SUMMARY
Intraoperative nerve monitoring (IONM) aimed at reducing the injuries of recurrent laryngeal nerve during thyroidectomy is controversial. We conducted a meta-analysis to assess the incidence of nerve injuries with or without IONM. Studies published from January 1994 to February 2012 in English language on humans were identified. Heterogeneity of studies was checked by the Higgins test. Summary estimates of predictive values of injury were made using the Mantel-Haenszel test based on the fixed-effects model. Publication bias was assessed by a funnel plot and Egger's method. Eight articles were selected accounting a total of 5257 nerves at risk. IONM revealed a significant impact in preventing transient injuries (positive predictive value = 5% [95% CI: 2-8], negative = 96% [95% CI: 91-100], relative risk = 0.73 [95% CI: 0.54-0.98], p = 0.035), whereas they failed to demonstrate effect on permanent injuries (positive predictive value = 2% [95% CI: 0.6-3.8], negative 99% [95% CI: 97-100], relative risk = 0.73 [95% CI: 0.44-1.23], p = 0.235). This meta-analysis demonstrated the merit of IONM in preventing transient injury during thyroidectomy. No advantage was found in permanent injuries.
KEY WORDS: Intraoperative neurostimulation, Recurrent laryngeal nerve, Thyroid surgery, Meta-analysis
RIASSUNTO
L'utilità del monitoraggio intraoperatorio dei nervi periferici (IONM), allo scopo di ridurre il danno dei nervi ricorrenti nel corso della chirurgia tiroidea, rappresenta ancora un aspetto controverso. Abbiamo, quindi, compiuto una metaanalisi, allo scopo di definire l'incidenza di danno nervoso con e senza IONM. Sono stati dapprima identificati gli studi eseguiti dal gennaio 1994 fino al febbraio 2012 in lingua inglese. L'eterogeneità degli studi presi in considerazione è stata valutata con il test di Higgins. Una valutazione complessiva del valore predittivo di danno è stata eseguita utilizzando il test di Mantel-Haenszel, basato sul modello effetti-fissi. Eventuali problemi legati alla pubblicazione sono stati valutati con un funnel plot e il metodo di Egger. Sono stati, alla fine, selezionati 8 lavori, per un numero complessivo di tronchi nervosi a rischio pari a 5.257. L'indagine ha mostrato un ruolo rilevante dello IONM nel prevenire danni nervosi transitori (valore predittivo positivo = 5% [95%CI:2-8], negativo = 96% [95%CI:91-100], rischio relativo = 0,73 [95%CI:0,54-0,98], p = 0,035), mentre non è stato possibile mettere in evidenza un effetto sul danno permanente [valore predittivo positivo = 2% (95%CI:0.6- 3.8), negativo 99% (95%CI:97-100), rischio relativo = 0,73 (95%CI:0,44-1,23), p = 0,235]. La meta analisi ha dimostrato l'importanza dello IONM nel prevenire il danno nervoso transitorio durante la tiroidectomia, mentre non è stato possibile rendere evidente un suo ruolo per quanto riguarda il danno permanente.
Introduction
In thyroid surgery, optimal exposure of the gland and clear identification of anatomical structures are the cornerstone to enhance the patient safety. Many refinements have been introduced in recent decades, including the use of intraoperative nerve monitoring (IONM), which has the objective of lowering the incidence of thyroidectomyassociated hoarseness related to recurrent laryngeal nerve (RLN) injury. The incidence of RLN injury after thyroidectomy widely varies in the literature, ranging from 0.4% to 7.2% for temporary paresis and from 0% to 5.2% for permanent paralysis 1-3. This incidence is often underestimated because injury may be ignored or undetected at postoperative laryngeal examination. In addition, the risk of RLN injury is increased in patients with local malignancy, previous thyroid surgery, neck irradiation, substernal goiter or anatomic variability of the nerve.
IONM has gained widespread acceptance as an adjunct to the gold standard of visual nerve identification, and this technique can be used to distinguish both the RLN and external branch of the superior laryngeal nerve 4 5. However, it remains unclear whether IONM adds any value to the clinical outcome of thyroidectomy in terms of preserved individual voice performance. Uncertainty in the literature concerning the merits of IONM led us to conduct the present meta-analysis. The objective of the present study was to assess the risk of transient or permanent RLN injury in thyroid surgery performed with or without IONM.
