Abstract
Introduction
Until recently, health care systems in the United States often lacked a unified approach to prevent and manage chronic disease. Recent efforts have been made to close this gap through various calls for increased collaboration between public health and health care systems to better coordinate provision of services and programs. Currently, the extent to which the public health workforce has responded is relatively unknown. The objective of this study is to explore health care system collaboration efforts and activities among a population-based sample of state public health practitioners.
Methods
During spring 2013, a national survey was administered to state-level chronic disease public health practitioners. Respondents were asked to indicate whether or not they collaborate with health care systems. Those who reported “yes” were asked to indicate all topic areas in which they collaborate and provide qualitative examples of their collaborative work.
Results
A total of 759 respondents (84%) reported collaboration. Common topics of collaboration activities were tobacco, cardiovascular health, and cancer screening. More client-oriented interventions than system-wide interventions were found in the qualitative examples provided. Respondents who collaborated were also more likely to use the Community Guide, use evidence-based decision making, and work in program areas that involved secondary, rather than primary, prevention.
Conclusion
The study findings indicate a need for greater guidance on collaboration efforts that involve system-wide and cross-system interventions. Tools such as the Community Guide and evidence-based training courses may be useful in providing such guidance.
Introduction
Effective prevention and management of chronic conditions is a high priority — chronic disease affects nearly 1 in 2 adults in the United States and accounts for 75% of our nation’s health care costs (1,2). Efforts to reduce the burden of chronic disease have been fragmented, with different health care systems working independently to achieve outcomes (3).
Increased collaboration among different health care systems to prevent and manage chronic diseases has been recently prioritized (3–6). In 2012, for example, the Institute of Medicine (IOM) published a national report, Primary Care and Public Health: Exploring Integration to Improve Population Health, which recognized need and identified opportunities for health care to improve population health (3). The Patient Protection and Affordable Care Act (ACA) emerged in the IOM’s report as a key vehicle for health systems to achieve increased collaboration.
The Centers for Disease Control and Prevention (CDC) and the Public Health Accreditation Board (PHAB) have reinforced the vision for more unified chronic disease approaches across health care systems. Two of CDC’s 4 key chronic disease practice domains call on public health to improve the services provided by health care systems (4). Health care system collaboration is now required by PHAB for health departments’ accreditation, and the movement toward collaborative chronic care continues to grow (5).
However, despite the growing emphasis on these issues, few data are available on how the public health workforce has responded to the call for greater collaboration. The objective of our study is to bridge this gap by using a mixed methods study with 2 goals: 1) to explore the patterns and correlates of public health’s collaboration with health care systems from the perspective of state public health practitioners, and 2) to compare practitioners’ collaborations with those recommended by CDC.
Methods
During spring 2013, a national online survey was administered to state-level public health practitioners whose primary work was preventing and managing chronic diseases. Human subject approval was obtained from the Institutional Review Board of Washington University in St Louis.
State health department program managers and staff from all 50 states and the District of Columbia were invited to participate in the survey if they primarily worked in program areas of cancer, tobacco, physical activity, nutrition, obesity prevention, diabetes prevention, and cardiovascular health. Eligible invitees were identified by searching state health department websites and member lists obtained from partner organizations. Eligibility of invitees was verified by telephone as needed. A total of 1,169 eligible participants were invited to complete the survey through a personalized e-mail invitation. Respondents were offered a $20 Amazon.com gift card on completion of the survey.
Previous research and 5 rounds of advisory input from an international team were used to construct the initial survey instrument (7–9). The survey was refined through cognitive response testing with 11 former chronic disease practitioners, and a reliability test–retest sample of 75 current state-level chronic disease practitioners was used to establish internal consistency among most of the 68 items included in the final survey (Cronbach’s α ≥ .70). The final 15-minute survey was programmed into Qualtrics survey software (Qualtrics, LLC) for online administration. Further description of survey development and data collection are published elsewhere (9), and a copy of the full questionnaire is available on request.
Measures
Although the survey’s content was designed to explore a multitude of purposes, our study focused on characteristics of state health department practitioners and their program or work unit’s collaborations with health care systems, their personal use of evidence-based decision making (EBDM), and their personal use of the US Preventive Services Task Force’s Community Guide. Items used to assess these concepts are described below.
Characteristics of state health department practitioners were assessed through basic demographic questions, which included items such as age, sex, years worked in public health, and the main program area in which respondents worked. All respondents were asked to indicate their personal use of EBDM within their work by using a single item, with a 7-point Likert scale ranging from “strongly disagree” to “strongly agree.” The concept of EBDM was defined for respondents as “prioritizing issues and implementing interventions based on sound science combined with community engagement, sound management, and evaluation” (10).
