Abstract
Microglia, the only non-neuroepithelial cells found in the parenchyma of the central nervous system (CNS), originate during embryogenesis from the yolk sac and enter the CNS quite early (embryonic day 9.5-10 in mice). Thereafter, microglia are maintained independently of any input from the blood and in particular do not require hematopoietic stem cells as a source of replacement for senescent cells. Monocytes are hematopoietic cells, derived from bone marrow. The ontogeny of microglia and monocytes is important for understanding CNS pathologies. Microglial functions are distinct from those of blood-derived monocytes, which invade the CNS only under pathological conditions. Recent data reveal that microglia play an important role in managing neuronal cell death, neurogenesis and synaptic interactions. Here we discuss physiology of microglia and the functions of monocytes in CNS pathology. We address the roles of microglia and monocytes in neurodegenerative diseases as an example of CNS pathology.
Introduction
Microglia are resident mononuclear phagocytes in the central nervous system (CNS) which are traditionally considered to be involved mainly in immune responses and inflammatory diseases. Perivascular, choroid plexus and meningeal macrophages, monocyte-derived cells, are also phagocytic cells in the CNS and have at times been referred to as either macrophages or microglia without specifically addressing their origin. Over the past two decades, research on brain myeloid cells has been markedly improved by the advent of new tools in imaging, genetics and immunology, and has opened up a new era in understanding and treating CNS pathologies.
Recent studies revealed that microglia are the only myeloid cells found in the healthy CNS parenchyma. Microglia and monocyte-derived cells are distinct by their ontogeny, physiology, and response to environmental changes. When the CNS is inflamed, all these cells can give rise to macrophages, as defined by morphology and surface staining-yet functions of individual macrophages may differ radically, according to their ontogeny. Understanding macrophage ontogeny and functions will help to determine potential roles of modulating microglial activation and monocyte infiltration in disease treatment.
Ontogeny
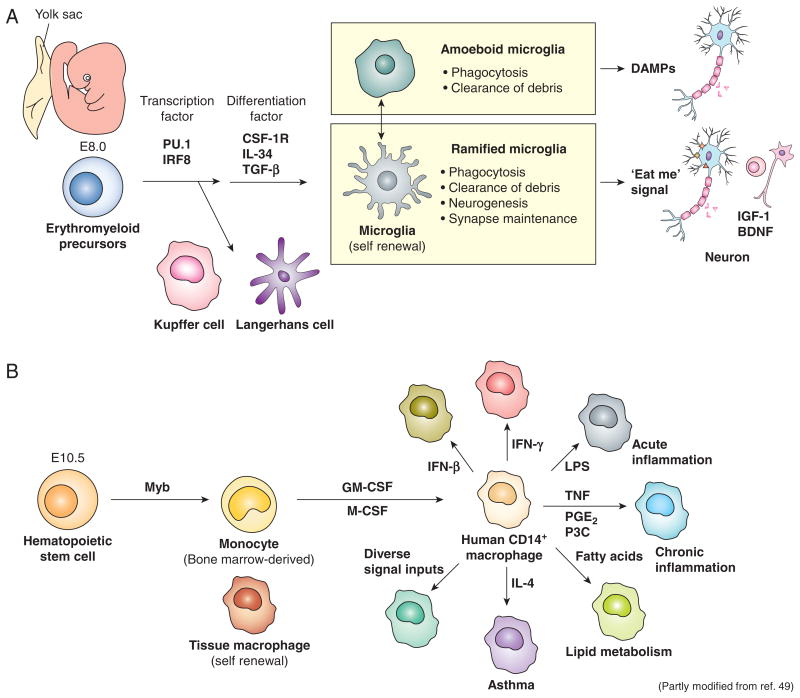
Monocytes are blood mononuclear cells and are renewed continually from bone-marrow hematopoietic stem cells throughout life. During postnatal life, myeloid progenitor cells in the bone marrow give rise to common monocyte-dendritic-cell progenitors, which in turn yield blood monocytes and dendritic-cell progenitors. Tissue macrophages can be derived early in development from yolk-sac primitive macrophages and subsequently from blood monocytes and circulating mononuclear phagocyte progenitors. Tissue macrophages are maintained either by local self-renewal or by influx of cells from the circulation (1).In mice, hematopoietic cells appear within the hematogenic endothelium of the aorta-gonado-mesonephros region at E10.5 (2) and migrate to the fetal liver, where they expand and differentiate starting from E12.5 (3). The transcription factor Myb is required for development of hematopoietic stem cells and all CD11bhigh monocytes and macrophages, but is dispensable for yolk sac macrophages and for the development of yolk sac-derived F4/80bright macrophages in several tissues, such as liver Kupffer cells, epidermal Langerhans cells, and microglia-cell populations that are Pu.1-dependent (4) (Figure 1).
Figure 1.
Microglia and monocytes ontogeny and their characteristics. Microglia are derived from primitive macrophages in a Myb-independent manner via PU.1- and IRF8- dependent pathways. This lineage is mainly regulated by CSF-1R, its ligand IL-34 and TGF-β. Microglia are maintained independently of circulating monocytes throughout life. In the steady state apoptotic neurons expressing ‘eat-me’ signals are removed by ramified microglia. Ramified microglia are also essential component of neurogenesis and synapse maintenance. Microglial IGF-1 and BDNF are key mediators of synaptic plasticity. In response to tissue damage, DAMPs are released and cause microglia to release of neurotoxic factors from microglia. Monocytes are derived from hematopoietic stem cells appear at E 10.5. Transcription factor Myb is required for development. Human CD14+ macrophage has several spectrum of activation signatures depending on a stimuli.
Microglial origin and developmental lineage were controversial and a consensus about microglial ontogeny was reached only recently. According to one view, microglia were thought to originate from a neuroepithelial precursor while others proposed that meningeal macrophages penetrated the brain during embryonic development, when they were first isolated from leech CNS preparations in 1920. Later, in the 1990s, post-natal and adult microglia were proposed to be derived from blood-borne monocytes (5).
It is now recognized that the late-embryonic and adult mouse brain parenchyma contain microglial progenitors (6) which have been detected in the brain rudiment from embryonic day 8 (E8), after their appearance in the yolk sac (7). It was established in late 90's that microglia were not epithelial, using mice that lack the transcriptional factor PU.1 (Pu.1-/- mice), which is expressed exclusively in cells of the hematopoietic lineage (8). Pu.1-/- mice lack not only microglia in the CNS but also the myeloid lineage as well as B cells and T cells. In vivo lineage tracing studies also showed that adult microglia derive from primitive myeloid progenitors that arise embryonically mainly between E7.0 and E7.5 and that they are highly proliferative throughout embryonic life (9). Moreover, it was shown that postnatal hematopoietic progenitors do not contribute to microglial homeostasis in the adult mouse brain, using irradiated newborns with hematopoietic cells isolated from congenic mice, adult congenic bone marrow chimera models and parabiotic mice (9). Postnatal microglia are maintained independently of circulating monocytes throughout life (10) and dying microglia are replaced entirely from cells that colonize the brain before birth. It remains uncertain whether new microglia arise by asymmetric division from an uncharacterized progenitor or by symmetric division from another microglial cell. In addition, during experimental autoimmune encephalomyelitis in which hematopoietic cells infiltrate the CNS, their presence is transient and they do not contribute to the microglial pool (11). Given these results, microglia are a cardinal example of a tissue macrophage population derived from embryonic progenitors in the yolk sac and maintained independently of input from hematopoietic stem cells.
