Abstract
Background
Despite evidence that daily weighing is an effective strategy for weight control, concerns remain regarding the potential for negative psychological consequences.
Purpose
The goal of the study was to examine the impact of a daily self-weighing weight loss intervention on relevant psychological constructs.
Design
A 6-month RCT.
Setting/participants
The study sample (N=91) included overweight men and women in the Chapel Hill NC area.
Intervention
Between February and August 2011, participants were randomly assigned to a daily self-weighing intervention or delayed intervention control group. The 6-month intervention included daily weighing for self-regulation of diet and exercise behaviors using an e-scale that transmitted weights to a study website. Weekly e-mailed lessons and tailored feedback on daily self-weighing adherence and weight loss progress were provided.
Main outcome measures
Self-weighing frequency was measured throughout the study using e-scales. Weight was measured in-clinic at baseline, 3 months, and 6 months. Psychological outcomes were assessed via self-report at the same time points.
Results
In 2012, using linear mixed models, there were no significant differences between groups in depressive symptoms, anorectic cognitions, disinhibition, susceptibility to hunger, and binge eating. At 6 months, there was a significant group × time interaction for body dissatisfaction (p=0.007) and dietary restraint (p<0.001) with the intervention group reporting lower body dissatisfaction and greater dietary restraint compared to controls.
Conclusions
Results indicate that a weight loss intervention that focuses on daily self-weighing does not cause adverse psychological outcomes. This suggests that daily weighing is an effective and safe weight-control strategy among overweight adults attempting to lose weight.
Introduction
The high prevalence of obesity1 indicates the need for effective and sustainable weight-control strategies. One such strategy that is associated with weight loss success is daily self-weighing.2–5 Adoption of this behavior remains limited, however, because of concerns regarding adverse psychological consequences.6–8 A recent review showed that frequent self-weighing is not associated with negative mood or body dissatisfaction among treatment-seeking overweight and obese adults.9 Most studies, however, were conducted post hoc,4,10 and of the limited experimental evidence, most tested high-intensity, multicomponent interventions,11,12 which might mitigate any negative effects of daily weighing.
The purpose of this analysis was to examine the impact of a 6-month, lower-intensity daily self-weighing weight loss intervention on relevant psychological outcomes. As reported elsewhere,13 the intervention was found to be feasible and effective for producing clinically meaningful weight loss. The current analysis provides a multidimensional view of the psychological effects of daily weighing under lower-intensity conditions. It was hypothesized that the intervention would not adversely affect psychological outcomes as compared to a delayed-intervention control group.
Methods
Participants
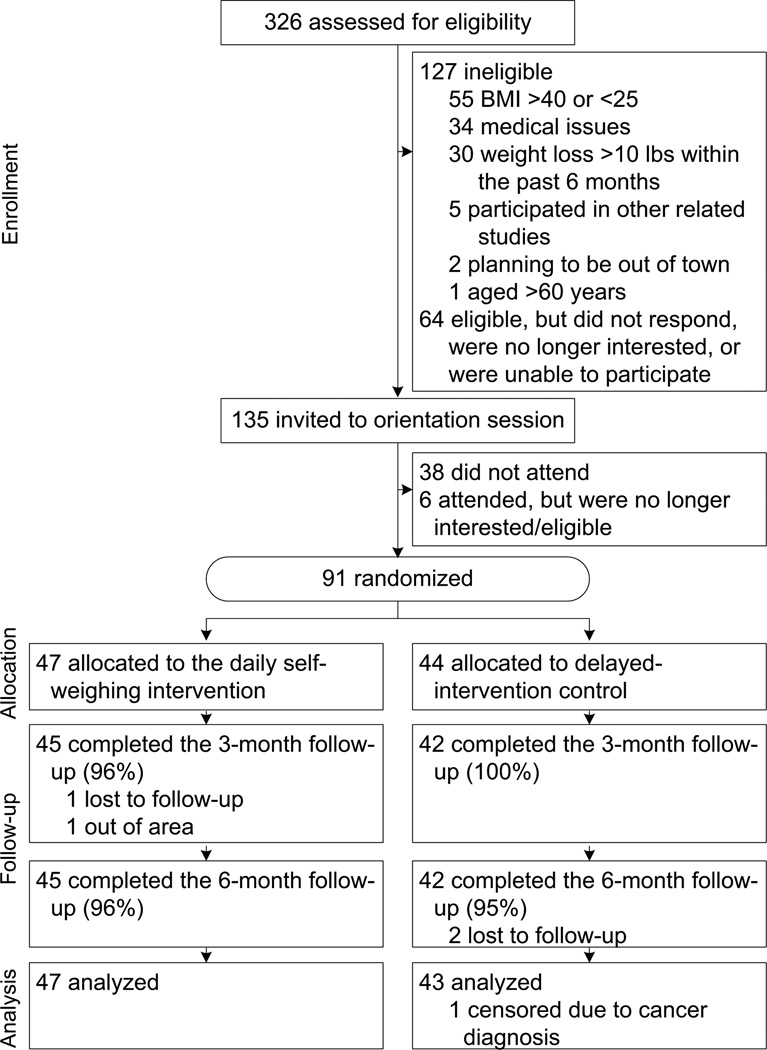