Respondents were asked to report their use of the Community Guide. Response options included “yes, often,” “yes, sometimes,” “no,” and “I'm not familiar with the Community Guide.”
Health care system collaboration, the primary outcome for our study, was assessed through 3 items. Respondents were asked, “Does your program or work unit collaborate with health care systems that include hospitals, outpatient clinics, and/or Federally-qualified health centers?” Response options included “yes,” “no,” and “I’m not sure.” Respondents who selected “yes” were asked to indicate topic areas of collaboration activities from a provided list of options (Figure 1). Additionally, respondents who reported collaboration were asked to type an example of their collaborative work into a text box.
Figure 1.
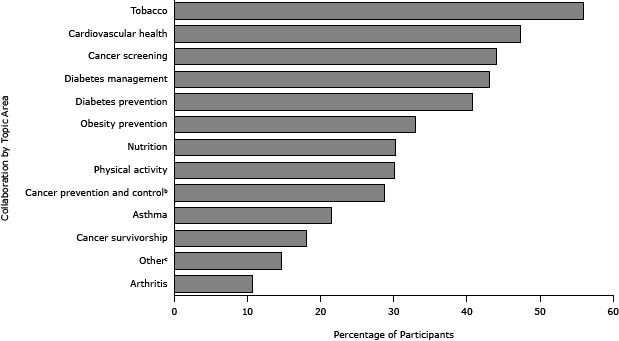
Self-reported topic areas for health care system collaboration (N = 759). Participants in a 2013 national survey of state health department chronic disease prevention staff who reported collaboration with health care systems were asked to indicate all topic areas of collaboration from a provided list. Percentages total more than 100% because participants could choose all topic areas that applied. Cancer prevention and control programs do not include cancer screening. “Other” areas commonly self-reported were maternal–child health, breast-feeding, cancer registry, and adolescent health.
| Topic Area of Collaboration Activity | %a |
|---|---|
| Tobacco | 55.9 |
| Cardiovascular health | 47.3 |
| Cancer screening | 44.0 |
| Diabetes management | 43.1 |
| Diabetes prevention | 40.7 |
| Obesity prevention | 33.0 |
| Nutrition | 30.2 |
| Physical activity | 30.1 |
| Cancer prevention and control | 28.7 |
| Asthma | 21.5 |
| Cancer survivorship | 18.0 |
| Other | 14.7 |
| Arthritis | 10.7 |
Data analysis
Descriptive and multivariate analyses were conducted using IBM SPSS Statistics 21 to explore frequencies and associations with health care system collaboration. “Health care system collaboration,” “use of EBDM,” and “use of Community Guide” were recoded into binary variables. Significance was set at P < .05.
For multivariate analyses, differences in health care system collaboration were examined through bivariate analyses that used both survey data and state characteristics (11–13), and the bivariate results were used to construct logistic regression models. Variables with moderate to high proportions of shared variance were not included in the model to reduce possible effects of multicollinearity (Pearson’s r > .20). The final model included “program area,” “use of EBDM,” and “use of Community Guide” and met all model assumptions.
Qualitative methods were used to code common themes among respondents’ health care collaboration examples. Common themes were grouped into 14 categories based on the Chronic Care Model, a 6-component framework that improves chronic care and associated health outcomes (Figure 2) (14). Two authors (L.E., R.J.) independently coded the 642 collaboration examples by using QSR NVivo 10 software (QSR International Pty Ltd) with high average inter-rater agreement (κ = .86).
Figure 2.
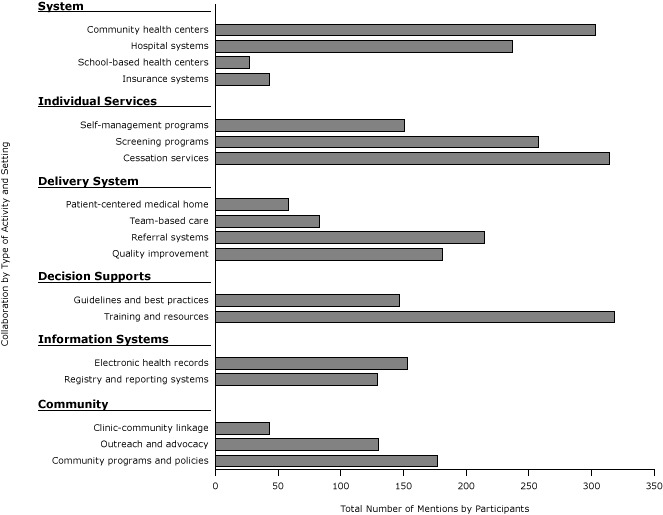
Collaboration examples by common settings and activities, derived from qualitative data (N = 642). Participants in a 2013 national survey of state health department chronic disease prevention staff who reported collaboration with health care systems were asked to provide an example of their collaborative work.
