Abstract
Controlling pain in patients with fractured ribs is essential for preventing secondary complications. Conventional medications that are administered orally or by using injections are sufficient for the treatment of most patients. However, additional aggressive pain control measures are needed for patients whose pain cannot be controlled effectively as well as for those in whom complications or a transition to chronic pain needs to be prevented. In this study, we retrospectively analyzed the medical records of patients in our hospital to identify the efficacy and characteristics of intercostal nerve block (ICNB), as a pain control method for rib fractures. Although ICNB, compared to conventional methods, showed dramatic pain reduction immediately after the procedure, the pain control effects decreased over time. These findings suggest that the use of additional pain control methods (e.g. intravenous patient-controlled analgesia and/or a fentanyl patch) is recommended for patients in who the pain level increases as the ICNB efficacy decreases.
Keywords: Intercostal nerve block, Pain control, Rib fracture
INTRODUCTION
Thoracic injuries have a number of causes including falls, traffic accidents, sports injuries, and physical assaults. The forms of thoracic injuries are diverse, and they include simple bruises and rib fractures as well as traumatic hemothorax or pneumothorax associated with internal organ damage from rib fractures; in extreme cases, open thoracic trauma with exposure of the thoracic cavity occurs. Among these injuries, the most common forms leading to hospitalization are simple bruises or blunt trauma in the form of a rib fracture, with complaints of tenderness around the injured area and pain during exercising, coughing, and/or breathing. Depending on the chief complaints, the first doctor examining the patient conducts the physical examination and observes a simple chest radiograph, nuclear scan, computed tomography, or thoracic ultra-sonogram. In most cases, conservative treatment consisting of an analgesic, muscle relaxant, in the form of injection, or oral medication is administered; however, depending on the patient’s degree of pain or the injury severity, hospitalization and more aggressive pain control measures may be required. Thus, depending on the injury severity, differences in treatment methods, hospitalization, and/or treatment duration are determined. Most of the pain is eliminated after 2–3 days of conservative treatment in most common blunt trauma cases, and a prescription of 2–3 weeks of oral analgesics is enough after discharge.
Pain control is essential for not only primary pain relief but also preventing secondary complications such as atelectasis or pneumonia as well as the transition to chronic pain. Accordingly, further steps are now being taken from the conventional pain control medication and techniques by the introduction of more aggressive pain control measures such as the intercostal nerve block (ICNB) (Moore and Bridenbaugh, 1962; Wurnig et al., 2002), transcutaneous electrical nerve stimulation (TENS) (Oncel et al., 2002), and intravenous patient-controlled analgesia (IV PCA). Used early on, these aggressive measures increase patient satisfaction and prevent secondary complications. The purpose of this study was to compare the use of ICNB, as an aggressive pain control measure, with conventional oral or injectable medications in terms of the hospitalization length or medication administration duration along with pain relief degree in patients with thoracic injuries.
MATERIALS AND METHODS
Subjects
In this study, among those patients who were admitted to our hospital between March 2008 and December 2012 with thoracic injuries, those with rib fractures were allocated to either the conventional pain control group (control group) or conventional pain control plus ICNB group (experimental group), and their medical records were retrospectively analyzed. In this study, the index and methods needed for analysis were performed as indicated below by using a statistical method (chi-square test, SPSS 12.0) for analysis with the statistical significance level set at a P-value of less than 0.05.
Measurement and data index
Parameters such as sex, age, causes of rib fracture, most painful or tender area, number of patients in the control and experimental groups, presence of ICNB-related complications (pneumothorax or hemothorax), and need for chest tube insertion were investigated.
At the time of the initial outpatient visit or emergency room admission, the patients were presented with the Visual Analog Scale (VAS), which scores the pain level from 0 to 10 points, and the pain level at the time was evaluated objectively (Fig. 1).
Fig. 1.
Visual Analog Scale.
For the conventional pain control group (control group) and conventional pain control plus ICNB group (experimental group), the pain levels during hospitalization (immediately after medication or ICNB, 1 day later, and 7 days later) were evaluated by using the VAS, and their values were compared to the initial pain level. The length of hospitalization was compared between the control and experimental groups.
RESULTS
Patients’ general characteristics
For the duration of this study, there were 54 patients (44 men, 10 women) with an average age of 48.50 yr (23–83 yr). The causes of thoracic injury consisted of 24 falls, 17 traffic accidents, 11 physical assauls, and 2 other causes. The most painful or tender area was the left side in 28 and the right side in 26.
Of the 54, 31 received the conventional medication treatment (control group) and 23 received the conventional medication treatment along with ICNB (experimental group). There were no ICNB-related complications (pneumothorax or hemothorax).
A total of 17 patients, 11 from the control group and 6 from the experimental group, required chest tube insertion due to rib fracture-related lung injuries resulting in traumatic hemothorax or pneumothorax (Table 1).
