Abstract
Positive affect predicts improved glycemic control and longevity in adults with type 2 diabetes. We tested DAHLIA, a self-paced online intervention for type 2 diabetes that teaches positive affect skills such as savoring, gratitude, and acts of kindness. Participants (n=49) were randomized to the 5-week DAHLIA course or an emotion-reporting waitlist control. DAHLIA was understood and accepted by participants and showed good retention (78%). At post-intervention, DAHLIA participants showed a significantly greater decrease in depression than controls (−4.3 vs. +0.6 points on the CES-D, p =.05). Secondary analyses found that this effect was considerably stronger in intervention recipients recruited online than those recruited in person. Intervention recipients recruited online also showed significantly increased positive affect, reduced negative affect, and reduced perceived stress. There were no effects on measures of diabetes-specific efficacy or sense of burden, or preliminary measures of health behaviors. This successful feasibility and efficacy trial provides support for a larger trial focusing more specifically on health behavior.
Positive affect plays a unique adaptive role in psychological and physical health. For people with diabetes, analyses from our research team indicate that positive affect prospectively predicts lower risk of mortality (HR = .86, CI = .78–.96, p = .008) independent of the effect of negative affect [1]. Positive affect is also uniquely associated with better glycemic control in individuals with type 2 diabetes [2] as well as healthy individuals [3].
Exercise, healthy diet, and adherence to medication and other health care recommendations are all paramount to health and well being, particularly among those with a chronic illness such as type 2 diabetes. In observational studies, positive affect is associated with an increased likelihood of physical activity[4,5,6,7] and healthy eating[5,8], as well as a lower likelihood of tobacco use [9,10]. Research on individuals newly diagnosed with HIV indicates that positive affect prospectively predicts greater liklihood of engagement in care and better medication adherence [11]. A series of studies by Isen and colleagues provided a self-affirmation, coping, and positive emotion intervention to several different patient populations and found an overall relationship between positive affect change and health behavior change[12,13,14,15].
We have developed an intervention consisting of skills to increase positive emotion that shows promise for improving psychological well being in people experiencing significant life stress [16,17,18]. The potential benefits include not only the health correlates of positive affect described above, but also improved psychological well-being and coping with life stressors. The intervention is based on revised Stress and Coping Theory[19] and the Broaden-and-Build Theory of positive emotion[20]. These theories describe ways positive emotion supports coping and well-being, such as providing a psychological “time-out” from experiences of distress and helping individuals invest in intellectual and social resources that support future coping.
Positive Affect and Depression
Depression is common in people with type 2 diabetes[21] and is associated with poorer glycemic control, increased symptoms and complications, poorer adherence to exercise and diet recommendations[22], and elevated risk of mortality, over and above the elevations in risk associated with diabetes itself[23].
Interventions based on increasing positive affect and experiences have shown promise as a treatment for depression. A meta-analysis of 25 programs targeting constructs such as gratitude, happiness, and optimism found a medium effect size for relief of depression symptoms (median r = .26), with stronger effects for currently-depressed participants[24]. These positive psychology interventions show effectiveness and durability similar to that of psychotherapy or pharmacotherapy[24]. The focus on pleasurable and rewarding activities of positive psychology interventions resembles the approach of Behavioral Activation (BA) therapies, which have also shown substantial effectiveness at treating depression [25]. Psychological interventions that specifically target depression in samples of people with type 2 diabetes have shown some efficacy (e.g.[26]) but tend to be time intensive for both the patient and the provider, expensive to deliver, and difficult to disseminate in home or other non-clinic settings [27].
Online intervention delivery addresses many of these challenges. Interventions delivered online via computer or mobile format are comparatively inexpensive, easily delivered at multiple locations like clinics, libraries or other public computer terminals, patients’ homes, or even in transit using mobile devices; and are available at times convenient for patients which maximizes the likelihood that the intervention will be accessed. Furthermore, online formats can offer a flexible menu of content to meet individual patient needs and preferences, can include automatic reminders or boosters via email or text, and easily provide ongoing content and support at low cost.
Online interventions for diabetes self-management and depression are feasible and have shown some efficacy [28]|[29] at improving symptoms of depression and some health outcomes. In a meta-analysis, Pal and colleagues[30] found that online diabetes self-management interventions have a small, but statistically significant, effects on HbA1c, diet, and lipids, but do not consistently improve depression symptoms.
Several meta-analyses of internet and computerized interventions, both self-help and clinician-assisted[31,32,33,34], found that internet interventions can reduce symptoms of depression, including among those who might otherwise lack access to treatment. The most successful of these interventions have a variety of components and interactive elements to encourage engagement (including Beating the Blues, which is approved for use by the British National Institute for Health and Clinical Excellence [35,36,37,38,39,40].)
The DAHLIA Intervention
We have developed an intervention (DAHLIA: Developing Affective HeaLth to Improve Adherence) consisting of 8 skills that have been empirically demonstrated to enhance day-to-day positive emotion or adaptive coping. The skills are:
Lesson content and exercises are described in Table 1. The full rationale and development methodology have been described previously [16,17]. Generally, the intervention is based on skills for improving coping or generating positive affect that have been validated in past research. Participants practice one or more of these skills each day. Mindfulness exercises are continued throughout the intervention because we believe they may also help participants recognize and appreciate positive events, even in the context of chronic stress.
Table 1.
Intervention Content
|
Week 1: Positive events |
Noticing small, everyday positive events. Savoring and capitalizing to increase the impact of a positive event. Potential for positive events to reduce stress and increase coping resources, even for people suffering severe difficulties. Depression-related biases that can make noticing or remembering positive events more difficult. The value of scheduling pleasant events. |
| Exercises | Daily positive events journal Daily gratitude journal (continues through all weeks of intervention in order to provide an exercise that is simple and attainable even when other material is challenging) |
|
Week 2: Mindfulness |
Cognitive and emotional benefits of present-focused attention and nonjudgment. Covers both informal mindfulness and brief formal meditation practice. Using present-focused awareness and acceptance to combat rumination. |
| Exercises | Pick an everyday activity to do mindfully 10-minute mindful breathing recorded meditation (continues through all weeks of the intervention in order to support recognizing positive experiences even in stressful contexts) |
|
Week 3: Reappraisal |
Applying positive reappraisal to everyday stressors; disputing excessively negative interpretations and finding “silver linings.” Role of negative cognitions in causing or maintaining depression. |
| Exercises | Daily reappraisal journal |
|
Week 4: Strengths and Goals |
How to recognize personal strengths. Support for acknowledging strengths even when feeling bad about oneself. Techniques for setting goals that are appropriately challenging but still feasible. Finding goals that will provide enjoyment or mastery experiences. |
| Exercises | Daily strengths journal (record ways you used a personal strength or talent) Select a goal for the week and record progress daily |
|
Week 5: Acts of Kindness |
The personal and relational benefits of performing small acts of kindness, even when under stress. Small prosocial acts that can be performed even if relatively socially isolated. |
| Exercises | Do something nice for someone else each day and record it in a daily kindness journal |
The intervention targets improvements in depression rather than diabetes-specific cognitions and health behaviors. Participants are told that they can choose to apply the skills to coping with diabetes, or to other domains of life in which they would like to increase positive emotion or cope more effectively.