Eligibility criteria included adults aged 18–60 years, BMI of 25–40, Internet access, and no medical conditions that might affect participation, including recent hospitalization for depression, or diagnosis of bipolar disease, schizophrenia, or eating disorder. Following eligibility screening, informed consent was obtained and baseline measures were taken. Participants (N=91) were randomized to a daily self-weighing intervention (n=47) or a delayed intervention control group (n=44). All participants were reassessed at 3 and 6 months (Figure 1). Data collection occurred from February to August 2011 in Chapel Hill NC. The University of North Carolina at Chapel Hill IRB approved and monitored the study.
Figure 1.
Participant enrollment and retention flow
Intervention Description
A description of the intervention has been previously published.13 Briefly, participants were instructed to self-regulate behaviors by weighing daily using an e-scale. The e-scale used the wireless cellular network to transmit weight data to a website that displayed individualized weight graphs, and provided objective data for each participant in a separate researcher interface. These data were used to provide tailored feedback self-weighing frequency and weight loss via weekly e-mails that also included behavioral weight-control lessons. The control group received no intervention during the study period and was blinded to the focus on daily weighing.
Measures
Height was collected using a wall-mounted stadiometer, and weight was measured using a digital scale in-clinic. Self-weighing frequency was measured objectively using the e-scales. Several self-report measures on cognitive and behavioral constructs were assessed. These constructs have been examined in previous self-weighing analyses.4,8,12
Body satisfaction
The 16-item Body Shape Questionnaire measured attitudes surrounding body shape concern and body dissatisfaction.14 Participants were asked a variety of questions regarding feelings about their appearance over the past 4 weeks, with six response options ranging from never to always (e.g., Have you been so worried about your shape that you have been feeling you ought to diet?). Total scores were calculated and participants missing >1 item were excluded (3 months, n=9; 6 months, n=3).
Depressive symptoms
Depressive symptoms were measured using the 20-item Center for Epidemiologic Studies Depression scale.15,16 Participants were asked how often they felt a certain way over the past week with four response options ranging from rarely to all the time (e.g., I was bothered by things that usually don’t bother me). Total scores ≥16 are indicative of depression.17 Participants missing ≥1 item were excluded from the analysis (3 months, n=2; 6 months, n=4).
Disordered eating cognitions and behaviors
A 12-item version of the Mizes Anorectic Cognitions Questionnaire assessed dysfunctional cognitions regarding fear of weight gain, self-control as the basis of self-esteem, and weight as the basis of approval.18 These cognitions are associated with disordered eating among nonclinical populations.19 Participants were asked to rate their beliefs and attitudes via five responses options ranging from strongly agree to strongly disagree (e.g., If my weight goes up, my self-esteem goes down). Total scores were calculated, and participants missing >1 item were excluded (3 months, n=9; 6 months, n=3).
The Questionnaire for Eating and Weight Patterns Revised assessed binge eating.20,21 Differences were examined between groups in the likelihood of reporting any binge eating (e.g., During the past month, did you often eat within any two-hour period what most people would regard as an unusually large amount of food?). Participants missing a response to this question were excluded from the analysis (3 months, n=9; 6 months, n=3).