| Type of Setting or Activity | n |
|---|---|
| Community health centers | 303 |
| Hospital systems | 237 |
| School-based health centers | 27 |
| Insurance systems | 43 |
| Self-management programs | 151 |
| Screening programs | 258 |
| Cessation services | 314 |
| Patient-centered medical home | 58 |
| Team-based care | 83 |
| Referral systems | 215 |
| Quality improvement | 181 |
| Guidelines and best practices | 147 |
| Training and resources | 318 |
| Electronic health records | 153 |
| Registry and reporting systems | 129 |
| Clinic-community linkage | 43 |
| Outreach and advocacy | 130 |
| Community programs and policies | 177 |
Results
We asked respondents to answer yes or no to the health care system collaboration survey item (Table 1). Of the 759 (84.0%) respondents who indicated collaboration with health care systems, respondents with more years worked in their specific health agency, their current position, and generally in public health were more likely to report collaboration (P = .006, P = .02, P = .01, respectively). In contrast, collaboration did not differ by respondents’ sex, age group, degree type (clinical vs nonclinical), or educational attainment.
Table 1. Participant and State Characteristics by Health Care Collaboration in a National Sample of US State Health Department Staff in Chronic Disease Prevention, 2013 (N = 904).
| Characteristics | Total Sample (N = 904) | Did Not Report Collaboration (N = 144) | Reported Collaboration (N = 759)a | P Valueb |
|---|---|---|---|---|
|
n (%) | ||||
| Program area | ||||
| Cancer prevention and control | 145 (16.1) | 6 (4.2) | 139 (18.3) | <.001 |
| Tobacco control | 161 (17.8) | 30 (20.8) | 131 (17.3) | |
| Obesity, physical activity, nutrition | 132 (14.6) | 45 (31.3) | 87 (11.5) | |
| Cardiovascular health and diabetes | 151 (16.7) | 6 (4.2) | 145 (19.1) | |
| Multiple areasc | 255 (28.2) | 38 (26.4) | 217 (28.6) | |
| Other areasd | 59 (6.5) | 19 (13.2) | 40 (5.3) | |
| Sex | ||||
| Female | 726 (80.4) | 108 (75.0) | 618 (81.4) | .08 |
| Male | 177 (19.6) | 36 (25.0) | 141 (18.6) | |
| Age, y | ||||
| 20–39 | 277 (30.8) | 52 (36.4) | 225 (29.8) | .07 |
| 40–49 | 248 (27.6) | 46 (32.2) | 202 (26.8) | |
| 50–59 | 246 (27.3) | 29 (20.3) | 217 (28.7) | |
| ≥60 | 127 (14.1) | 16 (11.2) | 111 (14.7) | |
| Use of Community Guide | ||||
| Often/Sometimes | 718 (80.0) | 92 (63.9) | 626 (83.0) | <.001 |
| No/Don’t know | 180 (20.0) | 52 (36.1) | 128 (17.0) | |
| Use of EBDMe in work | ||||
| Agree | 781 (87.7) | 114 (80.9) | 667 (88.9) | .007 |
| Do not agree | 110 (12.3) | 27 (19.9) | 83 (11.1) | |
| Educational level | ||||
| Master’s degree or higher | 632 (70.0) | 95 (66.0) | 537 (70.8) | .25 |
| No master’s degree | 271 (30.0) | 49 (34.0) | 222 (29.2) | |
| Degree type | ||||
| Clinical degreef | 177 (19.8) | 26 (18.1) | 151 (20.1) | .57 |
| Nonclinical degree | 717 (80.2) | 118 (81.9) | 599 (79.9) | |
| Years worked at agency, mean (SD) | 9.9 (7.9) | 8.3 (7.0) | 10.2 (8.0) | .006 |
| Years worked in position, mean (SD) | 4.9 (4.9) | 4.2 (3.9) | 5.1 (5.0) | .02 |
| Years worked in public health, mean (SD) | 14.7 (9.2) | 12.9 (8.8) | 15.0 (9.3) | .01 |
| Chronic disease funding per capitag, mean (SD) | 1.5 (1.2) | 1.3 (1.1) | 1.5 (1.2) | .04 |
| Total cancer mortality rate per 1000h, mean (SD) | 14.1 (14.1) | 18.2 (17.5) | 13.3 (13.3) | .002 |
| Percentage of state uninsured (%)i , mean (SD) | 14.4 (4.1) | 15.1 (4.3) | 14.2 (4.1) | .02 |
Abbreviations: EBDM, evidence-based decision making; SD, standard deviation.