Table 1.
Patient’s general characteristics
| Total (n= 54) | |
|---|---|
| Sex | Men 44; Women 10 |
| Age | Mean 45.50 yr (23–83 yr) |
| Causes | Falls 24 |
| Traffic accident 17 | |
| Physical assault 11 | |
| Other 2 | |
| Side | Left 28; Right 26 |
| Group | Conventional (Control) 31 |
| Conventional + ICNB (Experimental) 23 | |
| Chest tube insertion | Control 11 |
| Experimental 6 |
ICNB, intercostal nerve block.
Results of treatments
The average number of fractured ribs in patients from the control and experimental groups were 3.19 (1–7) and 4.91 (1–9), respectively, a difference that was statistically significant (P=0.008). At the time of admission, the average pain scores for the control and experimental groups were 8.16 (2–10) and 9.43 (4–10), respectively, but the difference was not statistically significant (P=0.200).
The average pain scores immediately after medication administration (procedure) in the control and experimental groups were 7.42 (2–10) and 5.39 (0–9), respectively, showing a statistically significant reduction in pain in the experimental group (P=0.007).
The average pain scores 1 day after medication administration (procedure) in the control and experimental groups were 6.16 (2–10) and 5.04 (1–10), respectively, but were not statistically different (P=0.240); after 7 days, the pain scores in the control and experimental groups were 3.81 (1–8) and 3.65 (1–5), respectively, showing no statistically significant difference (P=0.944).
The average hospitalization lengths for the control and experimental groups were 9.35 days (2–49 days) and 10.61 days (4–22 days), respectively, but no statistically significant difference was observed (P=0.133) (Table 2, Fig. 2).
Table 2.
Results of treatment
| Cont. (n= 31) | Exp. (n= 23) | P-value | |
|---|---|---|---|
| No. rib fx | 3.19 (1–7) | 4.91 (1–9) | 0.008 |
| VAS score (initial) | 8.16 (2–10) | 9.43 (4–10) | 0.200 |
| Post-Tx VAS score (immediately) | 7.42 (2–10) | 5.39 (0–9) | 0.007 |
| Post-Tx VAS score (1 d) | 6.16 (2–10) | 5.04 (1–10) | 0.240 |
| Post-Tx VAS score (7 d) | 3.81 (1–8) | 3.65 (1–5) | 0.944 |
| Hospital stay (d) | 9.35 (2–49) | 10.61 (4–22) | 0.133 |
Cont., control; Exp., experimental.
Fig. 2.
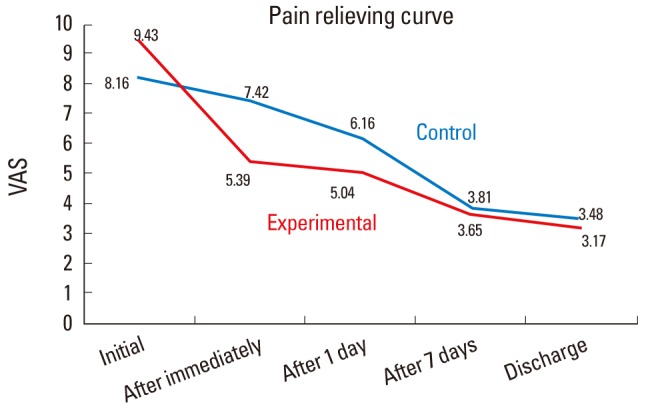
Pain relief curve.
DISCUSSION
In treating rib fractures among all thoracic injuries, optimal pain control is most important as it can not only relieve pain but also prevent complications in the respiratory system and related mortality. The efficacy of oral administration or injection of conventional non-steroidal anti-inflammatory drugs or opioid class drugs may vary among patients, but oral medications can generally be discontinued in 2–3 weeks. In this study, the pain reduction of the conventional medication were moderately efficient in both groups. However, more aggressive pain relief measures are being used after considering patient’s demand or advanced age as well as to prevent complications from underlying diseases. In this study, a statistically significant difference was observed in the number of fractured ribs between the control and experimental groups, while the pain levels at the time of admission did not show a statistically significant difference. These results indicated that the patients’ subjective pain levels were based on the number of fractures, thereby reflecting the allocation into the experimental group by patient’s request.