Materials and methods
Methodology was developed from standard guidelines outlined in the Cochrane Handbook for Systematic Reviews of Intervention (version 5.1.0) 6 and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement 7.
Literature review
We performed a literature search using electronic search engines PubMed and Ovid, and the Cochrane Library database to identify all clinical trials published between January 1994 and February 2012 that included the words "neuromonitoring AND thyroid AND neck surgery, intraoperative neuromonitoring, intraoperative electrophysiological monitoring, IONM, recurrent laryngeal nerve monitoring". The search was restricted to English-language literature and human subjects. We also checked the reference lists of all studies identified.
Inclusion criteria
Studies were included in the meta-analysis if they met the following criteria:
Randomised prospective trials or retrospective studies comparing patients undergoing thyroidectomy with or without IONM;
Surgery including total, subtotal or near-total thyroidectomy and thyroid lobectomy in patients presenting with thyroid cancer or benign thyroid disease;
Description of primary data, results of IONM testing, and clinical outcomes;
Nerve monitoring performed using different methods;
Possibility of data extraction/calculation from the published results.
In case of overlap between patient populations, authors and centres, the trial with the largest number of patients was selected.
Data collection for analysis
The reviewers (FR and VA) independently selected studies and extracted the following data from each article: inclusion and exclusion criteria for patient selection, study design, patient characteristics (i.e. number, mean age, sex ratio), details of IONM assessment and study endpoints. Reported findings were defined as true positive in case of injury in the absence of IONM, and false positive in case of absence of injury with IONM. True negative was determined in patients without injury and without IONM, and false negative in patients with injury with IONM. The objective of the analysis was to assess the presence of either transient or permanent RLN injury. Any disagreement was resolved after discussion.
Statistical analysis
All analyses were performed using Stata/SE 12.0 statistical software (StataCorp, College Station, TX, USA). For each study selected data were presented as positive predictive value (PPV), which is the number of true positive/ (number of true positive + number of false positive), and negative predictive value (NPV), number of true negative/ (number of true negative + number of false negative). Risk ratio (RR) with 95% confidence intervals (CI) was also calculated to establish the usefulness of IONM for the prediction of transient and permanent injury after surgery. The Higgins test (I2) was performed to check the heterogeneity of the studies analysed. On the basis of this test, summary estimates of predictive values in terms of injury were made using the Mantel-Haenszel method, which is based on the fixed-effects model. Publication bias was assessed using a funnel plot and Egger's method. The relative contribution of each study to the meta-analysis was calculated according to the amount of information it contained, the number of nerves at risk and their variability. The influence of individual studies on the summary-effect estimate was evaluated using influence analysis. Any individual study suspected of having excessive influence, that is point estimate of its "omitted" analysis lying outside the confidence interval (CI) of "combined" analysis, was removed from the study. Meta-regression analysis was conducted to investigate whether the type of study (randomised or other) was associated with the treatment effect. All analyses were performed for both transient and permanent RLN injuries. Statistical significance was set at p<0.05. Unless otherwise specified, the p-value was considered to be 2-tailed.
Results
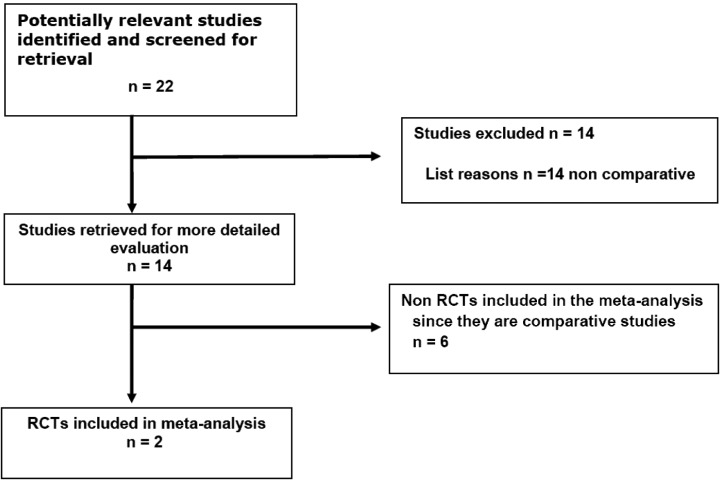
After excluding ineligible studies, eight articles were identified for full review 8-15 (Fig. 1). One study was not considered in the meta-analysis on permanent injuries because of the absence of relevant events (12). The eight studies selected included a total of 3029 patients with 5257 nerves at risk. The mean age of patients was 62 years (range 48–67 years), and the mean sex ratio was 3.76 (range 2.44-8.09). Table I details the characteristics of the studies included in the meta-analysis. Table II shows the incidence of transient and permanent RLN injury with or without the use of IONM. Table III shows the PPV, NPV, RR and corresponding 95% CI for each study on transient and permanent injuries.