The Present Study
Because this was a very early study, we chose to focus on establishing efficacy relative to an emotion-reporting control group while gathering participant feedback and data on retention. Our primary hypothesis was that the DAHLIA intervention would lead to improvements in important components of psychological well-being: Decreased stress, negative affect, and symptoms of depression, and increased positive affect.
We also explored the possibility that the intervention would lead to improvements in several diabetes-specific measures: diabetes-related self-efficacy, diabetes-related distress, physical exercise, medication adherence, and daily glucose testing. We considered these secondary hypotheses because the proximal targets of the intervention were the psychological outcomes.
Finally, we performed exploratory analyses comparing participants recruited in-person from a diabetes education class to a more heterogeneous group recruited online. We did not have a priori hypotheses about how they might differ.
Method
The study protocol was approved by the UCSF Committee on Human Research. All participants had an in-person or telephone conversation with a recruiter who explained the study and answered their questions, after which they read a written informed consent statement and gave consent to participate on the study website.
Participants
Participants were 53 adults with type 2 diabetes. They were recruited either in person through diabetes education classes at the University of California, San Francisco Diabetes Education Center (n = 28) or online through advertisements in the “volunteers” section of the San Francisco Bay Area Craigslist (n = 25). The online ad described the study as “testing whether learning skills for creating positive emotions and enjoying life might make people better at dealing with diabetes-related stress and taking care of their health” and described the compensation for completing study assessments (see “Procedure,” below). Participants recruited in person received a similar description from a study staff member.
Materials
On the first 1–2 days of each week, participants read a brief lesson introducing that week’s skill(s). For the rest of the week, they received a “home practice” assignment consisting of one or more simple practices, such as noticing positive events or tracking progress toward an attainable goal. Participants were asked to visit the website every day to record their home practice and complete the daily emotion reporting questionnaire.
New lessons became available 7 days after beginning the previous lesson, provided that the participant completed the home practice at least once. Participants were also allowed to postpone beginning a new lesson if they did not have time to read the material on the day it became available.
Procedure
After completing an online informed consent, participants completed the baseline questionnaire battery. They then began filling out daily emotion reports. Those who completed four emotion reports within the first 7 days were randomized to begin the intervention or to the control condition in which participants continued for 60 days of emotion reporting only1. Throughout the study, participants in both groups received an automated daily email with a link to the website. The email included a link that could be used to opt out of future reminders, but no participant chose to do so.
The post-intervention questionnaire battery was administered a week after the final lesson for intervention participants. This was an average of 57 days after the baseline measures for intervention participants (due to participants who opted to spend more than one week on some of the lessons) and an average of 63 days after baseline for control participants2. Finally, all participants received a follow-up phone call from an interviewer to collect feedback about their experience in the study approximately 7 days after the post-intervention questionnaires. Control participants were then given access to the intervention website.
Participants were paid $1 for each daily report completed, $20 for completing the final questionnaires and phone interview, and $20 if they completed the study within 75 days with reports on 75% of all days. The maximum total a participant could receive was $100. Intervention participants were informed that the compensation was for completing the daily questionnaires, and that they could continue visiting the site and earning payment for completing assessments even if they chose not to continue with the intervention. None of the participants did this (all either chose to continue with the intervention or dropped out of the study).
Measures
Primary outcome measures
Depressive Symptoms were measured using the CES-D[69], a measure of clinical and subclinical depressive symptomatology. On a 4-point scale, participants indicated how often they had felt symptoms in the past week (0 = “Rarely or none of the time – less than 1 day”; 4 = “All of the time – 5–7 days”), such as “I felt that I could not shake off the blues even with help from my family or friends.”
Perceived Stress was measured with the Perceived Stress Scale (PSS; [70,71]). The PSS is a widely-used measure of psychological stress designed for community samples. We used the 10 item version of the scale in which participants respond how often (1 = “never” to 5 = “very often”) during the past month they experienced thoughts and feelings such as “felt that you were unable to control the important things in your life” and “been unable to control irritations in your life.”
Positive and Negative Affect were measured with the Differential Emotions Scale (DES; [72]). Participants are asked to rate on a nine-point scale how often they experienced each of 23 positive and negative emotions, such as “grateful” or “anxious or scared” (0 = “Not at all”; 8 = “All the time”). Positive and negative emotion scores were calculated based on two different versions of the DES, one given at baseline and post-intervention that asked about the last two weeks, and one given every day of the study that asked about the past 24 hours. For the daily measure, the baseline score was an average of the reports from the run-in emotion reporting period and the post-intervention score was an average of the last four days of the study.
Diabetes-specific psychological measures
Diabetes self efficacy was measured using a version of the Confidence in Diabetes Self-Care scale (CIDS;[73]) adapted for type 2 diabetes. Participants used a 5-point scale to rate their confidence that they could perform 23 self-care activities, such as “check your feet for sores or blisters every day” and “ask your doctor questions about your treatment plans.”
Diabetes-related distress was measured using the Diabetes Distress Scale (DDS; [74]). Participants read 16 potential diabetes-related difficulties and use a 5-point scale to rate how much of a problem each one had been over the past month.
Health Behaviors
Each day participants were asked three health behavior questions about the previous day: Whether they had tested their blood sugar (not at all, once, or more than once), whether they had taken their medication as directed (none, some, or all), and how much walking or exercise they had done (<10 minutes, 10–30 minutes, or >30 minutes). The measure was scored 1 for days on which the participant was “fully adherent” (tested glucose at least twice, took all medication, or >30 minutes of activity) and 0 otherwise. Daily scores were then averaged to create a pre-intervention score (based on the emotion-reporting run-in period) and a post-intervention score (based on the last 4 days of the study) for each measure. Thus, scores of 0 represent nonadherence or imperfect adherence on all days during the period, and scores of 1 represent perfect adherence on all days.
