KEY WORDS: Bond failure, split-mouth design, thermo-plastic transfer tray
The bonding of orthodontic attachments to etched enamel surface is a well-established clinical procedure. There are at present direct[1] and indirect[2] procedures to bond the attachments to the teeth. The advantages and disadvantages of both the procedures were tested for bond failure rates for many years with biased results.[3,4,5] The operator preference for direct over indirect was 13:1 in spite of the advantages of Indirect procedure.[6] Over the years both indirect technique and adhesive material used have been constantly undergoing new innovations, but seemingly costly.
Therefore, the aim of our study is to highlight the use of a simple, practitioner friendly, inexpensive and ease of manipulation, of a single thermo-plastic transfer tray material along with single light cure adhesive to evaluate the bond failure rates in clinical situations when both the procedures are used in split-mouth design.
Materials and Methods
The armamentarium used were diagnostic instruments, thermo-plastic sheets (2 mm), bio-star machine, light cure equipment, Transbond XT resin and bonding agent, study casts, MBT -022 brackets and gauge [Figure 1].
Figure 1.
Division of samples. Group- A (Green) - Direct bonding Group B (Red) - Indirect Bonding
A total of 32 patients who came for orthodontic treatment, requiring fixed orthodontic appliance therapy were taken for the study. All patients had full complement of tooth, with good oral hygiene. Patients with deep-bite, crowns and veneers, and partially erupted cases were excluded from the study. The patients were randomly divided into two groups: Group A and Group B. A split-mouth design was used to randomize the study sample.
Division of sample
Patients were randomly divided into two groups (Group A and Group B). A splitmouth study design was used. For each patient, both the sides contained, both the groups so that they were distributed equally with out bias. After initial prophylaxis, both the procedures were done as per manufactures instructions. All patients were initially motivated and reviewed for bond failures and recorded for six months.
Split-mouth design
Group A: Consisted of fifteen patients with maxillary right and mandibular left quadrants bonded using direct bonding technique, whereas contra-lateral sides were bonded using indirect bonding technique.
Group B: Consisted of 15 patients with maxillary left and mandibular right quadrants bonded using direct bonding technique, whereas contra-lateral sides were bonded using indirect bonding technique.
Transfer tray fabrication for indirect bonding procedure[Figure 2]
Figure 2.
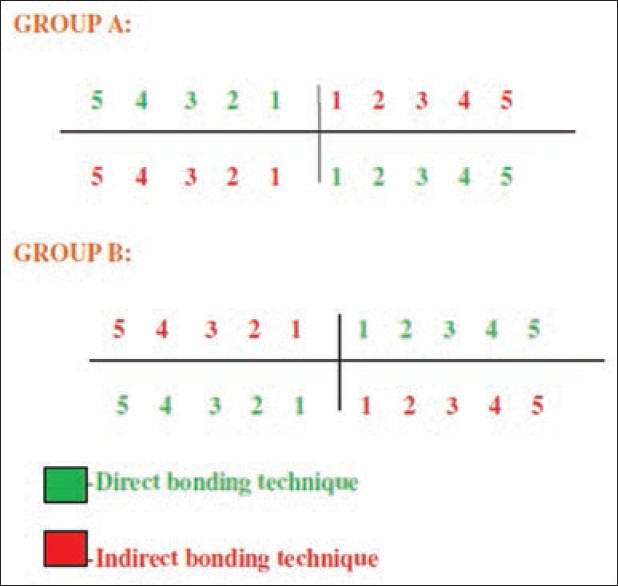
Split- Mouth Technique. Group- A (Green) - Direct bonding Group B (Red) - Indirect Bonding
A customized method of indirect bonding was followed for all patients, using transparent thermo-plastic sheet of 2 mm thickness. Accurate alginate impressions of both arches were made and the models were poured with-out voids or air bubbles. When the models were absolutely dried, the long axis of the teeth was marked and MBT bracket positioning gauge was used to mark the vertical height for individual teeth. A thin coat of separating medium (cold mold seal) was diluted with water (1:3 ratio) applied evenly all over the model and allowed to dry for 24 h.[7]
Transbond XT light cure adhesive was evenly spread over the bracket mesh and placed onto the dental model with respect to the long axis and vertical height markings. The excess flash was removed and each bracket was cured for 20 s each side (occlusal and gingival) to form the custom base.[8]
Transfer trays were constructed using soft clear thermo-plastic sheet of 2 mm thickness in a bio-star machine.[9] The formed tray was then dipped in warm water for 30 min allowing the separating medium to dissolve, which facilitate easy removal of tray from the model with-out any distortion. The transfer trays for all patients were extended 2 mm below the gingival margin on buccal and lingual/palatal side. The bracket hook areas be trimmed/cut off the bonding tray to permit easy removal.[6]
The transfer trays were then gently rinsed with running tap water to remove the separating medium and allowed to dry for 30 min. Each of custom base was cleaned by applying methyl methacrylate monomer about 10 min prior to bonding and then thoroughly dried. Brackets were then bonded to the tooth for both methods as per manufacturer's instructions.
