Abstract
Purpose
Quality of life (QOL) among adolescents with neonatal brachial plexus palsy (NBPP) is an important but unexplored topic. To date, few NBPP studies use comprehensive patient-reported outcome measures, and none specifically address the adolescent population. This study explores the long-term QOL and patient expectations among adolescents with NBPP using qualitative and quantitative approaches.
Methods
Eighteen adolescents with residual NBPP impairment between the ages of 10 to 17 years along with their parents were included in our study. Adolescents and their parents underwent separate one hour tape-recorded semi-structured interviews, which were audio recorded and transcribed. We also collected quantitative patient outcome measures to quantify the degree of each adolescent’s functional impairment and to increase our understanding of long-term quality of life and patient expectations.
Results
Thirteen females and five males with a mean age of 11.6 years participated in our study. Through qualitative analysis we identified the following factors contributing to overall QOL from the patient and parent perspective: social impact and peer acceptance, emotional adjustment, aesthetic concerns and body image, functional limitations, physical and occupational therapy, finances, pain, and family dynamics. Despite residual impairment, most adolescents and their parents reported a good overall QOL according to quantitative outcome measures, with adolescents reporting slightly higher QOL than their parents. However, both adolescents and their parents report relatively modest satisfaction with their current condition and express expectations for improvement in multiple areas.
Discussion
Understanding patient expectations and QOL in NBPP adolescents are essential for medical decision-making and advancing care. Our study results showed that functional and aesthetic factors were responsible for the majority of observed differences in QOL among NBPP adolescents. We also found that the PODCI might be more sensitive than the CHQ in assessing patient expectations and quality of life among this patient population.
Keywords: Brachial Plexus Palsy, Patient Expectations, Qualitative
INTRODUCTION
Adolescents with residual deficits from neonatal brachial plexus palsy (NBPP) encompass a wide range of clinical presentations and neurologic impairments that require unique and tailored treatment algorithms.(1, 2) Over the past several decades, advances in microsurgical nerve repair/reconstruction have changed the landscape of long-term surgical management and treatment outcomes among adolescents with NBPP.(1-4) Despite these advancements, little information exists regarding patient-rated outcome measures for NBPP and the long-term psychosocial impact of NBPP on children and their families.
Traditionally, functional health status and surgical outcomes for NBPP have been measured using a variety of validated physician-derived scores based primarily on objective physical exam findings, such as the modified Mallet Classification, Toronto Test Score, and Active Movement Scale.(5-6) However, across all disciplines of medicine, physicians, payers, and policy-makers have increasingly recognized the importance of incorporating subjective opinions and expectations from the patient point of view when evaluating health outcomes.(7-9) For reconstructive procedures aimed solely at improving QOL rather than increasing life expectancy, it is imperative to identify the best method of assessing patient expectations and global health-related QOL in order to develop valid outcome measures to guide surgical treatment, economic analyses, and health policy.(5-10)
Despite recognition and progress in the development of patient-rated outcome tools for other chronic pediatric conditions, outcome measures for NBPP remain relatively understudied.(11) Among the few published NBPP studies that have utilized comprehensive patient-rated outcome measures, none have specifically focused on the adolescent population.(6,12-13) Understanding the contribution of various psychosocial factors to overall health status and patient expectations in the adolescent population is most important, because of rapidly changing emotional needs, increasing desire for independence, and greater emphasis on peer acceptance during this period. Moreover, as children with NBPP mature, differences in measured health outcomes and patient expectations between adolescents and their parents are unknown.
The purpose of this study is to explore and describe the long-term global QOL and patient expectations among adolescents with NBPP from the patient and parent perspective using qualitative and quantitative research methods. Specifically, we aimed to identify factors that influence subjective patient-rated outcomes and treatment desires to better understand the evaluation of adolescent upper extremity impairments and brachial plexus palsies.