Analytic Plan
For each dependent variable (depression, perceived stress, positive and negative affect, diabetes self-efficacy, diabetes distress, and diabetes-relevant health behaviors) change over time was assessed using a regression model with Time 2 as the dependent variable and Time 1 and treatment condition as simultaneous predictors. In follow-up analyses, we then expanded the model to include recruitment type (online recruitment vs. in person), with participants recruited online as the reference group, and the interaction between recruitment type and condition.
Results
The overall sample was 50.9% female and had a median age of 54 years. The sample was 36% Caucasian, 23% African-American, 19% Asian or Asian-American, 8% non-White Hispanic; 15% identified as other races or declined to respond. Intervention and control groups did not differ on age (F = 2.59, p = .11), gender (χ2 = .66, p = .42), or any racial category (χ2 < .1.63, p > .20). At baseline the groups did not differ on any outcome measures (F < 2.55, p>.12).
Completion Rates
Of the 53 participants recruited, 49 (92%) completed the initial emotion reporting run-in and were randomized (see Figure 1 for the CONSORT flow diagram). Forty-two participants (25 intervention and 17 control; 79% of the original sample) completed the final questionnaires. This is the sample used in the analyses reported below.
Figure 1.
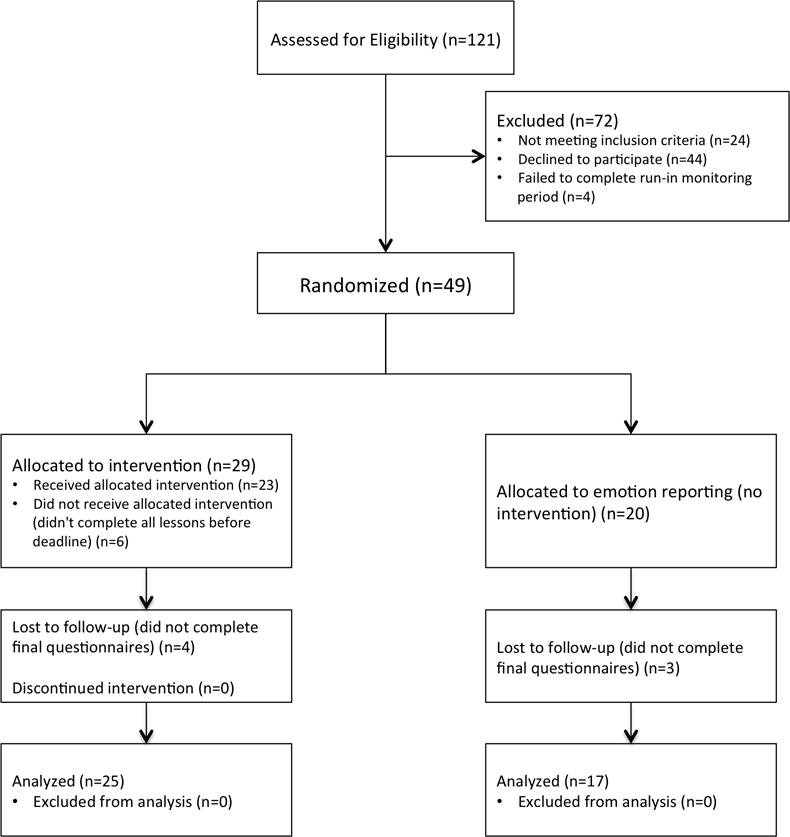
CONSORT flow diagram
Control participants were considered “full completers” if they submitted at least half of the daily emotion reports (30 of 60). Intervention participants were considered full completers if they reached the fifth and final lesson. Thirty-eight participants (72% of the original sample) met this criterion.
Website Use
Participants visited the study website an average of 5.0 times per week. Control participants visited significantly more frequently than intervention participants (5.8 vs. 4.5 visits / week; F = 4.28, p = .05, η2 = .10), possibly due to the greater time commitment required for intervention visits (reading lessons or doing exercises in addition to completing the emotions questionnaire).
Primary Outcomes: Depression, Affect, and Perceived Stress
Results are summarized in Table 2.
Table 2.
Pre- and Post-intervention outcome scores (mean and SD).
| Pre-intervention | Post-intervention | Treatment effect* | |
|---|---|---|---|
| CES-D (Depression) | |||
| Emotion reporting | 17.1 (15.4) | 17.7 (14.7) | β = −.21, p = .05 |
| DAHLIA intervention | 16.9 (11.6) | 12.6 (14.7) | |
| PSS (Perceived Stress) | |||
| Emotion reporting | 1.84 (.84) | 1.72 (.80) | β = −.13, p = .31 |
| DAHLIA intervention | 1.71 (.65) | 1.51 (.58) | |
| Daily positive affect | |||
| Emotion reporting | 5.13 (1.94) | 4.64 (2.13) | β = −.09, p = .46 |
| DAHLIA intervention | 5.10 (1.39) | 4.77 (1.42) | |
| Daily negative affect | |||
| Emotion reporting | 2.69 (1.25) | 2.39 (.86) | β = −.15, p = .32 |
| DAHLIA intervention | 2.37 (1.08) | 2.08 (1.00) | |
Regression parameter for condition predicting post-intervention score while controlling for pre-intervention score.
Depression
Depression scores dropped significantly in the intervention condition compared to control (β = −.21, p = .05). Scores in the intervention condition dropped by 4.3 points, from a mean of 16.9 – above the threshold for probable clinical depression – to 12.6, well below the threshold. Exploratory analysis found that this effect did not appear for the subset of positive affect CES-D items (β = .05, p = .71), but only the negative items (β = −.25, p = .03).
Perceived Stress
The intervention did not have a significant effect on PSS scores (β = −.13, p = .31).
Positive and Negative Affect
The retrospective and averaged daily measures were strongly correlated with each other for both PA and NA and at both timepoints (rs ranging from .61 to .85, p < .001). There was no significant effect of condition for positive or negative affect, using either measure (|β| < .15, p > .20).
Diabetes-Specific Psychological Measures
Neither the diabetes self-efficacy scale nor the diabetes distress scale showed any intervention effect (|β| < .09, p > .20).