Because of missing data, not all categories total 144 and 759. Percentages represent valid nonmissing cases.
P values for continuous variables were calculated by t tests, and χ2 tests were conducted for binary variables to test significance.
Multiple areas included generalists or practitioners whose primary work spanned several chronic disease program areas (eg, epidemiologists, chronic disease directors).
Other areas included arthritis, school health, oral health, and other, less commonly mentioned areas.
EBDM is defined as “prioritizing issues and implementing interventions based on sound science combined with community engagement, sound management, and evaluation” (10).
Clinical degrees include doctor of medicine, doctor of osteopathic medicine, doctor of dental surgery, registered dietitian, certified diabetes educator, and all nursing degrees (registered nurse, licensed practical nurse, bachelor of science in nursing, advanced practice registered nursing, or “other nursing”).
Data from Centers for Disease Control and Prevention, Justification of Estimates for Appropriations Committees. Totaled from 4 chronic disease categories: breast and cervical cancer, tobacco, comprehensive cancer, diabetes prevention (11).
Data from National Cancer Institute and Centers for Disease Control and Prevention, State Cancer Profiles (12).
Data from US Census Bureau American Community Survey, 2010 American Community Survey 1-Year Estimates (13).
A higher percentage (83%) of respondents who reported collaboration reported use of EBDM in their work and use of the Community Guide compared with those who did not report collaboration (P = .007 and P < .001, respectively). Health system collaboration was associated with the main program area in which respondents worked and was more often reported among those working across multiple program areas (28.6%), in cardiovascular health and diabetes (19.1%), or in cancer prevention and control (18.3%) compared with other areas (P < .001).
Bivariate analyses also indicated significant differences in health care collaboration by state characteristics. Respondents from states with higher chronic disease funding dollars per capita, lower cancer mortality rates, and lower percentage of population uninsured were more likely to report collaboration (P = .04, P = .002, P = .02, respectively).
Self-reported topics of collaboration activities from the 759 respondents who reported collaboration are displayed in Figure 1. Tobacco cessation was the most commonly reported topic area of collaboration (55.9%), followed by cardiovascular health (47.2%), cancer screening (44.0%), and diabetes management (43.1%). Common “other” responses included maternal-child health, breastfeeding, and cancer registry.
We grouped the 642 qualitative examples of self-reported collaboration by type of collaborative activity and health system settings (Figure 2). Respondents most frequently reported collaborative work with community health centers (47.2%) and hospital systems (36.9%). Commonly mentioned collaborative activities were training providers and providing resources such as toolkits (49.5%), tobacco cessation services such as quitline referrals and support for cessation programs (48.9%), and general cancer screening services (40.2%). The least common collaboration activities mentioned included clinic–community linkages (6.7%), support for Patient-Centered Medical Homes (9.0%), and promotion of team-based care (eg, promotion of patient navigators) (12.9%). We list respondents’ comments about these and other collaborations (Box).
Box. Health Care Collaboration Among State Health Department Chronic Disease Prevention Staff From All 50 US States That Reported Collaboration With Health Care Systems, Spring 2013 (N = 642).
| Activity | Collaboration Examples |
|---|---|
| Individual services | “The program reviews the Certifications of the 32 Diabetes Self-Management Training (DSMT) Sites, collects sites’ CQI objectives, and DSMT participant goals (set and accomplished). Oversees and administers the New Instructor Program for all DSMT instructors in the State.” |
| Delivery system | “We have implemented a program that assists primary care health care practices to implement components of the chronic care model to become NCQA-recognized patient-centered medical homes.” |
| “[Changed] EHR so that a fully electronic process for identifying, offering assistance, and referring those that wanted assistance to quit tobacco was developed. Further, the [cessation] counselor treating the patient electronically sends a follow up report back to the referring provider.” | |
| Decision supports | “Health systems change and infrastructure building to ensure patients are screened for CRC. Examples include office policy development, building EHR cancer registries, and developing patient reminders.” |
| “[State] set up a Chronic Disease Collaborative that involves members across various sectors including health care systems to address common goals, objectives, and strategies. This opportunity allows members to collaborate and share information and resources.” | |
| Information systems | “We work with the largest health insurance provider to implement a free clinical information system. This free Web-based system . . . allows the providers to monitor [risk factors] . . . see at a glance missed care opportunities and can generate letters to send to patients to encourage them to call the office for an appointment. We currently have over 70% of the state providers enrolled in the system.” |
| “We are currently working on a collaborative effort to build a network of electronic records access to help improve the surveillance aspects of chronic disease in [state] while linking this with Medicaid. There is a lot of coordination happening to adopt this in our state.” | |
| Community | “A centralized referral system has been implemented with patient navigation services to assist the patients referred from the practices to [12 community evidence-based lifestyle and disease management programs].” |
Abbreviations: CQI, continuous quality improvement; CRC, colorectal cancer; EHR, electronic health record; NCQA, National Committee for Quality Assurance.
