Abstract
Primary cutaneous aspergillosis (PCA) is a rare fungal infection in premature infants. Extreme prematurity, immature immune system, therapy with broad-spectrum antibiotics and systemic steroids, as well as hyperglycaemia and a vulnerable and very thin epidermal layer are considered risk factors in this patient population. We present a premature male infant born at 24+3 weeks of gestation with PCA, successfully treated with amphotericin and surgical curettage of the ulcerating skin lesions. Complete resolution of the lesions was achieved and scarring was barely visible at later follow-up.
Background
Very premature neonates are at particular risk for opportunistic fungal infections. This is due to various factors including immature immune system, frequent and often prolonged use of broad-spectrum antibiotics, susceptibility to hyperglycaemia and the use of corticosteroids. Being nursed in a humid environment and thus at risk for skin maceration, they may experience breaches of the skin barrier all of which increases the risk of infections. Nearly all fungal infections in premature infants are caused by the Candida species, with other fungi accounting for a very limited number of cases.
Primary cutaneous aspergillosis (PCA) is a rare fungal infection in premature infants, that may cause extensive tissue destruction as well as systemic illness with high mortality rates. Early recognition and treatment are essential for a successful outcome. We report a case of PCA in an extremely low birth weight male infant. Surgical excision of localised lesions combined with prompt diagnosis and early specific treatment led to rapid near-complete resolution of the skin lesions.
Case presentation
A male preterm infant was born to a 28-year-old mother at 24+3 weeks of gestation due to preterm labour, with a birth weight of 750 g. The baby was delivered vaginally shortly after admission of the mother, therefore no antenatal steroid was given. The APGAR score was 6 and 7, at 1 and 5 min, respectively. The patient developed respiratory distress syndrome requiring intubation and a total of two doses of surfactant. Owing to presumed sepsis, he was started on ampicillin and gentamicin. The antibiotics were stopped after 72 h, as blood cultures taken at birth remained negative. On the fourth day of life (DOL), he developed severe, persistent hyperglycaemia requiring intravenous insulin over the next 3 weeks. Owing to feeding intolerance, periumbilical erythaema and an increase in neutrophil bands (20%), the patient was restarted on antibiotics on the fifth DOL. Blood cultures grew Enterococcus faecalis, and antibiotic therapy with amoxicillin/clavulanic acid according to antimicrobial susceptibility was continued for a total of 7 days. During the antimicrobial therapy, the infant developed several discrete vesicles in the right inguinal region, which over the next few days slowly progressed to raised, indurated erythematous nodules with yellow crusted central necrosis (figure 1), eventually leaving clusters of deep necrotic ulcers (figure 2). On initial clinical suspicion of a cutaneous pseudomonal infection, the antibiotic therapy was changed to cefepime. Surgical and dermatological consults were obtained and excision of the necrotic tissue along with biopsies to rule out PCA was suggested.
Figure 1.

Erythematous, indurated papules with central, yellow crusted necrosis 7 days after initial presentation of skin lesions.
Figure 2.

Progressive central ulceration on day 10.
Investigations
Swabs of the lesions grew Enterobacter cloacae and Aspergillus fumigatus. A small increase in neutrophil bands was seen as the lesions appeared, with an otherwise unremarkable white cell count. C reactive protein remained normal. The skin biopsies confirmed the suspected fungal aetiology (figures 3 and 4).
Figure 3.
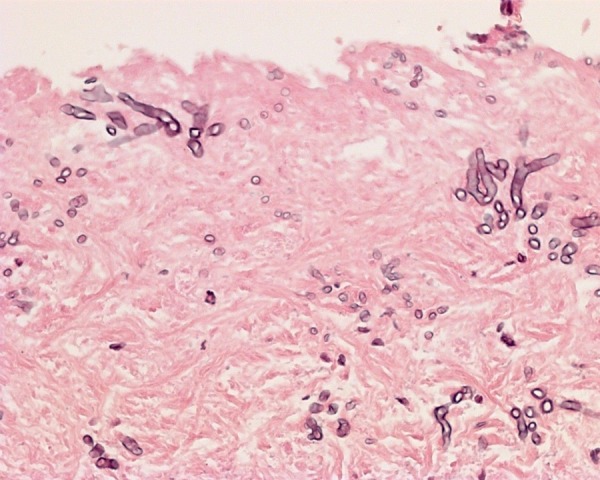
H&E, ×400. Necrosis colonised by conidia and some dichotomously branching hyphae. The mycotic colonisation is mainly seen in necrotic tissue without significant inflammatory infiltration.
