Abstract
Persistent musculoskeletal pain is common after motor vehicle collision (MVC) and often results in substantial disability. The objective of this study was to identify distributions of post-MVC pain which most interfere with specific life functions and which have the greatest interference with aggregate life function. Study data were obtained from a prospective longitudinal multicenter emergency department-based cohort of 948 European Americans experiencing MVC. Overall pain (0–10 numeric rating scale (NRS)), pain in each of 20 body regions (0–10 NRS), and pain interference (Brief Pain Inventory, 0–10 NRS) were assessed 6 weeks, 6 months, and 1 year after MVC. After adjustment for overall pain intensity, an axial distribution of pain caused the greatest interference with most specific life functions (R2 = 0.15–0.28, association p-values <.001) and with overall function. Axial pain explained more than twice as much variance in pain interference as other pain distributions. However, not all patients with axial pain had neck pain. Moderate or severe low back pain was as common as neck pain at week 6 (prevalence 37% for each) and overlapped with neck pain in only 23% of patients. Further, pain across all body regions accounted for nearly twice as much of the variance in pain interference as neck pain alone (60% vs. 34%). These findings suggest that studies of post-MVC pain should not focus on neck pain alone.
1. Introduction
Motor vehicle collisions (MVCs) result in fifty million injuries worldwide and almost four million US emergency department visits each year [36,49]. In the US, approximately 90% of individuals presenting to the emergency department (ED) for care after MVC are discharged to home after ED evaluation [41]. Health care expenses and productivity loss from persistent post-MVC pain cost an estimated $29 billion per year in the US alone [16,20]. The development of effective interventions to prevent persistent pain after MVC and the advancement of understanding to guide these interventions remain important international research priorities [29,58].
Most contemporary studies of post-MVC pain focus primarily or exclusively on pain in the neck region (e.g., [32,45]). Although pain location has been linked to function and psychological conditions in patients with chronic non-malignant pain [14,18,23] and the extent of pain has been consistently linked to pain interference in different patient populations [1,6,35], little is currently known regarding patterns of pain experienced by individuals after MVC. In addition, little is currently known regarding how these patterns of pain influence overall pain interference and specific functional disability and this influence evolves over time. A better understanding of the association between post-MVC pain distribution and functional outcomes has the potential to enrich our understanding of which individuals are at greatest risk for disability and of the functional challenges experienced by patients with specific locations/distributions of pain. Understanding how post-MVC pain location and distribution impact specific life functions would also be valuable to practitioners designing treatment interventions for individuals with persistent post-MVC pain and assessing the functional outcomes of these interventions. In addition, evaluating the influence of pain duration and of individual demographic characteristics on activity interference can provide us with additional information regarding how the functional toll of pain of a given severity and distribution changes over time.
We previously evaluated the prevalence of pain in individual body regions in the hours after MVC [8] and six weeks after MVC [33]. In these studies, we found that pain in specific body areas in the axial region (e.g. neck, shoulders, back) were most commonly reported. However, patients do not experience individual body regions of pain in isolation, but rather experience patterns of pain distributed across body regions. In this study, we sought to assess patterns of persistent pain across body regions that are common after MVC. Also, most importantly, we sought to assess the impact of different patterns of persistent pain on pain interference with specific life functions and with overall function. Because pain in axial regions has been associated with worse physical and mental health in the general population [11,31,52] and because movement of the neck and back are necessary to perform most life functions, we hypothesized that an axial distribution of pain after MVC would result in greater disability than other pain distributions. In addition, we also evaluated the influence of post-MVC pain duration and of individual sociodemographic factors (age, sex, and education) on pain-related functional interference.
2. Methods
2.1. Study design and participants
This multicenter emergency department (ED)-based observational cohort study evaluated pain and functional outcomes 6 weeks, 6 months, and 1 year after MVC. Participating centers included eight EDs in four no-fault insurance states in the U.S. (Massachusetts, Florida, Michigan, and New York). Recruitment took place between February 2009 and October 2011. Institutional Review Board approval for the study was obtained at each study site and each participant provided written informed consent. Complete information regarding study design, procedures, and methods has previously been described [39].
Eligible patients were alert, oriented English-speaking European Americans 18–65 years of age who were present to one of the study site EDs for evaluation after MVC. Patients were included regardless of the location of impact to the vehicle; location of impact has been shown to not be a strong determinant of post-MVC pain distribution [4,28]. Patients with spinal fracture or dislocation, or neurologic signs including decreased/absent deep tendon reflexes or weakness, skull fracture, facial fracture, intracranial injury, long bone fracture or laceration with significant hemorrhage, and those presenting more than 24 hours after injury were excluded, as were prisoners, pregnant patients, and individuals who cannot read English. Patients who were clinically unstable or who had potentially life-threatening injuries were also excluded.
2.2. Data collection procedures
Patients were screened and recruited by research assistants at each ED site. Baseline interviews were completed in the ED; follow-up interviews were completed via internet self-report survey or via telephone interview 6 weeks, 6 months, and 1 year after MVC. Each research assistant conducting follow-up interviews completed a study training module followed by an interview with a standardized mock patient. Comparison of mock patient data across research assistants demonstrated an error rate of 1.3%.
2.3. Measures
Demographic information (age, sex, education, relationship/marital status) was assessed during the baseline ED interview using standardized questionnaire items. Injury scoring of each patient injury was performed using the Abbreviated Injury Scale (AIS), an anatomically-based scoring system that classifies each injury according to its relative severity on a six point ordinal scale [3]. Pain intensity, distribution, and pain interference were assessed via telephone interview or a web-based questionnaire. Location and intensity of pain symptoms during the past week were assessed 6 weeks, 6 months, and 1 year after MVC using the modified Regional Pain Scale [56]. Pain intensity in each region was evaluated via numeric rating scale (NRS) from 0 (no pain) to 10 (maximum possible pain). Overall pain intensity was also assessed using the 0 to 10 NRS. Widespread pain was defined according to American College of Rheumatology 1990 criteria [57].
