Abstract
Osteomyelitis caused by Candida glabrata is rare and its optimal treatment is unknown. Here we report a case of osteomyelitis caused by C. glabrata in the distal phalanx in a 54-year-old woman. Despite partial resection of the nail and administering a 1-month course of antibiotics for paronychia, the local swelling remained and an osteolytic lesion was found. C. glabrata osteomyelitis of the distal phalanx was later diagnosed after curettage. Thereafter, the patient was treated with antifungal agents for 3 months. The infection eventually resolved, and radiological healing of the osteolytic lesion was achieved. Antifungal susceptibility testing should be performed in the case of osteomyelitis caused by nonalbicans Candida species, due to their resistance to fluconazole.
1. Introduction
Invasive candidiasis has increased in prevalence with the increase in the elderly population, but Candida osteomyelitis is relatively rare [1]. The most frequent mechanism of bone infection in Candida osteomyelitis is hematogenous dissemination, and the most commonly affected sites in adults are the vertebra, ribs, and sternum [2, 3]. We report a case of osteomyelitis caused by C. glabrata affecting the distal phalanx of the middle finger, which was successfully treated with operative debridement followed by a 3-month course of antifungal treatment.
2. Case Report
A 54-year-old woman with a treatment history of hypertension presented with progressive pain in the left middle finger, which had persisted for the past 4 months. She worked as an esthetician scrubbing scurf and had been treated by a local doctor when her pain first developed. She underwent partial resection for an ingrown nail and received antibiotics treatment for paronychia of the finger. When her condition did not improve, she was referred to our department because of residual pain and osteomyelitis suspected from local inflammatory findings.
The fingertip was swollen with scales around the nail wall (Figure 1). Radiography revealed osteolysis and disruption of the ulnar cortical bone of the distal phalanx. Her white blood cell count was 5.3 × 103/mm3 and C-reactive protein was 0.03 mg/dL. Magnetic resonance imaging of the finger revealed diffuse high signal intensity in the bone marrow of the distal phalanx and a subcutaneous fluid-like lesion with an isosignal intensity area on T1 weighted images and a high signal intensity area on T2 weighted images (Figure 2).
Figure 1.

Anteroposterior and lateral radiographs at the first presentation.
Figure 2.
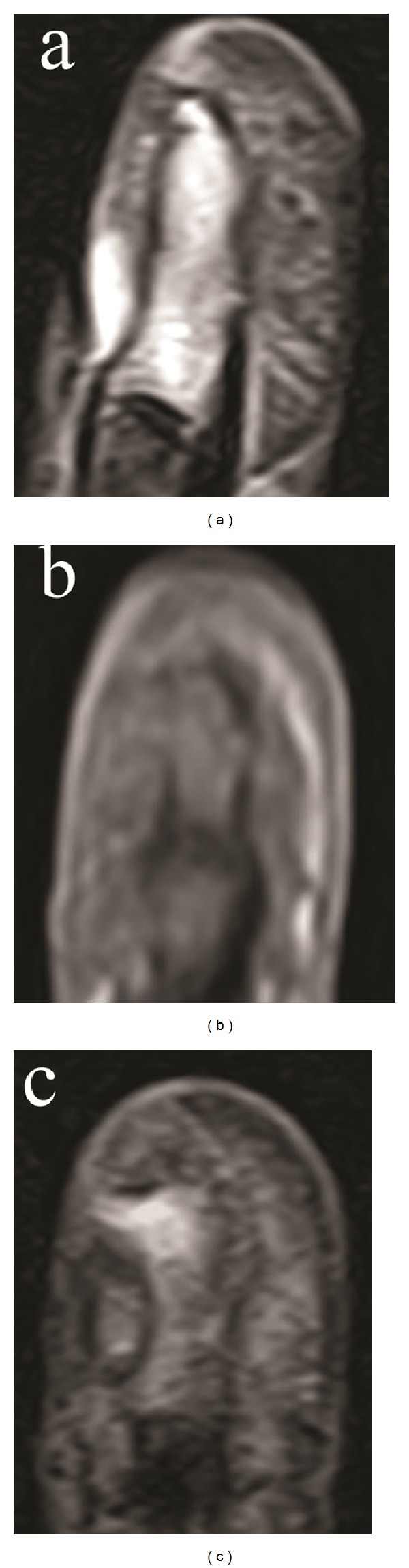
Sagittal view of short time inversion recovery magnetic resonance images (MRI) (a) and coronal views of T1 weighted (b) and T2 weighted (c) MRI.
Debridement and curettage were performed via the ulnar midlateral approach. A partial defect of the cortical bone, through which surrounding subcutaneous tissue is connected to the bone marrow, was noted. A small amount of pus-like fluid was aspirated from a cavity in the distal phalanx (Figure 3). The distal interphalangeal joint was immobilized postoperatively with a splint for 2 months.
Figure 3.

Intraoperative findings showing a partial defect of the ulnar cortical bone of the distal phalanx.
