SUMMARY
To analyse the complications related to pexy, the main clinical manifestations that may raise suspicions of a pexy line rupture/detachment, the most suitable diagnostic technique and the optimum treatment to resolve this complication. This is a retrospective chart review in tertiary university referral centre. Medical charts of patients with oncological laryngeal pathologies admitted to the Otolaryngology Department of the University Hospital of Modena between May 2003 and March 2012 were analysed. Ten patients with rupture of the pexy were identified and included in the present study. The clinical manifestations were dysphagia, alteration of sensitivity of hypopharyngeallaryngeal structures, fever, infection and diastasis of surgical wounds, bleeding, dysphonia and aspiration pneumonia. Rupture of the pexy was diagnosed through endoscopic evaluations, radiological techniques or directly in the operating room during revision surgery of the earlier operation. Surgical treatments, coupled with effective swallowing rehabilitation, allowed progressive functional recovery. Patients were hospitalised until recovery of laryngeal functions was complete. In conclusion, pexy line rupture is one of the complications in the post-operative period of partial laryngectomies. Certain clinical manifestations may indicate this complication, helping the surgeon to establish an early diagnosis and administer prompt treatment.
KEY WORDS: Pexy, Partial laryngectomies, Laryngeal cancer, Dysphagia, Dyspnoea
RIASSUNTO
L'obbiettivo di questo studio è analizzare le complicanze correlate alla pessia, le principali manifestazioni cliniche che possano far nascere il sospetto di distacco di pessia, le principali tecniche diagnostiche e il miglior trattamento per risolvere questa complicanza. Trattasi di una revisione retrospettiva della documentazione clinica in un centro universitario di riferimento terziario. Sono state analizzate le cartelle cliniche di pazienti affetti da patologia laringea oncologica ricoverati nella Struttura Complessa di Otorinolaringoiatria dell'Azienda Ospedaliero-Universitaria di Modena tra maggio 2003 e marzo 2012. Dieci pazienti con distacco di pessia sono stati identificati ed inclusi in questo studio. Le manifestazioni cliniche riscontrate sono state: disfagia, alterazione della sensibilità delle strutture ipofaringo-laringee, febbre, infezione e diastasi delle ferite chirurgiche, emorragia, disfonia e polmoniti ab-ingestis. Il distacco di pessia è stato diagnosticato mediante valutazioni fibroendoscopiche, imaging radiologico o direttamente in sala operatoria durante il primo intervento o durante la chirurgia di revisione. Concludendo il distacco di pessia è una delle complicanze postoperatorie delle laringectomie parziali e alcune manifestazioni cliniche possono farla sospettare aiutando il chirurgo a giungere ad una diagnosi precoce, così da effettuare il prima possibile un adeguato trattamento.
Introduction
The word pexy is derived from the Greek word pêxy, which means union or fixation. By performing a pexy, the surgeon performs a fixation of tissues to try to restore the anatomy and function of the organ. Partial laryngectomies consist of a partial laryngeal resection which allows cancers of the larynx to be removed sparing the three laryngeal functions: swallowing, breathing and phonation. Different types of partial laryngectomy are described in the literature according to the different surgical techniques used for reconstruction. In supraglottic horizontal laryngectomy, the upper part of the larynx, excluding the vocal folds, is removed and the aero-digestive carrefour is reconstructed by a direct suture between the residual part of thyroid cartilage and the hyoid bone (thyro-hyoido-pexy) 1. In supracricoid partial laryngectomy, the supracricoid larynx, excluding the epiglottic stump, is removed and a suture is made among the cricoid, the residual part of the epiglottis and the hyoid bone (cricohyoidoepiglottopexy) 2 3. If the resection also includes the whole epiglottis, a supracricoid partial laryngectomy with cricohyoidopexy is performed 4. In a subtotal partial laryngectomy, the pexy is performed among the trachea, epiglottis and hyoid bone (tracheohyoidoepiglottopexy) or between the trachea and hyoid bone (tracheohyoidopexy), if the epiglottis and the hyothyroepiglottic space is removed 5. Even in horizontal glottectomy, a pexy is required, as codified by Calearo and Teatini 6. In particular, a thyrocricopexy must be made after removal of the entire glottis.
The objective of this study is to describe the complications and the main clinical manifestations related to pexy line rupture/detachment. The most suitable diagnostic techniques and optimum treatment to resolve this complication are also described.