Microglia also differ from monocytes by virtue of the factors that regulate their development. Colony stimulating factor-1 (CSF-1) and its receptor (CSF-1R) control the differentiation of most macrophage populations in adult mice. During embryogenesis, however, CSF-1R expression is required for yolk sac macrophages and microglial development, but not for monocytes (9). Additionally, interleukin-34 (IL-34) and CSF-1, the established ligands of CSF-1R, act in complementary and partially-compensatory fashion towards microglia. In particular, IL-34 deficiency affects microglial cell number in specific regions of the adult brain (12), indicating a selective role for IL-34 in microglial survival and homeostasis in the adult brain. Extending these insights, it was found that mouse microglia derive from primitive c-kit+ erythromyeloid precursors that are detected in the yolk sac as early as E8 (13). Also, microgliogenesis is not only dependent on Pu.1, but also requires Irf8, whereas Myb, Id2, Batf3 and Klf4 are not required (13). TGF-β was recently identified as a major differentiation factor for microglia (Figure 1). The lack of TGF-β affects microglial development beginning at E14.5, but does not affect microglial progenitors at the E10.5 stage (14). A deeper understanding of the mechanisms that control developmental microglial proliferation and differentiation, as well as maintenance in the adult brain is important for clarifying microglial responses to brain disorders and how it differs from that of monocyte-derived cells.
Microglial functions in the CNS
As macrophages of the CNS, microglia are the primary immune effector cells in the brain parenchyma. A more comprehensive understanding shows that microglia contribute materially to brain development and homeostasis, as their activities include regulation of cell death, synapse elimination, neurogenesis, and neuronal surveillance, in the healthy brain. Microglial cells also promote programmed neuronal cell death during development. A recent study using Nanostring expression profiling and Ingenuity Pathway Analysis®revealed that the functions most associated with microglia were related to nervous system development (14). Based on these physiological functions, microglial responses in pathological states will define disease outcomes as much by loss-of-homeostatic function as by gain-of-toxic function or deployment-of-protective or trophic function. This concept is lost when microglia are termed “resting” or “activated”. In that sense, these categories are no longer useful.
Microglia and neuronal cell death
Highly ramified microglia were presumed to be resting and inactive in the healthy brain. In vivo imaging approaches significantly changed our view of microglia by showing that they are found in a state of continuous spontaneous movement in the healthy adult brain (15, 16). Microglia constantly scan their environment, including neurons and astrocytes, with long cellular processes that undergo continuous cycles of extension, withdrawal and de novo formation (15). This physiological motility may in part serve a housekeeping function, enabling microglial cells to effectively patrol the microenvironment and to clear accumulated metabolic products and deteriorated tissue components.
Amoeboid microglia phagocytose apoptotic neurons associated with programmed cell death (PCD)(17). This process is understood to comprise a number of discrete signaling interactions, including microglial response to neuronal ‘eat-me’ signals, microglia priming neurons for PCD, and microglia directly triggering PCD by the release of neurotoxic substances (18, 19). In mammals, one ‘eat-me’ signal is phosphatidylserine (PS), which is exposed on the outer leaflet of the plasma membrane of dying or highly-stressed cells (20). In addition, apoptotic cells display multiple ‘eat-me’ markers and their combinatorial signaling to phagocytes (including down regulation of ‘don't eat-me’ signals) enhances engulfment. PS binds adhesive ‘bridging’ molecules present in extracellular fluid such as C3bi, which promotes phagocytosis through its recognition by complement-receptor-3 (CR3/CD11b) expressed by macrophages. Milk fat globule epidermal growth factor-8 (MGF-E8; lactadherin) is a soluble protein that can bind PS and serve as an adaptor to vitronectin receptor (αv β3/5 integrins) on phagocytes to promote uptake of apoptotic or stressed cells. Calreticulin and annexin A1 colocalize with PS on the surface of apoptotic cells (21, 22). Brain-specific angiogenesis inhibitor 1 (BAI1) is a receptor that directly recognizes PS on apoptotic cells and promotes phagocytosis (23). The externalization of PS on neurons is not synonymous with cell death and is reversible. Under specific circumstances, microglia may accordingly phagocytose viable neurons and contribute to pathogenesis (24)(Figure 1).
In the healthy CNS, microglia remove cellular debris without changing their ramified phenotype. In large CNS injuries causing extensive neuronal death, demyelination or blood hemorrhage, signals termed damage associated molecular patterns (DAMPs) are released by damaged neural cells or provided by plasma proteins, to which microglia are never exposed in the healthy brain. DAMPs promote microglial morphological transformation and gene-expression changes, likely by altering the balance between ‘on’ and ‘off’ signals. ‘Off’ signals are generated constitutively in the healthy brain and help to establish the physiological microglial phenotype. Many of the known ‘off’ signals are neuronally-derived, including fractalkine paired with the microglial receptor CX3CR1;CD200 paired with microglial CD200R1;CD22 with microglial CD45; CD47 with microglial CD172a/SIRPα (25) and TREM2b (1, 26). Additionally, the blood-brain barrier excludes all plasma proteins, so that entry of these components delivers a potent ‘on’ signal to microglia. In pathological states ‘on’ signals such as increased extracellular ATP and UTP from damaged neural cells prevail over ‘off’ signals, resulting in the phenotypic change of microglial cells, including altered morphology, proliferative capacity and gene expression.
Microglia and neurogenesis
In mammals including primates, neurogenesis occurs predominantly in the subgranular zone (SGZ) of the dentate gyrus in the hippocampal formation and in the subventricular zone (SVZ) of the lateral ventricle (27). Neurogenesis occurs throughout life in the adult brain and ramified microglia are an essential component of the neurogenic niche in the SGZ of the adult hippocampus. Apoptotic neurons are removed by ramified microglia in the healthy CNS. Microglia direct the migration and differentiation of neural progenitor cells (NPCs) by secreting soluble factors that promote neurogenesis (28). During the first postnatal week of life, Layer V cortical neurons require microglial accumulation along subcerebral and callosal projection axons because microglia-derived insulin-like growth factor 1 (IGF-1) is an important factor for neuron survival (29). In adult mice, removal of microglial brain-derived neurotrophic factor (BDNF) resulted in deficits in multiple learning tasks and significant reduction in motor-learning-dependent synapse formation (30). Microglial BDNF increased neuronal tropomysin-related kinase receptor (Trk)-B phosphorylation, a key mediator of synaptic plasticity, which suggests that microglia have important physiological functions by promoting learning-related synapse formation (30) (Figure 1).