Dietary restraint, disinhibition, and hunger
The 51-item Three-Factor Eating Questionnaire was used to measure cognitive dietary restraint (restraint from eating in order to lose weight); disinhibition (perceptions regarding loss of control with eating); and susceptibility to hunger.22 Participants reported agreement with a variety of statements (e.g., When I smell a sizzling steak or see a juicy piece of meat, I find it difficult to keep from eating, even if I have just finished a meal). Total scores were calculated for each of the constructs and participants missing >1 item were excluded from analysis (3 months, n=9; 6 months, n=3).
Data Analysis
Chi-square and ANOVA tests were conducted to examine differences in baseline characteristics and attrition across groups. Any differences were controlled for by inclusion in the models. Intent-to-treat analyses using linear mixed models with random intercept and maximum-likelihood estimates were conducted to examine the effect of treatment group on continuous outcomes. Generalized estimating equation (GEE) models examined differences in dichotomous outcomes. Separate models for each of the outcomes examined the effects of group, time, and group × time interaction at both 3 and 6 months. All participants were included in the analyses with the assumption that missing values were missing at random. Analyses were conducted in 2012 using SPSS for Mac (Version 19) with an alpha of <0.05 to assess significance.
Results
Table 1 shows baseline characteristics across study groups. Participants were on average aged 44±11 years; obese (BMI: 32.15± 3.8); predominantly female (75%); white (74%); and college-educated (78%) with no history of depression/anxiety (88%) or tobacco use (90%). Groups differed only on baseline BMI, with the intervention group having higher average BMI. Ninety-eight percent of participants completed the data collection visits that included in-clinic weights and completion of one paper questionnaire (CESD [Center for Epidemiologic Studies, Depression]). Web-based questionnaires were completed by 90% of participants at 3 months and 97% at 6 months with no significant differences between groups (3 months, p=0.49; 6 months, p=0.24).
Table 1.
Baseline demographic data for control and intervention group participants (N=91)
| Control (n=44) |
Intervention (n=47) |
p-value | |
|---|---|---|---|
| Age, years | 44.7 ± 10.6 | 43.0 ± 11.4 | 0.45 |
| Gender | 0.31 | ||
| Male | 9 (21) | 14 (30) | |
| Female | 35 (80) | 33 (70) | |
| Race/ethnicity | 0.76 | ||
| Black | 8 (18) | 6 (13) | |
| White | 31 (71) | 36 (77) | |
| Other | 5 (11) | 5 (10) | |
| College Degree | 35 (80) | 36 (77) | 0.73 |
| BMI | 31.05 ± 3.13 | 33.18 ± 4.03 | 0.006 |
| Self-weighing Frequency | 0.12 | ||
| Daily | 11 (25) | 5 (10.6) | |
| Several Times/Week | 12 (27) | 9 (20) | |
| One time/week | 3 (7) | 8 (17) | |
| Less than one time/week | 18 (41) | 24 (52) | |
| History of Depression or Anxiety | 4 (9) | 7 (15) | 0.53 |
| Any Tobacco Use | 7 (16) | 2 (4) | 0.08 |
Note: Data are M±SD or n (%) unless otherwise indicated.
Main results have been published elsewhere.13 Briefly, compliance to daily self-weighing was high among intervention participants: 51% weighed every day and 94% weighed ≥5 days/week. Intervention participants weighed on average more days/week compared to controls (6.1 ±1.1 vs 1.1±1.5; p<0.01). At 6 months, the intervention group lost significantly more weight (M [95% CI]= −13.6 lbs. [−18.5, −8.8] vs −0.68 lbs. [−2.4, 1.0]; p<0.001) compared to controls.
Table 2 presents changes in psychological outcomes within group and across groups over time. There were no significant differences between groups for depressive symptoms, anorectic cognitions, disinhibition, susceptibility to hunger or binge eating. For body dissatisfaction, there was a significant group by time interaction at 6 months (p=0.007) with the intervention group reporting lower average scores. Similarly, at both 3 and 6 months, the intervention group reported significantly greater dietary restraint compared to controls (p<0.001). Also observed were significant decreases in disinhibition (p<0.001); susceptibility to hunger (p=0.045); and binge eating (p=0.022) among intervention participants at 6 months compared to baseline. There were no significant changes within the control group.
Table 2.