Fig. 1.
Flow chart of the study.
Table I.
Main demographic features of studies selected for meta-analysis.
| Author Year | Type of study | Total patients | Total nerves at risk | Cancer | Men (%) |
|---|---|---|---|---|---|
| Atallah et al. 2009 (8) | Non-randomised | 261 | 421 | 17 | 23.0 |
| Barczyń ski et al. 2009 (9) | Randomised | 1000 | 2000 | 60 | 9.06 |
| Brauckhoff et al. 2002 (10) | Non-randomised | 97 | 182 | 75 | 42.3 |
| Chan et al. 2006 (11) | Non-randomised | 639 | 1000 | 141 | 24.7 |
| Dionigi et al. 2009 (12) | Randomised | 72 | 224 | 44 | 13.9 |
| Robertson et al. 2004 (13) | Non-randomised | 165 | 236 | 78 | 22.9 |
| Shindo & Chheda 2007 (14) | Non-randomised | 684 | 1043 | 377 | NA |
| Yarbrough et al. 2004 (15) | Non-randomised | 111 | 151 | 76 | 36.9 |
NA = not applicable
Table II.
Incidence of transient and permanent RLN injuries.
| Author | Transient injuries (%) | Permanent injuries (%) | ||
|---|---|---|---|---|
| With IONM | Without IONM | With IONM | Without IONM | |
| Atallah et al. 2009 (8) | 8.8 | 9.1 | 3.9 | 3.8 |
| Barczyń ski et al. 2009 (9) | 1.9 | 3.8 | 0.8 | 1.2 |
| Brauckhoff et al. 2002 (10) | 1.89 | 4.55 | 0.0 | 2.27 |
| Chan et al. 2006 (11) | 3.4 | 4.0 | 0.8 | 1.2 |
| Dionigi et al. 2009 (12) | 2.7 | 8.3 | 0.0 | 0.0 |
| Robertson et al. 2004 (13) | 3.45 | 4.24 | 0.86 | 2.54 |
| Shindo & Chheda 2007 (14) | 2.09 | 2.96 | 1.64 | 1.61 |
| Yarbrough et al. 2004 (15) | 15.4 | 11.9 | 3.8 | 5.1 |
Table III.
Positive predictive value (PPV), negative predictive value (NPV) and relative risk (RR) regarding transient and permanent injuries.