Signaling by fractalkine (CX3CL1) to its receptor (CX3CR1) is a well characterized example of a neuron-microglia communication system in the neurogenic niche. CX3CR1 is expressed by all microglia in the brain and CX3CL1 is constitutively expressed at high levels on healthy neurons. Lack of or a reduction in CX3CR1 results in decreased neurogenesis, disruption of hippocampal circuit integrity and impairments in spatial learning and other behavioral and learning tasks (31, 32). Neuronal loss and enhanced neurodegeneration and inflammation also occur in models of Parkinson's disease and amyotrophic lateral sclerosis (26). Reintroducing CX3CL1 into the hippocampus of aged animals rescues the decreasing neurogenesis generally observed in aging animals (33). These studies suggest that microglial dysfunction has a significant impact on neuronal function.
Microglia and synapses in neuronal circuits
There has been extensive investigation of putative roles of microglia in the context of disease, including injury models, cerebral ischemia and neurodegenerative diseases. Microglia have been attributed an extraordinary ability to respond rapidly and perform a broad range of functions. For example, in the laser-lesion model, microglia near the site of the laser-ablated lesion respond within minutes by polarizing their highly motile processes towards the lesion (16). Microglia in cerebral ischemic lesions dramatically increase synaptic contacts, followed by frequent disappearance of the presynaptic terminal (34). Further analysis showed that microglia play a role in remodeling synapses under physiological conditions, particularly during development. Microglia interact with spines, synaptic terminals, and synaptic clefts in the developing primary mouse visual cortex V1 in vivo (35). Spines often change size upon microglial contact and the spines that microglia alter are eliminated, suggesting that microglia may be key regulators of structural spine plasticity and elimination of spines. Furthermore, retinal transforming growth factor (TGF)-β secreted by astrocytes regulates neuronal C1q expression, resulting in C3-dependent microglial synaptic elimination in the developing brain (36). Of note, these activities of microglia are regulated by neuronal activity.
It was hypothesized that microglia play an active role in either synapse stripping, a process in which microglia selectively remove synapses from injured neurons. However, several studies of nerve injury show that microglia proliferation following the injury is not an essential process in the remodeling or withdrawal of presynaptic contacts from an injured neuron (37). In murine prion disease, the loss of presynaptic boutons is an initial event preceding degeneration of the cell body. Also, in amyotrophic lateral sclerosis, synapses at the neuromuscular junction degenerate prior to the cell body. It is suggested that the presynaptic degeneration occurs independent of synaptic activity and synaptic vesicle recycling (38, 39), and that the synaptic loss is a neuron-autonomous event facilitated without direct involvement of microglial cells (40). Understanding mechanisms of synapse degeneration will be crucial, as cognitive decline is strongly correlated with loss of presynaptic terminals.
Monocyte functions in the CNS
The CNS is immune-privileged, secluded from circulation by the blood brain barrier, and is equipped with its own myeloid cell population, the microglial cells. Based on the classical perspective of immune-brain interactions, infiltrating macrophages were traditionally viewed as pathogenic by definition. However, over the past two decades, research has revealed a pivotal role of monocyte-derived macrophages in CNS repair and has opened up new avenues for understanding and treating CNS pathologies. Here we discuss the diversity of monocyte-derived macrophages, the induction and resolution of inflammation as well as monocyte involvement in neural tissue regeneration and renewal, matrix remodeling, debris clearance and angiogenesis.
Monocyte surface markers
Because of the diversity of monocyte-derived macrophages, their roles in the CNS are controversial. Monocyte-derived macrophages have multiple subpopulations according to their locations, surface markers and phenotypes. Distinct types of macrophages are found in different locations in the CNS, including perivascular cells, meningeal macrophages and blood-borne monocytes, and they differ in their morphology and functions (41, 42). Monocytes are blood mononuclear cells that express CD11b, CD11c, CD14 and (variably) CD16 in humans, and CD11b and CD45 in mice. In the CNS, perivascular macrophages, meningeal macrophages and choroid plexus macrophages, which control local immune surveillance, express CX3CR1CD11b+ CD45hi. While inflammatory monocytes (Ly6Chi CCR2+ CX3CR1lo) are highly motile and are rapidly recruited to inflamed tissues, a non-overlapping population of blood monocytes (Ly6Clo CCR2lo/neg CX3CR1hi) are proposed to be important for patrolling along blood vessels (and are termed ‘patrolling monocytes’ (43). In steady state, Ly6Clo monocytes originate from Ly6Chi blood monocytes (44). The Ly6Chi CCR2+ monocytes are able to produce inflammatory molecules, such as tumor necrosis factor (TNF)-α and inducible nitric oxide synthase (iNOS) (45). Disease-specific mobilization and recruitment of CD11b+Ly6Chi CCR2+ monocytes into the inflamed CNS was recently observed in a number of studies (46, 47).
Phenotypes of macrophages
Macrophages have remarkable plasticity that allows them to efficiently respond to environmental signals and change their phenotype, and their physiology can be markedly altered by both innate and adaptive immune responses. Two useful macrophage phenotypes are termed M1 (IFN-γ-stimulated inflammatory macrophages) and M2 (IL4—or IL13-stimulated alternatively activated cells). The reckless application of these limited polarized state terminologies to other circumstances threatens to vitiate their meaning. It has been universally observed that the myeloid compartment has an extremely broad transcriptional repertoire depending on the different environmental signals in chronic inflammation, chronic infection, or cancer. A study of human macrophages with transcriptome–based network analysis delineated nine distinct macrophage activation programs (48) expressed in response to a suite of stimuli in vitro. When adding stimuli such as free fatty acids, high-density lipoprotein (HDL), or stimuli associated with chronic inflammation, a spectrum of macrophage-activation signatures quickly overwhelmed the bipolar axis demonstrated by cells treated with type II IFN or IL4/13 (Figure 1). This group also identified transcription factors associated with particular phenotypes. Further understanding of the transcriptional regulation of macrophages would help to selectively target specific subsets therapeutically.
Are monocytes “Bad” or “Good” in the CNS?
Monocytes are heterogeneous under neurodegenerative conditions in the CNS. Anti-inflammatory treatment with FK506 or minocycline, a synthetic tetracycline derivative, decreases phagocytic activation and lesion size after injury and confers variable degrees of neuroprotection in spinal cord injury, traumatic brain injury, and stroke (49-51). Early depletion of presumed peripheral macrophages using clodronate diminishes secondary tissue damage and was shown to have some beneficial effect (52). However, monocyte-derived macrophages also show immune-resolving characteristics and express anti-inflammatory cytokines. These cells contribute to motor function recovery following spinal cord injury (53) and promote survival of neurons and cell renewal in the injured retina (54). Moreover, they restrict accumulation of other inflammatory leukocytes including neutrophils and resident microglia, mediate debris clearance by phagocytosis, and regulate the extracellular matrix and glial scarring surrounding the damaged area (55).