Psychological outcomes by group and across time
| p-valueb | ||||||||
|---|---|---|---|---|---|---|---|---|
| Assessment Perioda | Time | Group | Group × Time Interaction |
|||||
| Outcome Variable and Group |
Baseline (n=91) |
3 months (n=82) |
6 months (n=88) |
3 months vs baseline |
6 months vs baseline |
Baseline to 3 months |
Baseline to 6 months |
|
| Depressive Symptomsc | ||||||||
| Intervention | 7.9 (1.3) | 8.0 (1.3) | 8.5 (1.3) | 0.856 | 0.815 | 0.359 | 0.859 | 0.228 |
| Control | 8.6 (1.3) | 9.1 (1.3) | 10.2 (1.3) | 0.669 | 0.187 | |||
| Difference between groups | −0.40 (−3.4, 2.6) | −1.0 (−4.0, 2.0) | ||||||
| Anorectic Cognitions | ||||||||
| Intervention | 32.9 (1.0) | 32.5 (1.0) | 31.7 (1.0) | 0.553 | 0.090 | 0.794 | 0.293 | 0.406 |
| Control | 31.9 (1.0) | 32.6 (1.1) | 31.5 (1.0) | 0.390 | 0.586 | |||
| Difference between groups | −1.1 (−3.2, 1.0) | −0.84 (−2.9, 1.2) | ||||||
| Body Dissatisfaction | ||||||||
| Intervention | 109.7 (4.7) | 100.5 (4.8) | 98.9 (4.8) | 0.013 | 0.003 | 0.490 | 0.052 | 0.007 |
| Control | 106.2 (4.9) | 107.1 (4.9) | 109.1 (4.9) | 0.813 | 0.427 | |||
| Difference between groups | −10.1 (−20.3, 0.14) | −13.7 (−23.7, −3.7) | ||||||
| Dietary Restraint | ||||||||
| Intervention | 9.3 (0.59) | 12.9 (0.60) | 13.4 (0.60) | <0.001 | <0.001 | 0.004 | <0.001 | <0.001 |
| Control | 9.3 (0.60) | 9.9 (0.62) | 9.6 (0.61) | 0.133 | 0.415 | |||
| Difference between groups | 2.9 (1.7, 4.2) | 3.7 (2.5, 5.0) | ||||||
| Disinhibition | ||||||||
| Intervention | 8.3 (0.44) | 7.5 (0.45) | 7.0 (0.45) | 0.036 | <0.001 | 0.966 | .225 | 0.119 |
| Control | 7.8 (0.45) | 7.7 (0.46) | 7.3 (0.46) | 0.702 | 0.168 | |||
| Difference between groups | −0.61 (−1.6, 0.38) | −0.77 (−1.7, 0.20) | ||||||
| Susceptibility to Hunger | ||||||||
| Intervention | 5.7 (0.43) | 5.2 (0.45) | 4.9 (0.44) | 0.176 | 0.045 | 0.011 | 0.065 | 0.192 |
| Control | 6.5 (0.44) | 7.0 (0.45) | 6.4 (0.45) | 0.206 | 0.885 | |||
| Difference between groups | −1.0 (−2.1, 0.06) | −0.70 (−1.8, 0.36) | ||||||
| Binge Eating, n (%) | ||||||||
| Intervention | 14 (30) | 11 (27) | 6 (14) | 0.653 | 0.022 | 0.879 | 0.099 | 0.079 |
| Control | 8 (18) | 13 (32) | 9 (21) | 0.075 | 0.139 | |||
| OR (95% CI) | 2.5 (0.8, 8.6) | 3.9 (0.9, 10.0) | ||||||
All values are M (SE) unless otherwise specified; values for difference between groups are M (95% CI).
Significant p-values are shown in bold.
Depressive Symptoms: p-values derived from the transformed variable with raw Ms and SEs are presented.
All models controlled for baseline BMI.
Sensitivity analyses were conducted within the intervention group to examine psychological outcomes by weight loss. Meaningful weight loss was defined as losing ≥3% of initial body weight.23 Intervention participants who lost weight (n=27) at 6 months had significantly lower body dissatisfaction (p=0.019) and depressive symptoms (p=0.01), and higher levels of dietary restraint (p=0.003) compared to baseline. Intervention participants who did not lose weight (n=20) reported improvements in dietary restraint (p=0.036), but no significant changes in body satisfaction or depressive symptoms between baseline and 6 months, suggesting that daily weighing did not lead to adverse outcomes in the absence of weight loss.