| Author | Transient injuries | Permanent injuries | ||||
|---|---|---|---|---|---|---|
| PPV% (95% CI) | NPV% (95% CI) | RR (95% CI) | PPV% (95% CI) | NPV% (95% CI) | RR (95% CI) | |
| Atallah et al. (2009) (8) | 5 (3-9) | 95 (91-98) | 0.92 (0.40-2.10) | 4 (2-7) | 96 (92-98) | 1.00 (0.38-2.64) |
| Barczyń ski et al. (2009) (9) | 4 (3-5) | 98 (97-99) | 0.50 (0.29-0.86) | 1 (0-2) | 99 (98-100) | 0.67 (0.27-1.62) |
| Brauckhoff et al. (2002) (10) | 2 (0-8) | 99 (94-100) | 0.43 (0.04-4.64) | 1 (0-6) | 100 (96-100) | 0.29 (0.01-6.93) |
| Chan et al. (2006) (11) | 4 (2-6) | 97 (95-98) | 0.85 (0.45-1.60) | 1 (0-3) | 99 (98-100) | 0.66 (0.19-2.34) |
| Dionigi et al.* (2009) (12) | 3 (0-7) | 99 (95-100) | 0.35 (0.04-3.27) | - | - | - |
| Robertson et al. (2004) (13) | 4 (1-9) | 97 (91-99) | 0.83 (0.23-3.01) | 3 (0-7) | 99 (95-100) | 0.34 (0.04-3.27) |
| Shindo & Chheda (2007) (14) | 3 (1-5) | 98 (97-99) | 0.71 (0.32-1.54) | 0 (0-1) | 100 (99-100) | 1.11(0.10-12.19) |
| Yarbrough et al. (2004) (15) | 1 (0-2) | 83 (70-92) | 1.28 (0.53-3.07) | 5 (1-14) | 96 (87-100) | 0.76 (0.13-4.35) |
| Total meta-analysis | 5 (2-8) | 96 (91-100) | 0.73 (0.54-0.98) | 2 (0.6-3.8) | 99 (97-100) | 0.73 (0.44-1.23) |
Dionigi et al. was excluded for the absence of RLN permanent palsy
Transient injury
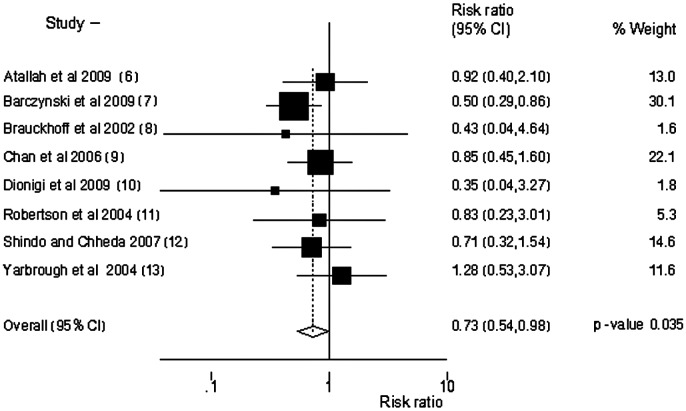
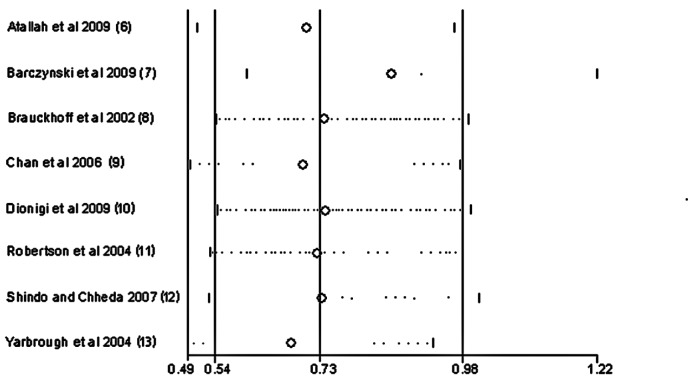
Overall results yielded by the Mantel-Haenszel method (fixed effect suggested by the heterogeneity test: I2 = 0.5%, p = 0.708) demonstrated a significant role of IONM in predicting RLN transient injuries: PPV was 5% (95% CI: 2–8) and the NPV was 96% (95% CI: 91-100), RR of 0.73 (95% CI: 0.54-0.98) with p = 0.035 (Fig. 2). Influence analysis was performed to identify studies with excessive influence (Fig. 3). The Begg test revealed that no bias was found in the publications used for the meta- analysis (Kendall's score, one-sided, p = 1.000). The type of study was not associated with the treatment effect (p = 0.078).
Fig. 2.
Forest plot depicting the contribution (box area) and the relative risk of transient injury with/without IONM in each study included in the metaanalysis.
Fig. 3.
Influence of transient injury with/without IONM in studies included in the meta-analysis.