Figure 4.
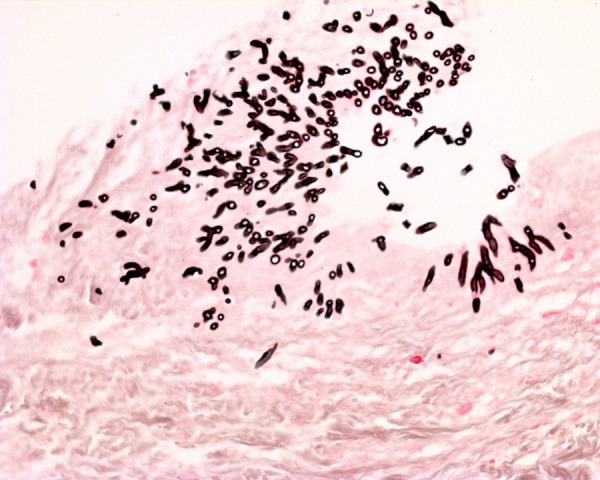
Grocott's silver stain, ×400. Necrosis colonised by conidia and some dichotomously branching hyphae.
Differential diagnosis
The lesions of PCA could be mistaken for bullous impetigo caused by Staphylococcus aureus, ecthyma gangrenosum secondary to pseudomonas or thermal burns from tcCO2 probe placement. Our patient was given antibiotics to cover for pseudomonas until wound swabs ruled out this cause. The location and the progressive changes in the initial lesion were not typical of any burns.
Treatment
The condition was successfully treated with liposomal amphotericin 5 mg/kg/day for 14 days and surgical excision of necrotic parts of the lesions. An immediate improvement was seen, but the deep ulcers left extensive inguinal scarring. Physiotherapy was started to avoid hip contractures as well as daily moisturising cream application to keep the skin soft.
Outcome and follow-up
The clinical course in the following weeks was further complicated by the development of necrotising enterocolitis (NEC) necessitating long-term parenteral nutrition, catheter-associated sepsis and cholestasis. NEC was treated conservatively, but intestinal stenosis requiring surgery became evident on resuming enteral feeding.
The aspergillus infection left scars that were still visible at later follow-up examinations; there were no signs of contractures. Despite a very complicated neonatal course with several infections and NEC, the neurodevelopmental outcome of this patient appears to be satisfactory. At the follow-up examination at corrected age of 20 months, no delays in motor and mental development were detected.
Discussion
Few cases of PCA in the very low birth weight population have been published in the literature.1–4 Most were extremely premature infants with high mortality rates due to secondary systemic infections and often with a delay in diagnosis and treatment. The combination of initial unspecific and variable skin changes, the rarity of the condition as well as the difficulties in obtaining an early clinical and microbiological diagnosis, increase the risk of a delay in instituting effective antifungal therapy. Biopsy is usually necessary to confirm the condition. In our patient the skin lesions initially presented as discrete papules during treatment for suspected sepsis. As they changed to a more necrotic appearance 6 days after initial presentation, suggesting that a pseudomonal or fungal infection might be the cause, the first swabs were taken. Biopsy carried out 3 days later confirmed the diagnosis. Antifungal treatment was instituted 11 days after eruption of the initial skin changes. In our case, there was a significant delay between first symptoms and diagnosis, and the outcome might not have been that favourable if early secondary systemic involvement had occurred.