Pain interference with life functions was assessed using the Brief Pain Inventory (BPI) [10,26]. The relationship between pain intensity and pain interference with life function (disability) using BPI subscales has been demonstrated across multiple studies [10,26,48]. BPI subscales assess interference with seven life functions (general activity, walking ability, mood, relations with other people, sleep and enjoyment of life) on a 0–10 scale, where 0 represents “does not interfere” and 10 indicates “interferes completely” [10]. Pain interference scores assessed at 6 weeks were used in statistical analyses, except for analyses evaluating the effect of time from trauma, in which pain interference scores from the respective timepoint were used.
2.4. Statistical analyses
Values of interference subscales were averaged to calculate a pain interference total score for each individual [10]. Reliability of this score was assessed by Cronbach’s alpha and by evaluating correlation coefficients between this score and individual subscale scores.
Principal component analysis was used to reduce the dimensionality of the regional pain data (obtained from the 20-item regional pain scale) and identify specific post-MVC pain distributions. The principal component method was used to extract the components. The number of components to retain was determined by applying Kaiser-Guttman criterion [59] and by visual exploration of a scree plot. A varimax (orthogonal) and oblique rotation were applied, and the results were compared for interpretability. In interpreting the rotated factor pattern, an item was determined to load on a given component if the factor loading was 0.50 of greater for that component [19]. Items were allowed to load on more than one component only if the anatomical location of the item suggested its contribution to more than one pain region. Association of the principal components with pain interference subscales and total score was performed using a general linear model. Adjustment for participant age and sex was performed by running regression models with these predictors and outputting the residuals. The strength of association between each principal component and these residuals was evaluated using the coefficient of determination (R2).
Association of sociodemographic factors with pain interference outcomes was performed using a general linear model adjusted for overall pain intensity and pain distribution (identified using the principal component analysis described above). Association of pain extent (widespread pain vs. regional pain) was adjusted for pain intensity only.
The effect of pain duration on pain interference was assessed using a linear mixed model with pain interference total score 6 weeks, 6 months, and 1 year after MVC as outcomes. Within-subject correlation of model residuals was accounted for by using an unstructured covariance matrix. All statistical analyses were performed using SAS (version 9.2, SAS Institute Inc., Cary, NC). P-values <0.05 were considered statistically significant.
Mean pain interference total scores and bootstrap-derived 95% confidence intervals for each overall pain value were plotted, stratified by the predictor of interest (i.e. age tertile, sex, educational attainment, relationship status, widespread pain, and time of assessment). Computation of plotted statistics and figure plotting were performed using the R package ggplot2 [54].
3. Results
A total of 10,629 patients admitted to the ED after motor vehicle collision were screened, 1,416 met eligibility criteria, 969 consented to participate in the study, and 948 participants completed baseline evaluations (Fig. 1). Outcome evaluations were completed in 859/948 (91%) of participants at 6 weeks, 839/948 (89%) of participants at 6 months, and 861/948 (91%) of participants at 1 year. Socio-demographic characteristics of participants evaluated at each timepoint are presented in Table 1. Consistent with study exclusion criteria, participants had only minor injury: 99% of participants had a maximum Abbreviated Injury Scale (AIS) score of one. The remaining 1% had an AIS score of two. Pain in the head, neck, shoulder, and back regions were most common (Fig. 2); 437/859 (51%) participants had moderate or severe axial pain at 6 weeks. Individuals with pain in these regions were also most likely to report widespread pain (Fig. 2). Overall, widespread pain was present in 179/859 (21%) individuals at 6 weeks. Across follow-up timepoints, pain interference summary scores showed high reliability (Cronbach alpha 0.94–0.96) and were moderately correlated with overall pain scores (Table 2). Pain interference subscales were positively correlated with each other (Pearson correlation coefficients 0.55–0.86) (Table 2).
Figure 1.
Flowchart of the study.
Table 1.
Sociodemographic characteristics of study participants at baseline, week 6, month 6, and year 1 after motor vehicle collision.
| ED N=948 |
Week 6 N=859* |
Month 6 N=839* |
Year 1 N=861* |
|||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | (%) | n | (%) | N | (%) | n | (%) | |
| Sex | ||||||||
| Males | 373 | (39) | 321 | (37) | 318 | (38) | 321 | (37) |
| Females | 575 | (61) | 538 | (63) | 521 | (62) | 540 | (63) |
| Age tertiles | ||||||||
| 18–26 years | 315 | (33) | 272 | (32) | 263 | (31) | 272 | (32) |
| 27–41 years | 319 | (34) | 289 | (34) | 283 | (34) | 292 | (34) |
| 42–65 years | 314 | (33) | 298 | (35) | 293 | (35) | 297 | (34) |
| Education | ||||||||
| High school or less | 351 | (37) | 335 | (39) | 328 | (39) | 334 | (39) |
| Some college | 369 | (39) | 330 | (38) | 325 | (39) | 332 | (39) |
| College degree or more | 226 | (24) | 193 | (22) | 185 | (22) | 194 | (23) |
| Missing | 2 | - | 1 | - | 1 | - | 1 | - |
| Relationship | ||||||||
| None | 297 | (32) | 265 | (31) | 254 | (31) | 259 | (30) |
| Not living together | 146 | (16) | 127 | (15) | 115 | (14) | 130 | (15) |
| Living together | 492 | (53) | 457 | (54) | 460 | (55) | 462 | (54) |
| Missing | 13 | - | 10 | - | 10 | - | 10 | - |
ED=Emergency Department;
with non-missing data in the Brief Pain Inventory
Figure 2.
Prevalence of pain by body region six weeks after motor vehicle collision, and proportion of patients who had pain in each body region who had widespread pain. Widespread pain was defined according to American College of Rheumatology 1990 criteria [57].
Table 2.