METHODS
Previous studies evaluating outcomes for NBPP have only used quantitative research methods to assess QOL. Although quantitative methodology rigorously tests well-specified hypotheses and measures various outcomes with statistical significance, the results and subsequent implications of these studies are limited to the a-priori perspective of the study investigators at the time of initial study design.(10,14-15) Alternatively, qualitative research allows researchers to gain insight into a variety of theory-generating aims by exploring and describing social and emotional phenomena associated with various aspects of health care and patient outcomes.(10, 14-18) We used grounded theory, a type of qualitative methodology, to guide both data collection and analysis. Grounded theory uses analytical induction to identify themes or categories of ideas as they emerge from the data (developing them from the “ground-up” rather than defining them prior to study initiation).(10, 18-20) Data are collected through open-ended or semi-structured interviews with a purposive sample of individuals or focus groups.(10, 15, 19-23) These data are then iteratively coded through a rigorous process that allows multiple theories and data hypotheses to emerge simultaneously in an unbiased systematic fashion.(10,15,19-23) This methodology is best used for generating additional contextual information about complex health care topics for which research is not well established, or when conventional quantitative theories seem premature or inadequate.(10, 14-18) In addition to qualitative interview data, we also collected several quantitative patient outcome measures to increase our understanding of overall quality of life and patient expectations among this patient population.
Study Sample
Because the objective of qualitative studies is to generate themes of interest rather than to statistically quantify measured health outcomes, validity is generally judged on the basis of sample selection and depth/scope of interview content rather than sample size as in quantitative studies that use systematic random sampling with adequate power to prove an a-priori hypothesis.(10,14-18) For this study, we chose to purposively sample adolescents diagnosed with NBPP who suffered from some degree of residual impairment beyond infancy and underwent some combination of surgery, Botox injections (Allergan Inc, Irvine, California), and/or continued therapy and follow-up. To explore divergences in experience between maturing adolescents and their health care proxies, we also chose to interview the parents of NBPP patients. Eligible adolescent-parent pairs were recruited via two methods: 1) from Institutional Review Board (IRB) approved data repository for NBPP patients, and 2) through a list of physical and occupational therapists known to treat infants with NBPP throughout the state of Michigan. Eighteen consecutive patient-parent pairs with adolescents between the ages of 10-17 years were selected to participate in separate one hour semi-structured interviews. Both informed consent from each parent/guardian and an additional informed assent from each minor were required for participation in this study.
Data Collection
Adolescents and their parents underwent separate, one hour, tape-recorded interviews in a semi-structured format using an interview guide focused on medical decision-making and quality of life. The former topic was examined in an analysis separate from this one.(24) Adolescents and parents were interviewed separately to examine differences in opinion and ensure comprehensive coverage of interview topics. Each parent was interviewed before the adolescent to obtain general information and for building rapport in case the adolescent was too shy to comment on his/her condition.
For objective functional scores, we collected the British Medical Research Council (MRC) scale for muscle strength, the Mallet score (to assess shoulder function), and the Raimondi score (to assess hand function).(25-27) We also collected information regarding adolescent specific global quality of life using the Child Health Questionnaire (CHQ) and the Pediatric Outcomes Data Collection Instrument (PODCI).(28-32) The CHQ and the PODCI are the only two outcome measures specifically designed to evaluate adolescent outcomes with separate parent and adolescent survey forms.(28-30) These outcomes tools were developed by pediatricians and orthopaedic surgeons, respectively, to assess overall quality of life (including psychosocial and emotional health in addition to function). Although the PODCI contains more specific questions regarding upper and lower extremity impairments, the CHQ includes a broader range of topics, such as the impact of the child’s health on family dynamics.(31-32)
Data Analysis
All audio-recordings were immediately transcribed verbatim after each interview so that findings from early interviews could be explored and verified in greater depth with subsequent study subjects.(10, 15) Once the transcripts were finalized, open coding and identification of key concepts were performed independently by two members of the research team (B.P.L. and L.S.) to reduce personal bias in interpretation of transcripts.(10, 15) After open coding of all transcripts was completed by both reviewers, a final codebook was generated that included categories, codes, and subcodes.(10, 15) This codebook was then applied to each individual transcript and the final coded transcripts were analyzed to identify code frequency patterns and obtain representative quotations for inclusion in the manuscript.(10, 15) Throughout the coding process, the research team convened to collaborate on their discrete findings and resolve any discrepancies.
Mean and median values were calculated for each functional outcome measure (MRC, Mallet, and Raimondi score) and quality of life outcome score (CHQ and PODCI). Effect sizes were then calculated to determine the magnitude of difference between our NBPP study population and published values for the general population (normal control). An effect size of 0.2 was defined as a small effect, 0.5 as a medium effect, and 0.8 as a large effect based on Cohen’s criteria.(33) Paired t tests were used to evaluate statistically significant differences in response between adolescents and their parents. All analyses were performed using SAS (SAS Institute Inc., Cary, North Carolina). Statistical significance for all analyses was set at p < 0.05.