Aspergillus is a ubiquitous mould easily isolated from air, soil and dust. Outbreaks of aspergillus infections in neonatal intensive care units (NICUs) have been reported in association with humidifying chambers of incubators, adhesive taping, gauze and non-sterile gloves as possible reservoirs.5 6 Singer et al7 describe an outbreak of aspergillosis in a NICU in which three of four infected preterm infants died due to secondary systemic infection. The source of the infection proved to be contaminated latex finger stalls. An association with construction work in the NICU surroundings, which may stir up spores, has been suggested. An infant in the incubator next to our patient also developed a macerated erythematous rash, which grew aspergillus on skin swab culture, but the skin changes resolved quickly without treatment. A search in the NICU environment for possible reservoirs was undertaken by the hospital infection control team, but without positive results. There was no construction work or renovation going on at this time.
Our patient had many of the risk factors associated with fungal infections in preterm infants. His extreme prematurity might be considered the basis of all other risks, including exposure to broad-spectrum antibiotics with potentially profound impact on skin microbiota composition, hyperglycaemia requiring insulin and repeated skin breaches in an environment with high ambient humidity. Despite the time delay between eruptions of the lesions until definitive diagnosis, our patient was successfully treated with liposomal amphotericin B and surgical curettage of the necrotic tissue. We chose to treat with a high dose of liposomal amphotericin recommended for invasive fungal infections and for a total of 14 days. In cases of PCA refractory to amphotericin, successful treatment with voriconazole has been reported in the literature.8 9 Owing to an immediate clinical response, our patient did not need additional antifungal treatment.
Learning points.
Primary cutaneous aspergillosis should be suspected in the extremely low birth weight population with rapidly progressive necrotic/ulcerating skin lesions.
A skin biopsy is usually necessary to confirm the diagnosis.
Prompt diagnosis and treatment with systemic antifungal therapy, and possibly surgical curettage, increases the chances of a favourable outcome.
Footnotes
Contributors: BR performed the literature review, collected clinical details, photographs and drafted the manuscript. PAD provided photographs and description of the histology. CK and JM revised the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Woodruff CA, Hebert AA. Neonatal primary cutaneous aspergillosis: case report and review of the literature. Pediatr Dermatol 2002;19:439–44 [DOI] [PubMed] [Google Scholar]
- 2.Andresen J, Nygaard EA, Størdal K. Primary cutaneous aspergillosis (PCA)—a case report. Acta Paediatr 2005;94:761–2 [DOI] [PubMed] [Google Scholar]
- 3.Herron MD, Vanderhooft SL, Byington C, et al. Aspergillosis in a 24-week newborn: a case report. J Perinatol 2003;23:256–9 [DOI] [PubMed] [Google Scholar]
- 4.Erişir-Oygucu S, Akcan AB, Oygür N. Primary cutaneous aspergillosis in an extremely low birth weight preterm. Turk J Pediatr 2009;51:621–3 [PubMed] [Google Scholar]
- 5.Stock C, Veyrier M, Raberin H, et al. Severe cutaneous aspergillosis in a premature neonate linked to nonsterile disposable glove contamination? Am J Infect Control 2012;40:465–7 [DOI] [PubMed] [Google Scholar]
- 6.Etienne KA, Subudhi CP, Chadwick PR, et al. Investigation of a cluster of cutaneous aspergillosis in a neonatal intensive care unit. J Hosp Infect 2011;79:344–8 [DOI] [PubMed] [Google Scholar]
- 7.Singer S, Singer D, Rüchel R, et al. Outbreak of systemic aspergillosis in a neonatal intensive care unit. Mycoses 1998;41:223–7 [DOI] [PubMed] [Google Scholar]
- 8.Santos RP, Sánchez PJ, Mejias A, et al. Successful medical treatment of cutaneous aspergillosis in a premature infant using liposomal amphotericin B, voriconazole and micafungin. Pediatr Infect Dis J 2007;26:364–6 [DOI] [PubMed] [Google Scholar]
- 9.Frankenbusch K, Eifinger F, Kribs A, et al. Severe primary cutaneous aspergillosis refractory to amphotericin B and the successful treatment with systemic voriconazole in two premature infants with extremely low birth weight. J Perinatol 2006;26:511–14 [DOI] [PubMed] [Google Scholar]