Mean Brief Pain Inventory pain interference subscale scores and overall pain at week 6, month 6 and year 1.
| Scale | Intercorrelations (Pearson r) between interference subscales at week 6
|
Week 6 Mean(SD) |
Month 6 Mean(SD) |
Year 1 Mean(SD) |
|||||
|---|---|---|---|---|---|---|---|---|---|
| 1. | 2. | 3. | 4. | 5. | 6. | ||||
| Pain interference total | 2.4(2.6) | 1.6(2.4) | 1.4(2.2) | ||||||
| 1.General activity | 2.8(3.1) | 1.8(2.7) | 1.6(2.6) | ||||||
| 2.Enjoyment of life | 0.76 | 2.3(3.1) | 1.5(2.6) | 1.3(2.5) | |||||
| 3.Mood | 0.76 | 0.78 | 2.9(3.2) | 1.7(2.7) | 1.5(2.5) | ||||
| 4.Normal work | 0.86 | 0.75 | 0.73 | 2.8(3.3) | 1.8(2.9) | 1.6(2.7) | |||
| 5.Relations with other people | 0.62 | 0.74 | 0.73 | 0.64 | 1.6(2.7) | 1.1(2.4) | 0.9(2.1) | ||
| 6.Sleep | 0.71 | 0.68 | 0.68 | 0.68 | 0.60 | 2.9(3.3) | 2.0(3.0) | 1.6(2.8) | |
| 7.Walking ability | 0.67 | 0.64 | 0.60 | 0.68 | 0.57 | 0.55 | 1.5(2.6) | 1.1(2.3) | 1.1(2.3) |
| Cronbach alpha (standardized) | 0.94 | 0.95 | 0.96 | ||||||
| Overall pain intensity | 3.8(2.8) | 3.1(2.8) | 3.2(2.9) | ||||||
| Pearson r* | 0.72 | 0.70 | 0.66 | ||||||
Pearson correlation between pain interference summary score and overall pain severity (0–10 NRS).
SD=Standard Deviation.
3.1. Principal components of pain distribution at week 6 after MVC and their association with pain interference
Principal components analysis (PCA) was performed to reduce the dimensionality of pain location data. PCA of the responses to the 20-item Regional Pain Scale questionnaire at the 6-week time point identified five components with eigenvalues greater than one (termed PC1-PC5). Visual examination of a screeplot was also consistent with five meaningful factors. Together these five factors accounted for 66% of the total variance in the Regional Pain Scale.
Initially both varimax (orthogonal) and oblique rotation were performed. After oblique rotation, the correlations between the components were in the range 0.17–0.37. Both rotations yielded nearly identical interpretable distribution of scale items across the five factors (Table 3). Because orthogonal principal components allow us to assess the independent contribution (i.e., R-squared) of each component in pain interference models, orthogonal rotation is preferred even if the data suggest correlation between components [47]. Therefore, only orthogonal rotation results were retained for subsequent analyses. Pain in the hips and upper and lower legs had the highest loadings (>0.50) on PC1 (termed “Leg pain”). Head, neck, shoulders, and upper and lower back pain had the highest loadings on PC2 (“Axial pain”). Pain in the right and left sides of the jaw contributed most to PC3 (“Jaw pain”). Pain in the right shoulder, right upper arm, and right lower arm loaded on PC4 (“Right arm pain”). Finally, pain in the left upper arm, left lower arm, and chest loaded on PC5 (“Left arm pain”). Of note, shoulder pain loaded both on the corresponding arm and the axial region. Abdominal pain did not load on any of the factors.
Table 3.
Loadings of individual regional pain scores on derived principal components at week 6 after motor vehicle collision.
| Region |
 PC1 “Leg pain” |
 PC2 “Axial pain” |
 PC3 “Left arm pain” |
 PC4 “Right arm pain” |
 PC5 “Jaw pain” |
|---|---|---|---|---|---|
| Head | 0.09 | 0.64* | 0.17 | 0.16 | 32 |
| Jaw, Left Side | 0.19 | 0.19 | 0.19 | 0.06 | 0.88* |
| Jaw, Right Side | 0.25 | 0.15 | 0.12 | 0.14 | 0.88* |
| Neck | 0.11 | 0.82* | 0.12 | 0.23 | 0.16 |
| Left Shoulder | 0.02 | 0.64* | 0.51* | 0.08 | 0.05 |
| Right Shoulder | 0.10 | 0.56* | 0.08 | 0.64* | 0.06 |
| Upper Back | 0.21 | 0.76* | 0.15 | 0.16 | 0.08 |
| Left Upper Arm | 0.12 | 0.39 | 0.73* | 0.21 | 0.14 |
| Right Upper Arm | 0.20 | 0.26 | 0.23 | 0.79* | 0.14 |
| Left Lower Arm | 0.20 | 0.12 | 0.75* | 0.28 | 0.10 |
| Right Lower Arm | 0.26 | 0.07 | 0.34 | 0.75* | 0.08 |
| Chest | 0.30 | 0.09 | 0.48 | 0.20 | 0.19 |
| Abdomen | 0.41 | 0.14 | 0.25 | 0.03 | 0.21 |
| Lower Back | 0.41 | 0.67* | 0.06 | −0.05 | 0.00 |
| Left Hip | 0.60* | 0.26 | 0.39 | −0.10 | 0.14 |
| Right Hip | 0.70* | 0.29 | −0.03 | 0.21 | 0.15 |
| Left Upper Leg | 0.68* | 0.17 | 0.40 | −0.03 | 0.12 |
| Right Upper Leg | 0.78* | 0.14 | −0.01 | 0.31 | 0.07 |
| Left Lower Leg | 0.62* | 0.04 | 0.34 | 0.06 | 0.14 |
| Right Lower Leg | 0.66* | 0.03 | 0.04 | 0.30 | 0.09 |
Factor loadings >.50 are marked with (*); SD=Standard Deviation; PC=Principal Component.
Each principal component was significantly associated with each interference subscale and total interference score (all p-values <0.001). Axial pain (PC2) explained more variance in individual interference subscales (R-squared = 0.15–0.28) than pain in other regions (Fig. 3), with generally more than twice as much influence on specific aspects of disability as pain in other regions (Fig. 3). The one exception was interference in walking ability, which was best explained by leg pain (R-squared = 0.23). Left and right arm pain (PC3 and PC4) explained 2–5% of the variance in each interference subscale, and jaw pain explained less than 2% of total variance (Fig. 3). Similar results were obtained for pain and pain interference 6 months and 1 year after MVC (data not shown).
Figure 3.
Proportion of total variance (R-squared) in interference scales explained by regional pain factors, adjusted for participant age and sex.