RESULTS
Eighteen adolescent-parent pairs including five males and thirteen females with NBPP averaging 11.6 years old participated (Table 1). Half of the adolescents had upper trunk pathology and half had panplexopathy, with the median Narakas score of 3.(34) Ten patients (56%) were managed with therapy alone, four patients (22%) were treated with therapy and Botox injections, and four patients (22%) underwent surgical interventions.
Table 1.
Patient Demographics
| Parameter | |
|---|---|
| Age (years) | |
| Mean | 11.6 |
| Range | 10-17 |
| Gender distribution | |
| Male | 5 |
| Female | 13 |
| Palsy Side | |
| Right | 14 |
| Left | 4 |
| Nerve Involvement | |
| Upper Trunk | 9 |
| Lower Trunk | 0 |
| Panplexopathy | 9 |
| Treatment Type | |
| Therapy Alone | 10 |
| Therapy + Botox | 4 |
| Therapy + Surgery | 4 |
| Narakas Score◆ | |
| Mean | 2.7 |
| Median | 3.0 |
| Range | 2-4 |
The Narakas classification is an accepted measure of the severity of NBPP based on neurological involvement and clinical exam. Scores range from one to four with one being the mildest and four being the most severe. (34)
Qualitative Findings
Qualitative interviews revealed twelve codes and twenty-six subcodes within two broad categories: (1) medical decision-making and (2) quality of life (Appendix A). This analysis will focus on quality of life. Figure 1 displays the frequency of each code and Table 2 summarizes themes and lists representative quotations from each code group. Among both parents and adolescents, we found that quality of life is largely determined by individual personal factors, such as functional limitations, aesthetic concerns and body image, emotional adjustment/psychological coping, and social impact/peer acceptance. The relative contribution of contextual or environmental factors such as, family dynamics, finances, and frequent physical and occupational therapy on global quality of life were more prominent in adult interviews.
Figure 1.
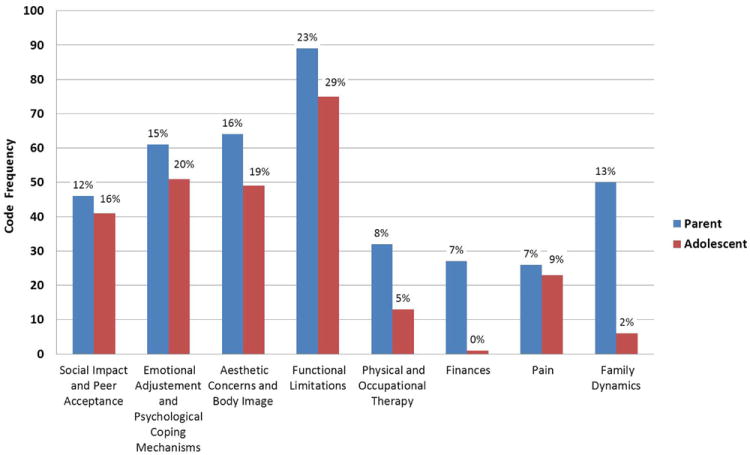
Frequency and Relative Percentages of Codes
Table 2.