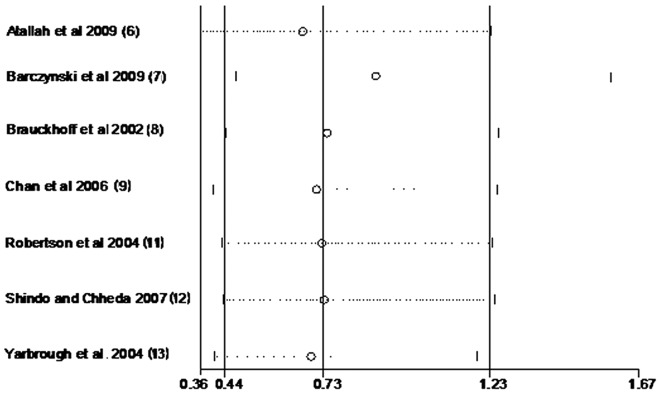
Permanent injury
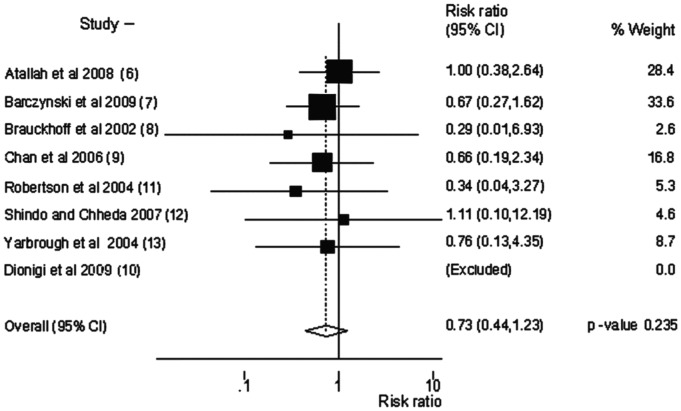
Permanent RLN injuries were not predictable by IONM as demonstrated by the overall results yielded by the Mantel-Haenszel method (fixed effect suggested by the heterogeneity test: I2 = 4.2%, p = 0.969). The summary PPV was 2% (95% CI: 0.6–3.8) and the NPV was 99% (95% CI: 97-100) with a univariate RR of 0.73 (95% CI: 0.44-1.23) and p = 0.235 (Fig. 4). No study showed excessive influence as determined by influence analysis (Fig. 5). The Begg test revealed no publication bias, shown by Kendall's score (1-sided, p = 0.548). The type of study was not associated with the treatment effect (p = 0.303).
Fig. 4.
Forest plot depicting the contribution (box area) and the relative risk of permanent injury with/without IONM in each study included in the metaanalysis.
Fig. 5.
Influence of permanent injury with/without IONM in studies included in the meta-analysis.
Discussion
RLN palsy is a serious complication after thyroid surgery leading, depending on its severity, to voice disorders, respiratory distress and aspiration 16. Consequently, quality of life may be impacted, possibly prompting medico-legal litigation against the surgeon 17 18. During thyroidectomy, injury to the RLN may be a result of unintentional sectioning, stretching, thermal injury, entrapment by a ligature or ischaemia. Clear identification of the nerve by careful dissection, even in case of abnormal anatomy, is the best approach to avoid nerve trauma. IONM by electrical stimulation has been described and proposed during thyroid surgery for more than four decades 19 20. It has the potential to enhance visual identification of the nerve, allowing more precise dissection and verification of its integrity, which minimises the risk of injury. A growing number of surgeons are using IONM in all cases of thyroid and parathyroid surgery, while others do so in selected patients considered at risk of RLN injury. However, many still do not use IONM, preferring direct visualisation. To the best of our knowledge, there is no overwhelming scientific evidence of its actual benefits in RLN preservation.
The current meta-analysis shows the impact of IONM on preventing transient RLN injury, but fails to demonstrate any effect on permanent palsy. This apparent discrepancy is related to the fact that transient injury occurs more frequently than permanent damage, and evolves in the majority of cases towards complete recovery and normal vocal cord function in the long term.
Although a beneficial effect of IONM in terms of lower incidence of transient and permanent nerve palsy has been suggested 21 22, many studies question its added value 23 26. The relationship between IONM and functional postoperative outcome has therefore proven to be less evident to define than expected, yielding a number of conflicting results. These discrepancies may be related to a relatively low PPV 5. As the incidence of RLN palsy is low in experienced hands, to demonstrate the added value of IONM, one may postulate that inclusion of a large number of patients is needed. The current meta-analysis does not support this premise, however, as the positive contribution of IONM was observed in studies with no more than 2000 nerves at risk 9 10. It is also worth mentioning that in the largest multi-institutional prospective study evaluating a total of 16,448 consecutive thyroid procedures, IONM did not have any beneficial value compared to visual identification of RLN in the context of permanent paralysis 27. In this study, independent risk factors for permanent RLN paralysis included recurrent malignant or benign goiter, malignant disease, thyroid lobectomy, no nerve identification and low hospital or surgeon volume 27. It should be noted, however, that the latter study was removed from the current meta-analysis due to its overwhelming statistical weight and absence of data related to transient RLN palsy.