Health Behaviors
There were no significant effects of the intervention on any health behavior measure (|β| < .19, p > .20).
Most participants had perfect medication adherence on all days (19/24 or 76% at T1 and 21/24 or 84% at T2), suggesting that medication adherence is not a large concern in this population, or that problems with adherence that do exist are not picked up by self-report. Glucose testing was highly dichotomized, with nearly all participants scoring either 0 (never tested twice or more in a day) or 1 (tested twice or more every day; 88% scored 0 or 1 at baseline and 80% at post-intervention). There was almost no change between timepoints. We tested an alternate scoring method in which days with 1 glucose test were scored as 0.5 instead of 0, which produced more variance among the participants with imperfect adherence but did not change the results.
Exploratory Analyses
Online vs. Offline recruitment
Recruitment method did not predict likelihood of reaching randomization (χ2 = .85, p = .36). However, participants recruited online were significantly more likely to complete the final measures (92% vs. 68%, χ2 = 4.68, p = .03) and to be full completers (88% vs. 57%, χ2 = 6.20, p = .01). Condition assignment was not related to either completing the final measures or reaching the full completer criterion (χ2 < .13, p> .72).
Website Use
Frequency of visits was not affected by recruitment method and there was no interaction between recruitment method and condition. (F < .78, p > .38).
For the key psychological outcomes, the effects of adding recruitment type to the analyses are summarized in Table 3.
Table 3.
Pre- and Post-intervention outcome scores for participants recruited online only (mean and SD).
| Pre-intervention | Post-intervention | Treatment effect* | |
|---|---|---|---|
| CES-D (Depression) | |||
| Emotion reporting | 22.9 (17.6) | 22.8 (16.4) | β = −.34, p = .02 |
| DAHLIA intervention | 20.9 (11.5) | 13.7 (9.58) | |
| PSS (Perceived Stress) | |||
| Emotion reporting | 1.88 (1.02) | 1.97 (.88) | β = −.43, p = .01 |
| DAHLIA intervention | 2.09 (.58) | 1.50 (.69) | |
| Daily positive affect | |||
| Emotion reporting | 4.54 (1.81) | 4.17 (2.04) | β = .14, p = .40 |
| DAHLIA intervention | 4.68 (1.48) | 4.76 (1.43) | |
| Daily negative affect | |||
| Emotion reporting | 3.06 (1.44) | 2.56 (1.04) | β = −.32, p = .09 |
| DAHLIA intervention | 2.70 (1.29) | 1.78 (.70) | |
Regression parameter for condition predicting post-intervention score while controlling for pre-intervention score and condition X offline recruitment interaction (i.e., the parameter shown reflects effect of condition among online recruits only).
[note for reviewers: We used this statistic for consistency with the tests reported in the text. We also ran the tests by excluding offline recruits and using a single condition parameter, and the results were essentially unchanged.]
Depression and recruitment type
When recruitment type was added to the model, the effect of condition became stronger (β = −.34, p = .02). The interaction was not significant (β = .25, p = .21), though the intervention appears to have had a considerably stronger effect for participants recruited online (see Figure 2): a reduction of 7.2 points, from above to below the criterion for probable clinical depression; versus a 1.4 point reduction for those recruited offline.
Figure 2.
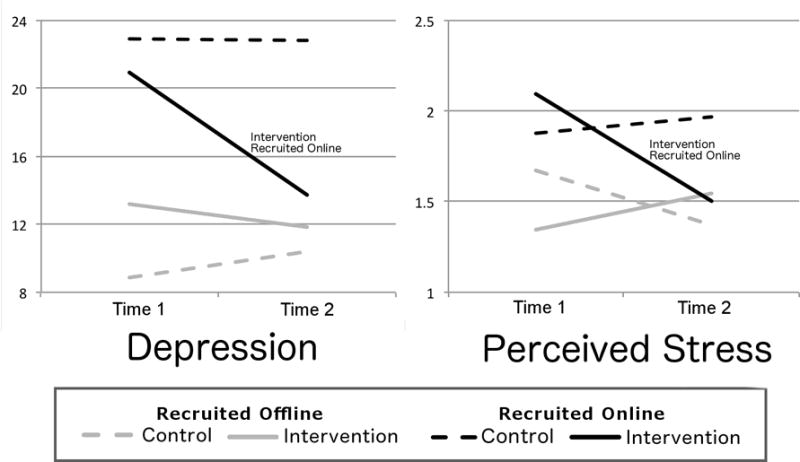
The DAHLIA intervention improves depression and perceived stress for participants recruited online, but not in person.
Perceived stress and recruitment type
When recruitment type was added, significant effects emerged (βcond = −.43, p = .01; βoffline = −.36, p = .08; βinteraction = .62, p = .01). Scores dropped significantly for participants in the intervention who were recruited online, but not those recruited offline (see Figure 2).
Positive affect and recruitment type
When recruitment type was added, a significant effect of condition emerged for retrospective PA (βcond = .32, p = .05); a marginal interaction indicated that the intervention increased PA only for intervention participants recruited online (βinteraction = −.35, p = .10). There were no significant effects for the averaged daily PA measure (see Figure 3).
Figure 3.
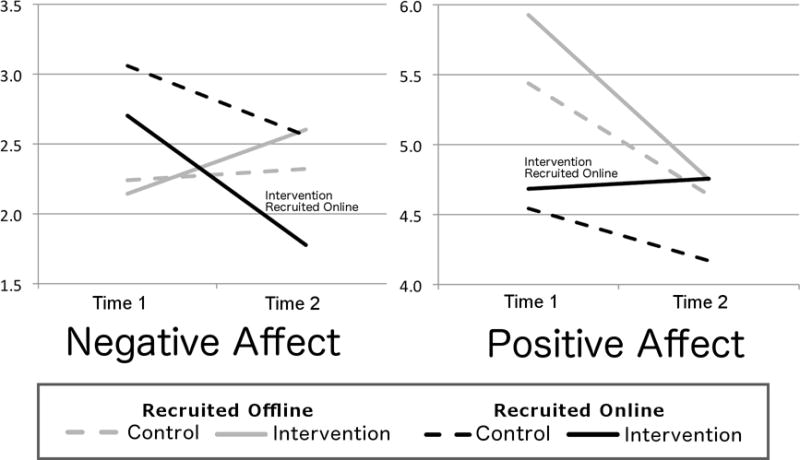
The DAHLIA intervention marginally reduces daily negative affect (but not daily positive affect) for participants recruited online, but not in person.