Discussion
These results indicate that a weight loss intervention that focused on daily self-weighing did not cause adverse psychological outcomes among overweight and obese adults. There were no significant differences between intervention and control groups in depressive symptoms, anorectic cognitions, disinhibition, perceived susceptibility to hunger, or binge eating. Intervention participants demonstrated greater improvements in body satisfaction and eating behavior cognitions relative to controls.
These findings are consistent with previous research examining daily self-weighing and psychological outcomes in adults. Previous analyses have shown that depression and body satisfaction do not vary by self-weighing frequency.4,10 Among participants enrolled in self-regulation interventions for weight control that included daily self-weighing, there was no increased risk for development of eating disorders, negative body image, mood disorders,11 or binge eating.12
There are important strengths of the current study that build on the current evidence base regarding adverse psychological outcomes associated with self-weighing. The intervention instructed participants to weigh daily at the outset, which is in contrast to previous post hoc analyses that examined effects among those who chose to weigh daily.4,10 Given that almost all of the intervention participants weighed ≥5 days/week, this study provided a good opportunity to examine whether more-frequent self-weighing leads to adverse outcomes, even in the absence of weight loss. To better understand the effects of daily weighing, the current study focused on testing a lower-intensity approach that included daily self-weighing as the primary self-monitoring tool for self-regulation without any intensive face-to-face or individualized support.
Refuting previous claims that self-weighing leads to poorer body image,6 the current study found improvements in body satisfaction. Consistent with previous studies,24 the authors suspect that body satisfaction improved as a result of weight loss. Two additional findings support this notion. First, intervention participants who did not lose weight had no change in body satisfaction, indicating that daily weighing in the absence of weight loss is not harmful. Second, there were no significant changes in body satisfaction over time among control participants. Regarding dietary cognitions, restraint increased as a result of the intervention, with a trend toward decreases in disinhibition and susceptibility to hunger. These outcomes are associated with weight loss success25 and expected given that most interventions are designed to produce such changes.26
Limitations
This study has several limitations. Because the study design did not isolate daily self-weighing, it is not possible determine whether the effects seen are related to daily self-weighing or the other intervention components. The sample size was relatively small and consisted predominantly of highly educated white women without depression or anxiety or a history of eating disorders. Therefore, the findings may not generalize beyond these population characteristics. Examining the effect of daily weighing among those predisposed to eating disorders is an important analysis that could not be made in the current study.
Conclusion
This study found that a lower-intensity self-regulation program that focuses on daily weighing is effective for weight loss among overweight and obese adults and does not lead to increases in depressive symptoms or disordered eating behaviors and cognitions. Daily self-weighing should be implemented into weight-control programs without concerns for negative psychological consequences.
Acknowledgements
The authors thank the Lineberger Comprehensive Cancer Center, Cancer Control Education Program Fellowship (#R25 CA057726) and the University of North Carolina at Chapel Hill, Gillings School of Public Health Dissertation Award for providing funding for this study. The authors also acknowledge the staff at the UNC Weight Research Program for their valuable support and all study participants for their contribution to this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among U.S. adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 2.Vanwormer JJ, French SA, Pereira MA, Welsh EM. The impact of regular self-weighing on weight management: a systematic literature review. Int J Behav Nutr Phys Act. 2008;5:54. doi: 10.1186/1479-5868-5-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Annals of Behavioral Medicine. 2005;30(3):210–216. doi: 10.1207/s15324796abm3003_5. [DOI] [PubMed] [Google Scholar]