Controversies may be also related to poor uniformity of patient groups across different studies and lack of randomised controlled trials. Nerve injury risk during surgery for multinodular goiters is obviously lower than in case of surgery for large substernal masses growing in a restricted space, prior surgery due to fibrous tissue adhering firmly to the gland, surgery for thyroid cancer with lymph node dissection and recurrent malignancy with possible tumour infiltration of the nerve. For any given group of patients assessed by risk-group stratification, only prospective randomised controlled trials, possibly multicentre to reach a significant volume, have the potential to determine whether IONM achieves better results than direct identification of RLN by visual inspection. The individual performance of the surgeon has been shown to be the single most important factor related to postoperative outcome in case of surgery for "simple" benign goiters 28. In this context, nerve injury risk is almost nil in the hands of experienced surgeons, and there is no consistent need for IONM. By contrast, it was recently demonstrated that IONM improves outcomes of surgery for well differentiated thyroid cancer 27. In fact, the use of IONM helps to avoid the problem of remnant thyroid tissue during dissection at the level of Berry's ligament, where the RLN may be branched.
Although there is no global consensus on its value in every thyroid surgical procedure, IONM plays a key role in many circumstances that could aggravate the risk of nerve injury.
Indeed, the main benefit of IONM is its ability to guide the surgeon in the event of variations in the expected anatomic course of the inferior laryngeal nerve 9, or in case of a non-recurrent inferior laryngeal nerve revealed by short latency, as recently demonstrated 30. The risk of nerve injury increases in patients with an anomalous RLN anatomy. Such variations include non-recurrence mainly on the right side 31 32, nerve displacement 33-35 by thyroid nodularity or paratracheal lymphadenopathy, extralaryngeal branching of the RLN observed in 30% of patients 31, and variations in the nerve course in relation to the inferior thyroid artery and Berry's ligament. In a recent analysis of RLN in 502 thyroid dissections, 60.8% of nerves were found to be in the expected tracheoesophageal groove position, while 4.9% were lateral and 28.3% were posterior to the trachea. Of greatest concern are cases where the RLN is located on the anterior surface of the thyroid gland (6%), which is a particularly high-risk area for nerve injury 36. IONM has also been shown to be helpful during minimal-access thyroid surgery procedures 37, including video-assisted thyroidectomy 12. As dissection is conducted in a narrow space, use of a stimulator helps to identify the plane of dissection and gives surgeons more confidence during surgery. However, benefits in terms of reduced postoperative morbidity were not demonstrated 12.
Despite the fact that the small number of included studies and lack of prospective randomised trials available for analysis limit the current meta-analysis, our results add new insights into the role of IONM during thyroidectomy, highlighting its merits in preventing transient injury. IONM methodology is a welcome adjunct to the surgical armamentarium, leading to better quality control during thyroid surgery. Further studies conducted according to international recommendations 4 are nevertheless required to confirm these findings in populations with different risk factors.