Materials and methods
Medical charts of patients in the Otolaryngology Department of the University Hospital of Modena with a diagnosis of pexy detachment between May 2003 and March 2012 were retrospectively analysed. The parameters evaluated for each patient were sex, age at surgery, type of partial laryngectomy, date of surgery, main clinical manifestations apparent after the operation, time of symptom onset, diagnostic techniques used and surgical treatment performed.
Results
Ten patients with rupture of the pexy were identified (9 male and 1 female) (Table I). The average age was 59 years (range 49-65). Six patients underwent partial laryngectomy with cricohyoidopexy (three with sparing of both arytenoids, three with sparing of only one of the arytenoids); in two patients, partial laryngectomy with cricohyoidoepiglottopexy (one of two with sparing of both arytenoids) was performed; one patient underwent tracheohyoidoepiglottopexy (with sparing of one arytenoid) and the last underwent supraglottic horizontal laryngectomy. The operations were carried out between June 2004 and November 2011. Of the 10 patients, three had their laryngectomy in our department, while the remaining seven had their laryngectomy in other hospitals, and were referred to our hospital for post-operative problems.
Table I.
Patient demographics.
| Patient | Sex | Age at surgery | Type of surgery | Date of surgery | Main manifestations | Time of symptom onset (postoperative day) | Diagnosis | Treatment |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 57 | CHP+A | May 2010 | Dysphagia, absence of sensivity of hypopharyngeal– laryngeal structures | 9 days | FEES, neck 3D CT, VFSS |
Surgical revision + laryngeal injection of Vox Implants |
| 2 | M | 62 | CHP | October 2011 | Dysphagia, reduced sensivity of hypopharyngeal– laryngeal structures | 9 days | FEES, neck 3D CT |
Logopaedic rehabilitation, laryngeal injection of Vox Implants |
| 3 | M | 58 | CHEP | February 2011 | Fever, infection and diastasis of cervical wound, bleeding | 6 days | Neck 3D CT | Antibiotic therapy + surgical revision |
| 4 | M | 65 | CHEP+A | November 2011 | Bleeding | 8 days | Intraoperative | Surgical revision |
| 5 | M | 54 | THEP +A | June 2007 | Laterocervical fistula | 10 days | Intraoperative | Surgical revision |
| 6 | M | 65 | CHP+A | June 2009 | Dysphagia | 9 days | FEES, neck CT, VFSS | Laryngeal injection of Vox Implants + surgical revision |
| 7 | M | 65 | SHL +A | June 2004 | Dysphagia | 9 days | Intraoperative | Surgical revision + laryngeal injection of Vox Implants |
| 8 | M | 54 | CHP | September 2005 | Aspiration pneumonia, dyspnoea, dysphonia | 27 days | Intraoperative | Surgical revision |
| 9 | M | 63 | CHP+A | August 2008 | Dysphagia, aspiration pneumonia, arytenoid paralysis | 9 days | FEES neck, 3D CT, cervical slice CT |
Surgical revision + laryngeal injection of Vox Implants |
| 10 | F | 49 | CHP | September 2008 | Dysphagia | FEES, neck 3D CT |
Surgical revision + laryngeal injection of Vox Implants |
M, male; F, female; CHEP, cricohyoidoepiglottopexy; CHP, cricohyoidopexy; THEP, tracheohyoidoepiglottopexy; A, arytenoid; SHL, supraglottic horizontal laryingectomy; FEES, functional endoscopic evaluation of swallowing; VFSS, videofluorographic swallowing study.
The most frequent clinical manifestation was dysphagia (6/10), followed by bleeding (2/10), aspiration pneumonia (2/10) and alteration of sensitivity of hypopharyngeal- laryngeal structures (2/10) (Table I). Other symptoms or clinical signs were: dyspnoea (1/10), dysphonia (1/10), fever (1/10), arytenoid paralysis (1/10), infection and diastasis of a cervical wound (1/10) and laterocervical purulent fistula (1/10).
The time of symptom onset ranged from the early postoperative period until 27 days after the operation.