Accounting for multivariate associations, participants who used the Community Guide were 2.6 times as likely to report collaboration with health care systems as those who did not use the Community Guide (Table 2) (P < .001). Similarly, participants who used EBDM were twice as likely to report collaboration as those who did not use EBDM (P = .01). The association between collaboration and the main program area in which respondents worked remained robust after adjusting for use of EBDM and the Community Guide. Compared with those working in obesity, physical activity, or nutrition, participants working in cancer prevention and control were 11.9 times as likely to report collaboration (P < .001), and those working in cardiovascular health and diabetes were 14.5 times as likely to report collaboration with health systems (P < .001). Although bivariate results indicated significant associations between state characteristics and health care system collaboration, practitioners’ likelihood of collaborating was not significantly influenced by state characteristics after adjusting for clustering effects by state membership.
Table 2. Health Care Collaboration in a National 2013 Sample of State Health Department Chronic Disease Prevention Staff (N = 904)a .
| Characteristics | OR (95% CI) | P Valueb |
|---|---|---|
| Program area | ||
| Obesity, physical activity, nutrition | 1 [Reference] | — |
| Tobacco control | 2.3 (1.3–3.9) | .004 |
| Cancer prevention and control | 11.9 (4.8–29.6) | <.001 |
| Cardiovascular health and diabetes | 14.5 (5.8–36.0) | <.001 |
| Multiple areas | 3.1 (1.8–5.1) | <.001 |
| Other areas | 1.2 (0.6–2.3) | .67 |
| Use of Community Guide | ||
| No/Don’t knowc | 1 [Reference] | — |
| Yes | 2.6 (1.7–4.0) | <.001 |
| Use of EBDM c in work | ||
| Do not agree | 1 [Reference] | — |
| Agree | 2.0 (1.2–3.3) | .01 |
Abbreviations: OR, odds ratio; CI, confidence interval; —, no P values for reference categories; EBDM, evidence-based decision making.
Multivariate odds ratios for health care collaboration likelihood are adjusted for program area, use of evidence-based decision making, and use of the Community Guide.
Logistic regression model used to determine P values of independent variables based on the Wald test for significance.
EBDM is defined as “prioritizing issues and implementing interventions based on sound science combined with community engagement, sound management, and evaluation” (10).
Discussion
The 2012 IOM report highlighted a key challenge: few examples of successful collaborative care between public health and health care systems on a large scale are known (3). Our study aimed to address this challenge by collecting and analyzing a nationwide sample of state health department practitioners’ collaborative efforts with health care systems to prevent and manage chronic disease. Our findings indicate that the public health workforce has responded to the call to action — most state health department practitioners in chronic disease prevention report that their work unit or program area collaborates with health care systems.
Standards set by CDC and PHAB may promote collaborations between public health and health care systems. Of the 4 practice domains in CDC’s National Center for Chronic Disease Prevention and Health Promotion, 2 require public health’s collaboration with health care systems. Domain 3 states that public health should improve the quality and accessibility of preventive services offered by health systems through use of health information technology, evidence-based chronic care delivery, and other interventions that align with the Community Guide (4). Domain 4, community-clinical linkages, encourages public health to facilitate cross-system referrals between clinics and communities to ensure that people who have or are at risk for chronic diseases have access to CDC-recommended programs and services to help prevent or manage their chronic conditions (4).
The PHAB echoes CDC’s recommendations. The accreditation of health departments has been referred to as one of the most important initiatives in transforming the performance and practice of public health practitioners (15). Twelve domains outline required actions for state health department accreditation. Domain 7 specifically requires health departments to link with health care systems through collaborative processes to improve health care systems’ capacity and provision of preventive services (5).