In the multiple sclerosis model experimental autoimmune encephalitis (EAE), CCR2+ Ly6Chigh monocytes are rapidly recruited to the inflamed CNS and play a crucial role in the effector phase of the disease (47). MHC classII-expressing macrophages are responsible for reactivation of pathogenic T cells at the CNS borders, the subarachnoid spaces of the meninges, and the perivascular spaces of the blood-brain barrier (56). Using double Cx3cr1GFP/CCR2RFP transgenic mice, it was shown that both Ly6chigh/CX3CR1low and Ly6clow/CX3CR1high monocyte-derived macrophages are present at the demyelination sites in EAE, while only the former are recruited in a CCR2-dependent manner and are believed to contribute to the activation of resident microglia (57).
One remaining question is: How do microglia and monocytes communicate with or regulate each other? Even when a stimulus is strong but short-lived, microglia can potentially cope with the danger signal, performing clearance of neurotoxic factors, supporting regeneration, and secreting neurotrophic factors supportive of remyelination. However, when the stimulus is intense or chronic, microglia can no longer handle the damage. These cells become neurotoxic and release reactive oxygen species, NO, proteases and inflammatory cytokines, all of which endanger neuronal activity (58). These activation stimuli result in signals for recruitment of monocytes to the damage site, which provide functions such as restriction of inflammation, restoration of homeostasis and support healing and renewal. In a mouse model of amyotrophic lateral sclerosis (ALS), microglia expressed increased CCL2 and other chemotaxis-associated molecules, which led to the recruitment of monocytes to the CNS (59). Impaired CX3CR1 signaling alters monocyte recruitment and its subsets after spinal cord injury (60). As a result, a CD11b+ Ly6Clo iNOS+ MHCII+ CD11c- population dominates the injury site of wild-type mice, while CD11b- CCR2+ Ly6Chi MHCII- CD11c+ cells predominate in spinal cord of CX3CR1GFP/GFP knockout mice. Mechanisms controlling diversity in CNS macrophages are not well defined.
Microglia and monocytes in neurodegenerative diseases
Alzheimer's disease
Alzheimer's disease (AD) is a neurodegenerative disease characterized by progressive loss of memory and other cognitive functions. Pathological characteristics of the AD brain are amyloid-β (Aβ) accumulation, neurofibrillary tangles (NFT), synaptic loss and neurodegeneration. Microglia accumulate around senile plaques in patients with AD and in animal models of AD. However, their role in the pathogenesis of AD remains to be elucidated. The response of microglia to Aβ peptides has been studied intensively since it was proposed that phagocytosis of these peptides by microglia could ameliorate the pathogenic cascade that occurs in the brains of AD patients. Microglia secrete proteolytic enzymes that degrade Aβ (61), and express receptors that promote the clearance and phagocytosis of Aβ (62, 63). However, microglia are also activated by Aβ and, once activated release inflammatory mediators which could promote AD pathology (64). It has been demonstrated with live imaging by two-photon microscopy that Cx3cr1 knockout prevents neuronal loss in a triple-transgenic mouse model of AD (65), although the extent of neuronal loss in this model is modest. Lack of CX3CR1 in microglia disrupts CX3CL1-CX3CR1 interactions, dysregulates microglial activity induced by neuronal stress, and results in enhanced release of soluble factors including IL-1 from activated microglia. Other studies showed that Cx3cr1 deficiency results in a gene dose-dependent reduction in Aβ deposition (66). Moreover, Cx3cr1-/- microglia had enhanced ability to phagocytose Aβ. Elucidating the regulatory effect of CX3CR1 on microglial functions in specific pathological environments will contribute to developing novel neurotherapeutics.
The role of monocytes in AD pathology has been reported to be beneficial. Studies using various conditional cell-depletion strategies in a mouse model of AD have shown that blood-derived macrophages can prevent the formation of or eliminate Aβ deposits (67, 68). Especially, the recruited blood-derived macrophages contribute to efficient amyloid elimination while arresting the local production of pro-inflammatory factors, including TNF (69). Stimulating perivascular macrophage turnover reduced cerebral amyloid angiopathy load independently of clearance by microglia (70). Monocyte-derived perivascular macrophages restrict vascular amyloid (dependent on CCR2) and promote Aβ transit to the vessel lumen. CX3CR1+ monocytes interact with Aβ+ vessel walls and take up Aβ (dependent on CX3CR1). Additionally, an important role of Ly6C-negative monocytes on clearance of vascular Aβ has been reported in AD transgenic mice (71). Using intravital two-photon microscopy, it was demonstrated that patrolling Ly6Clo monocytes monitor veins containing small Aβ aggregates, but not Aβ-positive arteries or Aβ-free blood vessels. These monocytes crawl inside the lumen of blood vessels independently of the direction of blood flow, scavenging Aβ. Moreover, the crawling monocytes carrying Aβ in veins recirculate back into the bloodstream. Depletion of Ly6C-negative monocytes increased amyloid load in the cortex and hippocampus. These data suggest the possibility of Ly6C-negative monocytes as a therapeutic target in AD.
Recent studies revealed multiple genetic risk factors for susceptibility to AD, including polymorphic variants of the myeloid cell molecules CD33 and TREM2. The expression of CD33 in microglial cells in AD brain is increased, and the numbers of CD33+cells correlated with insoluble Aβ levels (72). CD33 expression on monocytes is also observed and these cells have a reduced ability to phagocytose Aβ (73). In vitro, TREM2 on microglial cells, functions to stimulate phagocytosis on one hand and to suppress cytokine production and inflammation on the other (74, 75). In particular, TREM2 knockdown impaired phagocytosis of apoptotic neurons and increased TNFα and iNOS expression (75). These molecules may therefore have the ability to suppress inflammatory responses during the period of debris clearance after CNS injury.
Parkinson's disease
Parkinson's disease (PD), another neurodegenerative disorder, is characterized by the loss of dopaminergic neurons and dystrophic neurites in the substantia nigra. Mice deficient in CX3CR1 show increased microglial activation and enhanced dopaminergic cell loss in the substantia nigra after LPS administration (26). It was also shown that CD200-CD200R blocking exacerbates neurodegeneration in a rat model (76). Moreover, CX3CR1GFP/+ microglia have cell-to-cell contact with neurons and some microglia penetrate neuronal somata (77). These results suggest possible microglial involvement in the pathogenesis of PD. Infiltration of monocytes has not been reported and the role of monocytes in PD is unknown. DAP12 knock-in mice in which macrophages are defective in their number and functions results in less neuronal loss in murine model of PD compared with naïve mice, and further analyses to resolve the different role between microglia and monocytes are required.
