Abstract
A 61-year-old man was diagnosed with aortic stenoinsufficiency with periannular abscess, which involved the aortic root of noncoronary sinus (NCS) that invaded down to the central fibrous body, whole membranous septum, mitral valve (MV), and tricuspid valve (TV). The open complete debridement was executed from the aortic annulus at NCS down to the central fibrous body and annulus of the MV and the TV, followed by the left ventricular outflow tract reconstruction with implantation of a mechanical aortic valve by using a leaflet of the half-folded elliptical bovine pericardial patch. Another leaflet of this patch was used for the repair of the right atrial wall with a defect and the TV.
Keywords: 1. Endocarditis, 2. Aortic root, 3. Aortic valve, 4. Central fibrous body
CASE REPORT
A 61-year-old man complaining of syncope and chest pain came to our hospital. Ten days prior to hospitalization, he had had a fever, chills, and body ache. He had taken some medication from a local clinic for these symptoms, which were supposedly caused by a simple upper respiratory infection. Despite the medication, the patient had developed another symptom of syncope 7 days earlier and was transferred to the Neurology Department for evaluation. On arrival, he had mild fever (37.5°C) with chills, sweating, and dyspnea. The blood pressure was 110/40 mmHg, pulse rate 90/min, and respiratory rate 20/min. On the chest auscultation, a diastolic murmur was heard at the left upper sternal border. The laboratory tests showed leukocytosis (16,900 leukocytes/μL). The chest X-ray revealed cardiomegaly, and the electrocardiogram demonstrated a complete AV block. In the brain magnetic resonance imaging, there were multiple infarcts, which were thought to be caused by septic emboli. Echocardiography showed moderate aortic regurgitation with a retracted bicuspid aortic valve and periannular abscess. Therefore, we decided to perform an emergency operation. After the median sternotomy, ascending aortic and bicaval venous cannulation were done. Cardiopulmonary bypass was initiated, and the ascending aorta was then cross-clamped. After infusing the histidine-tryptophan-ketoglutarate solution through the retrograde cardioplegic catheter and local cooling with ice slush, transverse aortotomy was performed. The aortic valve was thickened and retracted; this was consistent with a rheumatic aortic stenosis. There was a commissural fusion between the noncoronary cusp and the right coronary cusp, which also had fibrous thickening with calcification and abscess (Fig. 1). The periannular abscess involved the aortic root of the base of noncoronary sinus (Fig. 2) and invaded down to the central fibrous body, whole membranous septum, and mitral and tricuspid valves (TVs) (Fig. 2). The aortic valve was excised carefully, and then, the infected tissue and the pus were removed meticulously from the abscess pocket down to the membranous septum, central fibrous body, annulus of the mitral valve (MV), and anteroseptal commissure of the TV. We also made an extended transseptal incision extending from the right atrial auricle to the TV to expose the lesion and achieve complete debridement. The septal and anterior leaflets of the TV were also partially resected due to vegetations. After the complete debridement of the infected area, we found a large defect including the left ventricular outflow tract (LVOT), which contained the membranous septum, central fibrous body extending to the TV, and mitral annulus. The MV itself was intact and had no vegetation. The reconstruction of the LVOT was performed with half-folded elliptical bovine pericardium (Peri-Guard; Synovis Surgical Innovation, St. Paul, MN, USA) (Fig. 3). The bovine pericardium was trimmed into an elliptical shape and a half-fold was made; then, its base was secured by interrupted suturing to the annulus of the MV by using reinforcement with a Teflon felt, followed by LVOT reconstruction using a leaflet of the half-folded elliptical bovine patch with aortic valve implantation concomitantly using a 21-mm mechanical valve (SJM Masters Series Valve; St. Jude Medical Inc., St. Paul, MN, USA) (Fig. 3). After closing the aortotomy site, tricuspid annuloplasty was done: partial excision and re-suspension of the septal and the anterior leaflet and anteroseptal commissuroplasty. The other half of the half-folded elliptical bovine patch was used for repairing the right atrial wall with a defect and TV. After weaning the patient from cardiopulmonary bypass, we conducted transesophageal echocardiography, which revealed neither an intracardiac shunt nor TV and MV regurgitation. Because the complete AV block was observed, we began temporary pacing at the rate of 80 beats/min after placing permanent pacing leads on the right atrial and ventricular walls. The total cardiopulmonary bypass and aortic cross clamping times were 303 minutes and 238 minutes, respectively. On postoperative day 1, we were able to wean the patient from mechanical ventilation and extubate an endotracheal tube. On postoperative day 6, we inserted the pacemaker generator. Microbiologic examination of the excised tissues showed no organisms on the Gram stain. Cultures of the aortic root abscess contents and vegetation were all negative. Intravenous antibiotics with ampicillin, nafcillin, and gentamicin were continued for approximately 6 more weeks. The echocardiography on postoperative day 51 revealed normal LV contractility, no intracardiac shunt, and a well-functioning prosthetic mechanical aortic valve without para-valvular leakage and tricuspid regurgitation. On postoperative day 56, the patient was discharged with oral anticoagulation.