In general, respondents mentioned types of collaboration activities recommended by CDC and PHAB. However, findings from this study indicate that state health departments may emphasize collaborations that focus on client-oriented services over changes to delivery and information systems. For example, respondents mentioned tobacco cessation and cancer screening services more frequently than electronic health records (EHRs) and referral systems.
Similar findings were published in a recent report of CDC’s colorectal cancer screening programs. Hannon and colleagues found that state health departments funded to increase screening among underserved populations were more likely to use client-oriented interventions (eg, small media) than interventions involving system-wide procedures such as provider reminder and recall systems (16). They also found that most grantees (96%) worked with health systems on small media interventions, yet only 32% of grantees reported using automated provider reminder systems (16). All of the 32% who successfully implemented provider reminders reported using EHRs. Grantees also noted difficulty in working with EHRs as a barrier to implementation of CDC-recommended interventions (16).
Further exploration of the relationship between public health’s implementation of evidence-based interventions and health care systems’ EHR capacity may be useful. Although use of EHRs increases the number of preventive services offered in clinical settings and improves health outcomes, they are underutilized (17–21). Maylahn and colleagues recently recommended collaborations involving EHRs to help public health and health care systems achieve common goals (22). More research is needed to identify collaborations that increase EHR capacity and implementation of recommended interventions.
Our study found that public health practitioners who reported use of the Community Guide and use of EBDM were significantly more likely to report collaboration with health care systems. Although the direction of the relationship cannot be determined from these cross-sectional data, our findings suggest that CDC’s promotion of the Community Guide through grant funding and practice domains is valuable as a potential guide to collaborative work.
A twofold increase in health care system collaboration was found among practitioners who used EBDM, which warrants exploring how training programs that teach EBDM competencies might influence collaboration activities. Courses in evidence-based public health teach practitioners a range of skills that have been shown to promote use of EBDM (23,24). Such courses may be used as training resources for collaborative activities.
Although no interactions were found between respondents’ program area, use of the Community Guide, and use of EBDM, we found differences in respondents’ likelihood to collaborate with health systems based on the main program area in which individuals worked. Program areas with more focus on secondary prevention (eg, cancer, tobacco cessation, cardiovascular health and diabetes) were more likely to collaborate across sectors. Some of these findings were expected. The Community Guide has more systematic guidance on clinically focused interventions for practitioners who work in secondary prevention compared with obesity, physical activity, and nutrition (25). More work is needed to identify effective interventions and define how primary prevention programs can strengthen cross-sector collaborations.
Recommendations
Findings from this study support the need for better guidance on collaborations that support health system infrastructure, and for increased collaboration guidance for additional chronic disease program areas. Although we found that most state health departments collaborate with health care systems, much work remains to be done. Patients receive only about half of the recommended clinical preventive services in primary care settings (16,26,27). Even with guidance from CDC and PHAB on evidence-based collaborative approaches, barriers inhibit state health departments’ use of such approaches. Lack of funding remains a common barrier (7,28). A key purpose of the IOM report was to identify potential funding avenues for collaboration. The IOM highlighted the ACA as a pathway for funding. Although Title IV of the ACA contains the most direct public health prevention funding opportunities, several ACA provisions, such as Patient-Centered Medical Homes and Accountable Care Organizations, allow for public health to invest in clinical services that promote more comprehensive chronic care (29). With combined efforts and leveraged resources, public health can work with health systems through these provisions to achieve common goals. In general, more research is needed to understand how state health departments use opportunities provided through the ACA to collaborate.
Results of collaborative work may guide future US collaborations. A scoping review from Canada on public health and health care collaboration validates benefits that include reduced hospital and emergency department use, improved chronic care delivery, increased identification of people at risk for chronic disease, and increased access to care (30). Such examples show that collaboration is both feasible and economically viable.
Because the survey was self-reported, we were unable to capture the quality and scope of responses and collaboration activities. For example, respondents were asked to report the collaboration of their program area or work unit, which makes it difficult to assess their personal involvement in collaborations. Self-reported survey data also make it difficult to delineate respondents’ primary program area; some between program areas may overlap, depending on different state health department structures. Respondents were not given a thorough definition of “health care system collaboration,” which may have caused interpretation inconsistencies among respondents. Lastly, the directionality of associations found cannot be determined because of the cross-sectional study design. Despite these limitations, our study contributes to the literature by identifying achievements and gaps in collaborations reported by a nationwide sample of public health practitioners and by providing next steps for collaboration guidance.