Amyotrophic lateral sclerosis
Amyotrophic lateral sclerosis (ALS) is another neurodegenerative disease affecting the motor system. There is increasing evidence that microglia are key components in ALS motor neuron degeneration. Mutation in superoxide dismutase 1 (mSOD1) is the most prominent cause of familial ALS. mSOD1 motor neurons co-cultured with wild-type microglia did not exhibit cell death, while mSOD1 microglia could induce wild-type motor neuron degeneration (78). Similarly, deletion of mSOD37R specifically from CD11b+myeloid cells extended the survival of mice significantly, particularly during the late phase of disease (79). Moreover, microglia express CCL2 and other chemotaxis-associated molecules, which lead to the recruitment of CCR2+ Ly6Chi monocytes to the spinal cord. This monocyte recruitment correlates with neuronal loss (59). Of note, transplantation of mSOD1G93A microglia into PU.1-/- mice did not induce motor neuron degeneration, indicating that mSOD1 in microglia alone is not sufficient to initiate disease (80).
Conclusions
We have briefly discussed differences between microglia and monocytes in terms of their origin and the roles in the CNS. Although triggers of microglia and monocyte reaction in diseases have been extensively studied, it these phenomena are complex and differ from disease to disease. Further efforts to reveal how they are controlled will be required.
Acknowledgments
We thank Lisa Spangler and Chris Nelson for their helpful suggestions.
Footnotes
Financial support: Research in the Ransohoff lab is supported by the NIH, the National MS Society, the Alzheimer's Association, the Guthy Jackson Charitable Foundation, the Department of Defense and the Williams Family Fund. We apologize to those whose work could not be discussed due to space constraints.
Abbreviations used in this article: CNS, central nervous system; PCD, programmed cell death; PS, phosphatidylserine; AD, Alzheimer's disease; Aβ, amyloid-β.
References
- 1.Ransohoff RM, Cardona AE. The myeloid cells of the central nervous system parenchyma. Nature. 2010;468:253–262. doi: 10.1038/nature09615. [DOI] [PubMed] [Google Scholar]
- 2.Boisset JC, van Cappellen W, Andrieu-Soler C, Galjart N, Dzierzak E, Robin C. In vivo imaging of haematopoietic cells emerging from the mouse aortic endothelium. Nature. 2010;464:116–120. doi: 10.1038/nature08764. [DOI] [PubMed] [Google Scholar]
- 3.Orkin SH, Zon LI. Hematopoiesis: an evolving paradigm for stem cell biology. Cell. 2008;132:631–644. doi: 10.1016/j.cell.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schulz C, Gomez Perdiguero E, Chorro L, Szabo-Rogers H, Cagnard N, Kierdorf K, Prinz M, Wu B, Jacobsen SE, Pollard JW, Frampton J, Liu KJ, Geissmann F. A lineage of myeloid cells independent of Myb and hematopoietic stem cells. Science. 2012;336:86–90. doi: 10.1126/science.1219179. [DOI] [PubMed] [Google Scholar]
- 5.Ling EA, Wong WC. The origin and nature of ramified and amoeboid microglia: a historical review and current concepts. Glia. 1993;7:9–18. doi: 10.1002/glia.440070105. [DOI] [PubMed] [Google Scholar]
- 6.Alliot F, Lecain E, Grima B, Pessac B. Microglial progenitors with a high proliferative potential in the embryonic and adult mouse brain. Proceedings of the National Academy of Sciences of the United States of America. 1991;88:1541–1545. doi: 10.1073/pnas.88.4.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alliot F, Godin I, Pessac B. Microglia derive from progenitors, originating from the yolk sac, and which proliferate in the brain. Brain research Developmental brain research. 1999;117:145–152. doi: 10.1016/s0165-3806(99)00113-3. [DOI] [PubMed] [Google Scholar]
- 8.McKercher SR, Torbett BE, Anderson KL, Henkel GW, Vestal DJ, Baribault H, Klemsz M, Feeney AJ, Wu GE, Paige CJ, Maki RA. Targeted disruption of the PU.1 gene results in multiple hematopoietic abnormalities. The EMBO journal. 1996;15:5647–5658. [PMC free article] [PubMed] [Google Scholar]
- 9.Ginhoux F, Greter M, Leboeuf M, Nandi S, See P, Gokhan S, Mehler MF, Conway SJ, Ng LG, Stanley ER, Samokhvalov IM, Merad M. Fate mapping analysis reveals that adult microglia derive from primitive macrophages. Science. 2010;330:841–845. doi: 10.1126/science.1194637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ajami B, Bennett JL, Krieger C, Tetzlaff W, Rossi FM. Local self-renewal can sustain CNS microglia maintenance and function throughout adult life. Nature neuroscience. 2007;10:1538–1543. doi: 10.1038/nn2014. [DOI] [PubMed] [Google Scholar]
- 11.Ajami B, Bennett JL, Krieger C, McNagny KM, Rossi FM. Infiltrating monocytes trigger EAE progression, but do not contribute to the resident microglia pool. Nature neuroscience. 2011;14:1142–1149. doi: 10.1038/nn.2887. [DOI] [PubMed] [Google Scholar]
- 12.Greter M, Lelios I, Pelczar P, Hoeffel G, Price J, Leboeuf M, Kundig TM, Frei K, Ginhoux F, Merad M, Becher B. Stroma-derived interleukin-34 controls the development and maintenance of langerhans cells and the maintenance of microglia. Immunity. 2012;37:1050–1060. doi: 10.1016/j.immuni.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kierdorf K, Erny D, Goldmann T, Sander V, Schulz C, Perdiguero EG, Wieghofer P, Heinrich A, Riemke P, Holscher C, Muller DN, Luckow B, Brocker T, Debowski K, Fritz G, Opdenakker G, Diefenbach A, Biber K, Heikenwalder M, Geissmann F, Rosenbauer F, Prinz M. Microglia emerge from erythromyeloid precursors via Pu.1- and Irf8-dependent pathways. Nature neuroscience. 2013;16:273–280. doi: 10.1038/nn.3318. [DOI] [PubMed] [Google Scholar]
- 14.Butovsky O, Jedrychowski MP, Moore CS, Cialic R, Lanser AJ, Gabriely G, Koeglsperger T, Dake B, Wu PM, Doykan CE, Fanek Z, Liu L, Chen Z, Rothstein JD, Ransohoff RM, Gygi SP, Antel JP, Weiner HL. Identification of a unique TGF-beta-dependent molecular and functional signature in microglia. Nature neuroscience. 2014;17:131–143. doi: 10.1038/nn.3599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nimmerjahn A, Kirchhoff F, Helmchen F. Resting microglial cells are highly dynamic surveillants of brain parenchyma in vivo. Science. 2005;308:1314–1318. doi: 10.1126/science.1110647. [DOI] [PubMed] [Google Scholar]