Because axial pain was more prevalent than pain in other regions and more commonly associated with widespread pain (Fig. 2), we repeated the analyses after adjustment for number of pain regions. Axial pain continued to have the greatest influence on pain interference after adjustment. Axial pain explained at least six times more variance in the interference subscales than any other body region, with the exception of walking ability, where leg pain remained most influential (data not shown).
3.2. Sociodemographic predictors of pain interference
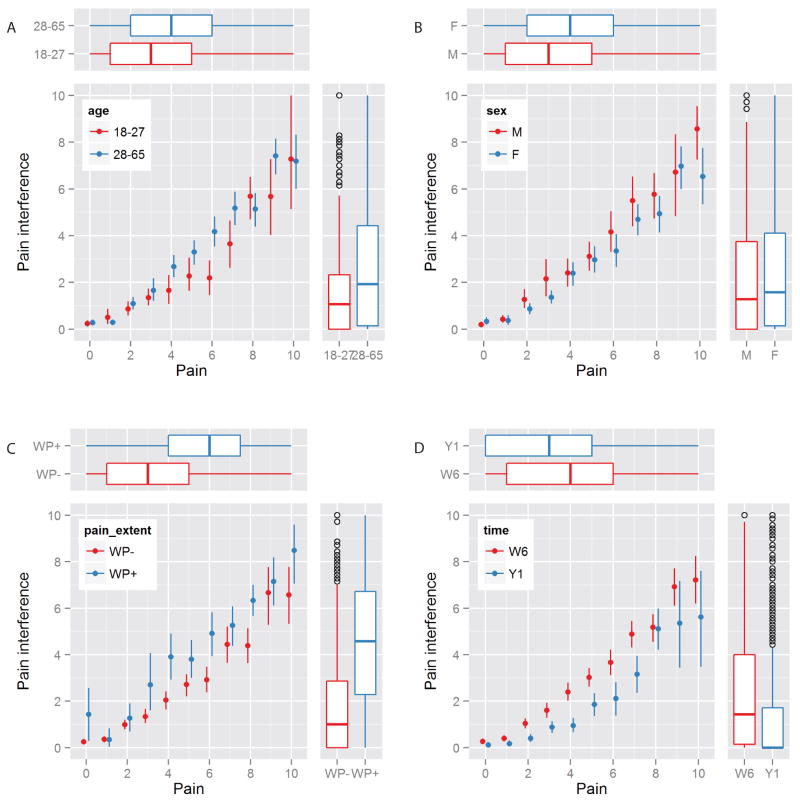
General linear models were used to assess sociodemographic predictors of pain interference, adjusting for overall pain intensity and pain distribution. Sex and age were highly significant predictors of pain interference (Table 4, Fig. 4A–B). Despite females reporting more severe overall pain than males, interference with life function from a given distribution/severity of pain was greater in males than in females. This difference was present for overall interference, and for all interference subscales except mood and walking ability (Table 4). Among the three age tertiles, the youngest group (18–26 years) reported lower pain interference in all subscales than the older age groups (27–41 and 42–65 years, Table 4 and Fig. 4A). After additional adjustment for age and sex, more educated participants reported higher pain interference with sleep, but not with other interference subscales or total interference. Relationship status was not associated with pain interference (Table 4).
Table 4.
Association of sociodemographic and pain symptom characteristics with pain interference subscale scores after motor vehicle collision. (Of note, all interference subscales scores are for the 6-week follow-up timepoint except for results presented by timepoint category.)
| Interference subscales
|
Total Interference | |||||||
|---|---|---|---|---|---|---|---|---|
| General activity | Enjoyment of life | Mood | Normal work | Relations with other people | Walking ability | Sleep | ||
| Sexa | ||||||||
| Males | 3.2 (0.1) | 2.7 (0.1) | 3.0 (0.1) | 3.2 (0.1) | 1.8 (0.1) | 1.6 (0.1) | 3.2 (0.1) | 2.7 (0.1) |
| Females | 2.6 (0.1) | 2.1 (0.1) | 2.8 (0.1) | 2.5 (0.1) | 1.4 (0.1) | 1.4 (0.1) | 2.7 (0.1) | 2.2 (0.1) |
| p-value | <.001 | <.001 | 0.37 | <.001 | 0.005 | 0.063 | 0.021 | <.001 |
| Agea | ||||||||
| 18–26 | 2.5 (0.1) | 1.9 (0.1) | 2.5 (0.1) | 2.3 (0.1) | 1.2 (0.1) | 1.2 (0.1) | 2.9 (0.2) | 2.1 (0.1) |
| 27–41 | 3.0 (0.1) | 2.7 (0.1) | 3.1 (0.1) | 3.1 (0.1) | 1.6 (0.1) | 1.5 (0.1) | 3.0 (0.1) | 2.6 (0.1) |
| 42–65 | 3.0 (0.1) | 2.4 (0.1) | 2.9 (0.1) | 3.0 (0.1) | 1.8 (0.1) | 1.7 (0.1) | 2.8 (0.1) | 2.5 (0.1) |
| p-value | 0.003 | <.001 | 0.019 | <.001 | 0.008 | 0.005 | 0.82 | <.001 |
| Educationa | ||||||||
| HS or less | 2.9 (0.1) | 2.3 (0.1) | 2.7 (0.1) | 2.9 (0.1) | 1.5 (0.1) | 1.5 (0.1) | 2.6 (0.1) | 2.4 (0.1) |
| Post-HS | 2.8 (0.1) | 2.4 (0.1) | 2.9 (0.1) | 2.8 (0.1) | 1.5 (0.1) | 1.4 (0.1) | 3.0 (0.1) | 2.4 (0.1) |
| College or more | 2.6 (0.1) | 2.1 (0.2) | 2.9 (0.2) | 2.5 (0.2) | 1.5 (0.2) | 1.5 (0.1) | 3.2 (0.2) | 2.3 (0.1) |
| p-value | 0.32 | 0.47 | 0.60 | 0.24 | 0.98 | 0.90 | 0.018 | 0.81 |
| Relationship statusa | ||||||||
| No relationship | 2.8 (0.1) | 2.4 (0.1) | 2.8 (0.1) | 2.8 (0.1) | 1.4 (0.1) | 1.6 (0.1) | 3.1 (0.2) | 2.4 (0.1) |
| Not living together | 2.7 (0.2) | 1.9 (0.2) | 2.9 (0.2) | 2.6 (0.2) | 1.8 (0.2) | 1.4 (0.2) | 2.7 (0.2) | 2.3 (0.1) |
| Living together/married | 2.9 (0.1) | 2.4 (0.1) | 2.9 (0.1) | 2.8 (0.1) | 1.5 (0.1) | 1.4 (0.1) | 2.8 (0.1) | 2.4 (0.1) |
| p-value | 0.58 | 0.10 | 0.87 | 0.73 | 0.31 | 0.21 | 0.30 | 0.79 |
| Pain distributiona | ||||||||
| Widespread | 3.9 (0.2) | 3.5 (0.2) | 3.8 (0.2) | 4.0 (0.2) | 2.6 (0.2) | 2.4 (0.2) | 3.6 (0.2) | 3.4 (0.1) |
| Regional | 2.5 (0.1) | 2.0 (0.1) | 2.6 (0.1) | 2.5 (0.1) | 1.3 (0.1) | 1.2 (0.1) | 2.7 (0.1) | 2.1 (0.1) |
| p-value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| Follow-up timepointb | ||||||||
Figure 4.
