Abstract
Sexual risk behavior and illicit drug use among people living with HIV/AIDS (PLWHA) contribute to poor health and onward transmission of HIV. The aim of this collaborative multi-site nursing research study was to explore the association between self-compassion and risk behaviors in PLWHA. Nurse researchers in Canada, China, Namibia, Puerto Rico, Thailand and the U.S. enrolled 2,182 PLWHA using convenience sampling. Over half of study participants were sexually active in the past three months. Participants with higher self-compassion were less likely to report sexual risk behavior. However, if a person also used illicit drugs, the relationship with self-compassion was reduced. Self-compassion may be a novel area for behavioral intervention development for PLWHA.
Keywords: HIV/AIDS, International Nursing Network for HIV/AIDS Research, nursing, self-compassion, sexual risk behavior, illicit drug use
Multi-site, collaborative research is a promising model for nursing science, and technological advances have helped these models expand over the past five years (Schluter, Turner, Huntington, Bain, & McClure, 2011). Collaborative models can be efficient, productive, and can lead to more generalizable findings (Beaver, 2004). The utility of such nursing research is particularly relevant for illnesses such as HIV/AIDS, which affects populations around the world and is demanding the attention of nurses globally. The International Nursing Network for HIV/AIDS Research (Holzemer, 2007) recently completed its fifth collaborative study, and this paper presents a sub-analysis on the role of self-compassion and unhealthy drug and sexual behaviors among people living with HIV/AIDS (PLWHA).
Background
Preventing HIV transmission and maintaining adherence to prescribed HIV treatments are of great concern for PLWHA, and are significant global public health priorities (Crepaz et al., 2006; McCoy, Kangwende, & Padian, 2010). Recently, much attention has been paid to preventing HIV transmission through antiretroviral (ARV) use, which lowers HIV viral load and reduces the chance of onward transmission of HIV (Donnell et al., 2010; Kalichman et al., 2011). The efficacy of ARV use for prevention, however, is dependent on adherence to the medications. In order for HIV treatment and prevention efforts to reduce transmission, attention to the individual PLWHA and the factors that support and inhibit adherence to treatment must be studied (Okonsky, 2011). Self-management of health behavior can include both positive and negative ways that individuals manage their health and symptoms (Eller et al., 2010; Nicholas et al., 2007).
One particular unhealthy behavior, illicit drug use, may complicate HIV self-management. Illicit drug use interferes with both medication access and adherence, and also may contribute to HIV pathogenesis, increased transmission risk, and destabilized sources of social and financial support (Mellins et al., 2009). Studies of risk behavior in PLWHA have shown an association between illicit drug use, particularly stimulants such as methamphetamine and crack cocaine, and behaviors that transmit HIV (Colfax et al., 2004; Hedden et al., 2011). Illicit drug use is also a risk factor for poor adherence to HIV medications, and its use is associated with lower CD4 counts and higher viral load (Samet, Walley, & Bridden, 2007). Crack cocaine use is associated with progression to AIDS (Baum et al., 2009). In a prospective study of illicit drug users, active stimulant users demonstrated smaller reductions in HIV viral load and smaller increases in CD4 cell count from baseline, controlling for ARV adherence (Baum et al., 2009). Data suggest that both ARV medication non-adherence and behavioral risks, such as those described above, occur in individuals who exhibit problems coping with their HIV diagnosis or who face specific psychosocial barriers (Moskowitz, Hult, Bussolari, & Acree, 2009; Sikkema et al., 2010). Problems coping with HIV can lead not only to illicit drug use, but also to fatalistic thoughts about their future, suicidal tendencies, and selective or non-disclosure of HIV status to offset discrimination and stigma in personal relationships and social contexts (Crepaz & Marks, 2001; Moskowitz et al., 2009).
The study of concepts associated with self and self-management is an important area of study in nursing (Wilkinson & Whitehead, 2009), and can be important for HIV care as well. Numerous psychological and social issues may affect the PLWHA's ability to manage a complex illness (Carrico, Neilands, & Johnson, 2010), but intervening on psychosocial factors as a way to reduce unhealthy behaviors and improve self-management among PLWHA needs further study. Self-management of a chronic health condition is a dynamic process consisting of three dimensions; context, process and outcomes and includes self-regulation and health behavior and its impact on health outcomes (Ryan & Sawin, 2009). Self-management behaviors improve health outcomes, but not all researchers, academics, and providers agree on the components and how best to incorporate them in order to improve health. Self-management is learned through experience, education, culture, scientific knowledge and growth and development, and includes behaviors that are amenable to change. Self-regulation and self-management behaviors in PLWHA including adherence to HIV medication are an important area of focus for interventions that are developed to improve the health of PLWHA. The relationship between HIV medication adherence and self-efficacy has been well documented (Johnson et al., 2007b), but there has been a lack of research examining other concepts such as self-compassion and the potential role it may have on HIV (Moskowitz & Seal, 2011) and self-management.
Self-compassion conceptually refers to treating oneself with the same concern and care that someone would treat a loved one who is experiencing difficulties in life such as being ill (Brion, Leary, & Drabkin, 2013; Neff, 2003). Although there is little research on addressing self-compassion in individuals who are engaging in unhealthy behaviors (such as sexual risk behavior and substance use) and who also are self-managing a chronic illness, this may be a particularly relevant area of study because levels of self-compassion could possibly be altered or improved (Neff, 2003). Brion and colleagues (2013) found that chronically ill individuals with higher levels of self-compassion exhibited more resilience in responding to their illness, including adherence to ARVs and ongoing medical treatments. Despite this formative work, however, few studies have examined the relationship between self-compassion and self-management or clinical outcomes in HIV. The purpose of this analysis, then, is to explore the relationship between unhealthy behaviors (i.e. sexual risk behavior, illicit drug use) and self-compassion among people living with HIV/AIDS in a multi-site nurse-led research collaboration.