References
- 1.Steurer M, Passler C, Denk DM, et al. Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope. 2002;112:124–133. doi: 10.1097/00005537-200201000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Barczyński M, Konturek A, Stopa M, et al. Total thyroidectomy for benign thyroid disease: is it really worthwhile? Ann Surg. 2011;254:724–729. doi: 10.1097/SLA.0b013e3182360118. [DOI] [PubMed] [Google Scholar]
- 3.Witt RL. Recurrent laryngeal nerve electrophysiologic monitoring in thyroid surgery: the standard of care? J Voice. 2005;19:497–500. doi: 10.1016/j.jvoice.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Randolph GW, Dralle H. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011;21(Suppl. 1):S1–S16. doi: 10.1002/lary.21119. [DOI] [PubMed] [Google Scholar]
- 5.Dralle H, Sekulla C, Lorenz K, et al. German IONM Study Group. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg. 2008;32:1358–1366. doi: 10.1007/s00268-008-9483-2. [DOI] [PubMed] [Google Scholar]
- 6.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. 2011. Version 5.1.0 (updated March 2011). The Cochrane Collaboration; http://www.cochranehandbook.org. [Google Scholar]
- 7.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA Statement for Reporting systematic reviews and meta-analyses of studies that evaluate health care interventions explanation and elaboration. PLoS Med. 2009;6:1–27. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atallah I, Dupret A, Carpentier AS, et al. Role of intraoperative neuromonitoring of the recurrent laryngeal nerve in high-risk thyroid surgery. J Otolaryngol Head Neck Surg. 2009;38:613–618. [PubMed] [Google Scholar]
- 9.Barczyński M, Konturek A, Cichon S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg. 2009;96:240–246. doi: 10.1002/bjs.6417. [DOI] [PubMed] [Google Scholar]
- 10.Brauckhoff M, Gimm O, Thanh PN, et al. First experiences in intraoperative neurostimulation of the recurrent laryngeal nerve during thyroid surgery of children and adolescents. J Pediatr Surg. 2002;37:1414–1418. doi: 10.1053/jpsu.2002.35403. [DOI] [PubMed] [Google Scholar]
- 11.Chan WF, Lang BH, Lo CY. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery. 2006;140:866–872. doi: 10.1016/j.surg.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 12.Dionigi G, Boni L, Rovera F, et al. Neuromonitoring and video- assisted thyroidectomy: a prospective, randomized casecontrol evaluation. Surg Endosc. 2009;23:996–1003. doi: 10.1007/s00464-008-0098-3. [DOI] [PubMed] [Google Scholar]
- 13.Robertson ML, Steward DL, Gluckman JL, Welge J. Continuous laryngeal nerve integrity monitoring during thyroidectomy: does it reduce risk of injury? Otolaryngol Head Neck Surg. 2004;131:596–600. doi: 10.1016/j.otohns.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 14.Shindo M, Chheda NN. Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2007;133:481–485. doi: 10.1001/archotol.133.5.481. [DOI] [PubMed] [Google Scholar]
- 15.Yarbrough DE, Thompson GB, Kasperbauer JL, et al. Intraoperative electromyographic monitoring of the recurrent laryngeal nerve in preoperative thyroid and parathyroid surgery. Surgery. 2004;136:1107–1115. doi: 10.1016/j.surg.2004.06.040. [DOI] [PubMed] [Google Scholar]
- 16.Bhattacharyya N, Fried MP. Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg. 2002;128:389–392. doi: 10.1001/archotol.128.4.389. [DOI] [PubMed] [Google Scholar]
- 17.Ready AR, Barnes AD. Complications of thyroidectomy. Br J Surg. 1994;81:1555–1556. doi: 10.1002/bjs.1800811103. [DOI] [PubMed] [Google Scholar]
- 18.Kern KA. Medicolegal analysis of errors in diagnosis and treatment of surgical endocrine disease. Surgery. 1993;114:1167–1173. [PubMed] [Google Scholar]
- 19.Shedd DP, Burget GC. Identification of the recurrent laryngeal nerve: electrical method for evaluation in the human. Arch Surg. 1966;92:861–864. doi: 10.1001/archsurg.1966.01320240049010. [DOI] [PubMed] [Google Scholar]
- 20.Flisberg K, Lindholm T. Electrical stimulation of the human laryngeal nerve during thyroid operation. Acta Otolaryngol. 1970;263:63–67. doi: 10.3109/00016487009131523. [DOI] [PubMed] [Google Scholar]