Association between pain and pain interference stratified by a) age, b) sex, c) widespread pain and d) time from trauma. Dots represent mean interference and vertical bars represent bootstrap-derived 95% confidence intervals for interference for each discrete value of the overall pain score. Boxplots represent median, lower, upper quartile and range for pain (horizontal boxplots at the top) and for pain interference (vertical boxplots at the right). M=male; F=female; WP+ =widespread pain present; WP− =no widespread pain; W6=week 6; Y1=year 1.
3.3. Widespread pain and pain interference
Pain extent was a significant predictor of pain interference, independent of the severity of pain. Participants with widespread pain had substantially higher pain interference with each of the evaluated life functions (Table 4, Fig. 4C).
3.4. Time from trauma and pain interference
After controlling for overall pain severity and pain distribution, time from trauma was inversely associated with pain interference (Table 4, Fig. 4D). Study participants reported less interference with life functions at month 6 and year 1 evaluations as compared to the week 6 evaluation, with a 38% reduction in pain interference observed between six weeks (mean interference 2.3±0.1 units) and one year (mean interference 1.4±0.1 units).
4. Discussion
In this study we sought to determine which locations/distributions of pain after MVC most interfere with specific life functions and have the greatest influence on overall disability. After adjustment for overall pain intensity, axial pain (pain in the neck, shoulders, and upper and lower back) was found to have the greatest impact on six of the seven specific life functions assessed, and also had the greatest influence on overall interference. In each of these areas, axial pain had more than twice as much impact on function as pain in other body regions. Widespread pain also had much more impact than regional pain. Pain of a specific intensity and distribution had a greater impact on disability among men and among those not in the youngest tertile of age. Across all participants, the degree of functional interference resulting from a specific intensity and distribution of pain decreased over time.
As hypothesized, we found that axial pain showed the strongest association with pain interference. Approximately half of study participants had moderate or severe axial pain at 6 weeks. However, not all patients with axial pain had neck pain. Moderate or severe low back pain was as common as neck pain at week 6 (prevalence 37% for each) and overlapped with neck pain in only 23% of patients. Further, pain across all body regions accounted for nearly twice as much of the variance in pain interference as neck pain alone (60% vs. 34%). These results indicate that pain in body regions other than the neck contributes substantially to pain-related disability after MVC, and suggest that studies of post-MVC pain outcomes should include a comprehensive assessment of pain across body regions.
These findings have several important implications for the treatment of individuals experiencing musculoskeletal pain after MVC. First, interventions seeking to achieve the greatest functional improvement should focus on axial pain outcomes, as these regions appear to have the greatest influence on disability. In addition, practitioners treating individuals with post-MVC axial pain disorders, and performing serial outcome assessments to monitor their patient’s progress, should be aware of which disability measures are most likely to be impacted by reductions in axial pain. For example, outcomes such as general activity, mood, and normal work would be valuable to assess, but walking ability is less likely to be impacted. Similar considerations apply to clinical trials of individuals with post-MVC axial pain. In addition, clinical prediction tools developed to identify those at high risk for persistent post-MVC pain should not focus on neck pain outcomes but rather should examine axial pain more generally, as this pain distribution has the greatest impact on function.
Our findings that individuals with widespread pain after MVC experienced substantially more pain interference than individuals with regional pain is consistent with previous studies [2,5,38] and suggests the importance of pain extent, as well as pain severity, on functional outcomes after MVC. Widespread musculoskeletal pain has been shown to affect working ability [34], life satisfaction and general health [5,38]. Therefore, individuals with widespread musculoskeletal pain might require more intensive treatment and also have greater potential to benefit from such treatment than individuals with localized pain.
Interestingly, while women reported more pain than men, after adjustment for overall pain intensity and distribution men reported significantly higher levels of pain interference than women. Although the majority of previous studies suggest that women are more likely to experience disability due to pain than men (i.e. [17,24,46]), a few studies found the opposite: disability was either more directly related to pain in men than in women [21], or was not associated with sex [27]. Of note, the study by Stubbs and coworkers [46] found that the difference in disability between males and females was attenuated when adjusted for pain severity. Interestingly, Hirsh and coworkers found that disability is directly related to pain in men, whereas the effect of pain on disability in women is mediated by negative mood [21]. Consistent with our work, a study by Fejer and colleagues [15], using two pain-related disability measures to evaluate the best cutoffs between mild, moderate and severe neck pain, has shown that females had a higher optimal single cutoff for neck pain than males, suggesting that females are more tolerant to pain of similar intensity than males.
In our study younger participants (18–26 years old) reported less pain interference than participants 27–65 years old. Several previous studies have observed a high prevalence of pain interference in older adults [44,50]. A population-based study of adults age 50 and older with regional pain revealed increased prevalence of pain interference among older individuals [50]. Another study found that among pain clinic patients with chronic pain, patients age 60 and older reported similar levels of pain intensity, worse physical functioning, but better mental health than younger adults with pain [55]. Similarly, advanced age has been associated with self-rated health status after controlling for pain and other socio-demographic factors among individuals 70 years and older [43]. The differences between younger and middle or older-age participants observed in our study might be explained by physiologic resilience to the effects of pain in younger adults. (For example, it has been shown experimentally that younger adults (age 18–25 years) have more active endogenous pain inhibition signaling than older adults [13]). The use of different coping mechanisms and strategies in younger patients might also contribute to this difference [25,30].