Results
A total of 30 patients were included in this study (18 females, 12 males, mean age 21.73 years, range: 15-28 years). A total of 518 brackets, were bonded, of which 256 were placed using direct bonding technique and 262 were placed using indirect bonding technique.
Since the data were paired from contra-lateral quadrants in split-mouth study and the distribution not normal, statistical analysis involved the use of the Z-test. A Z-test is any statistical test for which the distribution of the test statistic under the null hypothesis can be approximated by a normal distribution. Because of the central limit theorem, many test statistics are approximately normally distributed for large samples.
For comparing two groups results (failure or success outcomes), the Z-proportion test was used. P values were calculated using standard normal probability distribution functions, used to reject or accept the hypothesis of equality in proportions of two independent groups.
Overall failure rate
A total of 50 brackets were debonded from both groups (9.6% failure rate) over observation period of 6 months. Of the brackets placed with direct bonding technique, 27 brackets debonded (10.5% failure rate), whereas 23 brackets debonded (8.8% failure rate) when using indirect bonding technique [Table 1].
Table 1.
Over all failure rate between the groups
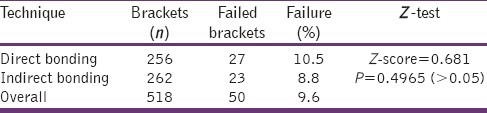
The Z-score was 0.681 and the P value was 0.4965. Since P > 0.05, the null hypothesis was accepted. The result was that there was no statistically significant (P > 0.05) difference between direct and indirect bonding technique in-terms of bond failure rate.
Bond failure rate for anteriors and posterior brackets for both procedures
In the anterior teeth, 19 brackets failed (10.8% failure rate) with direct bonding technique and 11 brackets failed (6.2% failure rate) with indirect bonding technique. In the posterior teeth, 8 brackets failed (9.8% failure rate) with direct bonding technique and 12 brackets failed (14.4% failure rate) with indirect bonding technique [Table 2].
Table 2.
Anterior and posterior failure rates between the groups
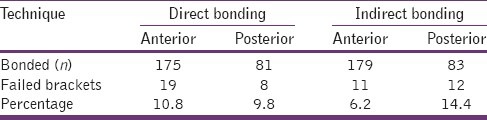
For the anterior comparison, Z-score was 1.592. The P value was 0.11184. Since P > 0.05, the null hypothesis was accepted. The result was not significant at <0.05. For the posterior comparison, the Z-score was - 0.896. The P value was 0.36812. Since P > 0.05, the null hypothesis was accepted. The result was not significant at <0.05.
Failure rate for individual tooth
Individual tooth failure rate showed, in-direct bonding technique mandibular centrals had highest failure rate of 20% followed by maxillary canine of 16.6%, whereas in indirect bonding technique, mandibular 2nd premolars had highest failure rate of 18.8% followed by mandibular 1st premolar and maxillary 2nd premolar of 16.6% respectively [Table 3].
Table 3.
Individual teeth failure rates between the groups
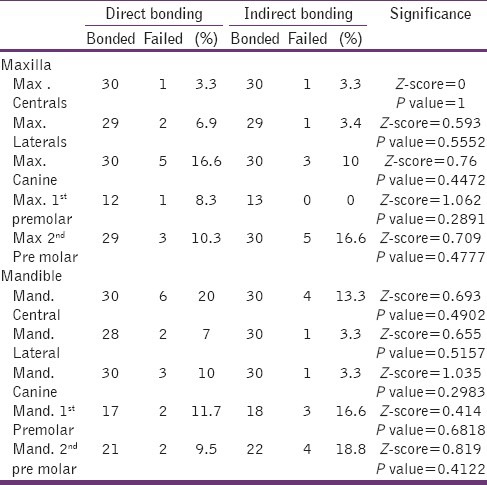
Since P > 0.05 for the entire individual tooth, the null hypothesis was accepted. The result was not significant at <0.05.