Worthley (1985) and Rauchwerger et al. (2013) stated that pain could be controlled by injecting anesthetics or steroids into the thoracic epidural space; it was reported to be effective for bilateral rib fractures. The technical methodology of ICNB was reported by Moore and Bridenbaugh (1962); it includes using medical imaging techniques to find the intercostal nerve targeted for blocking on the basis of the pain location, and then injecting a local anesthetic into the target area. The advantages of ICNB are as follows: relatively simple for use; no neurological complications due to nausea, vomiting, dizziness, or bleeding; and no complications from possible misjudgment observed in other measures such as thoracic epidural injection or IV PCA. The disadvantages include claims that it must be repeated every 6–8 h because its effects do not last long (Pederson et al., 1983) and the possibility of complications such as pneumothorax or hemothorax (Rauchwerger et al., 2013). Although no complications were observed in this study, significant pain reduction was observed immediately after treatment, a pattern of slowed pain reduction emerged 1 day after treatment, which is thought to be due to depletion of the medication used in ICNB (Wurnig et al., 2002). In addition, the lack of statistically significant differences between the two groups in the pain levels at 7 days after treatment, pain levels at the time of discharge, and the length of hospitalization leads us to believe that ICNB shows maximum efficacy immediately after treatment but then gradually diminishes (Fig. 2). Measures to address this effect are needed include the use of additional medication such as IV PCA, and/or a fentanyl patch.
Other pain control measures include the intrapleural injection of a local anesthetic (Mann et al., 1992) or a paravertebral block, which is used primarily in unilateral rib fracture cases. In addition, although supporting medical evidence may be insufficient, pain control in patients with rib fractures by using acupuncture has also been reported (Ho et al., 2014).
Evidence supporting the use of aggressive pain control for rib fracture pain includes not only the aforementioned prevention of potential complications but also the prevention of sustained disability that can develop from the pain not being controlled aggressively enough early on, leading to chronic pain. According to the report by Gordy et al. (2014) stated that chronic pain developed in 28% of patients with rib fractures, and 40% of patients developed disabilities from chronic pain.
The limitations of this study include the retrospective nature of the study, examination of ICNB only among several possible pain control measures, and no differentiation of the pain caused by the chest tube insertion. However, this study confirmed the efficacy and the characteristics of ICNB use in patients with rib fractures.
Herein, we can conclude that ICNB has the advantage of showing dramatically more effective pain control, in comparison to conventional medications, in the initial stage of treatment of patients with thoracic injuries. However, such effect did not extend for the entire duration of the hospitalization and gradually diminished, which indicates that when the pain becomes more severe after ICNB, more aggressive pain control measures are required.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- Gordy S, Fabricant L, Ham B, Mullins R, Mayberry J. The contribution of rib fractures to chronic pain and disability. Am J Surg. 2014;207:659–663. doi: 10.1016/j.amjsurg.2013.12.012. [DOI] [PubMed] [Google Scholar]
- Ho HY, Chen CW, Li MC, Hsu YP, Kang SC, Liu EH, Lee KH. A novel and effective acupuncture modality as a complementary therapy to acute pain relief in inpatients with rib fractures. Biomed J. 2014;37:147–155. doi: 10.4103/2319-4170.117895. [DOI] [PubMed] [Google Scholar]
- Mann LJ, Young GR, Williams JK, Dent OF, McCaughan C. Intrapleural bupivacain in the control of postthoracotomy pain. Ann Thorac Surg. 1992;53:449–454. doi: 10.1016/0003-4975(92)90267-8. [DOI] [PubMed] [Google Scholar]
- Moore DC, Bridenbaugh LD. Intercostal nerve block in 4,333 patients: indications, techniques, and complications. Anesth Analg. 1962;41:1–11. [PubMed] [Google Scholar]
- Oncel M, Sencan S, Yildiz H, Kurt N. Transcutaneous nerve stimulation for pain management in patients with uncomplicated minor rib fractures. Eur J Cardiothorac Surg. 2002;22:13–17. doi: 10.1016/s1010-7940(02)00206-3. [DOI] [PubMed] [Google Scholar]
- Pederson VM, Schulze S, Hoier-Madsen K, Halkier E. Air-flow meter assessment of the effect of intercostals nerve blockage on respiratory function in rib fractures. Acta Chir Scand. 1983;149:119–120. [PubMed] [Google Scholar]
- Rauchwerger JJ, Candido KD, Deer TR, Frogel JK, Iadevaio R, Kirschen NB. Thoracic epidural steroid injection for rib fracture pain. Pain Practice. 2013;13:416–421. doi: 10.1111/j.1533-2500.2012.00596.x. [DOI] [PubMed] [Google Scholar]
- Worthley LIG. Thoracic epidural in the management of chest trauma. A study of 161 cases. Int Care Med. 1985;11:312–315. doi: 10.1007/BF00273543. [DOI] [PubMed] [Google Scholar]
- Wurnig PN, Lackner H, Teiner C, Hollaus PH, Pospisil M, Fohsl-Grande B, Osarowsky M, Pridun NS. Is intercostal block for pain management in thoracic surgery more successful than epidural anesthesia? Eur J Cardiothorac Surg. 2002;21:1115–1119. doi: 10.1016/s1010-7940(02)00117-3. [DOI] [PubMed] [Google Scholar]