Negative affect and recruitment type: For NA, the retrospective measure had a similar pattern of marginal effects (βcond = −.35, p = .08; βinteraction = .46, p = .10), indicating that the intervention reduced NA for participants recruited online but not offline. The averaged daily measure showed the same pattern, though the interaction fell short of significance (βcond = −.32, p = .09; βinteraction = .38, p = .13; see Figure 3).
Diabetes Specific Measures
Adding recruitment group did not change these results (|β| < .13, p > .20), with the exception of a marginal interaction between condition and recruitment group for the CIDS (β = .−.45, p = .08). The pre-post change in CIDS score for intervention-offline participants was marginally significant on its own (t(10) = 1.92, p = .08), tentatively suggesting that the intervention may have led to reduced diabetes self-efficacy for this subset of participants.
Baseline differences in depression
Participants recruited online had much higher baseline symptoms of depression than those recruited offline (CESD score of 21.8 vs. 11.2; F = 8.03, p = .01, η2 = .17). We repeated the analyses of positive affect, negative affect, and perceived stress with baseline CESD score (centered) and the interaction between recruitment method and baseline CESD added to the model. If the interaction between recruitment group and condition were significantly reduced, this would suggest that the difference in intervention efficacy between recruitment groups is fully or partially explained by differences in baseline depression.
Baseline depression strongly predicted increases over time in negative affect (β =.74, p = .02) and, marginally, perceived stress (β =.52, p = .06) but did not predict positive affect (β −.13, p = .51). The magnitude of the interaction between treatment group and recruitment method was effectively unchanged for positive affect (β changed from −.35 to −.43, new p = .09) or negative affect (β changed from .46 to .41, new p = .15).
The interaction between treatment group and recruitment method was substantially reduced for perceived stress (β changed from .62 to .37, new p = .19). However, the alternate interaction between depression and recruitment method did not approach significance for this or any other outcome (|β| < .12, p > .51). Thus, it does not appear that the differential intervention effects by recruitment group can be explained by their baseline differences in depression.
Discussion
We found that an online intervention targeting positive affect skills was able to reduce depression symptoms in adults with type 2 diabetes. The intervention is well suited to broad, inexpensive dissemination, and has the potential to substantially improve quality of life. We demonstrated good retention and adherence, paving the way for future effectiveness research.
Notably, our intervention reduced depression symptoms regardless of participants’ baseline symptom levels. This adds to the growing evidence that interventions based on positive emotions are accessible and effective even for individuals already experiencing depression[75], rather than being restricted to those who are doing well. This points to potential effectiveness in both a preventative and a treatment role.
Unexpectedly, we found that the intervention’s effects were on the negative, rather than the positive, CES-D items; there were also clearer effects on negative affect than on positive affect. We consider this finding a mystery and do not have a clear explanation for it. It does not reduce the potential impact of a reduction in depression symptoms, though it does make the mechanism and nature of the effects less clear.
Feasibility and acceptability
The intervention appears feasible, with a 79% completion rate. Intervention participants visited the website an average of 4.5 times / week, and completed the assigned activities (lessons or skill practice, plus the emotion questionnaire) on nearly all visits. Visit frequency was slightly higher in the emotion-reporting control condition, possibly due to the lower time requirement for control visits. Participants in both groups reported that the daily reminder emails were helpful.
During post-study interviews, participants expressed that they understood the intervention content and found it sensitive and useful. Their comments also suggested that they understood and retained specific intervention concepts, such as mindful awareness and appreciating positive events without denying negative ones. For example, one participant said, “Little things that used to make me angry could become big things and annoy me all day, and now I can just let them go. It’s helped me to be more optimistic, and be present in the moment.” Another said, “these skills can help me see […] Instead of diabetes controlling my life, it’s just a part of my life […] Because I really believe now, having diabetes is a terrible thing, but it’s helped me live a healthier lifestyle that otherwise I wouldn’t have.”
Others commented on the applicability of the intervention to diabetes-related health behaviors, although this was not an explicit focus of the intervention: “Whenever I would get upset, I would stop by the store and buy some kind of pastry. But I haven’t done that lately […] It pretty much taught me how to get through stress without going to my comfort food and overindulging.”
Participants who dropped out generally cited time constraints; none raised issues with the content of the intervention.
Online vs. offline recruitment
The effect of the intervention was considerably stronger among participants recruited over the Internet compared to participants recruited in-person. Online recruits in the intervention condition also showed significant reductions in negative affect and perceived life stress relative to online controls. For positive affect, they improved according to the retrospective measure but not the averaged daily measures.
There are no obvious demographic differences that might explain these differential effects. Participants recruited online were significantly higher on baseline depression symptoms (CES-D 21.8 vs. 11.2), but exploratory analyses suggest that baseline depression differences were not related to intervention effectiveness. It is possible that online recruits were simply more comfortable with using websites or more amenable to learning skills online. It is also possible that online recruits were more actively seeking information or help for their diabetes compared to the participants who were recruited in person through the clinic, though the two groups did not differ on number of visits to the website.
Limitations of the current study
This pilot study provides initial evidence that an online positive emotions intervention can be delivered in an effective, understandable, and sensitive manner to adults with type 2 diabetes, with strong participant engagement and adherence. However, it was not powered to detect downstream changes leading from psychological benefits to health behaviors and health outcomes. Based on the promising psychological outcomes in this study, we are planning a larger intervention study that will collect valid health behavior and health outcome measures, including preventative healthcare utilization, adherence to personalized medication regimens, electronic glucose monitor records, and long-term morbidity and mortality. This will also be a key requirement for rigorous, gold-standard internet-based trials, in order to corroborate participants’ reports of diabetes diagnosis and symptom change.
It will also be important for future studies to test the DAHLIA intervention against a more potent control treatment. Because of the low cost of this intervention, and because individuals typically do not receive interventions of this type (i.e., there is no comparable treatment-as-usual), any degree of efficacy is of potential value. However, comparison with a persuasive placebo control or a psychosocial intervention not based on positive psychology principles will be critical in order to test the proposed importance of positive affect as a mechanism for change, and to guide further intervention development.
The intervention appears to have been effective in a sample recruited online, but less so in a sample recruited in-person from a diabetes clinic. In fact there was some suggestion of reduced diabetes self-efficacy among intervention participants recruited in person, though this was a marginally significant finding and may have occurred by chance. In future research we plan to measure additional variables related to demographics, internet and technology use, learning preferences, and readiness to engage in health behavior change. These will help us determine the cause of this difference and predict which individuals are good candidates for an online intervention and which, if any, might respond negatively.