Methods
This cross-sectional study was conducted under the auspices of the International Nursing Network for HIV/AIDS Research (Holzemer, 2007; Kemppainen et al., 2013; Nokes et al., 2012; Webel et al., 2012). Data were collected from sites in Vancouver, Canada; Shanghai, China; Windhoek, Namibia; San Juan, Puerto Rico; and Bangkok, Thailand, and from 11 sites in the United States (U.S.) (Boston, MA, Chicago, IL, Cleveland, OH, Corpus Christi, TX, Durham, NC, Harlingen, TX, Honolulu, HI, Newark, NJ, New York, NY, San Francisco, CA, San Juan, PR, Seattle, WA, and Wilmington, NC). Each site director agreed to adhere to the common protocol and to take responsibility for financial, ethical and legal aspects of the study at her/his own site. The common protocol was designed with input from site directors over the course of two in-person meetings of the nurse-researcher collaboration.
Participants
Each site sought to recruit a minimum of 100 adults living with HIV infection using a convenience sample. For a number of reasons – the exploratory nature of the study, the large number of sites, and the lack of information on differences in self-compassion that might be clinically significant – we did not conduct a power analysis to determine the sample size. Participants were recruited from HIV community-based organizations and HIV care clinics, using two methods. First, flyers were posted in participating sites, and people who were interested in the study could call to make an appointment with an investigator or to learn when the research team would be present at the site for data collection. In the second method, members of the research team were available in waiting rooms where only PLWHA were present, and announced the study to all present; people who were interested in participating then approached the researchers. At each site, data were collected until a minimum of 100 PLWHA had completed the study. Inclusion criteria were: (1) being 18 years or older; (2) self-reported HIV-positive serostatus; and (3) ability to provide informed consent in the local language (e.g. English, Thai, Chinese, local Namibian dialect, or Spanish).
After recruitment and screening, all participants gave written, informed consent, and completed a self-administered survey. Participants who were unable to read the survey were given the opportunity to complete the survey via verbal interview with the help of a research assistant. Upon completing the survey, participants were given a financial acknowledgement to compensate them for their time. These ranged from U.S.$5–6 in Thailand and China, to U.S.$15–$30 in the U.S. and Namibia. Although compensation varied by site, the amounts were determined based upon each site primary investigators’ prior experience working with PLWHA research participants in these particular sites, and were approved as being appropriate by each site’s institutional review board (IRB).
Measurement
The study questionnaire included 16 different instruments, and those that were used in this analysis are described below. On average, participants took 30–60 minutes to complete the entire study booklet. All variables in this analysis were chosen a priori consistent with our prior work and our hypothesis that self-compassion is related to self-care for PLWHA.
Demographics
This instrument used in prior Network studies consists of 20 items about demographics and illness characteristics. It included questions on age, gender, race, ethnicity, education, adequacy of income, health insurance, date of HIV diagnosis, self-reported current CD4 count (Cunningham, Rana, Shapiro, & Hays, 1997; Kalichman, Rompa, & Cage, 2000), HIV viral load, co-occurring health conditions, HIV transmission route, and general health.
Illicit Drug Use
This 10-item survey, modified from an existing assessment of drug use (Lightfoot et al., 2005), examined self-reported recent use of licit and illicit drugs, including tobacco, alcohol, cocaine, crack, heroin, inhalants, marijuana, opiates and methamphetamine/speed. Participants are asked how many days per week they used each drug on average, over the past three months. Measuring illicit drug use in this manner has been tested for both reliability and validity in community based studies (Denis et al., 2012). For this analysis, the items were combined and dichotomized into one variable measuring any illicit drug use, including stimulants, crack, heroine, inhalants, opiates, or speed (yes/no) in the past three months (we did not include marijuana or alcohol) (Dowling-Guyer et al., 1994).
Self-Compassion
Neff (2003) developed and validated a 26-item self-report inventory to measure individual differences in the tendency to be self-compassionate. A shorter 12-item brief version of the self-compassion scale was subsequently developed (Raes, Pommier, Neff, & Van Gucht, 2011). This Brief Version Self-Compassion Inventory showed internal reliability (alpha ≥0.86) as well as construct validity. Participants were asked to rate how they dealt with difficult situations on a 5-point scale, (where 1=almost never, 2=rarely, 3=sometimes, 4=frequently and 5=almost always). Sample items included, "When I'm feeling down I tend to obsess and fixate on everything that's wrong," and "When I see aspects of myself that I don't like, I get down on myself”. After reverse scoring several items, responses are summed to calculate a total score. Lower scores represent lower self-compassion. In the current study we used the shorter version to decrease participant burden, and found the reliability to be acceptable for the purposes of this project (Chronbach's alpha = .71) (Kemppainen et al., 2013).
Sexual Risk Behavior
In order to capture risky behaviors, such as PLWHA engaging in unprotected sex, our analysis focused on participants who reported being sexually active in the past 3 months (Koblin et al., 2003). Sexual risk behavior was measured using a set of questions (Koblin et al., 2003) that measured the number of times and number of partners that the respondent reported engaging in sexual behaviors known to transmit HIV, including unprotected insertive and receptive anal intercourse, or vaginal intercourse (Catania, Kegeles, & Coates, 1990). We did not measure oral sex because the data on HIV transmission via oral sex is inconclusive and research indicates that oral sex does not usually occur in isolation of vaginal or anal intercourse (Parsons et al., 2005; Vittinghoff et al., 1999). We coded participants as engaging in sexual risk behavior if they reported any anal or vaginal intercourse with a partner, without a condom, in the previous three months. This measure of self-reported sexual risk behavior has been utilized in many studies which rely on self-reported sexual behavior in studies of HIV (Catania, Gibson, Chitwood, & Coates, 1990).
Translation
At four of the participating sites, the instruments were translated from English to the local language(s). These sites were Shanghai, China (Chinese), Bangkok, Thailand (Thai), San Juan, Puerto Rico (Spanish), and Windhoek, Namibia (Afrikaans and Oshiwambo). Each site followed established translation procedures (Beaton, Bombardier, Guillemin, & Ferraz, 2000) in order to ensure reliability of translated instruments. This process included initial translation (forward) by an expert whose primary language was Thai, Spanish, Afrikaans, Oshiwambo or Chinese; next back translation was conducted; then review and adjudication; pilot testing; and finally a consensus meeting was held to approve the translated version of the measure. Psychometric estimates for each of these instruments was beyond the scope of this analysis, a more in-depth discussion of cross-cultural translation of the brief version of the self-compassion instrument can be found in Kemppainen (2013).