Flomoxef sodium (2,000 mg/day) was given intravenously for 7 days postoperatively. C. glabrata was detected in fluid culture, and histological findings showed a granuloma with lymphocyte infiltration and a small quantity of spores (Figure 4). Intravenous itraconazole (400 mg/day) was given for 3 days, followed by intravenous fluconazole (200 mg/day) for 5 days due to the side effects of itraconazole. The patient was further treated with oral flucytosine (3,000 mg/day) for 3 months. Her clinical findings improved and her pain disappeared within 1 month after surgery, and she returned to work 2 months after surgery. At the final followup (10 months after surgery), new bone formation was seen at the bone defect in the distal phalanx and the cortical bone disruption was healed with no recurrence of inflammation (Figure 5).
Figure 4.
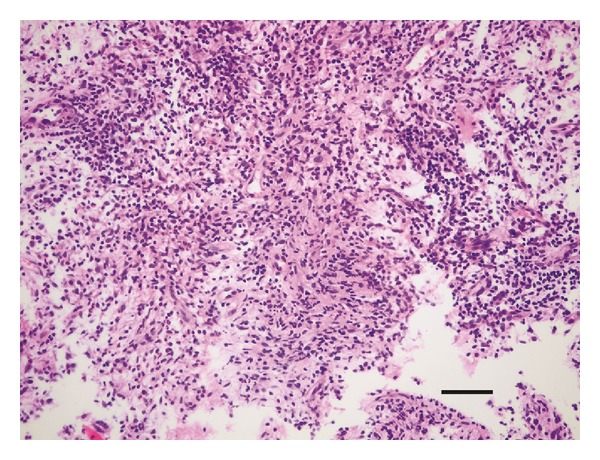
Histological findings of the lesion (hematoxylin eosin staining). The scale bar indicates 50 μm.
Figure 5.
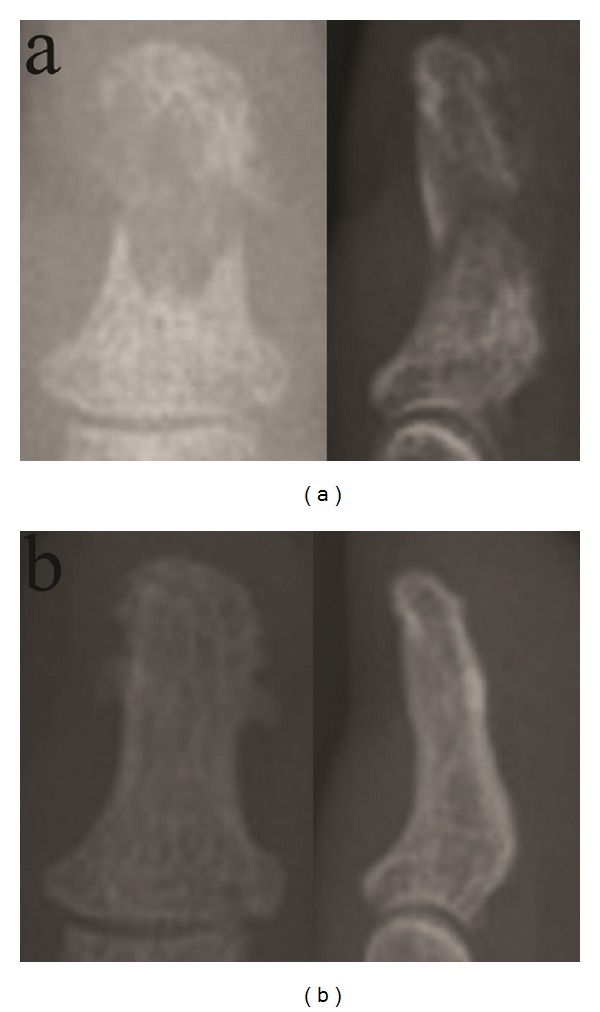
Anteroposterior and lateral radiographs at 1 month (a) and 10 months (b) after surgery.
3. Discussion
Candida osteomyelitis is relatively rare, with most reports limited to case descriptions and a few case series. On the other hand invasive candidiasis is becoming more prevalent as medicine continues to change, including the extensive use of prophylactic antifungal agents, broad-spectrum antibacterial agents, and medical devices (e.g., chronic indwelling intravascular catheters) and the patient population continues to change [1]. In the case of Candida osteomyelitis, the mechanisms of bone infection are classified as follows: hematogenous dissemination (67%), direct inoculation (25%), and contiguous infection (9%) [2]. The most common infecting species are C. albicans (69%), C. tropicalis (15%), and C. glabrata (8%) [3], and the most commonly affected sites in adults are the vertebra, ribs, and sternum. Candida osteomyelitis of the phalanx is relatively rare [2, 4, 5].