The diagnostic techniques included functional endoscopic evaluation of swallowing (FEES); neck anterolateral x-rays and 3D CT scan (Figs. 1-2); videofluorographic study of swallowing (VFSS); direct observation during revision surgery. Surgical treatments performed in patients affected by rupture of the pexy were revision surgery of the pexy; laryngeal injection of Vox® Implants (Table I). Surgical treatments, coupled with effective swallowing rehabilitation, allowed progressive functional recovery. Patients were hospitalised until complete healing of cervical wounds or lung infections and recovery of laryngeal functions was completed. Dysphagia was resolved and all patients took meals regularly through natural ways.
Fig. 1.

A post-operative latero-lateral neck X-ray in a patient who underwent partial reconstructive laryngectomy: the detachment of the pexy is visible as an air band between the hyoid bone (above) and the cricoid cartilage (below).
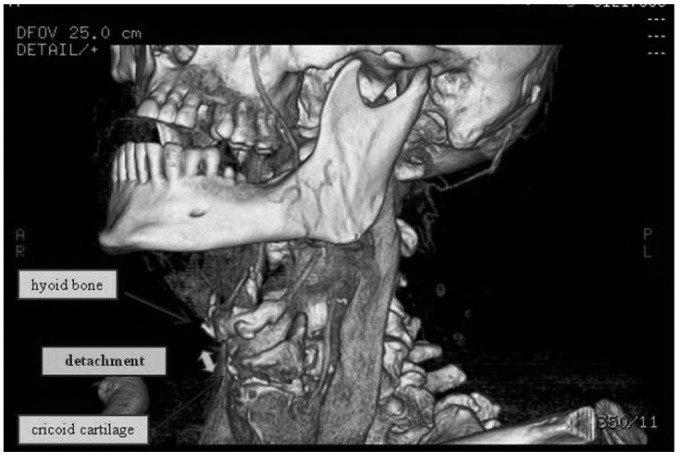
Fig. 2.
A 3D neck CT scan shows the gap between the hyoid bone (above) and the cricoid cartilage (below) in a patient with detachment of the pexy who underwent partial reconstructive laryngectomy.
Discussion
Rehabilitation of the patient who undergoes partial laryngectomy is a very important part of clinical management. On the second or third post-operative day, the cuffed tracheotomy tube, introduced at the end of the operation, is usually replaced with a fenestrated tracheotomy tube. On the 7-8th post-operative day, the patient begins swallowing exercises under the guidance of a speech therapist, if not contraindicated by clinical issues or post-operative complications. For a number of days, semi-solid food is taken by the patient until solid foods can be ingested. Liquids are usually swallowed with more difficulty, and are the last to be introduced in the patient's diet. Decannulation must take place as soon as possible to avoid complications such as appearance of granulation tissue or subcutaneous emphysema caused by the tracheostomy tube itself 7-9. The weaning from the tracheostomy tube may occur by the placement of a smaller tracheostomy tube or by its closure with a cap.
Pexy line rupture is an infrequent complication that may occur in patients with normal post-operative course after partial laryngectomies. In our experience, the onset of some clinical manifestations may raise suspicions of a pexy line disorder. In our cohort of patients, the symptoms appeared from the beginning of swallowing exercises on the 7-8th post-operative day until the 27th post-operative day.
Signs and symptoms of detachment of the pexy appeared in the first few days after wound healing (8-10th post-operative day) in almost all patients (9/10). Only one patient showed a complication related to the pexy after 26 days.
Dysphagia is the most frequently reported symptom. When detachment of the pexy occurs, the residual portion of the larynx cannot move upwards and allow satisfactory swallowing for the patient. Six patients experienced this on the 7-8th post-operative day. Dysphagia was the only symptom in two patients, while in the other four it was associated with absence or reduction in sensitivity of hypopharyngeal-laryngeal structures or aspiration pneumonia. Bleeding from the cervical wound occurred early in a sudden and dramatic way sufficient to require emergency revision surgery in the operating room. The appearance of bleeding suggests an unexpected failure of a vessel ligation, probably after a patient effort with increased intrathoracic pressure. Bleeding occurred in two patients and was the only sign in one. The absence or reduction in sensitivity of hypopharyngeal-laryngeal structures may be related to an intraoperative surgical error when the superior laryngeal nerve is not spared, and was found in two patients. Both underwent supracricoid partial laryngectomy with cricohyoidopexy. FEES allowed the alteration of bolus transit to be verified in these patients. Wound infection with onset of fever and diastasis of the cervical wound was present in one patient. It appeared on the sixth post-operative day associated with bleeding and required surgical treatment that allowed the pexy line rupture to be observed directly, and at the same time to be repaired. Aspiration pneumonia, dyspnoea and dysphonia occurred in the patient who revealed detachment of the pexy on the 26th post-operative day. These symptoms usually occur in patients who have begun vocal and swallowing rehabilitation.