Because our study design allowed us to prospectively evaluate pain and pain interference over time after MVC, we were able to assess the effect of time on pain interference. After adjusting for pain intensity and distribution, we found that study participants experienced on average a 38% reduction in pain interference between six weeks and one year. The observed decrease in pain interference for a given level of pain speaks to the resiliency of individuals experiencing traumatic events and may be explained by the adoption of more effective methods of coping with pain over time, or by other factors. This finding is consistent with observations that quality of life improves over time after other forms of trauma [37,51,53]. This finding is also in agreement with the results by Fejer and colleagues, who evaluated the optimal cutoffs for neck pain using two measures of pain-related disability and found that the optimal single cutoff is higher for chronic neck pain than for acute and subacute neck pain [15].
Several limitations should be considered when interpreting our study results. First, the participants in our study were European Americans age 18 to 65 years of age who presented to the ED for evaluation. The extent of pain following MVC and determinants of widespread pain may differ in other ethnic and racial groups, older adults [40], and individuals who do not come to the emergency department for evaluation after MVC. In addition, our study did not adjust for factors such as comorbid conditions [12,42], psychological distress [9], expectations of recovery [22], or insurance and litigation [7,33] when evaluating the association between pain patterns and disability. These factors have been shown to predict pain outcomes. However, our goal was to describe cross-sectional associations between pain locations and pain-related disability. We did not attempt to assess the causal relationship between pain location and disability, independent of all other factors. This might a valuable area of future inquiry. Additionally, our study focused on individuals who were evaluated in the ED and subsequently discharged to home, a population which comprises approximately 90% of all patients seen in U.S. EDs after MVC. The pain experiences may differ among those patients experiencing more serious injuries who are admitted to the hospital. Although 99% of study participants had only minor injury (an AIS score of 1), more subtle differences in injury severity were not measured, and such differences may have explained some of the observed variation in pain and pain interference by age, gender, and pain location. Finally, no data were available for the first few weeks after MVC. Knowing the early trajectory of pain and pain related interference in this population may be important to fully characterize the post-MVC outcomes.
In conclusion, our study results indicate that after controlling for pain severity, axial and widespread pain result in greater pain interference after MVC than non-axial or more localized pain. Interventions seeking to achieve the greatest functional improvement in post-MVC pain should focus on axial pain or widespread pain, as these regions appear to have the greatest influence on disability. In addition, ED-based clinical prediction tools should be developed which are informed by the extensive previous literature on chronic pain risk factors and identify adults at high risk of developing axial pain. Finally, practitioners treating individuals with post-MVC pain disorders, and performing serial outcome assessments to monitor their patient’s progress, should select disability measures most impacted by reductions in their patient’s specific pain distribution.
SUMMARY.
In this prospective study (n = 948), axial and widespread pain had the greatest influence on life interference during the year after MVC.
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R01AR056328 (McLean) and the National Institute on Aging of the National Institutes of Health under Award Number K23AG038548 (Platts-Mills). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The authors report no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Amris K, Waehrens EE, Jespersen A, Bliddal H, Danneskiold-Samsoe B. Observation-based assessment of functional ability in patients with chronic widespread pain: a cross-sectional study. Pain. 2011;152(11):2470–2476. doi: 10.1016/j.pain.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 2.Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Characteristics of subjects with chronic pain, in relation to local and widespread pain report. A prospective study of symptoms, clinical findings and blood tests in subgroups of a geographically defined population. Scand J Rheumatol. 1996;25(3):146–154. doi: 10.3109/03009749609080005. [DOI] [PubMed] [Google Scholar]
- 3.Baker SP, O’Neill B, Haddon W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 4.Berglund A, Alfredsson L, Jensen I, Cassidy JD, Nygren A. The association between exposure to a rear-end collision and future health complaints. J Clin Epidemiol. 2001;54(8):851–856. doi: 10.1016/s0895-4356(00)00369-3. [DOI] [PubMed] [Google Scholar]
- 5.Bergman S, Jacobsson LT, Herrstrom P, Petersson IF. Health status as measured by SF-36 reflects changes and predicts outcome in chronic musculoskeletal pain: a 3-year follow up study in the general population. Pain. 2004;108(1–2):115–123. doi: 10.1016/j.pain.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Birley T, Goebel A. Widespread Pain in Patients with Complex Regional Pain Syndrome. Pain Pract. 2013 doi: 10.1111/papr.12092. [DOI] [PubMed] [Google Scholar]
- 7.Blyth FM, March LM, Nicholas MK, Cousins MJ. Chronic pain, work performance and litigation. Pain. 2003;103(1–2):41–47. doi: 10.1016/s0304-3959(02)00380-9. [DOI] [PubMed] [Google Scholar]