Discussion
Bonding of orthodontic attachments to tooth can be accomplished either through direct or indirect methods. The advent of direct bonding procedure and the light cure resins have given the operator an unlimited working time and ease of work in minimizing errors during bonding. Direct bonding is still more preferred procedure than indirect bonding by most of the operators. However, achieving an accurate and consistent bracket positioning for the posterior continues to pose a problem because of inaccessibility. A significantly superior, efficient and effective indirect bonding methods has been developed, which has improved accuracy and reduced chair side time for both patient and the operator over the last three decades.[8,9,10]
In addition to being a highly sensitive technique, indirect bonding has two significant disadvantages. First, the occluso-gingival insertion of the transfer tray causes the adhesive coated brackets to scrape along the tooth surface resulting in uneven distribution, rather than perpendicular placement. Second, when opaque trays were used the putty covering the palatal side prevent the light from entering the palatal and occlusal aspect during curing.[11]
In this study, both the direct and indirect bonding technique were done using split-mouth design to eliminate the bias between right and left side and between upper and lower bonding. Forces from mastication and hygiene maintenance can also be an important factor for bond failure between right and left side.[12]
The “On command” curing advantages of light cured resin over auto polymerization resins, in bond failure rates have been studied by many authors with no significant difference between them.[13,14] The bond strength and bond survival rate of Conventional halogen and high speed curing (light-emitting diode, plasma) were compared, to be of little or no significant between them.[15,16]
The transfer tray used in indirect bonding, in this study is 2 mm soft thermo-plastic sheet. Light intensity is inversely proportional to the square of the distance from light source. The dual trays used in the earlier studies, not only increased the distance of the light source from the bracket but may act as a factor to reduce the light intensity for curing.[7] If a light cure is used with tray technique, the tray has to be transparent enough to allow light transmission [Figure 3].[17]
Figure 3.

Related to transfer tray procedures
Bond failure rate of direct and indirect bonding methods have been compared for many decades. In our study, the overall bond failure rate between direct and indirect bonding was found to be 10.5% and 8.8% respectively with no significant statistical difference between the two. The results of this study were similar to earlier studies[5,18] with no significant difference between the two methods. In our study, there was proportionate increase in bond failure rate of both the methods when compared to the other mentioned studies, which could be attributed to the dissimilar materials used, population bias and motivation factor. A bond failure rate below 10% is clinically acceptable as suggested by Cal-Neto et al.[19]
In our study, comparing the anterior and posterior brackets, the indirect method showed more bond survival rate than direct, in the anterior than posterior. Though the difference was not statistically significant, the increase in bond failure could be attributed to arch alignment discrepancy at the start of the treatment.[12] Bond failure in posterior segment for indirect method, was suggested to be due to difficulty in transfer tray removal and seepage of saliva between the tray and tooth on the etched tooth. Furthermore, variation in adhesive thickness during tray insertion, leading to uneven adhesive distribution could be the possible factor for the bond failure. Adhesive thickness up to 0.5 mm had no significant effect on bond strength.[15]
In individual tooth bond failure rate, the mandibular centrals showed the maximum failure rates. The reason could be attributed to varying trauma from incisive forces.[12] The bond failure of mandibular and maxillary premolar brackets in indirect method showed more failure rates, due to saliva seepage,[3] variation in adhesive thickness, other reasons suggested are aprismatic enamel and increased curvature of buccal surface may affect micro mechanical bond strength of the brackets.[8,12,15,20]
Conclusions
In this study, Bond failures were observed due to various reasons, which were found to be in concurrence with other earlier studies. The bond failure rate was found to be <10% for over-all comparison, anterior – posterior comparison, and individual tooth comparison, which was clinically acceptable. Bond failures that resulted from transfer tray removal were due to operator's error. Debonding of brackets was also recorded due to occlusal interference from high masticatory load and tooth brushing as heard from the patients. The operator error could be reduced, and adequate patient motivation could prevent some of these avoidable etiological factors in increasing bond survival rate.