Data Management
Each site was responsible for their own data collection, ensuring completeness of the survey, entering and cleaning their data in an SPSS template, and securing the data. After these tasks were complete for all participants at each site, the data were de-identified and sent to the coordinating center at the University of California, San Francisco (UCSF). Once received, the data were cleaned and aggregated in SPSS, and instrument sub-factor and total scores were calculated.
Ethical Review
The University of California, San Francisco Committee on Human Research conducted the primary ethical review for this study. Once approval was received, each of the sites submitted the proposal to their local Institutional Review Board (IRB) for independent ethical review and approval. Each site received approval from their local IRB prior to implementing any study procedures.
Analysis
Analyses for this report were conducted in Stata 11 (StataCorp, 2010) and Mplus 7 (Muthén & Muthén, 1998–2012). We first conducted bivariate logistic regression to examine associations between the variables of interest (illicit drug use and self-compassion) and sexual risk behavior. These variables, listed in Table 2, were then entered into a multivariable regression model to examine whether illicit drug use and self-compassion were significantly associated with sexual risk behavior when adjusting for potential confounders (gender, self-esteem, HIV medication use). We then developed a path mediation model with Mplus to investigate whether illicit drug use mediates the relationship between self-compassion and sexual risk behavior. Path models are superior to older methods using a series of regression equations for estimating mediated effects (Iacobucci, Saldanha, & Deng, 2007).
Table 2.
Predictors of Sexual Risk Behavior
| OR (95% CI; p-value) |
Adjusted OR* (95% CI, p-value) |
|
|---|---|---|
| Illicit drug use | 1.75 (1.18, 2.60; p=.005) | 1.67 (1.10, 2.54; p=.02) |
| Self-compassion | .98 (.96, 1.00; p=.014) | .96 (.93, .99; p=.02) |
| Gender | .88 (.71, 1.09; p=.24) | .85 (.66, 1.10; p=.19) |
| Self-Esteem | .99 (1.00, 1.04; p=.80) | .97 (.93, 1.00; p=.12) |
| HIV medication use | .99 (.84, 1.17; p=.90) | 1.02 (.86, 1.22; p=.811) |
Results
Overall, 1,211 (55.4%) of the 2,182 PLWHA who participated in the study reported being sexually active in the prior three months and were included in this sub-analysis. Sexually active participants came from all countries where the study was conducted, however, over two-thirds (80.4%) were from the U.S. including Puerto Rico. Sexually active participants were a mean age of 43.1 years and the majority (68.5%) were male (Table 1). Most were unemployed (70.0%), and many perceived their income to be barely adequate to meet their needs (26.3%). Eighty percent of the female participants reported having children, whereas 36% of the males reported having children. Participants reported living with HIV for a mean of 12 years (±7.6 years), 43.7% had ever received an AIDS diagnosis, and most were currently taking HIV medication (82.8%). The mean self-compassion score (range 10–50) was 38.7 (±7.5), which suggests a moderate level of self-compassion.
Table 1.
Demographic and HIV Health Indicators for All Participants Who Were Sexually Active in the Past 3 Months
| Male (n=830) |
Female (n=337) |
Transgender / Other (n=34) |
Total (n=1,211)* |
||
|---|---|---|---|---|---|
| Mean (SD) or Frequency (%) | |||||
| Age (years) | 43.8 (9.6) | 41.8 (8.8) | 40.8 (9.1) | 43.1 (9.4) | |
| Race | |||||
| Asian/Pacific Islander | 21 (2.6) | 11 (3.3) | 2 (5.9) | 34 (2.8) | |
| African American / Black | 298 (36.2) | 120 (35.7) | 14 (41.2) | 433 (36.1) | |
| Hispanic/Latino | 166 (20.2) | 66 (19.6) | 10 (29.4) | 243 (20.3) | |
| Native American/Indian | 17 (2.1) | 6 (1.8) | 2 (5.9) | 25 (2.1) | |
| White/Anglo | 175 (21.2) | 47 (14.0) | 2 (5.9) | 226 (18.9) | |
| Other | 18 (2.1) | 7 (2.1) | 2 (5.9) | 27 (2.3) | |
| African – Namibia | 35 (4.3) | 32 (9.5) | 2 (5.9) | 69 (5.8) | |
| Asian – China & Thailand | 94 (11.4) | 47 (14.0) | 0 (0.0) | 141 (11.8) | |
| Completed Education Level | |||||
| 11th grade or less | 178 (21.5) | 129 (38.3) | 10 (29.4) | 320 (26.6) | |
| High School or GED | 323 (39.1) | 104 (30.9) | 13 (38.2) | 441 (36.7) | |
| 2 years of college/AA/Technical | 189 (22.9) | 70 (20.8) | 9 (26.5) | 268 (22.3) | |
| College Degree (B.S. or B.A.) | 96 (11.6) | 23 (6.8) | 1 (2.9) | 120 (10.0) | |
| Master’s Degree | 35 (4.2) | 10 (3.0) | 0 (0.0) | 45 (3.7) | |
| Doctorate | 6 (0.7) | 1 (0.3) | 1 (2.9) | 8 (0.7) | |
| Perceived Income Adequacy | |||||
| Totally Inadequate | 120 (17.5) | 69 (23.3) | 3 (10.0) | 194 (19.0) | |
| Barely Adequate | 185 (27.0) | 69 (23.3) | 13 (43.3) | 269 (26.3) | |
| Enough | 381 (55.5) | 158 (53.4) | 14 (46.7) | 559 (54.7) | |
| Currently work for pay | 262 (32.0) | 88 (26.4) | 6 (17.7) | 359 (30.0) | |
| Have Health Insurance | 589 (71.2) | 251 (75.2) | 25 (73.5) | 873 (72.5) | |
| Have Children | 324 (40.0) | 269 (80.3) | 6 (17.7) | 602 (50.7) | |
| One or more children living with participant | 95 (31.9) | 126 (52.7) | 1 (16.7) | 222 (40.1) | |
| Year Diagnosed with HIV | 1998 (8.0) | 1999 (7.1) | 1999 (7.2) | 1999 (7.8) | |
| Have AIDS Diagnosis | 354 (43.7) | 146 (44.4) | 12 (36.4) | 512 (43.7) | |
| CD4+T cell count | 485 (367) | 528 (392) | 282 (260) | 491 (372) | |
| Detectable HIV Viral Load (of those who know) | 154 (27.3) | 77 (39.1) | 4 (30.8) | 365 (30.4) | |
| Currently taking HIV meds | 679 (83.5) | 266 (81.9) | 25 (75.8) | 970 (82.8) | |
| Self-compassion Score | 38.5 (7.3) | 38.5 (7.5) | 36.4 (4.6) | 38.4 (7.3) | |
| Any illicit drug use | 241 (29.5) | 73 (21.7) | 18 (56.3) | 332 (28.0) | |
| Have had unprotected sex in the last 3 months | 354 (42.7) | 127 (37.7) | 15 (44.1) | 496 (41.3) | |
10 people did not report gender. Of these, 7 did not report sex at birth, 2 were born male, and 1 was born female.