- 4.Welsh EM, Sherwood NE, VanWormer JJ, Hotop AM, Jeffery RW. Is frequent self-weighing associated with poorer body satisfaction? Findings from a phone-based weight loss trial. J Nutr Educ Behav. 2009 Nov-Dec;41(6):425–428. doi: 10.1016/j.jneb.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.VanWormer JJ, Martinez AM, Martinson BC, et al. Self-weighing promotes weight loss for obese adults. Am J Prev Med. 2009;36(1):70–73. doi: 10.1016/j.amepre.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 6.Dionne MM, Yeudall F. Monitoring of weight in weight loss programs: a double-edged sword? J Nutrition Education Behavior. 2005;37(6):315–318. doi: 10.1016/s1499-4046(06)60162-0. [DOI] [PubMed] [Google Scholar]
- 7.Ogden J, Whyman C. The effect of repeated weighing on psychological state. European Eating Disorders Review. 1997;5(2):121–130. [Google Scholar]
- 8.Klos LA, Esser VE, Kessler MM. To weigh or not to weigh: the relationship between self-weighing behavior and body image among adults. Body Image. 2012;9(4):551–554. doi: 10.1016/j.bodyim.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 9.O'Neil PM, Brown JD. Weighing the evidence: benefits of regular weight monitoring for weight control. J Nutrition Education and Behavior. 2005;37(6):319–322. doi: 10.1016/s1499-4046(06)60163-2. [DOI] [PubMed] [Google Scholar]
- 10.Linde JA, Jeffery RW, Finch EA, et al. Relation of body mass index to depression and weighing frequency in overweight women. Prev Med. 2007;45(1):75–79. doi: 10.1016/j.ypmed.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gokee-Larose J, Gorin AA, Wing RR. Behavioral self-regulation for weight loss in young adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2009;6:10. doi: 10.1186/1479-5868-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL, Machan J. STOP regain: are there negative effects of daily weighing? J Consult Clin Psychol. 2007 Aug;75(4):652–656. doi: 10.1037/0022-006X.75.4.652. [DOI] [PubMed] [Google Scholar]
- 13.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. The efficacy of a daily self-weighing weight loss intervention using smart scales and email. Obesity. 2013 Mar 20; doi: 10.1002/oby.20396. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Evans C, Dolan B. Body Shape Questionnaire: derivation of shortened" alternate forms". Int J Eating Disorders. 1993;13:315–321. doi: 10.1002/1098-108x(199304)13:3<315::aid-eat2260130310>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 15.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385. [Google Scholar]
- 16.Ensel W. Measuring depression: The CES-D Scale. In: Lin N, Dean A, Ensel W, editors. Social Support, Life Events and Depression. New York: Academic Press; 1986. pp. 51–70. [Google Scholar]
- 17.Zich JM, Attkisson CC, Greenfield TK. Screening for depression in primary care clinics: the CES-D and the BDI. The International Journal of Psychiatry in Medicine. 1990;20(3):259–277. doi: 10.2190/LYKR-7VHP-YJEM-MKM2. [DOI] [PubMed] [Google Scholar]
- 18.Mizes JS, Christiano B, Madison J, Post G, Seime R, Varnado P. Development of the Mizes Anorectic Cognitions Questionnaire-Revised: Psychometric properties and factor structure in a large sample of eating disorder patients. International Journal of Eating Disorders. 2000;28(4):415–421. doi: 10.1002/1098-108x(200012)28:4<415::aid-eat9>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 19.Osman A, Chiros CE, Gutierrez PM, Kopper BA, Barrios FX. Factor structure and psychometric properties of the brief Mizes Anorectic Cognitions questionnaire. J Clin Psych. 2001;57(6):785–799. doi: 10.1002/jclp.1049. [DOI] [PubMed] [Google Scholar]
- 20.Spitzer RL, Devlin M, Walsh BT, et al. Binge eating disorder: A multisite field trial of the diagnostic criteria. Int J Eating Disorders. 1992;11(3):191–203. [Google Scholar]
- 21.Nangle DW, Johnson WG, Carr-Nangle RE, Engler LB. Binge eating disorder and the proposed DSM-IV criteria: psychometric analysis of the Questionnaire of Eating and Weight Patterns. Int J Eating Disorders. 1994;16(2):147–157. doi: 10.1002/1098-108x(199409)16:2<147::aid-eat2260160206>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 22.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J psychosomatic research. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 23.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J obesity (2005) 2006;30(3):391–399. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 24.Foster GD, Wadden TA, Vogt RA. Body image in obese women before, during, and after weight loss treatment. Health Psychology. 1997;16(3):226. doi: 10.1037//0278-6133.16.3.226. [DOI] [PubMed] [Google Scholar]
- 25.Foster G, Wadden T, Swain R, Stunkard A, Platte P, Vogt R. The Eating Inventory in obese women: clinical correlates and relationship to weight loss. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 1998;22(8):778. doi: 10.1038/sj.ijo.0800659. [DOI] [PubMed] [Google Scholar]
- 26.Clark MM, Marcus BH, Pera V, Niaura RS. Changes in eating inventory scores following obesity treatment. International Journal of Eating Disorders. 1994;15(4):401–405. doi: 10.1002/eat.2260150411. [DOI] [PubMed] [Google Scholar]