Fig. 1.
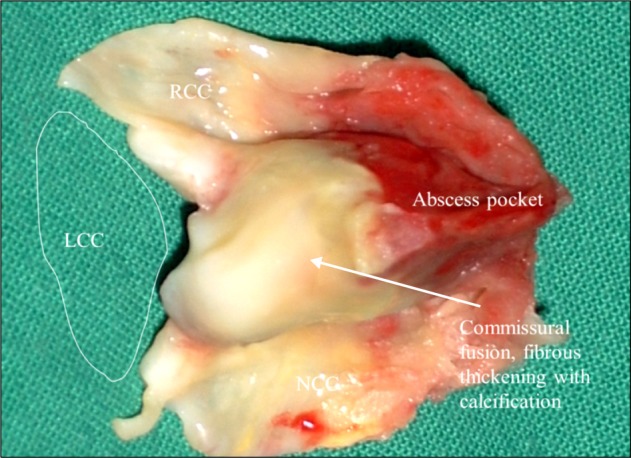
The aortic valve was thickened and retracted. There was a commissural fusion as well as an abscess pocket between NCC and RCC, and fibrous thickening with calcification. RCC, right coronary cusp; LCC, left coronary cusp; NCC, noncoronary cusp.
Fig. 2.
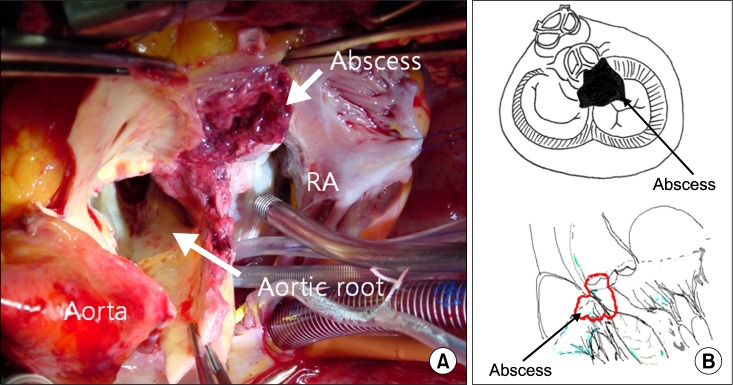
(A) Photograph of the abscess pocket. (B) Diagram of the abscess pocket. RA, right atrial.
Fig. 3.
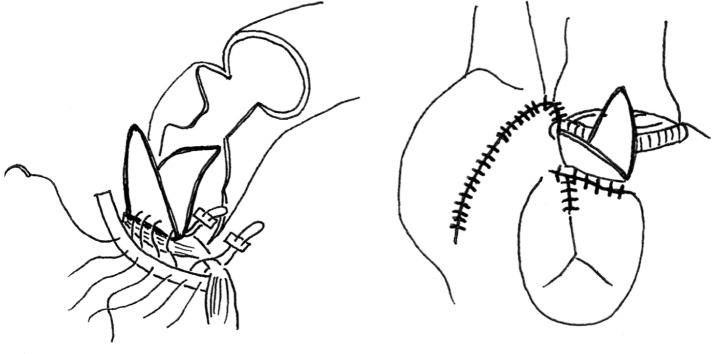
Schematic representation of the operation: left ventricular outflow tract reconstruction and repair of the right atrial wall of the tricuspid valve with a half-folded elliptical bovine patch.