Participants in this study were paid for completing the daily and pre-post assessments. This increases the per-participant cost of the intervention and reduces the generalizability of our results. However, we felt that payment was important in order to compensate participants for putting time into an untested intervention, and to avoid problems with selective reporting at post-intervention. We are currently pilot testing variants on the intervention that use other methods to enhance retention, including self-tracking feedback and gamification, lower-burden mobile exercises, and peer support.
Finally, this study did not include follow-up assessments that would allow us to assess long-term intervention effects. Longer-term health and psychological follow-up will be included in future studies.
Conclusion
We have demonstrated that individuals with type 2 diabetes find our online positive emotion skills intervention engaging and feasible to complete. The intervention shows potential to reduce symptoms of depression, even in participants with elevated– and in many cases likely clinically significant – levels of baseline depression. The intervention also showed broader psychological efficacy in individuals recruited online, on whom we plan to focus in future research. We are currently working with collaborators to combine our stress-coping and resource-building model of positive emotions with a more direct health behavior adherence intervention[27]. The planned intervention study will gather more definitive effectiveness data, including personalized health behavior adherence and health outcome data with longer-term followup.
Supplementary Material
Acknowledgments
We gratefully acknowledge the support of the following colleagues: Elizabeth Bartmess provided training and oversight in software user experience testing. Heather Coleman performed user experience testing and contributed to intervention development. Stephanie Maurer assisted with study protocol development. Marlene Bedrich and Gloria Yee at the UCSF Diabetes Education Center helped tailor the intervention for a type 2 diabetes population and permitted us to recruit participants at their classes.
This publication was supported by 1) NIMH K24 5K24MH093225-02 and 2) the National Center for Research Resources and the National Center for Advancing Translational Sciences, NIH, through UCSF-CTSI Grant Number UL1 RR024131. The sponsors had no role in the conduct of the research, analysis, or preparation of the manuscript.
Footnotes
Author Contributions
JTM developed the original positive affect intervention and oversaw the design and execution of the study. MAC led adaptation of the intervention, implemented the study, and performed the analyses. JRH and MEP contributed to intervention adaptation, study logistics, and participant recruitment and contact. LRS contributed to intervention adaptation and study design. The manuscript was prepared by MAC and JTM and approved by all authors.
We used fully random assignment based on a computerized random number generator. This led to a chance discrepancy in cell sizes: 29 participants were assigned to the intervention and 20 to the control condition.
The length of the emotion reporting period was based on our estimate of how long it would take intervention participants to complete the lessons. Average time to complete the intervention was lower than expected, leading to the slight mismatch between groups in time spent in the study.
Conflicts of Interest
None
References
- 1.Moskowitz JT, Epel ES, Acree M. Positive affect uniquely predicts lower risk of mortality in people with diabetes. Health psychology: official journal of the Division of Health Psychology, American Psychological Association. 2008;27:S73–82. doi: 10.1037/0278-6133.27.1.S73. [DOI] [PubMed] [Google Scholar]
- 2.Nefs G, Pouwer F, Denollet J, Kramer H, Wijnands-van Gent CJM, et al. Suboptimal glycemic control in type 2 diabetes: A key role for anhedonia? Journal of psychiatric research. 2012;46:549–554. doi: 10.1016/j.jpsychires.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 3.Tsenkova VK, Dienberg Love G, Singer BH, Ryff CD. Coping and positive affect predict longitudinal change in glycosylated hemoglobin. Health Psychology. 2008;27:S163. doi: 10.1037/0278-6133.27.2(Suppl.).S163. [DOI] [PubMed] [Google Scholar]
- 4.Baruth M, Lee D-C, Sui X, Church TS, Marcus BH, et al. Emotional outlook on life predicts increases in physical activity among initially inactive men. Health Education & Behavior. 2011;38:150–158. doi: 10.1177/1090198110376352. [DOI] [PubMed] [Google Scholar]
- 5.Grant N, Wardle J, Steptoe A. The relationship between life satisfaction and health behavior: a cross-cultural analysis of young adults. International journal of behavioral medicine. 2009;16:259–268. doi: 10.1007/s12529-009-9032-x. [DOI] [PubMed] [Google Scholar]
- 6.Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among US community-dwelling adults. Journal of Community Health. 2008;33:40–50. doi: 10.1007/s10900-007-9066-4. [DOI] [PubMed] [Google Scholar]
- 7.White DK, Keysor JJ, Neogi T, Felson DT, LaValley M, et al. When it hurts, a positive attitude may help: association of positive affect with daily walking in knee osteoarthritis. Results from a multicenter longitudinal cohort study. Arthritis Care & Research. 2012;64:1312–1319. doi: 10.1002/acr.21694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelloniemi H, Ek E, Laitinen J. Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite. 2005;45:169–176. doi: 10.1016/j.appet.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Leventhal AM, Ramsey SE, Brown RA, LaChance HR, Kahler CW. Dimensions of depressive symptoms and smoking cessation. Nicotine & Tobacco Research. 2008;10:507–517. doi: 10.1080/14622200801901971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Niemiec CP, Ryan RM, Patrick H, Deci EL, Williams GC. The energization of health-behavior change: examining the associations among autonomous self-regulation, subjective vitality, depressive symptoms, and tobacco abstinence. The Journal of Positive Psychology. 2010;5:122–138. [Google Scholar]