Candida is now recognized to be a cause of deep-site infections, including osteomyelitis, in patients with risk factors such as diabetes mellitus, deficient cell-mediated immunity, neutropenia, steroid use, central catheter insertion, total parenteral nutrition, and a prior history of broad-spectrum antimicrobials use. C. glabrata is an increasingly important cause of candidemia, now accounting for about one quarter of Candida bloodstream infections in the United States [6]. However, osteomyelitis caused by C. glabrata is a relatively rare condition and, to our knowledge, only a few cases have been reported [7–10]. The present case of osteomyelitis was caused by C. glabrata affecting the distal phalanx of the middle finger but without any of those risk factors. In addition, chronic paronychia caused by Candida species occurs generally among workers with the exposure to excessive moisture [11]. Thus we guess that C. glabrata initially caused paronychia which further developed into osteomyelitis of the phalanx through contiguous infection mechanism over 4 months before the consultation.
Although susceptibility testing to antifungal agents was not performed in this case, osteomyelitis was successfully cured with surgical curettage followed by antifungal treatment (flucytosine) for 3 months. Flucytosine has comparatively low toxicity and was given without any combination dosages of other antifungal agents to avoid side effects. Compared with patients infected with C. albicans, those with nonalbicans Candida species including C. glabrata are more likely to have received an inadequate dose of fluconazole as initial therapy because C. glabrata often exhibits resistance to fluconazole [12]. Therefore we emphasize to carry out susceptibility testing to obtain accurate MIC values and to choose the antifungal agents, in which amphotericin B would be the first choice, in the case of osteomyelitis caused by nonalbicans Candida species [3, 7–10].
Another study reported a severe case of osteomyelitis for 6 months caused by C. guilliermondii in a 57-year-old patient that resulted in partial amputation of the affected finger [4], and the strains isolated in culture were highly resistant to fluconazole and itraconazole. As a result, the symptoms progressed, and a deep and painful ulcer with radiologic signs of progressing acroosteolysis required partial amputation at the distal interphalangeal joint. Because bone and joint fungal infection are difficult to diagnose and as delayed diagnosis can lead to a progression of infection, fungal infection should be considered as a differential diagnosis in cases presenting with prolonged or chronic refractory inflammation, even in the digits.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Pappas PG. Invasive Candidiasis. Infectious Disease Clinics of North America. 2006;20(3):485–506. doi: 10.1016/j.idc.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Gamaletsou MN, Kontoyiannis DP, Sipsas NV, et al. Candida osteomyelitis: analysis of 207 pediatric and adult cases (1970–2011) Clinical Infectious Diseases. 2012;55(10):1338–1351. doi: 10.1093/cid/cis660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slenker AK, Keith SW, Horn DL. Two hundred and eleven cases of Candida osteomyelitis: 17 case reports and a review of the literature. Diagnostic Microbiology and Infectious Disease. 2012;73(1):89–93. doi: 10.1016/j.diagmicrobio.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Tietz HJ, Czaika V, Sterry W. Case report. Osteomyelitis caused by high resistant Candida guilliermondii . Mycoses. 1999;42(9-10):577–580. doi: 10.1046/j.1439-0507.1999.00497.x. [DOI] [PubMed] [Google Scholar]
- 5.Bannatyne RM, Clarke HM. Ketoconazole in the treatment of osteomyelitis due to Candida albicans. Canadian Journal of Surgery. 1989;32(3):201–202. [PubMed] [Google Scholar]
- 6.Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clinical Microbiology Reviews. 2007;20(1):133–163. doi: 10.1128/CMR.00029-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrow JD, Manian FA. Vertebral osteomyelitis due to Candida glabrata: a case report. Journal of the Tennessee Medical Association. 1986;79(7):409–410. [PubMed] [Google Scholar]
- 8.Dwyer K, McDonald M, Fitzpatrick T. Presentation of Candida glabrata spinal osteomyelitis 25 months after documented candidaemia. Australian and New Zealand Journal of Medicine. 1999;29(4):571–572. doi: 10.1111/j.1445-5994.1999.tb00767.x. [DOI] [PubMed] [Google Scholar]
- 9.Seravalli L, van Linthoudt D, Bernet C, et al. Candida glabrata spinal osteomyelitis involving two contiguous lumbar vertebrae: a case report and review of the literature. Diagnostic Microbiology and Infectious Disease. 2003;45(2):137–141. doi: 10.1016/s0732-8893(02)00497-2. [DOI] [PubMed] [Google Scholar]
- 10.Dailey NJM, Young EJ. Candida glabrata spinal osteomyelitis. The American Journal of the Medical Sciences. 2011;341(1):78–82. doi: 10.1097/MAJ.0b013e3181f6c6ea. [DOI] [PubMed] [Google Scholar]
- 11.Amako M, Ariono H, Nemoto K. Infection around the nails. Monthly Book Derma. 2011;(184):76–80. [Google Scholar]
- 12.Klevay MJ, Horn DL, Neofytos D, Pfaller MA, Diekema DJ. Initial treatment and outcome of Candida glabrata versus Candida albicans bloodstream infection. Diagnostic Microbiology and Infectious Disease. 2009;64(2):152–157. doi: 10.1016/j.diagmicrobio.2009.03.007. [DOI] [PubMed] [Google Scholar]