Representative Quotations
|
Social Impact and Peer Acceptance
| |
| Peer acceptance and fear of being teased or excluded from social groups was a prominent theme throughout our interviews. In addition, many adolescents commented on the importance and positive influence of obtaining support from other adolescents with NBPP through various camps, therapy groups, or online. | “I really think it’s helpful to talk to other kids with NBPP. It’s helpful to know that I’m not the only one who has gone through all of this.” (Adolescent 44549 – 10 year old female) |
|
| |
|
Emotional Adjustment and Psychological Coping Mechanisms
| |
| Despite their impairments, most adolescents had a positive view of themselves overall. Negative coping mechanisms were more common among younger adolescents and adolescents with greater levels of impairment. Older adolescents generally dealt with their impairments in a constructive manner either through learned compensation techniques, acceptance, or anticipation and alteration of activities if they believed their impairment would limit them in any way. | “I got teased in the fourth grade. They’d call me ‘overblown bicep’ and ‘fat arm.’ Sometimes I would get really self-conscious and discouraged and think that my arm looks weird and that people are staring at me.”(Adolescent 21398– 10 year old female) |
| “My arm used to make me mad and sad because I couldn’t be like everybody else… ‘why can’t I raise my hand like this?’ and stuff like that. I don’t worry about it anymore.”(Adolescent 99859– 17 year old female) | |
|
| |
|
Aesthetic Concerns and Body Image
| |
| Almost all adolescents and parents commented on aesthetics and body image regarding arm position, length/size discrepancies, and clothing restrictions. | “I don’t like wearing half sleeves or quarter length sleeves because it looks like a long sleeve on my right (palsy) arm but a quarter sleeve on my left (non-palsy) arm.” (Adolescent 44549 – 10 year old female) |
|
| |
|
Functional Limitations
| |
| Most adolescents were extremely functional and able to accomplish basic activities of daily living due to the high degree of learned compensation. Many females reported difficulty grooming their hair and both sexes noted difficulty playing in certain sports or musical instruments. | “A lot of times I have to put myself in certain positions to do things, like opening a jar- I have to squeeze it in between my arms instead of gripping it with my hand. And when I type, I have to position my fingers in a different way on the keyboard so I can reach the keys.” (Adolescent 26926 – 13 year old male) |
|
| |
|
Physical and Occupational Therapy
| |
| Many parents commented on the time commitment of formal therapy visits. Depending on the ease of access to a nearby therapist, many adolescents would miss school and their parent would need to take off from work. | “It’s kind of hard to get here if you’re travelling. And a lot of times too, when they get school-age it’s like you’re always having to take them out of school. And I also have to take off from work to take her to therapy.” (Parent 11020– 12 year old female) |
|
| |
|
Finances
| |
| All participants in our study had some form of insurance coverage. However, some parents reported frustrations regarding the cumbersome process of talking with insurers to confirm coverage or extended therapy visits. | “Most insurance companies have limitations on how long you can be in therapy. There’s also the cost of driving to therapy every day. There’s no way I could have worked and done this.” (Parent 21398– 10 year old female) |
|
| |
|
Pain
| |
| Occasionally some patients or their parents reported hypersensitivity or mild discomfort with therapy exercises or prolonged activity. No patients reported significant pain that impaired daily living. | “She occasionally complains of pain in her shoulder area. Maybe 1-2 times per month. It’s never been so bad that we’ve had to take her to see a doctor or seek any medicine for it.” (Parent 90398– 10 year old female) |
|
| |
|
Family Dynamics
| |
| Almost all parents acknowledged the emotional adjustment of other family members in response to raising a child with physical impairment. Many relied on the help of extended family. Few parents reported negative effects on parental/sibling relationships. | “My mother in law and my mother both would watch my older daughter that first year quite a bit while I would take my daughter to therapy” (Parent 21398– 10 year old female) |
Quantitative Findings
We also collected quantitative information to assess functional impairment, measure QOL, and determine patient expectations among NBPP adolescents. Our study included patients with a wide range of residual functional deficits as measured by MRC, Mallet, and Raimondi hand score (Table 3).(24-26) The majority of adolescents and their parents report a relatively good quality of life compared to normal control subjects in the CHQ and the PODCI (Table 4). However, a wide range was observed in both outcomes tools with functional limitations being responsible for the greatest difference in score (larger effect sizes for functional outcome parameters).
Table 3.
Functional Outcome Measures
| Outcome Measure | Mean Score (Range) | Median Score (Range) | Expected Value for Normal Control Subjects |
|---|---|---|---|
| MRC§ | 3.61 (2-5) | 4.00(2-5) | 5 |
|
| |||
| Mallet* | |||
| Active Abduction | 2.72 (2-4) | 3.00(2-4) | 5 |
| External Rotation | 2.50 (2-4) | 2.00(2-4) | 5 |
| Hand to Head/Nape of Neck | 3.17 (2-4) | 3.00(2-4) | 5 |
| Hand to Back | 2.89 (2-4) | 3.00(2-4) | 5 |
| Hand to Mouth | 3.22 (2-4) | 3.00(2-4) | 5 |
|
| |||
| RaimondiΔ | 3.61 (0-5) | 4.00(0-5) | 5 |
British Medical Research Council (MRC) scale for muscle strength measures biceps motor strength graded from 0 (not testable) to 5 (normal strength). MRC grade 3 or higher is considered functional in muscle power. (25)
The Mallet classification system evaluates the global movement and functions of the upper extremity (primarily shoulder function). The scale assesses five movements (listed above) and grades each one from one to five with one being no movement/range of motion and five being normal movement/range of motion. (26)
The Raimondi classification is used to evaluate hand function. Scores range from zero to five with zero representing complete paralysis and five representing excellent function. (27)
Table 4.