- 21.Thomusch O, Sekulla C, Walls G, et al. Intraoperative neuromonitoring of surgery for benign goiter. Am J Surg. 2002;183:673–678. doi: 10.1016/s0002-9610(02)00856-5. [DOI] [PubMed] [Google Scholar]
- 22.Randolph GW, Kobler JB, Wilkins J. Recurrent laryngeal nerve identification and assessment during thyroid surgery: laryngeal palpation. World J Surg. 2004;28:755–760. doi: 10.1007/s00268-004-7348-x. [DOI] [PubMed] [Google Scholar]
- 23.Beldi G, Kinsbergen T, Schlumpf R. Evaluation of intraoperative recurrent nerve monitoring in thyroid surgery. World J Surg. 2004;28:589–591. doi: 10.1007/s00268-004-7226-6. [DOI] [PubMed] [Google Scholar]
- 24.Hermann M, Hellebart C, Freissmuth M. Neuromonitoring in thyroid surgery: prospective evaluation of intraoperative electrophysiological responses for the prediction of recurrent laryngeal nerve injury. Ann Surg. 2004;240:9–17. doi: 10.1097/01.sla.0000132260.34503.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loch-Wilkinson TJ, Stalberg PLH, Sidhu SB, et al. Nerve stimulation in thyroid surgery: is it really useful? ANZ J Surg. 2007;77:377–380. doi: 10.1111/j.1445-2197.2007.04065.x. [DOI] [PubMed] [Google Scholar]
- 26.Higgins TS, Gupta R, Ketcham AS, et al. Recurrent laryngeal nerve monitoring versus identification alone on postthyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope. 2011;121:1009–1017. doi: 10.1002/lary.21578. [DOI] [PubMed] [Google Scholar]
- 27.Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004;136:1310–1322. doi: 10.1016/j.surg.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 28.Hermann M, Alk G, Roka R, et al. Laryngeal recurrent nerve injury in surgery for benign thyroid diseases effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg. 2002;235:261–268. doi: 10.1097/00000658-200202000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barczyński M, Konturek A, Stopa M, et al. Clinical value of intraoperative neuromonitoring of the recurrent laryngeal nerves in improving outcomes of surgery for welldifferentiated thyroid cancer. Polski Przeglad Chirurgiczny. 2011;83:196–203. doi: 10.2478/v10035-011-0030-8. [DOI] [PubMed] [Google Scholar]
- 30.Brauckhoff M, Machens A, Sekulla C, et al. Latencies shorter than 3.5 ms after vagus nerve stimulation signify a nonrecurrent inferior laryngeal nerve before dissection. Ann Surg. 2011;253:1172–1177. doi: 10.1097/SLA.0b013e3182128b9e. [DOI] [PubMed] [Google Scholar]
- 31.Toniato A, Mazzarotto R, Piotto A, et al. Identification of the nonrecurrent laryngeal nerve during thyroid surgery: 20-year experience. World J Surg. 2004;28:659–661. doi: 10.1007/s00268-004-7197-7. [DOI] [PubMed] [Google Scholar]
- 32.Rocco A, Maurizi M, Galli J, et al. Sul nervo laringeo inferiore non ricorrente. Acta Otorhinolaryngol Ital. 1994;14:535–541. [PubMed] [Google Scholar]
- 33.Randolph GW. Surgical anatomy of the recurrent laryngeal nerve. In: Randolph GW, editor. Surgery of the Thyroid and Parathyroid Glands. 1st edition. Philadelphia, PA: Saunders; 2003. pp. 300–342. [Google Scholar]
- 34.Zábrodský M, Bouček J, Kastner J, et al. Immediate revision in patients with bilateral recurrent laryngeal nerve palsy after thyroid and parathyroid surgery. How worthy is it? Acta Otorhinolaryngol Ital. 2012;32:222–228. [PMC free article] [PubMed] [Google Scholar]
- 35.Sancho JJ, Pascual-Damieta M, Pereira JA, et al. Risk factors for transient vocal cord palsy after thyroidectomy. Br J Surg. 2008;95:961–967. doi: 10.1002/bjs.6173. [DOI] [PubMed] [Google Scholar]
- 36.Hisham AN, Lukman MR. Recurrent laryngeal nerve in thyroid surgery: a critical appraisal. ANZ J Surg. 2002;72:887–889. doi: 10.1046/j.1445-2197.2002.02578.x. [DOI] [PubMed] [Google Scholar]
- 37.Terris DJ, Anderson SK, Watts TL, et al. Laryngeal nerve monitoring and minimally invasive thyroid surgery: complementary technologies. Arch Otolaryngol Head Neck Surg. 2007;133:1254–1257. doi: 10.1001/archotol.133.12.1254. [DOI] [PubMed] [Google Scholar]