- 16.Davalos D, Grutzendler J, Yang G, Kim JV, Zuo Y, Jung S, Littman DR, Dustin ML, Gan WB. ATP mediates rapid microglial response to local brain injury in vivo. Nature neuroscience. 2005;8:752–758. doi: 10.1038/nn1472. [DOI] [PubMed] [Google Scholar]
- 17.Marin-Teva JL, Cuadros MA, Calvente R, Almendros A, Navascues J. Naturally occurring cell death and migration of microglial precursors in the quail retina during normal development. The Journal of comparative neurology. 1999;412:255–275. [PubMed] [Google Scholar]
- 18.Marin-Teva JL, Cuadros MA, Martin-Oliva D, Navascues J. Microglia and neuronal cell death. Neuron glia biology. 2011;7:25–40. doi: 10.1017/S1740925X12000014. [DOI] [PubMed] [Google Scholar]
- 19.Marin-Teva JL, Dusart I, Colin C, Gervais A, van Rooijen N, Mallat M. Microglia promote the death of developing Purkinje cells. Neuron. 2004;41:535–547. doi: 10.1016/s0896-6273(04)00069-8. [DOI] [PubMed] [Google Scholar]
- 20.Fadok VA, Bratton DL, Rose DM, Pearson A, Ezekewitz RA, Henson PM. A receptor for phosphatidylserine-specific clearance of apoptotic cells. Nature. 2000;405:85–90. doi: 10.1038/35011084. [DOI] [PubMed] [Google Scholar]
- 21.Fricker M, Oliva-Martin MJ, Brown GC. Primary phagocytosis of viable neurons by microglia activated with LPS or Abeta is dependent on calreticulin/LRP phagocytic signalling. Journal of neuroinflammation. 2012;9:196. doi: 10.1186/1742-2094-9-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McArthur S, Cristante E, Paterno M, Christian H, Roncaroli F, Gillies GE, Solito E. Annexin A1: a central player in the anti-inflammatory and neuroprotective role of microglia. Journal of immunology. 2010;185:6317–6328. doi: 10.4049/jimmunol.1001095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mori K, Kanemura Y, Fujikawa H, Nakano A, Ikemoto H, Ozaki I, Matsumoto T, Tamura K, Yokota M, Arita N. Brain-specific angiogenesis inhibitor 1 (BAI1) is expressed in human cerebral neuronal cells. Neuroscience research. 2002;43:69–74. doi: 10.1016/s0168-0102(02)00018-4. [DOI] [PubMed] [Google Scholar]
- 24.Neher JJ, Emmrich JV, Fricker M, Mander PK, Thery C, Brown GC. Phagocytosis executes delayed neuronal death after focal brain ischemia. Proceedings of the National Academy of Sciences of the United States of America. 2013;110:E4098–4107. doi: 10.1073/pnas.1308679110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Beek EM, Cochrane F, Barclay AN, van den Berg TK. Signal regulatory proteins in the immune system. Journal of immunology. 2005;175:7781–7787. doi: 10.4049/jimmunol.175.12.7781. [DOI] [PubMed] [Google Scholar]
- 26.Cardona AE, Pioro EP, Sasse ME, Kostenko V, Cardona SM, Dijkstra IM, Huang D, Kidd G, Dombrowski S, Dutta R, Lee JC, Cook DN, Jung S, Lira SA, Littman DR, Ransohoff RM. Control of microglial neurotoxicity by the fractalkine receptor. Nature neuroscience. 2006;9:917–924. doi: 10.1038/nn1715. [DOI] [PubMed] [Google Scholar]
- 27.Gage FH. Mammalian neural stem cells. Science. 2000;287:1433–1438. doi: 10.1126/science.287.5457.1433. [DOI] [PubMed] [Google Scholar]
- 28.Walton NM, Sutter BM, Laywell ED, Levkoff LH, Kearns SM, Marshall GP, 2nd, Scheffler B, Steindler DA. Microglia instruct subventricular zone neurogenesis. Glia. 2006;54:815–825. doi: 10.1002/glia.20419. [DOI] [PubMed] [Google Scholar]
- 29.Ueno M, Fujita Y, Tanaka T, Nakamura Y, Kikuta J, Ishii M, Yamashita T. Layer V cortical neurons require microglial support for survival during postnatal development. Nature neuroscience. 2013;16:543–551. doi: 10.1038/nn.3358. [DOI] [PubMed] [Google Scholar]
- 30.Parkhurst CN, Yang G, Ninan I, Savas JN, Yates JR, 3rd, Lafaille JJ, Hempstead BL, Littman DR, Gan WB. Microglia promote learning-dependent synapse formation through brain-derived neurotrophic factor. Cell. 2013;155:1596–1609. doi: 10.1016/j.cell.2013.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rogers JT, Morganti JM, Bachstetter AD, Hudson CE, Peters MM, Grimmig BA, Weeber EJ, Bickford PC, Gemma C. CX3CR1 deficiency leads to impairment of hippocampal cognitive function and synaptic plasticity. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:16241–16250. doi: 10.1523/JNEUROSCI.3667-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paolicelli RC, Bolasco G, Pagani F, Maggi L, Scianni M, Panzanelli P, Giustetto M, Ferreira TA, Guiducci E, Dumas L, Ragozzino D, Gross CT. Synaptic pruning by microglia is necessary for normal brain development. Science. 2011;333:1456–1458. doi: 10.1126/science.1202529. [DOI] [PubMed] [Google Scholar]
- 33.Bachstetter AD, Morganti JM, Jernberg J, Schlunk A, Mitchell SH, Brewster KW, Hudson CE, Cole MJ, Harrison JK, Bickford PC, Gemma C. Fractalkine and CX 3 CR1 regulate hippocampal neurogenesis in adult and aged rats. Neurobiology of aging. 2011;32:2030–2044. doi: 10.1016/j.neurobiolaging.2009.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wake H, Moorhouse AJ, Jinno S, Kohsaka S, Nabekura J. Resting microglia directly monitor the functional state of synapses in vivo and determine the fate of ischemic terminals. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009;29:3974–3980. doi: 10.1523/JNEUROSCI.4363-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tremblay ME, Lowery RL, Majewska AK. Microglial interactions with synapses are modulated by visual experience. PLoS biology. 2010;8:e1000527. doi: 10.1371/journal.pbio.1000527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bialas AR, Stevens B. TGF-beta signaling regulates neuronal C1q expression and developmental synaptic refinement. Nature neuroscience. 2013;16:1773–1782. doi: 10.1038/nn.3560. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 37.Perry VH, O'Connor V. The role of microglia in synaptic stripping and synaptic degeneration: a revised perspective. ASN neuro. 2010;2:e00047. doi: 10.1042/AN20100024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caleo M, Restani L, Perry VH. Silencing synapses: a route to understanding synapse degeneration in chronic neurodegenerative disease. Prion. 2013;7:147–150. doi: 10.4161/pri.23327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caleo M, Restani L, Vannini E, Siskova Z, Al-Malki H, Morgan R, O'Connor V, Perry VH. The role of activity in synaptic degeneration in a protein misfolding disease, prion disease. PloS one. 2012;7:e41182. doi: 10.1371/journal.pone.0041182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Siskova Z, Page A, O'Connor V, Perry VH. Degenerating synaptic boutons in prion disease: microglia activation without synaptic stripping. The American journal of pathology. 2009;175:1610–1621. doi: 10.2353/ajpath.2009.090372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prinz M, Priller J, Sisodia SS, Ransohoff RM. Heterogeneity of CNS myeloid cells and their roles in neurodegeneration. Nature neuroscience. 2011;14:1227–1235. doi: 10.1038/nn.2923. [DOI] [PubMed] [Google Scholar]