Our study showed that appearance of the symptoms just mentioned, particularly dysphagia, after a partial laryngectomy in a patient without post-operative complications, may indicate detachment of the pexy. Subsequently, we considered it appropriate to perform instrumental tests to confirm clinical suspicions. We first submitted our patients to FEES10 performed by a phoniatric surgeon and speech therapist. This exam allowed us to identify the incorrect passage of the bolus in the digestive tract: all patients undergoing FEES presented penetration of the bolus in the respiratory tract. In two patients, FEES was very useful to identify alterations of laryngeal sensitivity during passage of the bolus.
Laryngeal aspiration can be detected by a videofluorographic swallowing study (VFSS). This permits the visualization of bolus flow in real time in relation to structural movement throughout the upper aerodigestive tract and detection of the presence and timing of aspiration 11. VFSS was performed in two patients by a radiologist experienced in visceral diagnostics, and in association with FEES, helped to make the diagnosis of a swallowing disorder.
A neck 3D CT scan was performed in six of 10 patients. 3D CT is a new technology in imaging diagnostics which gives high definition three-dimensional reconstructions, including multiplanar reformations (MPR) reconstructed from thin axial slices 12. This technique allows a rupture of the pexy to be confirmed if there is a gap of more than 3 cm between the lower border of the hyoid bone and the cricoid cartilage 13.
In some patients, diagnosis of rupture of the pexy was made during revision surgery, because of both the need to re-operate promptly owing to the sudden onset of a complication such as bleeding from the cervical wound, and the difficulty in reaching a diagnosis because of very poor or lack of signs and symptoms.
A pexy line disorder after a partial laryngectomy is an infrequent complication. In the literature, the incidence of rupture of the pexy is reported to range from 0.8% 14 to 4.9% 15. In a large series, Rizzotto et al. have detected rupture of the pexy in 4 of 469 cases.16 Over a 9-year period, the incidence of this complication in our ENT Department was 1.4% (3/215). According to the literature, the early post-operative period is the most frequent in the development of this complication, and the presence of splitting at the hyoid bone-cricoid or thyroid cartilage junction and elevation of the neck flap with subcutaneous emphysema, is supportive of the diagnosis 17. Some authors have identified transection of the cricoid arch by sutures, a partial resection or a non-ossified cricoid, and the need to relocate a tracheal cannula in an emergency as predisposing factors for detachment of the pexy 14. Other authors have indicated previous laryngeal irradiation as one of the most important risk factors for rupture of the pexy, because of osteitis induced on the hyoid bone 15. A pexy line rupture is confirmed when there is a gap of more than 30 mm between the lower border of the hyoid bone and the cricoid cartilage from the CT scan in a patient having difficulty swallowing 13. To avoid this complication, before doing a pexy, Naudo et al. 18 suggested a mediastinal dissection of the anterior tracheal wall to reduce the tension at the level of the suture line and to include the first two tracheal rings in the pexy when possible. Tension-free sutures should be made 1 cm away from the midline at the time of the pexy in the initial surgery to avoid rupture of the pexy 14. The sutures may be preceded by slightly flexing the head of the patient forward.
Sutures of synthetic absorbable material (Vicryl®, PDS®) are usually used. The most commonly used are PDS® (polydioxanone, Ethicon Inc., New Jersey, USA), a monofilament which is absorbed slowly over a period of 6 to 7 months or Vicryl® (polyglactin, Ethicon Inc., New Jersey, USA), a twisted polyfilament which completely dissolves over a shorter period (up to 3 months). When a cricohyoidoepiglottopexy is performed, three thick sutures pass under the cricoid toward the laryngeal lumen, transfix the epiglottis and cross below the hyoid bone 3. A cricohyoidopexy is realized by thick sutures (no. 2 or 3) which pass between the first tracheal ring and below the residual cricoid arch, surround below the hyoid bone 4. To obtain a correct pexy, the anterior margin of the cricoid must be behind the hyoid bone after ligation of the sutures 3 so as to avoid post-operative stenosis of the neoglottis.