Hence, concluding this study, that bond survival rate in both the methods, using the transparent thermo-plastic transfer tray of 2 mm thickness, had no significant differences between them. This transfer tray method was time saving, inexpensive and ease of manipulation with-out compromising on the bonding procedure. Both the technique exhibited their advantages and disadvantages in the course of this study. Finally, it will be the operators choice to feel the convenience of procedure to use them to their advantage.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Newman GV. Epoxy adhesives for orthodontic attachments: Progress report. Am J Orthod. 1965;51:901–12. doi: 10.1016/0002-9416(65)90203-4. [DOI] [PubMed] [Google Scholar]
- 2.Silverman E, Cohen M, Gianelly AA, Dietz VS. A universal direct bonding system for both metal and plastic brackets. Am J Orthod. 1972;62:236–44. doi: 10.1016/s0002-9416(72)90264-3. [DOI] [PubMed] [Google Scholar]
- 3.Zachrisson BU, Brobakken BO. Clinical comparison of direct versus indirect bonding with different bracket types and adhesives. Am J Orthod. 1978;74:62–78. doi: 10.1016/0002-9416(78)90046-5. [DOI] [PubMed] [Google Scholar]
- 4.Read MJ, O’Brien KD. A clinical trial of an indirect bonding technique with a visible light-cured adhesive. Am J Orthod Dentofacial Orthop. 1990;98:259–62. doi: 10.1016/S0889-5406(05)81603-8. [DOI] [PubMed] [Google Scholar]
- 5.Aguirre MJ, King GJ, Waldron JM. Assessment of bracket placement and bond strength when comparing direct bonding to indirect bonding techniques. Am J Orthod. 1982;82:269–76. doi: 10.1016/0002-9416(82)90461-4. [DOI] [PubMed] [Google Scholar]
- 6.Gorelick L. Bonding/the state of the art. A national survey. J Clin Orthod. 1979;13:39–53. [PubMed] [Google Scholar]
- 7.Krug AY, Conley RS. Shear bond strengths using an indirect technique with different light sources. J Clin Orthod. 2005;39:485–7. [PubMed] [Google Scholar]
- 8.Sondhi A. Efficient and effective indirect bonding. Am J Orthod Dentofacial Orthop. 1999;115:352–9. doi: 10.1016/s0889-5406(99)70252-0. [DOI] [PubMed] [Google Scholar]
- 9.Moshiri F, Hayward MD. Improved laboratory procedure for indirect bonding. J Clin Orthod. 1979;13:472–3. [PubMed] [Google Scholar]
- 10.Koo BC, Chung CH, Vanarsdall RL. Comparison of the accuracy of bracket placement between direct and indirect bonding techniques. Am J Orthod Dentofacial Orthop. 1999;116:346–51. doi: 10.1016/s0889-5406(99)70248-9. [DOI] [PubMed] [Google Scholar]
- 11.Husain A, Ansari T, Mascarenhas R, Shetty S. A new approach to indirect bonding. J Clin Orthod. 2009;43:652–4. [PubMed] [Google Scholar]
- 12.Kinch AP, Taylor H, Warltier R, Oliver RG, Newcombe RG. A clinical trial comparing the failure rates of directly bonded brackets using etch times of 15 or 60 seconds. Am J Orthod Dentofacial Orthop. 1988;94:476–83. doi: 10.1016/0889-5406(88)90005-4. [DOI] [PubMed] [Google Scholar]
- 13.Sonis AL. Comparison of a light-cured adhesive with an autopolymerizing bonding system. J Clin Orthod. 1988;22:730–2. [PubMed] [Google Scholar]
- 14.Armas Galindo HR, Sadowsky PL, Vlachos C, Jacobson A, Wallace D. An in vivo comparison between a visible light-cured bonding system and a chemically cured bonding system. Am J Orthod Dentofacial Orthop. 1998;113:271–5. doi: 10.1016/s0889-5406(98)70296-3. [DOI] [PubMed] [Google Scholar]
- 15.Manzo B, Liistro G, De Clerck H. Clinical trial comparing plasma arc and conventional halogen curing lights for orthodontic bonding. Am J Orthod Dentofacial Orthop. 2004;125:30–5. doi: 10.1016/j.ajodo.2003.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Koupis NS, Eliades T, Athanasiou AE. Clinical evaluation of bracket bonding using two different polymerization sources. Angle Orthod. 2008;78:922–5. doi: 10.2319/072807-351.1. [DOI] [PubMed] [Google Scholar]
- 17.Read MJ, Pearson AI. A method for light-cured indirect bonding. J Clin Orthod. 1998;32:502–3. [PubMed] [Google Scholar]
- 18.Thiyagarajah S, Spary DJ, Rock WP. A clinical comparison of bracket bond failures in association with direct and indirect bonding. J Orthod. 2006;33:198–204. doi: 10.1179/146531205225021615. [DOI] [PubMed] [Google Scholar]
- 19.Cal-Neto JP, Miguel JA. An in vivo evaluation of bond failure rates with hydrophilic and self-etching primer systems. J Clin Orthod. 2005;39:701–2. [PubMed] [Google Scholar]
- 20.Millett DT, Hallgren A, Cattanach D, McFadzean R, Pattison J, Robertson M, et al. A 5-year clinical review of bond failure with a light-cured resin adhesive. Angle Orthod. 1998;68:351–6. doi: 10.1043/0003-3219(1998)068<0351:AYCROB>2.3.CO;2. [DOI] [PubMed] [Google Scholar]