The increase in chronic diseases and the emphasis on collaboration from CDC and PHAB increase the likelihood that cross-sector efforts to prevent and manage chronic disease will grow. Systematic guidance is needed to identify collaboration activities that yield high public health impact and improved delivery systems for chronic care. Next steps may include comparisons of different types of cross-sector collaborations and their subsequent impact on system changes. Evaluation is also needed to better prioritize which types of collaboration activities should be the main focus of state health departments. Further research to fill the gaps identified by this study may help ensure that future collaborations result in improved systems, better care, and an overall reduced burden of chronic disease.
Acknowledgments
This study was funded by the National Cancer Institute of the National Institutes of Health (NIH) under award no. R01CA160327. This article is a product of a Prevention Research Center and was also supported by cooperative agreement no. U48/DP001903 from CDC. The findings and conclusions in this article are those of the authors and do not necessarily represent the official positions of NIH or CDC.
We appreciate the collaboration on this study with Vicki Benard, PhD, and Marcus Plescia, MD, MPH, at the Division of Cancer Prevention and Control, Centers for Disease Control and Prevention. We thank John W. Robitscher, MPH, National Association of Chronic Disease Directors, for his support of this study. We thank Leslie Best, consultant and retired chronic disease director, Pennsylvania Department of Health, for her perspectives on survey revisions and CDC initiatives. We are grateful to colleagues at the Prevention Research Center in St Louis, which is co-housed at the Brown School, Washington University in St Louis and College of Public Health and Social Justice, St Louis University: Jenine K. Harris, PhD, Katherine A. Stamatakis, PhD, MPH, and Elizabeth A. Baker, PhD, MPH, for their survey development expertise; Sonia Sequeira, MSW/MPH for her help with data collection and management while a graduate research assistant; and Linda Dix and Mary Adams for administrative support.
Footnotes
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors' affiliated institutions.
Suggested citation for this article: Elliott L, McBride TD, Allen P, Jacob RR, Jones E, Kerner J, et al. Health Care System Collaboration to Address Chronic Diseases: A Nationwide Snapshot From State Public Health Practitioners. Prev Chronic Dis 2014;11:140075. DOI: http://dx.doi.org/10.5888/pcd11.140075.
References
- 1. Institute of Medicine. Living well with chronic illness: a call for public health action. Washington (DC): National Academies Press; 2012. http://www.iom.edu/Reports/2012/Living-Well-with-Chronic-Illness.aspx. Accessed November 26, 2013.
- 2. Wu SY, Green A. Projection of chronic illness prevalence and cost inflation. Santa Monica (CA): RAND; 2000. [Google Scholar]
- 3. Institute of Medicine. Primary care and public health: exploring integration to improve population health. Washington (DC): National Academies Press; 2012. http://www.iom.edu/Reports/2012/Primary-Care-and-Public-Health.aspx. Accessed November 26, 2013. [PubMed]
- 4.Chronic disease prevention and health promotion domains. National Center for Chronic Disease and Health Promotion. Centers for Disease Control and Prevention; 2012. http://www.cdc.gov/chronicdisease/about/foa/docs/Four-Domains-Nov2012.pdf. Accessed December 2, 2013.
- 5.Standards and measures: version 1.0. Public Health Accreditation Board; 2011. http://www.phaboard.org/wp-content/uploads/PHAB-Standards-and-Measures-Version-1.0.pdf. Accessed December 4, 2013.
- 6. Stine NW, Chokshi DA, Gourevitch MN. Improving population health in US cities. JAMA 2013;309(5):449–50. 10.1001/jama.2012.154302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jacobs JA, Dodson EA, Baker EA, Deshpande AD, Brownson RC. Barriers to evidence-based decision making in public health: a national survey of chronic disease practitioners. Public Health Rep 2010;125(5):736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jacobs JA, Jones E, Gabella BA, Spring B, Brownson RC. Tools for implementing an evidence-based approach in public health practice. Prev Chronic Dis 2012;9:E116. http://www.cdc.gov/pcd/issues/2012/11_0324.htm. Accessed April 18, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Allen P, Sequeira S, Jacob RR, Hino AA, Stamatakis KA, Harris JK, et al. Promoting state health department evidence-based cancer and chronic disease prevention: a multi-phase dissemination study with a cluster randomized trial component. Implement Sci 2013;8:141. 10.1186/1748-5908-8-141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kohatsu ND, Robinson JG, Torner JC. Evidence-based public health: an evolving concept. Am J Prev Med 2004;27(5):417–21. [DOI] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. Justification of estimates for appropriations committees. Atlanta (GA): US Department of Health and Human Services; 2013. http://www.cdc.gov/fmo/topic/Budget%20Information/appropriations_budget_form_pdf/FY2013_CDC_CJ_Final.pdf. Accessed October 15, 2013.