Many participants reported substance use in the prior three months. Of the sexually active participants, the majority (53.5%) reported tobacco use, 25.8% reported alcohol use, and 29.7% reported using marijuana in the past three months. Over one quarter of participants (28.0%) reported any illicit drug use in the prior three months, with crack cocaine (15.4%) and cocaine (13.3%) being the most commonly reported drugs used.
Of the 1,211 people who reported any anal or vaginal sex in the past three months, 41% (n=496) reported one or more instances of sex without a condom; therefore engaging in sexual risk behavior. We next examined the association between self-compassion and illicit drug use and sexual risk behavior. People who reported illicit drug use in the prior three months were nearly twice as likely to report engaging in sexual risk behavior (AOR=1.7, 95% CI 1.28, 2.18) (Table 2). Those who reported higher self-compassion scores were significantly less likely to report sexual risk behavior in the last three months (AOR=0.96, 95% CI .94, .98). Following guidance from other studies of sexual risk behavior in PLWHA we controlled for HIV medication use and self-esteem (Bing et al., 2001; Johnson et al., 2007a; Markowitz et al., 2011; Venkatesh et al., 2012).
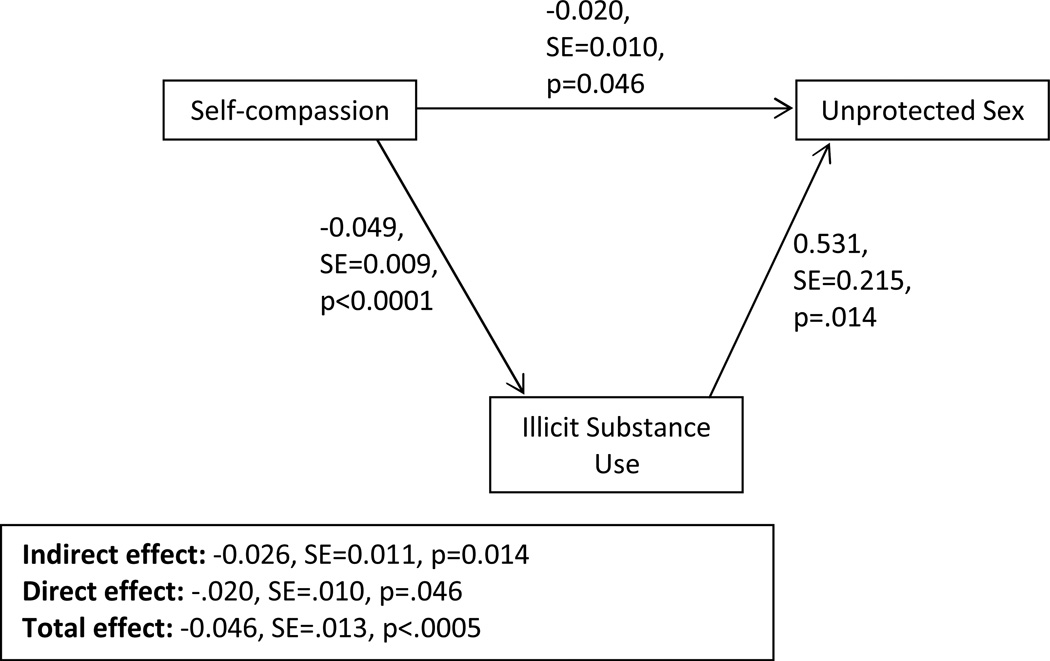
We then used path mediation modeling to examine whether use of illicit drugs mediated the association between self-compassion and unprotected sex. Robust standard errors were employed to account for the possible non-independence of the participants clustered by site (Figure 1). In addition, mediated effects are known to be non-normally distributed (Shrout & Bolger, 2002) so we employed an estimator that is robust to non-normality as well as non-independence (MLR, Muthén & Muthén, 1998–2012). The direct association between self-compassion and unprotected sex was significant (p = .046); in addition, the indirect association of self-compassion and unprotected sex, mediated by illicit drug use, was significant (p = .014). For example, a 10-point increase in self-compassion was associated with a 22.9% lower odds of unprotected sex, mediated by drug use. Thus, use of illicit drugs did significantly mediate the association of self-compassion and unprotected sex. The total effect – combined direct and indirect effects – of a 10-point increase in self-compassion predicted a 36.9% lower odds of having unprotected sex, p < .0005.
Figure 1.