According to some authors, the suture must be performed by three well separated stitches with the central one crossing the cricoid cartilage, hyoid bone and epiglottis (if present), at least 3 cm away from the tongue base 19.
In subtotal laryngectomy with tracheohyoidopexy (or tracheohyoidoepiglottopexy), suspension of the trachea to the hyoid is performed using five double stitches of resistant suture (Vicryl II, Dexon II), which are passed through the first and second tracheal ring, through the preepiglottic space (tracheohyoidoepiglottopexy (THEP)) and through the base of the tongue encircling the hyoid bone (THP and tracheohyoidopexy (THIP)) 5.
In thyro-cricopexy, after a horizontal glottectomy, three stitches of absorbable material join the cricoid arch to the thyroid cartilage stump above it 6. In a supraglottic horizontal laryngectomy, a suture is made with 4 or 5 stitches of absorbable material between the residual thyroid cartilage and the hyoid bone above it 1.
To prevent the complication of the rupture of the pexy, Rizzotto et al. 5 have described as basic manoeuvres the suspension of the thyroid gland, which is sutured to the suprahyoid muscles and performing a tracheostomy at the level of the 5th or 6th tracheal ring in order to hold the pexy and avoid any traction on it.
Preservation of the superior laryngeal nerve is very important to allow proper recovery of swallowing function after the operation. The surgeon must spare this nerve both in the initial stages of laryngeal resection and subsequently while performing the pexy. Rizzotto et al.5 recommended that the first stitch passes along the midline reaching within 1-2 cm of the base of the tongue, whereas the lateral stitches should pass in front of the posterior cricoid plate through the base of the tongue close to the hyoid bone so as not to damage the superior laryngeal nerve, lingual artery and hypoglossal nerve.
Treatment is usually performed by revision surgery of the pexy line or by a laryngeal injection of Vox® Implants. In the revision surgery, the patient undergoes a second operation in which the region of the pexy is identified and a re-suturing of the pexy is performed. Sometimes, it is useful to administer a laryngeal injection of Vox® Implants when it is necessary to provide greater competence to the neoglottis 20. Only rarely is it necessary to perform a total laryngectomy 15.
Open revision surgery is most suitable in large detachment of the pexy, when it is diagnosed early and the patient is still hospitalised, in cases of marked alteration of neoglottis which does not allow swallowing and in patients with infection or bleeding. Laryngeal injection of Vox® Implants is performed when the neoglottis competence is partially impaired and are not obvious major complications.
Is very important to diagnose rupture of the pexy as soon as possible. Early treatment prevents respiratory or infectious complications and massive bleedings, which can compromise the overall health of the patient.
Conclusions
Detachment of the pexy is an infrequent complication after partial laryngectomies. Dysphagia is the most frequent clinical manifestation and may occur between the 6th and the 27th post-operative days. Alteration of sensitivity of hypopharyngeal-laryngeal structures, fever, infection and diastasis of surgical wounds, bleeding, dysphonia and aspiration pneumonia can be the initial symptoms in the case of rupture of the pexy.
FEES, neck 3D CT scan, or VFSS can help in confirming the suspicion of a pexy line disorder, although in many cases direct observation during intraoperative revision surgery is necessary for definite diagnosis.
Acknowledgements
All of the authors have read and approved the manuscript. The present authors have no financial relationship to disclose.