DISCUSSION
Infective endocarditis with abscess formation is a rare, life-threatening condition, and it exhibits a high postoperative mortality. This medical condition is fatal because of the complicated anatomical features of the fibrous skeleton. This is also particularly true when the fibrous skeleton of the heart is extensively destroyed and the reconstructive procedures are complicated [1]. The fibrous skeleton of the heart is a complex framework that surrounds the orifices of the valves, the right and left fibrous trigone, and the membranous parts of the interatrial and interventricular septa [2]. Our case displayed fibrous skeleton destruction, which extended even to the MV and TV. After the meticulous debridement and resection of all infected and necrotic tissues, an appropriate reconstruction of defects ensured better surgical results. Unfortunately, current literature regarding the surgical management of fibrous skeleton destruction is limited. In the presence of endocarditis, annular destruction with a loss of ventricular or mitral aortic continuity demands extreme ingenuity for surgical treatment. David et al. [3] described a surgical method that involves replacing aortic and MVs after the reconstruction of the intervalvular fibrous body by using two triangular patches of glutaraldehyde-fixed bovine pericardium. They insisted that the glutaraldehyde-treated bovine pericardium is an excellent material for use in reconstructing the heart in patients with paravalvular abscess [3]. Kameyama et al. [4] presented a case of a combination of annuloaortic ectasia and infectious endocarditis that required reconstruction of the aortic root and aorto-mitral common annulus, and mitral valve replacement. Black et al. [5] reported that Konno aorto-ventriculoplasty, originally described for the enlargement of the aortic annulus and the LVOT, may be well suited for the debridement and repair of fibrous skeleton endocarditis. We present a case of the destructed fibrous skeleton—including LVOT, right fibrous trigone, membranous septum, and tricuspid and mitral annulus—which we successfully reconstructed with a bovine pericardial patch that had a half-folded elliptical shape. One leaflet of this patch was applied for LVOT reconstruction from the MV with aortic valve implantation, and the other for the right atrial wall with a defect and TV.
In conclusion, in the reconstruction of the LVOT with a defect, right fibrous trigone, and TV in the infective endocarditis, one half-folded elliptical pericardial patch could be a useful option to repair both the LVOT and the right-side area with a defect.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Anguera I, Miro JM, Cabell CH, et al. Clinical characteristics and outcome of aortic endocarditis with periannular abscess in the International Collaboration on Endocarditis Merged Database. Am J Cardiol. 2005;96:976–81. doi: 10.1016/j.amjcard.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 2.Moore KL, Dalley AF, Agur AM. Heart. In: Moore KL, Dalley AF, Agur AM, editors. Clinically oriented anatomy. 6th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2010. pp. 135–59. [Google Scholar]
- 3.David TE, Kuo J, Armstrong S. Aortic and mitral valve replacement with reconstruction of the intervalvular fibrous body. J Thorac Cardiovasc Surg. 1997;114:766–71. doi: 10.1016/S0022-5223(97)70080-1. [DOI] [PubMed] [Google Scholar]
- 4.Kameyama T, Ando F, Okamoto F, Hanada M, Sasahashi N. A brimmed valved conduitin repair of fibrous skeleton abscess. Ann Thorac Surg. 1998;66:2108–10. doi: 10.1016/s0003-4975(98)00765-6. [DOI] [PubMed] [Google Scholar]
- 5.Black MD, Walley VM, Keon WJ. Fibrous skeleton endocarditis: repair using Konno procedure. Ann Thorac Surg. 1994;57:225–8. doi: 10.1016/0003-4975(94)90408-1. [DOI] [PubMed] [Google Scholar]