Path Analysis
Discussion
This multi-site nursing collaborative study examined sexual risk behavior, illicit drug use and self-compassion in an international sample of PLWHA. The 1,211 sexually active PLWHA were, on average, middle-aged men. Most had known their HIV status for over 10 years and over two-thirds reported taking antiretroviral medication for their HIV. While only half of the total sample reported being sexually active in the last three months (N=1,211), more than half of the people who were having sex engaged in sexual risk behavior (anal or vaginal intercourse without use of a condom). Additionally, drug use in the past three months was common in this sample and included use of stimulants (cocaine, crack cocaine, and speed) and opiates (heroin and other non-prescribed opiates). The level of self-compassion in this sample was moderate, but varied, and was significantly lower in those individuals who had engaged in sexual risk behavior. While we do not have a biological test confirming substance use, self-report of illicit substance use is thought to be accurate and, if anything, underreported when self-report is utilized (Denis et al., 2012; Dowling-Guyer et al., 1994).
Specifically, we were looking at the novel concept of self-compassion and its relationship to illicit drug use and sexual risk behavior in PLWHA. An important finding from this study is that PLWHA in this sample who had higher levels of self-compassion had lower odds of engaging in sexual risk behavior. In addition we found that higher levels of illicit drug use were significantly associated with greater sexual risk behavior. While similar results linking illicit drug use to sexual risk behavior among PLWHA have previously been reported in the literature (Colfax et al., 2004; Purcell et al., 2007), this is the first study examining self-compassion and sexual risk behavior in PLWHA. Our results complement those of Magnus et al. (2010) who found that self-compassion was related to well-being in 252 women who exercise. Our examination of unhealthy behaviors in a sexually active population of PLWHA extends our understanding of this phenomenon. Because this is a cross-sectional study we cannot determine whether individuals who have more self-compassion are less likely to use illicit drugs thus establishing a causal relationship, nor do we know the clinical significance of different values on the self-compassion scale. Nonetheless, if self-compassion is associated with drug use as it is in this sample, this adds to our knowledge of possible ways to decrease drug use, which does have clinical significance. For example, counseling or interventions to improve self-compassion among PLWHA may help to reduce unhealthy behaviors (e.g. illicit drug use, sexual risk behavior) as a component of self-management.
Identifying effective approaches to addressing the risk behaviors that lead to increased morbidity and mortality in PLWHA has been a challenge in behavioral research and patient care. Moreover behavioral interventions beyond those for adherence to ARV medication have had little focus from nurse researchers. Self-compassion is an important subject for nursing research because it addresses the self and specific unhealthy-behaviors, a critical focus for research because of the advances made in HIV treatment as a means to HIV prevention (Cohen, McCauley, & Sugarman, 2012). Self-compassion, which in this sample is associated with less risk behavior, is novel and may be an important lens for the development of nursing policy and interventions with PLWHA and also with active illicit drug users. Increasing self-compassion could protect against maladaptive behaviors and promote better self-care leading to improved health outcomes in PLWHA and a decrease in the number of HIV transmission events.
Although not the focus of this study, it is critical for nurse scientists to study underlying causes of risk behavior. While self-compassion is an individual level concept, eliminating structural and societal barriers that add to stigma and discrimination could impact self-compassion. Stigma is a particularly important area of study in the field of HIV nursing research (Holzemer & Uys, 2004; Nyblade, 2006) and there is ample documentation that stigma impacts HIV morbidity. One explanation for our findings could be that those who do not blame themselves for their HIV status experience less stigma, have higher levels of self-compassion, and thus are more likely to do what they can to take care of themselves. This self-care includes decreasing sexual risk behavior and illicit drug use.
The study had limitations. First, a majority of our sites and site directors are from the U.S., and other countries are not as evenly represented. Therefore, it is important to understand the local context. In the U.S., the majority of PLWHA are men (often men who have sex with men), and people of color. This may explain why 70% of our sample was male, whereas worldwide, it is estimated that 52% of all PLWHA are women, a fact that will limit the generalizability of the study’s findings. In recent years, HIV has expanded greatly into the female population in the U.S., although women are still fewer than half of those living with HIV. The U.S. sample may also represent substantial regional differences, as sites included Puerto Rico (largely Hispanic and of mixed ethnicity) and Hawaii. In contrast, in Canada, China, Namibia, and Thailand the study took place in one region.
The preponderance of U.S.-based sites in this study may also represent a bias in our protocol development, perhaps leaning toward assessing concepts that are well established in the scientific literature but may not be not applicable outside of the U.S. However, the International Nursing Network for HIV/AIDS Research has experience working in international settings, which we believe has helped to minimize this bias. A further limitation was the variation in the types of settings from which participants were recruited which included clinic sites and community based HIV/AIDS organizations.
The study’s cross-sectional design limits the ability to make inferences about causality and changes over time. This design, along with the convenience sampling methodology, limited our ability to make statistical comparisons across sites and countries, possibly limiting the generalizability of the results. However, as the study was intended to be exploratory, possibly the first to examine the association of self-compassion to sexual risk behavior and illicit drug use, the results point to a novel area of research that may have important policy and clinical implications in the future. In addition, the self-compassion instrument does not have established cut-offs or guidelines for clinical or research use, somewhat limiting our ability to interpret.
One of our strengths as a Network is also one of our limitations, as we strive to collaborate with nurse researchers in countries that are experiencing large HIV epidemics. Because of this, we did not enter into this research with a funded research protocol, as is the case for other large collaborative studies but more with an emphasis on working with nurse scientists to answer a question that is central to nursing science and self-care in an often marginalized population.
Conclusion and Implications
Despite these limitations, this sample of participants can guide further in-depth examinations of the concepts of self-management and the association between self and risk behaviors that affect HIV morbidity and mortality. The growing prevalence of the global HIV/AIDS epidemic makes it imperative to develop new strategies to help PLWHA better manage their own health, which can in turn prevent onward transmission of HIV. One possible key to unlocking these behaviors is the role of self-compassion to ameliorate unhealthy behaviors such as illicit drug use which impacts rates of sexual risk behavior that can transmit HIV. These data provide a foundation to understanding which concepts may be modified, and also help us to describe the components of successful nurse-initiated, self-management interventions for PLWHA.