References
- 1.Alonso JM. Conservative surgery of cancer of the larynx. Trans Am Acad Ophthalmol Otolaryngol. 1947;51:633–642. [PubMed] [Google Scholar]
- 2.Majer EH, Rieder W. Technique de laryngectomie permettant de conserver la permeabilité respiratoire (la crico-hyoidopexie) Ann Otolaryngol. 1959;76:677–681. [Google Scholar]
- 3.Piquet JJ, Desaulty A, Decroix G. La crico-hyoido-pexie: technique operatoire et resultat fonctionels. Ann Otolaryngol Chir Cervicofac. 1974;91:681–686. [PubMed] [Google Scholar]
- 4.Labayle J, Bismuth R. La laryngectomie totale avec reconstruction. Ann Otolaryngol Chir Cervicofac. 1971;88:219–228. [PubMed] [Google Scholar]
- 5.Rizzotto G, Succo G, Lucioni M, et al. Subtotal laryngectomy with tracheohyoidopexy: a possible alternative to total laryngectomy. Laryngoscope. 2006;116:1907–1917. doi: 10.1097/01.mlg.0000236085.85790.d5. [DOI] [PubMed] [Google Scholar]
- 6.Calearo CV, Teatini G. Horizontal glottectomy. Laryngoscope. 1978;88:1529–1535. doi: 10.1002/lary.1978.88.9.1529. [DOI] [PubMed] [Google Scholar]
- 7.Carron MA, Kim SA, Sawhney R, et al. Airway obstruction by granulation tissue within a fenestrated tracheotomy tube: case report. Ear Nose Throat J. 2006;85:54–55. [PubMed] [Google Scholar]
- 8.Siddharth P, Mazzarella L. Granuloma associated with fenestrated tracheostomy tubes. Am J Surg. 1985;150:279–280. doi: 10.1016/0002-9610(85)90138-2. [DOI] [PubMed] [Google Scholar]
- 9.Mostert MJ, Stuart H. Subcutaneous emphysema caused by a fenestrated tracheostomy tube. Anaesthesia. 2001;56:191–192. doi: 10.1046/j.1365-2044.2001.01870-16.x. [DOI] [PubMed] [Google Scholar]
- 10.Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2:216–219. doi: 10.1007/BF02414429. [DOI] [PubMed] [Google Scholar]
- 11.Martin-Harris B, Jones B. The videofluorographic swallowing study. Phys Med Rehabil Clin N Am. 2008;19:769–785. doi: 10.1016/j.pmr.2008.06.004. viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujii N, Inamoto Y, Saitoh E, et al. Evaluation of swallowing using 320-detector-row multislice CT. Part I: single- and multiphase volume scanning for three-dimensional morphological and kinematic analysis. Dysphagia. 2011;26:99–107. doi: 10.1007/s00455-009-9268-2. [DOI] [PubMed] [Google Scholar]
- 13.Bely-Toueg N, Halimi P, Laccourreye O, et al. Normal laryngeal CT findings after supracricoid partial laryngectomy. AJNR Am J Neuroradiol. 2001;22:1872–1880. [PMC free article] [PubMed] [Google Scholar]
- 14.Laccourreye O, Brasnu D, Laccourreye L, et al. Ruptured pexis after supracricoid partial laryngectomy. Ann Otol Rhinol Laryngol. 1997;106:159–162. doi: 10.1177/000348949710600212. [DOI] [PubMed] [Google Scholar]
- 15.Decotte A, Serrano E, Woisard V, et al. Les lâchages de pexie dans les laryngectomies partielles supracricoidiennes: à propos de 5 cas. Rev Laryngol Otol Rhinol (Bord) 2009;130:225–229. [PubMed] [Google Scholar]
- 16.Rizzotto G, Crosetti E, Lucioni M, et al. Subtotal laryngectomy: outcomes of 469 patients and proposal of a comprehensive and simplified classification of surgical procedures. Eur Arch Otorhinolaryngol. 2012;269:1635–1646. doi: 10.1007/s00405-012-1928-4. [DOI] [PubMed] [Google Scholar]
- 17.Kasapoğlu F, Erişen L, Erdoğan C. Suspicion of cricohyoidopexy line rupture after supracricoid partial laryngectomy and the value of computed tomography to exclude this complication. Kulak Burun Bogaz Ihtis Derg. 2008;18:179–181. [PubMed] [Google Scholar]
- 18.Naudo P, Laccourreye O, Weinstein G, et al. Complications and functional outcome after supracricoid partial laryngectomy with cricohyoidoepiglottopexy. Otolaryngol Head Neck Surg. 1998;118:124–129. doi: 10.1016/S0194-5998(98)70388-2. [DOI] [PubMed] [Google Scholar]
- 19.Laudadio P, Presutti L, Dall'olio D, et al. Supracricoid laryngectomies: long-term oncological and functional results. Acta Otolaryngol. 2006;126:640–649. doi: 10.1080/00016480500469024. [DOI] [PubMed] [Google Scholar]
- 20.Bergamini G, Alicandri-Ciufelli M, Molteni G, et al. Rehabilitation of swallowing with polydimethylsiloxane injections in patients who underwent partial laryngectomy. Head Neck. 2009;31:1022–1030. doi: 10.1002/hed.21064. [DOI] [PubMed] [Google Scholar]