Quality of Life Outcome Measures
| Outcome Measure | Mean Score (Range) | Median Score (Range) | Expected Value for Normal Control Subjects | Effect Size◆ | P-value* |
|---|---|---|---|---|---|
| CHQ Adolescent† | |||||
| Physical Functioning | 91 (67-100) | 93 (67-100) | 97 | 0.77 | 0.43 |
| Role/Social – Physical | 96 (56-100) | 100 (56-100) | 97 | 0.12 | 0.09 |
| General Health | 77 (56 -94) | 80 (56-94) | 80 | 0.25 | 0.73 |
| Bodily Pain | 76 (50-100) | 75 (50-100) | 82 | 0.36 | 0.26 |
| Family Activities | 77 (42-100) | 83 (42-100) | 83 | 0.35 | - |
| Family Cohesion | 79 (30-100) | 85 (30-100) | 77 | 0.11 | - |
| Role/Social-Emotional/Behavioral | 93 (72-100) | 94 (72-100) | 93 | 0.01 | 0.17 |
| Self Esteem | 85 (46-100) | 88 (46-100) | 79 | 0.49 | 0.02 |
| Mental Health | 79 (44-100) | 81 (44-100) | 83 | 0.30 | 0.02 |
| Behavior | 85 (58-100) | 88 (58-100) | 84 | 0.09 | 0.05 |
|
| |||||
| CHQ Parent† | |||||
| Physical Functioning | 87 (28-100) | 97 (28-100) | 96 | 0.49 | |
| Role/Social – Physical | 85 (17-100) | 100 (17-100) | 94 | 0.36 | |
| General Health | 74 (10-100) | 80 (10-100) | 73 | 0.06 | |
| Bodily Pain | 69 (10-100) | 70 (10-100) | 82 | 0.55 | |
| Parent Impact – Time | 85 (33-100) | 89 (33-100) | 88 | 0.15 | |
| Parental Impact – Emotional | 68 (25-100) | 67 (25-100) | 80 | 0.61 | |
| Role/Social-Emotional/Behavioral | 86 (22-100) | 100 (22-100) | 93 | 0.28 | |
| Self Esteem | 73 (42-91) | 73 (42-91) | 80 | 0.42 | |
| Mental Health | 71 (35-95) | 75 (35-95) | 79 | 0.52 | |
| Behavior | 75 (30-100) | 75 (30-100) | 76 | 0.05 | |
|
| |||||
| PODCI Adolescent‡ | |||||
| Upper Extremity Function | 91 (63-100) | 96 (63-100) | 99 | 1.01 | 0.50 |
| Transfers and Basic Motility | 98 (92-100) | 98 (92-100) | 99 | 0.30 | 0.65 |
| Sports and Physical Function | 89 (75-100) | 92 (75-100) | 96 | 0.70 | 0.84 |
| Comfort/Pain | 79 (39-100) | 79 (39-100) | 89 | 0.61 | 0.84 |
| Happiness with Physical Condition | 85 (50-100) | 88 (50-100) | 82 | 0.18 | 0.11 |
| Global Function | 89 (74-100) | 90 (74-100) | 96 | 1.00 | 0.94 |
|
| |||||
| PODCI Parent‡ | |||||
| Upper Extremity Function | 88 (21-100) | 92 (21-100) | 99 | 0.79 | |
| Transfers and Basic Motility | 98 (89-100) | 100 (89-100) | 99 | 0.21 | |
| Sports and Physical Function | 89 (67-100) | 92 (67-100) | 94 | 0.49 | |
| Comfort/Pain | 80 (34-100) | 90 (34-100) | 89 | 0.43 | |
| Happiness with Physical Condition | 74 (30-100) | 83 (30-100) | 81 | 0.34 | |
| Global Function | 89 (53 - 99) | 95 (53-99) | 95 | 0.62 | |
Effect sizes were calculated to compare our NBPP study population to normal control values. Effect sizes of 0.2 are defined as small, 0.5 as medium, and 0.8 as large. (33)
Paired t tests were used to evaluate statistically significant differences in response between adolescents and their parents. P values of < 0.05 are considered statistically significant.