One approach to learning new techniques is to address these shared challenges in international collaborative nursing research. By working with nurse investigators around the globe, the Network is helping to elucidate the complex underlying factors that affect an HIV-infected person’s ability to manage their HIV disease. This information may lead to new nurse-initiated interventions that improve the health and well-being of the more than 30 million PLWHA worldwide. This type of research allows us to look at nursing care for specific illnesses across settings and to describe more fully the concepts that are important in nursing care and perhaps that resonate across continents. Globally, as the burden of HIV continues to grow, more responsibility and clinical management are being shifted to the profession of nursing (Callaghan, Ford, & Schneider, 2010). Nurse-led research is critical for informing both health policy and nursing practice. The results of collaborative nursing research, like the study presented here, can add to the clinical and policy knowledge base, help to inform interventions to improve the health of PLWHA world-wide and reduce onward transmission.
Acknowledgement
Financial Support
This project was supported in part by: NIH UL1 RR024131; NIHT32NR007081; NIH KL2RR024990; NIH R15NR011130; International Pilot Award, University of Washington Center for AIDS Research; University of Washington, School of Nursing; University of British Columbia School of Nursing Helen Shore Fund; Duke University School of Nursing Office of Research Affairs; MGH Institute for Health Professions; Rutgers College of Nursing; City University of New York; Irwin Belk Distinguished Professorship Fund – University of North Carolina Wilmington; Texas A&M University – Corpus Christi, College of Nursing and Health Sciences; Saint Louis College of Thailand. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or any other funders. The authors would like to thanks Dr. Bruce Cooper for statistical assistance.
Footnotes
Conflicts of Interest
The authors declare no conflicts of interest.
Contributor Information
Carol Dawson Rose, Email: carol.dawson-rose@ucsf.edu, UCSF School of Nursing, Dept. of Community Health Systems, San Francisco, CA 94143-0608, T: (415) 713-5252, F: (415) 476-4076.
Allison Webel, Case Western Reserve University, Bolten School of Nursing.
Kathleen M. Sullivan, University of Hawaii School of Nursing.
Yvette P. Cuca, UCSF School of Nursing.
Dean Wantland, Office of Research & Evaluation, Rutgers College of Nursing.
Mallory O. Johnson, UCSF.
John Brion, The Ohio State University College of Nursing.
Carmen J. Portillo, UCSF, School of Nursing.
Inge B. Corless, MGH Institute of Health Professions.
Joachim Voss, University of Washington.
Wei-Ti Chen, Yale University School of Nursing.
J. Craig Phillips, Faculty of Health Sciences, School of Nursing, University of Ottawa.
Lynda Tyer-Viola, Pavilion for Women, Texas Children’s Hospital.
Marta Rivero-Méndez, University of Puerto Rico.
Patrice K. Nicholas, Global Health and Academic Partnerships, Brigham and Women's Hospital and MGH Institute of Health Professions.
Kathleen Nokes, Hunter College, CUNY, Hunter Bellevue School of Nursing.
Jeanne Kemppainen, University of North Carolina Wilmington.
Elizabeth Sefcik, Texas A&M University-Corpus Christi.
Lucille Sanzero Eller, Rutgers College of Nursing.
Scholastika Iipinge, University of Namibia.
Kenn Kirksey, Nursing Strategic Initiatives, Lyndon B. Johnson Hospital – Executive Administration, Harris Health System.
Puangtip Chaiphibalsarisdi, School of Nursing, Shinawatra University.
Nancy Davila, University of Puerto Rico.
Mary Jane Hamilton, Texas A&M University – Corpus Christi.
Dorothy Hickey, Momentum AIDS Program & Assistant Adjunct Clinical Professor at New York City College of Technology.
Mary Maryland, Chicago State University College of Health Sciences, Department of Nursing.
Paula Reid, School of Nursing, The University of North Carolina at Wilmington.
William L. Holzemer, Rutgers College of Nursing.
References
- Baum MK, Rafie C, Lai S, Sales S, Page B, Campa A. Crack-cocaine use accelerates HIV disease progression in a cohort of HIV-positive drug users. Journal of Acquired Immune Deficiency Syndromes. 2009;50:93–99. doi: 10.1097/QAI.0b013e3181900129. [DOI] [PubMed] [Google Scholar]
- Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- Beaver D. Does collaborative research have greater epistemic authority? Scientometrics. 2004;60:399–408. [Google Scholar]
- Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, Turner BJ, Eggan F, Beckman R, Vitiello B, Morton SC, Orlando M, Bozzette SA, Ortiz-Barron L, Shapiro M. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry. 2001;58:721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- Brion J, Leary M, Drabkin A. Self-compassion and reaction to serious illness: The case of HIV. Health Psychology. 2013 [ePub ahead of print]. [Google Scholar]
- Callaghan M, Ford N, Schneider H. A systematic review of task- shifting for HIV treatment and care in Africa. Human Resources for Health. 2010;8:8. doi: 10.1186/1478-4491-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrico AW, Neilands TB, Johnson MO. Suicidal ideation is associated with HIV transmission risk in men who have sex with men. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2010;54(4):e3–e4. doi: 10.1097/QAI.0b013e3181da1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychological Bulletin. 1990;108:339–362. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: an AIDS risk reduction model (ARRM) Health Education and Behavior. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- Cohen MS, McCauley M, Sugarman J. Establishing HIV treatment as prevention in the HIV Prevention Trials Network 052 randomized trial: an ethical odyssey. Clinical Trials. 2012;9:340–347. doi: 10.1177/1740774512443594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, Celum C, Chesney M, Huang Y, Mayer K, Bozeman S, Judson FN, Bryant KJ, Coates TJ, Team ES. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. American Journal of Epidemiology. 2004;159:1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Lyles CM, Wolitski RJ, Passin WF, Rama SM, Herbst JH, Purcell DW, Malow RM, Stall R for the HIV/AIDS Prevention Research Synthesis Team. Do prevention interventions reduce HIV risk behaviours among people living with HIV? A meta-analytic review of controlled trials. AIDS. 2006;20:143–157. doi: 10.1097/01.aids.0000196166.48518.a0. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychology. 2001;20:291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- Cunningham WE, Rana HM, Shapiro MF, Hays RD. Reliability and validity of self-report CD4 counts-in persons hospitalized with HIV disease. Journal of Clinical Epidemiology. 1997;50:829–835. doi: 10.1016/s0895-4356(97)00061-9. [DOI] [PubMed] [Google Scholar]
- Denis C, Fatseas M, Beltran V, Bonnet C, Picard S, Combourieu I, Daulouede JP, Auriacombe M. Validity of the self-reported drug use section of the Addiction Severity Index and associated factors used under naturalistic conditions. Substance Use and Misuse. 2012;47:356–363. doi: 10.3109/10826084.2011.640732. [DOI] [PubMed] [Google Scholar]
- Donnell D, Baeten JM, Kiarie J, Thomas KK, Stevens W, Cohen CR, McIntyre J, Lingappa JR, Celum C Partners in Prevention, H. S. V. H. I. V. T. S. T. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375:2092–2098. doi: 10.1016/S0140-6736(10)60705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowling-Guyer S, Johnson ME, Fisher DG, Needle R, Watters J, Andersen M, Williams M, Kotransky L, Booth R, Rhodes F, Weatherby N, Estrada AL. Reliability of drug users' self-reported HIV risk behaviors and validity of self-reported recent drug use. Assessment. 1994;1:383–392. [Google Scholar]
- Eller LS, Bunch EH, Wantland DJ, Portillo CJ, Reynolds NR, Nokes KM, Coleman CL, Kemppainen JK, Kirksey KM, Corless IB, Hamilton MJ, Dole PJ, Nicholas PK, Holzemer WL, Tsai YF. Prevalence, correlates, and self-management of HIV-related depressive symptoms. AIDS Care. 2010;22:1159–1170. doi: 10.1080/09540121.2010.498860. [DOI] [PubMed] [Google Scholar]
- Hedden SL, Hulbert A, Cavanaugh CE, Parry CD, Moleko AG, Latimer WW. Alcohol, drug and sexual risk behavior correlates of recent transactional sex among female black South African drug users. Journal of Substance Use. 2011;16:57–67. doi: 10.3109/14659891003721141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzemer WL. University of California, San Francisco International Nursing Network for HIV/AIDS Research. International Nursing Review. 2007;54:234–242. doi: 10.1111/j.1466-7657.2007.00571.x. [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Uys LR. Managing AIDS stigma. Journal of Social Aspects of HIV/AIDS. 2004;1:165–174. doi: 10.1080/17290376.2004.9724839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacobucci D, Saldanha N, Deng X. A meditation on mediation: Evidence that structural equation models perform better than regressions. Journal of Consumer Psychology. 2007;17:139–153. [Google Scholar]
- Johnson MO, Charlebois E, Morin SF, Remien RH, Chesney MA National Institute of Mental Health Healthy Living Project, T. Effects of a behavioral intervention on antiretroviral medication adherence among people living with HIV: the healthy living project randomized controlled study. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2007a;46:574–580. doi: 10.1097/qai.0b013e318158a474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The Role of Self-Efficacy in HIV Treatment Adherence: Validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES) Journal of Behavioral Medicine. 2007b;30:359–370. doi: 10.1007/s10865-007-9118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Cherry C, Kalichman MO, Amaral CM, White D, Pope H, Swetzes C, Eaton L, Macy R, Cain D. Integrated behavioral intervention to improve HIV/AIDS treatment adherence and reduce HIV transmission. American Journal of Public Health. 2011;101:531–538. doi: 10.2105/AJPH.2010.197608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M. Reliability and validity of self-reported CD4 lymphocyte count and viral load test results in people living with HIV/AIDS. International Journal of STDs & AIDS. 2000;11:579–585. doi: 10.1258/0956462001916551. [DOI] [PubMed] [Google Scholar]
- Kemppainen J, Brion J, Wantland D, Sullivan KM, Nokes K, Bain CJ, Chen WT, Holzemer WL, Eller LS, Iipinge S, Johnson MO, Portillo CJ, Voss J, Tyer-Viola L, Corless IB, Nicholas P, Dawson Rose C, Phillips JC, Sefcik E, Rivero-Mendez M, Kirksey K. Use of a brief version of the self-compassion inventory with an international sample of people with HIV/AIDS. AIDS Care. 2013 doi: 10.1080/09540121.2013.780119. [ePub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Chesney MA, Husnik MJ, Bozeman S, Celum CL, Buchbinder S, Mayer K, McKirnan D, Judson FN, Huang Y, Coates TJ, Team ES. High-risk behaviors among men who have sex with men in 6 US cities: baseline data from the EXPLORE Study. American Journal of Public Health. 2003;93:926–932. doi: 10.2105/ajph.93.6.926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightfoot M, Rogers T, Goldstein R, Rotheram-Borus MJ, May S, Kirshenbaum S, Weinhardt L, Zadoretzky C, Kittel L, Johnson M, Gore-Felton C, Morin SF. Predictors of substance use frequency and reductions in seriousness of use among persons living with HIV. Drug and Alcohol Dependence. 2005;77:129–138. doi: 10.1016/j.drugalcdep.2004.07.009. [DOI] [PubMed] [Google Scholar]
- Magnus CMR, Kowalski KC, McHugh TF. The role of self-compassion in women's self-determined motives to exercise and exercise-related outcomes. Self and Identity. 2010;9:363–382. [Google Scholar]