- 11.Carrico AW, Moskowitz JT. Positive affect promotes engagement in care following HIV diagnosis. Health Psychology. doi: 10.1037/hea0000011. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mancuso CA, Choi TN, Westermann H, Wenderoth S, Hollenberg JP, et al. Increasing physical activity in patients with asthma through positive affect and self-affirmation: A randomized trial. Archives of internal medicine: archinternmed. 2012 doi: 10.1001/archinternmed.2011.1316. 2011.1316 v2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante JP, Isen AM, et al. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Archives of internal medicine. 2012;172:322. doi: 10.1001/archinternmed.2011.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peterson JC, Charlson ME, Hoffman Z, Wells MT, Wong S-C, et al. Randomized controlled trial of positive affect induction to promote physical activity after percutaneous coronary intervention. Archives of internal medicine: archinternmed. 2012 doi: 10.1001/archinternmed.2011.1311. 2011.1311 v2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peterson JC, Czajkowski S, Charlson ME, Link AR, Wells MT, et al. Translating basic behavioral and social science research to clinical application: The EVOLVE mixed methods approach. Journal of consulting and clinical psychology. 2013;81:217. doi: 10.1037/a0029909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saslow LR, Cohn M, Moskowitz JT. Positive Affect Interventions to Reduce Stress: Harnessing the Benefit while Avoiding the Pollyanna. In: Gruber J, Moskowitz JT, editors. The Dark and Light Sides of Positive Emotion. New York: Oxford University Press; (in press) [Google Scholar]
- 17.Moskowitz JT, Hult JR, Duncan LG, Cohn MA, Maurer SA, et al. A Positive Affect Intervention for People Experiencing Health-Related Stress: Development and Non-Randomized Pilot Test. Journal of Health Psychology. 2012;17:677–693. doi: 10.1177/1359105311425275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dowling GA, Merrilees J, Mastick J, Chang VY, Hubbard E, et al. Life enhancing activities for family caregivers of people with frontotemporal dementia. Alzheimer’s Disease and Associated Disorders. doi: 10.1097/WAD.0b013e3182a6b905. (in press) [DOI] [PubMed] [Google Scholar]
- 19.Folkman S. Positive psychological states and coping with severe stress. Social Science and Medicine. 1997;45:1207–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- 20.Fredrickson BL. What good are positive emotions? Review of General Psychology. 1998;2:300–319. doi: 10.1037/1089-2680.2.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Musselman DL, Betan E, Larsen H, Phillips LS. Relationship of depression to diabetes types 1 and 2: Epidemiology, biology, and treatment. Biological Psychiatry. 2003;54:317–329. doi: 10.1016/s0006-3223(03)00569-9. [DOI] [PubMed] [Google Scholar]
- 22.Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care, and glucose control in diabetes. General Hospital Psychiatry. 2003;25:246–252. doi: 10.1016/s0163-8343(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 23.Zhang X, Norris SL, Gregg EW, Cheng YJ, Beckles G, et al. Depressive symptoms and mortality among persons with and without diabetes. Am J Epidemiol. 2005;161:652–660. doi: 10.1093/aje/kwi089. [DOI] [PubMed] [Google Scholar]
- 24.Sin NL, Della Porta MD, Lyubomirsky S. Tailoring positive psychology interventions to treat depressed individuals. In: Donaldson SI, Csikzentmihalyi M, N J, editors. Applied positive psychology: Improving everyday life, health, schools, work, and society. New York: Routledge; 2011. pp. 79–96. [Google Scholar]
- 25.Kanter JW, Manos RC, Bowe WM, Baruch DE, Busch AM, et al. What is behavioral activation?: A review of the empirical literature. Clinical psychology review. 2010;30:608–620. doi: 10.1016/j.cpr.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 26.Katon WJ, Von Korff M, Lin EH, Simon G, Ludman E, et al. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Archives of general psychiatry. 2004;61:1042. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 27.Safren S, Gonzalez J, Wexler D, Psaros C, Delahanty L, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in patients with uncontrolled type 2 diabetes. Diabetes Care. doi: 10.2337/dc13-0816. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lorig K, Ritter PL, Laurent DD, Plant K, Green M, et al. Online Diabetes Self-Management Program A randomized study. Diabetes Care. 2010;33:1275–1281. doi: 10.2337/dc09-2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Glasgow RE, Boles SM, Mckay HG, Feil EG, Barrera M., Jr The D-Net diabetes self-management program: long-term implementation, outcomes, and generalization results. Preventive medicine. 2003;36:410–419. doi: 10.1016/s0091-7435(02)00056-7. [DOI] [PubMed] [Google Scholar]
- 30.Pal K, Eastwood SV, Michie S, Farmer AJ, Barnard ML, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. The Cochrane Library. 2013 doi: 10.1002/14651858.CD008776.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Christensen H, Griffiths KM, Farrer L. Adherence in internet interventions for anxiety and depression. J Med Internet Res. 2009;11:e13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cognitive behaviour therapy. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- 33.Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: Is human contact necessary for therapeutic efficacy? Clinical psychology review. 2011;31:89–103. doi: 10.1016/j.cpr.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 34.Van’t Hof E, Cuijpers P, Stein DJ. Self-help and Internet-guided interventions in depression and anxiety disorders: a systematic review of meta-analyses. CNS spectrums. 2009;14:34–40. doi: 10.1017/s1092852900027279. [DOI] [PubMed] [Google Scholar]
- 35.Proudfoot J, Goldberg D, Mann A, Everitt B, Marks I, et al. Computerized, interactive, multimedia cognitive-behavioural program for anxiety and depression in general practice. Psychological Medicine. 2003;33:217–227. doi: 10.1017/s0033291702007225. [DOI] [PubMed] [Google Scholar]
- 36.Andersson G, Bergstrom J, Hollandare F, Carlbring P, Kaldo V, et al. Internet-based self-help for depression: randomised controlled trial. Br J Psychiatry. 2005;187:456–461. doi: 10.1192/bjp.187.5.456. [DOI] [PubMed] [Google Scholar]
- 37.Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. Bmj. 2004;328:265. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Christensen H, Griffiths KM, Korten A. Web-based cognitive behavior therapy: analysis of site usage and changes in depression and anxiety scores. Journal of medical Internet research. 2002;4 doi: 10.2196/jmir.4.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clarke G, Kelleher C, Hornbrook M, DeBar L, Dickerson J, et al. Randomized effectiveness trial of an Internet, pure self-help, cognitive behavioral intervention for depressive symptoms in young adults. Cognitive behaviour therapy. 2009;38:222–234. doi: 10.1080/16506070802675353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Den Berg S, Shapiro D, Bickerstaffe D, Cavanagh K. Computerized cognitive–behaviour therapy for anxiety and depression: a practical solution to the shortage of trained therapists. Journal of Psychiatric and Mental Health Nursing. 2004;11:508–513. doi: 10.1111/j.1365-2850.2004.00745.x. [DOI] [PubMed] [Google Scholar]