- 12.State cancer profiles. National Cancer Institute and Centers for Disease Control and Prevention; 2010. http://statecancerprofiles.cancer.gov/. Accessed July 1, 2013.
- 13.US Census Bureau American Community Survey. 2010. American Community Survey 1-year estimates; generated using American FactFinder. http://factfinder2.census.gov. Accessed July 1, 2013.
- 14. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28(1):75–85. 10.1377/hlthaff.28.1.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Riley WJ, Bender K, Lownik E. Public health department accreditation implementation: transforming public health department performance. Am J Public Health 2012;102(2):237–42. 10.2105/AJPH.2011.300375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hannon PA, Maxwell AE, Escoffery C, Vu T, Kohn M, Leeman J, et al. Colorectal Cancer Control Program grantees’ use of evidence-based interventions. Am J Prev Med 2013;45(5):644–8. 10.1016/j.amepre.2013.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jamoom E, Beatty P, Bercovitz A, Woodwell D, Palso K, Rechtsteiner E. Physician adoption of electronic health record systems: United States, 2011. NCHS Data Brief 2012;98:1-8. [PubMed] [Google Scholar]
- 18. Frimpong JA, Jackson BE, Stewart LM, Singh KP, Rivers PA, Bae S. Health information technology capacity at federally qualified health centers: a mechanism for improving quality of care. BMC Health Serv Res 2013;13:35. 10.1186/1472-6963-13-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dexheimer JW, Talbot TR, Sanders DL, Rosenbloom ST, Aronsky D. Prompting clinicians about preventive care measures: a systematic review of randomized controlled trials. J Am Med Inform Assoc 2008;15(3):311–20. 10.1197/jamia.M2555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA 2005;293(10):1223–38. 10.1001/jama.293.10.1223 [DOI] [PubMed] [Google Scholar]
- 21. Calman N, Hauser D, Lurio J, Wu WY, Pichardo M. Strengthening public health and primary care collaboration through electronic health records. Am J Public Health 2012;102(11):e13–8. 10.2105/AJPH.2012.301000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maylahn C, Fleming D, Birkhead G. Health departments in a brave new world. Prev Chronic Dis 2013;10:E41. http://www.cdc.gov/pcd/issues/2013/13_0003.htm. Accessed December 4, 2013. 10.5888/pcd10.130003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health 2009;30:175–201. 10.1146/annurev.publhealth.031308.100134 [DOI] [PubMed] [Google Scholar]
- 24. Dreisinger M, Leet TL, Baker EA, Gillespie KN, Haas B, Brownson RC. Improving the public health workforce: evaluation of a training course to enhance evidence-based decision making. J Public Health Manag Pract 2008;14(2):138–43. 10.1097/01.PHH.0000311891.73078.50 [DOI] [PubMed] [Google Scholar]
- 25. Centers for Disease Control and Prevention. Guide to community preventive services. The Task Force on Community Preventive Services. http://www.thecommunityguide.org. Accessed December 9, 2013.
- 26. Porterfield DS, Hinnant LW, Kane H, Horne J, McAleer K, Roussel A. Linkages between clinical practices and community organizations for prevention: a literature review and environmental scan. Am J Public Health 2012;102(Suppl 3):S375–82. 10.2105/AJPH.2012.300692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003;348(26):2635–45. 10.1056/NEJMsa022615 [DOI] [PubMed] [Google Scholar]
- 28. Steele CB, Rose JM, Chovnick G, Townsend JS, Stockmyer CK, Fonseka J, et al. Use of evidence-based practices and resources among comprehensive cancer control programs. J Public Health Manag Pract 2014. Epub ahead of print. 10.1097/PHH.0000000000000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gourevitch MN, Cannell T, Boufford JI, Summers C. The challenge of attribution: responsibility for population health in the context of accountable care. Am J Prev Med 2012;42(6):S180–3. 10.1016/j.amepre.2012.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Martin-Misener R, Valaitis R, Wong ST, Macdonald M, Meagher-Stewart D, Kaczorowski J, et al. A scoping literature review of collaboration between primary care and public health. Prim Health Care Res Dev 2012;13(4):327–46. 10.1017/S1463423611000491 [DOI] [PubMed] [Google Scholar]