- Markowitz SM, O'Cleirigh C, Hendriksen ES, Bullis JR, Stein M, Safren SA. Childhood sexual abuse and health risk behaviors in patients with HIV and a history of injection drug use. AIDS and Behavior. 2011;15:1554–1560. doi: 10.1007/s10461-010-9857-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy S, Kangwende R, Padian N. Behavior change interventions to prevent HIV infection among women living in low and middle income countries: A systematic review. AIDS and Behavior. 2010;14:469–482. doi: 10.1007/s10461-009-9644-9. [DOI] [PubMed] [Google Scholar]
- Mellins CA, Havens JF, McDonnell C, Lichtenstein C, Uldall K, Chesney M, Santamaria EK, Bell J. Adherence to antiretroviral medications and medical care in HIV-infected adults diagnosed with mental and substance abuse disorders. AIDS Care. 2009;21:168–177. doi: 10.1080/09540120802001705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz DA, Seal DW. Self-esteem in HIV-positive and HIV-negative gay and bisexual men: implications for risk-taking behaviors with casual sex partners. AIDS and Behavior. 2011;15:621–625. doi: 10.1007/s10461-010-9692-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz JT, Hult JR, Bussolari C, Acree M. What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychological Bulletin. 2009;135:121–141. doi: 10.1037/a0014210. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. 7th ed. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Neff KD. The development and validation of a scale to measure self-compassion. Self and Identity. 2003;2:223–250. [Google Scholar]
- Nicholas PK, Kemppainen JK, Canaval GE, Corless IB, Sefcik EF, Nokes KM, Bain CA, Kirksey KM, Eller LS, Dole PJ, Hamilton MJ, Coleman CL, Holzemer WL, Reynolds NR, Portillo CJ, Bunch EH, Wantland DJ, Voss J, Phillips R, Tsai YF, Mendez MR, Lindgren TG, Davis SM, Gallagher DM. Symptom management and self-care for peripheral neuropathy in HIV/AIDS. AIDS Care. 2007;19:179–189. doi: 10.1080/09540120600971083. [DOI] [PubMed] [Google Scholar]
- Nokes K, Johnson MO, Webel A, Dawson Rose C, Phillips JC, Sullivan KM, Tyer-Viola L, Rivero-Mendez M, Nicholas PK, Kemppainen J, Sefcik E, Chen W-T, Brion J, Eller LS, Kirksey KM, Wantland D, Portillo CJ, Corless IB, Voss J, Iipinge S, Spellmann M, Holzemer WL. Focus on increasing treatment self-efficacy to improve human immunodeficiency virus treatment adherence. Journal of Nursing Scholarship. 2012;44:403–410. doi: 10.1111/j.1547-5069.2012.01476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade LC. Measuring HIV stigma: existing knowledge and gaps. Psychology, Health & Medicine. 2006;11:335–345. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- Okonsky JG. Problems taking pills: understanding HIV medication adherence from a new perspective. AIDS Care. 2011;23:1652–1659. doi: 10.1080/09540121.2011.579944. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Schrimshaw EW, Wolitski RJ, Halkitis PN, Purcell DW, Hoff CC, Gomez CA. Sexual harm reduction practices of HIV-seropositive gay and bisexual men: serosorting, strategic positioning, and withdrawal before ejaculation. AIDS. 2005;19(Suppl 1):S13–S25. doi: 10.1097/01.aids.0000167348.15750.9a. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Latka MH, Metsch LR, Latkin CA, Gomez CA, Mizuno Y, Arnsten JH, Wilkinson JD, Knight KR, Knowlton AR, Santibanez S, Tobin KE, Rose CD, Valverde EE, Gourevitch MN, Eldred L, Borkowf CB Team, f. t.I. S. Results from a randomized controlled trial of a peer-mentoring intervention to reduce HIV transmission and increase access to care and adherence to HIV medications among HIV-seropositive injection drug users. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2007;46:S35–S47. doi: 10.1097/QAI.0b013e31815767c4. [DOI] [PubMed] [Google Scholar]
- Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clinical Psychology & Psychotherapy. 2011;18:250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- Samet JH, Walley AY, Bridden C. Illicit drugs, alcohol, and addiction in human immunodeficiency virus. Panminerva Medica. 2007;49:67–77. [PubMed] [Google Scholar]
- Schluter PJ, Turner C, Huntington A, Bain C, McClure R. Work/life balance and health: the Nurses and Midwives e-cohort study. International Nursing Research. 2011;57:28–36. doi: 10.1111/j.1466-7657.2010.00849.x. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422. [PubMed] [Google Scholar]
- Sikkema K, Watt M, Drabkin A, Meade C, Hansen N, Pence B. Mental health treatment to reduce HIV transmission risk behavior: A positive prevention model. AIDS and Behavior. 2010;14:252–262. doi: 10.1007/s10461-009-9650-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 11. College Station, TX: StataCorp, LP; 2010. [Google Scholar]
- Venkatesh KK, de Bruyn G, Lurie MN, Modisenyane T, Triche EW, Gray GE, Welte A, Martinson NA. Sexual risk behaviors among HIV-infected South African men and women with their partners in a primary care program: implications for couples-based prevention. AIDS and Behavior. 2012;16:139–150. doi: 10.1007/s10461-011-9941-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittinghoff E, Douglas J, Judson F, McKirnan D, MacQueen K, Buchbinder SP. Per-contact risk of human immunodeficiency virus transmission between male sexual partners. American Journal of Epidemiology. 1999;150(3):306–311. doi: 10.1093/oxfordjournals.aje.a010003. [DOI] [PubMed] [Google Scholar]
- Webel A, Phillips JC, Rose CD, Holzemer WL, Chen WT, Tyer-Viola L, Rivero-Mendez M, Nicholas P, Nokes K, Kemppainen J, Sefcik E, Brion J, Eller L, Iipinge S, Kirksey K, Wantland D, Chaiphibalsarisdi P, Johnson MO, Portillo C, Corless IB, Voss J, Salata RA. A cross-sectional description of social capital in an international sample of persons living with HIV/AIDS (PLWH) BMC Public Health. 2012;12:188. doi: 10.1186/1471-2458-12-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson A, Whitehead L. Evolution of the concept of self-care and implications for nurses: a literature review. International Journal of Nursing Studies. 2009;46:1143–1147. doi: 10.1016/j.ijnurstu.2008.12.011. [DOI] [PubMed] [Google Scholar]