- 8.Bortsov AV, Platts-Mills TF, Peak DA, Jones JS, Swor RA, Domeier RM, Lee DC, Rathlev NK, Hendry PL, Fillingim RB, McLean SA. Pain distribution and predictors of widespread pain in the immediate aftermath of motor vehicle collision. Eur J Pain. 2013;17(8):1243–1251. doi: 10.1002/j.1532-2149.2013.00285.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castro WH, Meyer SJ, Becke ME, Nentwig CG, Hein MF, Ercan BI, Thomann S, Wessels U, Du Chesne AE. No stress--no whiplash? Prevalence of “whiplash” symptoms following exposure to a placebo rear-end collision. Int J Legal Med. 2001;114(6):316–322. doi: 10.1007/s004140000193. [DOI] [PubMed] [Google Scholar]
- 10.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 11.Cote P, Cassidy JD, Carroll L The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 1998;23(15):1689–1698. doi: 10.1097/00007632-199808010-00015. [DOI] [PubMed] [Google Scholar]
- 12.Dominick CH, Blyth FM, Nicholas MK. Unpacking the burden: understanding the relationships between chronic pain and comorbidity in the general population. Pain. 2012;153(2):293–304. doi: 10.1016/j.pain.2011.09.018. [DOI] [PubMed] [Google Scholar]
- 13.Edwards RR, Fillingim RB, Ness TJ. Age-related differences in endogenous pain modulation: a comparison of diffuse noxious inhibitory controls in healthy older and younger adults. Pain. 2003;101(1–2):155–165. doi: 10.1016/s0304-3959(02)00324-x. [DOI] [PubMed] [Google Scholar]
- 14.Eggermont LH, Bean JF, Guralnik JM, Leveille SG. Comparing pain severity versus pain location in the MOBILIZE Boston study: chronic pain and lower extremity function. J Gerontol A Biol Sci Med Sci. 2009;64(7):763–770. doi: 10.1093/gerona/glp016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fejer R, Jordan A, Hartvigsen J. Categorising the severity of neck pain: establishment of cut-points for use in clinical and epidemiological research. Pain. 2005;119(1–3):176–182. doi: 10.1016/j.pain.2005.09.033. [DOI] [PubMed] [Google Scholar]
- 16.Freeman MD, Croft AC, Rossignol AM, Weaver DS, Reiser M. A review and methodologic critique of the literature refuting whiplash syndrome. Spine (Phila Pa 1976) 1999;24(1):86–96. doi: 10.1097/00007632-199901010-00022. [DOI] [PubMed] [Google Scholar]
- 17.Greenspan JD, Craft RM, LeResche L, Arendt-Nielsen L, Berkley KJ, Fillingim RB, Gold MS, Holdcroft A, Lautenbacher S, Mayer EA, Mogil JS, Murphy AZ, Traub RJ. Studying sex and gender differences in pain and analgesia: a consensus report. Pain. 2007;132 (Suppl 1):S26–45. doi: 10.1016/j.pain.2007.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gronblad M, Jarvinen E, Airaksinen O, Ruuskanen M, Hamalainen H, Kouri JP. Relationship of subjective disability with pain intensity, pain duration, pain location, and work-related factors in nonoperated patients with chronic low back pain. Clin J Pain. 1996;12(3):194–200. doi: 10.1097/00002508-199609000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Hair JF, Anderson RE, Tatham RL, Black WC, editors. |. Title|, Vol. Volume|. City|: Publisher|, Year|. [Google Scholar]
- 20.Hartling L, Brison RJ, Ardern C, Pickett W. Prognostic value of the Quebec Classification of Whiplash-Associated Disorders. Spine (Phila Pa 1976) 2001;26(1):36–41. doi: 10.1097/00007632-200101010-00008. [DOI] [PubMed] [Google Scholar]
- 21.Hirsh AT, Waxenberg LB, Atchison JW, Gremillion HA, Robinson ME. Evidence for sex differences in the relationships of pain, mood, and disability. J Pain. 2006;7(8):592–601. doi: 10.1016/j.jpain.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Holm LW, Carroll LJ, Cassidy JD, Skillgate E, Ahlbom A. Expectations for recovery important in the prognosis of whiplash injuries. PLoS Med. 2008;5(5):e105. doi: 10.1371/journal.pmed.0050105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jordan KP, Sim J, Moore A, Bernard M, Richardson J. Distinctiveness of long-term pain that does not interfere with life: an observational cohort study. Eur J Pain. 2012;16(8):1185–1194. doi: 10.1002/j.1532-2149.2012.00118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: the role of catastrophizing. Pain. 2000;87(3):325–334. doi: 10.1016/S0304-3959(00)00296-7. [DOI] [PubMed] [Google Scholar]
- 25.Keefe FJ, Williams DA. A comparison of coping strategies in chronic pain patients in different age groups. J Gerontol. 1990;45(4):P161–165. doi: 10.1093/geronj/45.4.p161. [DOI] [PubMed] [Google Scholar]
- 26.Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, Cleeland CS. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004;20(5):309–318. doi: 10.1097/00002508-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Keogh E, McCracken LM, Eccleston C. Gender moderates the association between depression and disability in chronic pain patients. Eur J Pain. 2006;10(5):413–422. doi: 10.1016/j.ejpain.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 28.Krafft M, Kullgren A, Tingvall C, Bostrom O, Fredriksson R. How crash severity in rear impacts influences short- and long-term consequences to the neck. Accid Anal Prev. 2000;32(2):187–195. doi: 10.1016/s0001-4575(99)00083-4. [DOI] [PubMed] [Google Scholar]
- 29.Lamb SE, Gates S, Williams MA, Williamson EM, Mt-Isa S, Withers EJ, Castelnuovo E, Smith J, Ashby D, Cooke MW, Petrou S, Underwood MR. Emergency department treatments and physiotherapy for acute whiplash: a pragmatic, two-step, randomised controlled trial. Lancet. 2013;381(9866):546–556. doi: 10.1016/S0140-6736(12)61304-X. [DOI] [PubMed] [Google Scholar]
- 30.Lefebvre JC, Lester N, Keefe FJ. Pain in young adults. II: The use and perceived effectiveness of pain-coping strategies. Clin J Pain. 1995;11(1):36–44. [PubMed] [Google Scholar]
- 31.Linton SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976) 2000;25(9):1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 32.McLean SA. The potential contribution of stress systems to the transition to chronic whiplash-associated disorders. Spine. 2011;36(25 Suppl):S226–232. doi: 10.1097/BRS.0b013e3182387fb4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McLean SA, Ulirsch JC, Slade GD, Soward AC, Swor RA, Peak DA, Jones JS, Rathlev NK, Lee DC, Domeier RM, Hendry PL, Bortsov AV, Bair E. Incidence and predictors of neck and widespread pain after motor vehicle collision among US litigants and nonlitigants. Pain. 2014;155(2):309–321. doi: 10.1016/j.pain.2013.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miranda H, Kaila-Kangas L, Heliovaara M, Leino-Arjas P, Haukka E, Liira J, Viikari-Juntura E. Musculoskeletal pain at multiple sites and its effects on work ability in a general working population. Occup Environ Med. 2010;67(7):449–455. doi: 10.1136/oem.2009.048249. [DOI] [PubMed] [Google Scholar]