- 41.Murrell SA, Norris FH. Resources, life events, and changes in positive affect and depression in older adults. American Journal of Community Psychology. 1984;12:445–464. doi: 10.1007/BF00896505. [DOI] [PubMed] [Google Scholar]
- 42.Zautra AJ, Reich JW. Life events and perceptions of life quality: developments in a two-factor approach. Journal of Community Psychology. 1983;11:121–132. [Google Scholar]
- 43.Krause N. Positive life events and depressive symptoms in older adults. Behavioral Medicine. 1998;14 doi: 10.1080/08964289.1988.9935131. [DOI] [PubMed] [Google Scholar]
- 44.Lewinsohn PM, Hoberman HM, Clarke GN. The coping with depression course: Review and future directions. Canadian Journal of Behavioral Science. 1989;21:470–493. [Google Scholar]
- 45.Langston CA. Capitalizing on and coping with daily-life events: Expressive responses to positive events. Journal of Personality and Social Psychology. 1994;67:1112–1125. [Google Scholar]
- 46.Bryant FB. A four-factor model of perceived control: Avoiding, coping, obtaining, and savoring. Journal of Personality. 1989;57:773–797. [Google Scholar]
- 47.Emmons RA. Thanks! how the new science of gratitude can make you happier. New York: Houghton Mifflin; 2007. [Google Scholar]
- 48.Emmons RA, McCullough ME. Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. Journal of Personality and Social Psychology. 2003;84:377–389. doi: 10.1037//0022-3514.84.2.377. [DOI] [PubMed] [Google Scholar]
- 49.Kashdan TB, Uswatte G, Julian T. Gratitude and hedonic and eudaimonic well-being in Vietnam war veterans. Behaviour Research and Therapy. 2006;44:177–199. doi: 10.1016/j.brat.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 50.Kabat-Zinn J. Mindfulness-Based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice. 2003;10:144–156. [Google Scholar]
- 51.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 52.Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: Positive emotions, induced through meditation, build consequential personal resources. Journal of Personality and Social Psychology. 2008;95:1045–1062. doi: 10.1037/a0013262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grossman P, Tiefenthaler-Gilmer U, Raysz A, Kesper U. Mindfulness training as an intervention for fibromyalgia: Evidence of postintervention and 3-year follow-up benefits in well-being. Psychotherapy and Psychosomatics. 2007;76:226–233. doi: 10.1159/000101501. [DOI] [PubMed] [Google Scholar]
- 54.Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychology. 2003;22:487–497. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- 55.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer; 1984. [Google Scholar]
- 56.Reed MB, Aspinwall LG. Self-affirmation reduces biased processing of health-risk information. Motivation and Emotion. 1998;22:99–132. [Google Scholar]
- 57.Koole SL, Smeets K, van Knippenberg A, Dijksterhuis A. The cessation of rumination through self-affirmation. Journal of Personality and Social Psychology. 1999;77:111–125. [Google Scholar]
- 58.Taylor SE, Lerner JSS, D K, Sage RM, McDowell NKl. Are self-enhancing cognitions associated with healthy or unhealthy biological profiles? Journal of Personality and Social Psychology. 2003;85:605–615. doi: 10.1037/0022-3514.85.4.605. [DOI] [PubMed] [Google Scholar]
- 59.Strecher VJ, Seijts G, Kok GJ, Latham GP, Glasgow R, et al. Goal setting as a strategy for health behavior change. Health Education Quarterly. 1995;22:190–200. doi: 10.1177/109019819502200207. [DOI] [PubMed] [Google Scholar]
- 60.Carver CS, Scheier MF. Origins and functions of positive and negative affect: A control process view. Psychological Review. 1990;97:19–35. [Google Scholar]
- 61.Lent RW, Singley D, Sheu H-B, Gainor KA, Brenner BR, et al. Social cognitive predictors of domain and life satisfaction: Exploring the theoretical precursors of subjective well-being. Journal of Consulting and Clinical Psychology. 2005;52:429–442. [Google Scholar]
- 62.Emmons RA. Abstract versus concrete goals: Personal striving level, physical illness, and psychological well-being. Journal of Personality and Social Psychology. 1992;62:292–300. doi: 10.1037//0022-3514.62.2.292. [DOI] [PubMed] [Google Scholar]
- 63.Sheldon KM, Houser-Marko L. Self-concordance, goal attainment, and the pursuit of happiness: Can there be an upward spiral? Journal of Personality and Social Psychology. 2001;80:152–165. [PubMed] [Google Scholar]
- 64.Musick MA, Wilson J. Volunteering and depression: the role of psychological and social resources in different age groups. Social Science & Medicine. 2003;56:259–269. doi: 10.1016/s0277-9536(02)00025-4. [DOI] [PubMed] [Google Scholar]
- 65.Oman D, Thoresen CE, McMahon K. Volunteerism and mortality among the community-dwelling elderly. Journal of Health Psychology. 1999;4:301–316. doi: 10.1177/135910539900400301. [DOI] [PubMed] [Google Scholar]
- 66.Moen P, Dempster-McCain D, Williams RM. Successful aging. American Journal of Sociology. 1993;97:1612–1632. [Google Scholar]
- 67.Penner LA, Dovidio JF, Piliavin JA, Schroeder DA. Prosocial behavior: Multilevel perspectives. Annual Review of Psychology. 2005;56:365–392. doi: 10.1146/annurev.psych.56.091103.070141. [DOI] [PubMed] [Google Scholar]
- 68.Lyubomirsky S, King L, Diener E. The benefits of frequent positive affect: does happiness lead to success? Psychological Bulletin. 2005;131:803–855. doi: 10.1037/0033-2909.131.6.803. [DOI] [PubMed] [Google Scholar]
- 69.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1:385–401. [Google Scholar]
- 70.Cohen S. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health The Claremont Symposium on Applied Social Psychology. Thousand Oaks, CA: Sage Publications, Inc; 1988. pp. 31–67. [Google Scholar]
- 71.Cohen S, Williamson GM. Stress and infectious disease in humans. Psychol Bull. 1991;109:5–24. doi: 10.1037/0033-2909.109.1.5. [DOI] [PubMed] [Google Scholar]
- 72.Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality and Social Psychlogy. 2003;84:365–376. doi: 10.1037//0022-3514.84.2.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Van Der Ven N, Weinger K, Yi J, Pouwer F, Ader H, et al. The confidence in diabetes self-care scale: psychometric properties of a new measure of diabetes-specific self-efficacy in Dutch and US patients with type 1 diabetes. Diabetes Care. 2003;26:713–718. doi: 10.2337/diacare.26.3.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28:626–631. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 75.Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. Journal of clinical psychology. 2009;65:467–487. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