- 42.David S, Kroner A. Repertoire of microglial and macrophage responses after spinal cord injury. Nature reviews Neuroscience. 2011;12:388–399. doi: 10.1038/nrn3053. [DOI] [PubMed] [Google Scholar]
- 43.Geissmann F, Manz MG, Jung S, Sieweke MH, Merad M, Ley K. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327:656–661. doi: 10.1126/science.1178331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yona S, Kim KW, Wolf Y, Mildner A, Varol D, Breker M, Strauss-Ayali D, Viukov S, Guilliams M, Misharin A, Hume DA, Perlman H, Malissen B, Zelzer E, Jung S. Fate mapping reveals origins and dynamics of monocytes and tissue macrophages under homeostasis. Immunity. 2013;38:79–91. doi: 10.1016/j.immuni.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Serbina NV, Pamer EG. Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nature immunology. 2006;7:311–317. doi: 10.1038/ni1309. [DOI] [PubMed] [Google Scholar]
- 46.King IL, Dickendesher TL, Segal BM. Circulating Ly-6C+ myeloid precursors migrate to the CNS and play a pathogenic role during autoimmune demyelinating disease. Blood. 2009;113:3190–3197. doi: 10.1182/blood-2008-07-168575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mildner A, Mack M, Schmidt H, Bruck W, Djukic M, Zabel MD, Hille A, Priller J, Prinz M. CCR2+Ly-6Chi monocytes are crucial for the effector phase of autoimmunity in the central nervous system. Brain : a journal of neurology. 2009;132:2487–2500. doi: 10.1093/brain/awp144. [DOI] [PubMed] [Google Scholar]
- 48.Xue J, Schmidt SV, Sander J, Draffehn A, Krebs W, Quester I, De Nardo D, Gohel TD, Emde M, Schmidleithner L, Ganesan H, Nino-Castro A, Mallmann MR, Labzin L, Theis H, Kraut M, Beyer M, Latz E, Freeman TC, Ulas T, Schultze JL. Transcriptome-based network analysis reveals a spectrum model of human macrophage activation. Immunity. 2014;40:274–288. doi: 10.1016/j.immuni.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arvin KL, Han BH, Du Y, Lin SZ, Paul SM, Holtzman DM. Minocycline markedly protects the neonatal brain against hypoxic-ischemic injury. Annals of neurology. 2002;52:54–61. doi: 10.1002/ana.10242. [DOI] [PubMed] [Google Scholar]
- 50.Wells JE, Hurlbert RJ, Fehlings MG, Yong VW. Neuroprotection by minocycline facilitates significant recovery from spinal cord injury in mice. Brain : a journal of neurology. 2003;126:1628–1637. doi: 10.1093/brain/awg178. [DOI] [PubMed] [Google Scholar]
- 51.Sanchez Mejia RO, Ona VO, Li M, Friedlander RM. Minocycline reduces traumatic brain injury-mediated caspase-1 activation, tissue damage, and neurological dysfunction. Neurosurgery. 2001;48:1393–1399. doi: 10.1097/00006123-200106000-00051. discussion 1399-1401. [DOI] [PubMed] [Google Scholar]
- 52.Popovich PG, Guan Z, Wei P, Huitinga I, van Rooijen N, Stokes BT. Depletion of hematogenous macrophages promotes partial hindlimb recovery and neuroanatomical repair after experimental spinal cord injury. Experimental neurology. 1999;158:351–365. doi: 10.1006/exnr.1999.7118. [DOI] [PubMed] [Google Scholar]
- 53.Shechter R, London A, Varol C, Raposo C, Cusimano M, Yovel G, Rolls A, Mack M, Pluchino S, Martino G, Jung S, Schwartz M. Infiltrating blood-derived macrophages are vital cells playing an anti-inflammatory role in recovery from spinal cord injury in mice. PLoS medicine. 2009;6:e1000113. doi: 10.1371/journal.pmed.1000113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.London A, Itskovich E, Benhar I, Kalchenko V, Mack M, Jung S, Schwartz M. Neuroprotection and progenitor cell renewal in the injured adult murine retina requires healing monocyte-derived macrophages. The Journal of experimental medicine. 2011;208:23–39. doi: 10.1084/jem.20101202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shechter R, Raposo C, London A, Sagi I, Schwartz M. The glial scar-monocyte interplay: a pivotal resolution phase in spinal cord repair. PloS one. 2011;6:e27969. doi: 10.1371/journal.pone.0027969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bartholomaus I, Kawakami N, Odoardi F, Schlager C, Miljkovic D, Ellwart JW, Klinkert WE, Flugel-Koch C, Issekutz TB, Wekerle H, Flugel A. Effector T cell interactions with meningeal vascular structures in nascent autoimmune CNS lesions. Nature. 2009;462:94–98. doi: 10.1038/nature08478. [DOI] [PubMed] [Google Scholar]
- 57.Saederup N, Cardona AE, Croft K, Mizutani M, Cotleur AC, Tsou CL, Ransohoff RM, Charo IF. Selective chemokine receptor usage by central nervous system myeloid cells in CCR2-red fluorescent protein knock-in mice. PloS one. 2010;5:e13693. doi: 10.1371/journal.pone.0013693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.London A, Cohen M, Schwartz M. Microglia and monocyte-derived macrophages: functionally distinct populations that act in concert in CNS plasticity and repair. Frontiers in cellular neuroscience. 2013;7:34. doi: 10.3389/fncel.2013.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Butovsky O, Siddiqui S, Gabriely G, Lanser AJ, Dake B, Murugaiyan G, Doykan CE, Wu PM, Gali RR, Iyer LK, Lawson R, Berry J, Krichevsky AM, Cudkowicz ME, Weiner HL. Modulating inflammatory monocytes with a unique microRNA gene signature ameliorates murine ALS. The Journal of clinical investigation. 2012;122:3063–3087. doi: 10.1172/JCI62636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Donnelly DJ, Longbrake EE, Shawler TM, Kigerl KA, Lai W, Tovar CA, Ransohoff RM, Popovich PG. Deficient CX3CR1 signaling promotes recovery after mouse spinal cord injury by limiting the recruitment and activation of Ly6Clo/iNOS+ macrophages. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2011;31:9910–9922. doi: 10.1523/JNEUROSCI.2114-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Qiu WQ, Walsh DM, Ye Z, Vekrellis K, Zhang J, Podlisny MB, Rosner MR, Safavi A, Hersh LB, Selkoe DJ. Insulin-degrading enzyme regulates extracellular levels of amyloid beta-protein by degradation. The Journal of biological chemistry. 1998;273:32730–32738. doi: 10.1074/jbc.273.49.32730. [DOI] [PubMed] [Google Scholar]