- 35.Miro J, Gertz KJ, Carter GT, Jensen MP. Pain Location and Functioning in Persons With Spinal Cord Injury. PM R. 2014 doi: 10.1016/j.pmrj.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Report. 2010;(26):1–31. [PubMed] [Google Scholar]
- 37.Oster C, Willebrand M, Ekselius L. Health-related quality of life 2 years to 7 years after burn injury. J Trauma. 2011;71(5):1435–1441. doi: 10.1097/TA.0b013e318208fc74. [DOI] [PubMed] [Google Scholar]
- 38.Peolsson M, Borsbo B, Gerdle B. Generalized pain is associated with more negative consequences than local or regional pain: a study of chronic whiplash-associated disorders. J Rehabil Med. 2007;39(3):260–268. doi: 10.2340/16501977-0052. [DOI] [PubMed] [Google Scholar]
- 39.Platts-Mills TF, Ballina L, Bortsov AV, Soward A, Swor RA, Jones JS, Lee DC, Peak DA, Domeier RM, Rathlev NK, Hendry PL, McLean SA. Using emergency department-based inception cohorts to determine genetic characteristics associated with long term patient outcomes after motor vehicle collision: methodology of the CRASH study. BMC Emerg Med. 2011;11:14. doi: 10.1186/1471-227X-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Platts-Mills TF, Burke GF, Lee YM, Swor RA, Zaleski EZ, Clauw DJ, McLean SA. Pain and interference of pain with function and mood in elderly adults involved in a motor vehicle collision: a pilot study. Exp Aging Res. 2012;38(3):330–343. doi: 10.1080/0361073X.2012.672139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Platts-Mills TF, Hunold KM, Esserman DA, Sloane PD, McLean SA. Motor Vehicle Collision-related Emergency Department Visits by Older Adults in the United States. Acad Emerg Med. 2012;19(7):821–827. doi: 10.1111/j.1553-2712.2012.01383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rethelyi JM, Berghammer R, Kopp MS. Comorbidity of pain-associated disability and depressive symptoms in connection with sociodemographic variables: results from a cross-sectional epidemiological survey in Hungary. Pain. 2001;93(2):115–121. doi: 10.1016/S0304-3959(01)00301-3. [DOI] [PubMed] [Google Scholar]
- 43.Reyes-Gibby CC, Aday L, Cleeland C. Impact of pain on self-rated health in the community-dwelling older adults. Pain. 2002;95(1–2):75–82. doi: 10.1016/s0304-3959(01)00375-x. [DOI] [PubMed] [Google Scholar]
- 44.Scudds RJ, Ostbye T. Pain and pain-related interference with function in older Canadians: the Canadian Study of Health and Aging. Disabil Rehabil. 2001;23(15):654–664. doi: 10.1080/09638280110043942. [DOI] [PubMed] [Google Scholar]
- 45.Sterling M, Hendrikz J, Kenardy J, Kristjansson E, Dumas JP, Niere K, Cote J, Deserres S, Rivest K, Jull G. Assessment and validation of prognostic models for poor functional recovery 12 months after whiplash injury: a multicentre inception cohort study. Pain. 2012;153(8):1727–1734. doi: 10.1016/j.pain.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 46.Stubbs D, Krebs E, Bair M, Damush T, Wu J, Sutherland J, Kroenke K. Sex Differences in Pain and Pain-Related Disability among Primary Care Patients with Chronic Musculoskeletal Pain. Pain Med. 2010;11(2):232–239. doi: 10.1111/j.1526-4637.2009.00760.x. [DOI] [PubMed] [Google Scholar]
- 47.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. Allyn & Bacon, Inc; 2006. [Google Scholar]
- 48.Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic nonmalignant pain. J Pain. 2004;5(2):133–137. doi: 10.1016/j.jpain.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 49.Tanskanen A, Hintikka J, Honkalampi K, Haatainen K, Koivumaa-Honkanen H, Viinamaki H. Impact of multiple traumatic experiences on the persistence of depressive symptoms - a population-based study. Nord J Psychiat. 2004;58(6):459–464. doi: 10.1080/08039480410011687. [DOI] [PubMed] [Google Scholar]
- 50.Thomas E, Peat G, Harris L, Wilkie R, Croft PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP) Pain. 2004;110(1–2):361–368. doi: 10.1016/j.pain.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 51.Toien K, Bredal IS, Skogstad L, Myhren H, Ekeberg O. Health related quality of life in trauma patients. Data from a one-year follow up study compared with the general population. Scand J Trauma Resusc Emerg Med. 2011;19:22. doi: 10.1186/1757-7241-19-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Webb R, Brammah T, Lunt M, Urwin M, Allison T, Symmons D. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine (Phila Pa 1976) 2003;28(11):1195–1202. doi: 10.1097/01.BRS.0000067430.49169.01. [DOI] [PubMed] [Google Scholar]
- 53.Westgren N, Levi R. Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil. 1998;79(11):1433–1439. doi: 10.1016/s0003-9993(98)90240-4. [DOI] [PubMed] [Google Scholar]
- 54.Wickham H. ggplot2: elegant graphics for data analysis. Springer Inc; 2009. [Google Scholar]
- 55.Wittink HM, Rogers WH, Lipman AG, McCarberg BH, Ashburn MA, Oderda GM, Carr DB. Older and younger adults in pain management programs in the United States: differences and similarities. Pain Med. 2006;7(2):151–163. doi: 10.1111/j.1526-4637.2006.00113.x. [DOI] [PubMed] [Google Scholar]
- 56.Wolfe F. Pain extent and diagnosis: development and validation of the regional pain scale in 12,799 patients with rheumatic disease. J Rheumatol. 2003;30(2):369–378. [PubMed] [Google Scholar]
- 57.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 58.Yadla S, Ratliff JK, Harrop JS. Whiplash: diagnosis, treatment, and associated injuries. Curr Rev Musculoskelet Med. 2008;1(1):65–68. doi: 10.1007/s12178-007-9008-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yeomans KA, Golder PA. The Guttman-Kaiser Criterion as a Predictor of the Number of Common Factors. J Roy Stat Soc D-Sta. 1982;31(3):221–229. [Google Scholar]