- 62.Koenigsknecht J, Landreth G. Microglial phagocytosis of fibrillar beta-amyloid through a beta1 integrin-dependent mechanism. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2004;24:9838–9846. doi: 10.1523/JNEUROSCI.2557-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yan SD, Chen X, Fu J, Chen M, Zhu H, Roher A, Slattery T, Zhao L, Nagashima M, Morser J, Migheli A, Nawroth P, Stern D, Schmidt AM. RAGE and amyloid-beta peptide neurotoxicity in Alzheimer's disease. Nature. 1996;382:685–691. doi: 10.1038/382685a0. [DOI] [PubMed] [Google Scholar]
- 64.El Khoury JB, Moore KJ, Means TK, Leung J, Terada K, Toft M, Freeman MW, Luster AD. CD36 mediates the innate host response to beta-amyloid. The Journal of experimental medicine. 2003;197:1657–1666. doi: 10.1084/jem.20021546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fuhrmann M, Bittner T, Jung CK, Burgold S, Page RM, Mitteregger G, Haass C, LaFerla FM, Kretzschmar H, Herms J. Microglial Cx3cr1 knockout prevents neuron loss in a mouse model of Alzheimer's disease. Nature neuroscience. 2010;13:411–413. doi: 10.1038/nn.2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee S, Varvel NH, Konerth ME, Xu G, Cardona AE, Ransohoff RM, Lamb BT. CX3CR1 deficiency alters microglial activation and reduces beta-amyloid deposition in two Alzheimer's disease mouse models. The American journal of pathology. 2010;177:2549–2562. doi: 10.2353/ajpath.2010.100265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Butovsky O, Kunis G, Koronyo-Hamaoui M, Schwartz M. Selective ablation of bone marrow-derived dendritic cells increases amyloid plaques in a mouse Alzheimer's disease model. The European journal of neuroscience. 2007;26:413–416. doi: 10.1111/j.1460-9568.2007.05652.x. [DOI] [PubMed] [Google Scholar]
- 68.Town T, Laouar Y, Pittenger C, Mori T, Szekely CA, Tan J, Duman RS, Flavell RA. Blocking TGF-beta-Smad2/3 innate immune signaling mitigates Alzheimer-like pathology. Nature medicine. 2008;14:681–687. doi: 10.1038/nm1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Koronyo-Hamaoui M, Ko MK, Koronyo Y, Azoulay D, Seksenyan A, Kunis G, Pham M, Bakhsheshian J, Rogeri P, Black KL, Farkas DL, Schwartz M. Attenuation of AD-like neuropathology by harnessing peripheral immune cells: local elevation of IL-10 and MMP-9. Journal of neurochemistry. 2009;111:1409–1424. doi: 10.1111/j.1471-4159.2009.06402.x. [DOI] [PubMed] [Google Scholar]
- 70.Hawkes CA, McLaurin J. Selective targeting of perivascular macrophages for clearance of beta-amyloid in cerebral amyloid angiopathy. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:1261–1266. doi: 10.1073/pnas.0805453106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Michaud JP, Bellavance MA, Prefontaine P, Rivest S. Real-time in vivo imaging reveals the ability of monocytes to clear vascular amyloid beta. Cell reports. 2013;5:646–653. doi: 10.1016/j.celrep.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 72.Griciuc A, Serrano-Pozo A, Parrado AR, Lesinski AN, Asselin CN, Mullin K, Hooli B, Choi SH, Hyman BT, Tanzi RE. Alzheimer's disease risk gene CD33 inhibits microglial uptake of amyloid beta. Neuron. 2013;78:631–643. doi: 10.1016/j.neuron.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bradshaw EM, Chibnik LB, Keenan BT, Ottoboni L, Raj T, Tang A, Rosenkrantz LL, Imboywa S, Lee M, Von Korff A, Alzheimer Disease Neuroimaging I, Morris MC, Evans DA, Johnson K, Sperling RA, Schneider JA, Bennett DA, De Jager PL. CD33 Alzheimer's disease locus: altered monocyte function and amyloid biology. Nature neuroscience. 2013;16:848–850. doi: 10.1038/nn.3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rohn TT. The triggering receptor expressed on myeloid cells 2: “TREM-ming” the inflammatory component associated with Alzheimer's disease. Oxidative medicine and cellular longevity. 2013;2013:860959. doi: 10.1155/2013/860959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Takahashi K, Rochford CD, Neumann H. Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2. The Journal of experimental medicine. 2005;201:647–657. doi: 10.1084/jem.20041611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang S, Wang XJ, Tian LP, Pan J, Lu GQ, Zhang YJ, Ding JQ, Chen SD. CD200-CD200R dysfunction exacerbates microglial activation and dopaminergic neurodegeneration in a rat model of Parkinson's disease. Journal of neuroinflammation. 2011;8:154. doi: 10.1186/1742-2094-8-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Virgone-Carlotta A, Uhlrich J, Akram MN, Ressnikoff D, Chretien F, Domenget C, Gherardi R, Despars G, Jurdic P, Honnorat J, Nataf S, Touret M. Mapping and kinetics of microglia/neuron cell-to-cell contacts in the 6-OHDA murine model of Parkinson's disease. Glia. 2013;61:1645–1658. doi: 10.1002/glia.22546. [DOI] [PubMed] [Google Scholar]
- 78.Clement AM, Nguyen MD, Roberts EA, Garcia ML, Boillee S, Rule M, McMahon AP, Doucette W, Siwek D, Ferrante RJ, Brown RH, Jr, Julien JP, Goldstein LS, Cleveland DW. Wild-type nonneuronal cells extend survival of SOD1 mutant motor neurons in ALS mice. Science. 2003;302:113–117. doi: 10.1126/science.1086071. [DOI] [PubMed] [Google Scholar]
- 79.Boillee S, Yamanaka K, Lobsiger CS, Copeland NG, Jenkins NA, Kassiotis G, Kollias G, Cleveland DW. Onset and progression in inherited ALS determined by motor neurons and microglia. Science. 2006;312:1389–1392. doi: 10.1126/science.1123511. [DOI] [PubMed] [Google Scholar]
- 80.Beers DR, Henkel JS, Xiao Q, Zhao W, Wang J, Yen AA, Siklos L, McKercher SR, Appel SH. Wild-type microglia extend survival in PU.1 knockout mice with familial amyotrophic lateral sclerosis. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:16021–16026. doi: 10.1073/pnas.0607423103. [DOI] [PMC free article] [PubMed] [Google Scholar]