The CHQ is an instrument to measure global quality of life for children 5-18 years old. The survey contains both parent and child forms and includes 10 unique physical and psychosocial health domains that may be analyzed individually or combined (parent form only) to derive a physical summary score (including physical functioning, role/social-physical, general health, bodily pain, parental impact-time, parental impact-emotional) and a psychosocial summary score (including parental impact time, parental impact emotion, role/social-emotional/behavioral, self esteem, mental health, behavior).28 Normal values for parental responses were provided in the CHQ Scoring and Interpretation Manual28 and normal values for adolescent responses were extracted from the Raat H, et al. (29)
The PODCI is an instrument specifically designed to assess global quality of life among children with musculoskeletal disabilities and impairments. The survey contains both parent and child forms and includes six functional and psychosocial domains (listed above) that are each scaled from 0-100 with 100 being the highest level of function, happiness or comfort. Global function is calculated as the average of upper extremity function, transfers and basic mobility, sports and physical function, and comfort/pain scales. Normal values were extracted from Hunsaker FG, et al. (30)
With regards to adolescent/parent differences, adolescents were more happy and self-confident with their physical condition than their parents (Table 4, CHQ p=0.002 for self-esteem and mental health; PODCI p=0.11 for happiness with physical condition). In both the CHQ and the PODCI, NBPP adolescents demonstrated a lower quality of life with regards to pain/discomfort than normal control subjects. However, this did not comprise a large volume of conversation during our qualitative interviews.
We also examined patient expectations as measured by the PODCI (Table 5). We found that both adolescents and parents were modestly satisfied with their current condition. Improvements in functional ability and reduction of pain were the categories in which adolescents and parents expected the greatest improvement after treatment.
Table 5.
Patient Expectations
| PODCI Question† | Adolescent Mean Score (Median Score) | Parent Mean Score (Median Score) |
|---|---|---|
| To have pain relief‡ | 2.6 (2.0) | 1.8 (2.0) |
| To look better‡ | 2.6 (3.0) | 2.2 (2.0) |
| To feel better about myself‡ | 2.6 (2.5) | 1.6 (1.0) |
| To sleep more comfortably‡ | 3.0 (3.5) | 1.9 (2.0) |
| To be able to do more activities at home‡ | 2.4 (2.0) | 1.8 (1.5) |
| To be able to do more at school‡ | 2.3 (2.0) | 1.9 (1.5) |
| To be able to do more play or recreational activities‡ (biking, walking, doing things with friends) | 1.9 (1.5) | 1.8 (1.5) |
| To be able to do more sports‡ | 2.0 (1.0) | 1.8 (2.0) |
| To be free from pain or disability as an adult‡ | 2.2 (1.5) | 1.7 (1.0) |
| If you (or your child) had to spend the rest of your (his/her) life with your (his/her) bone and muscle condition as it is right now how would you (he/she) feel about it?Δ | 2.8 (3.0) | 3.0 (3.0) |
Questions within the PODCI outcomes tool to assess patient expectations for various outcome parameters. Questions were worded in the following manner, “As a result of my treatment, I expect…” (30)
Question was scored on a scale from 1-5: 1 = definitely yes, 2 = probably yes, 3 = not sure, 4 = probably not, 5 = definitely not.
Question was scored on a scale from 1-5: 1 = very satisfied, 2 = somewhat satisfied, 3 = neutral, 4 = somewhat dissatisfied, 5 = very dissatisfied.
Finally, at the conclusion of each interview, we asked each adolescent and parent which quality of life survey they preferred (Table 6). Overall, both parents and adolescents preferred the PODCI survey (p < 0.01) and felt it addressed more NBPP specific issues (p = 0.01). The PODCI was viewed as easier to understand (p = 0.36) and took less time to complete (p < 0.01 for adolescents, p = 0.06 for parents). With regards to specific contents, adolescents and parents agreed that the PODCI better evaluated functional issues (p < 0.01) and the CHQ better evaluated emotional issues and family dynamics (p < 0.01).
Table 6.
Survey Preferences
| Parameter | CHQ | PODCI | Both | Neither | P-value |
|---|---|---|---|---|---|
| Finish time (minutes) † | |||||
| Adolescents | 14 (8-25) | 10 (5-22) | - | - | <0.01 |
| Parents | 8 (5-14) | 8 (5-15) | - | - | 0.06 |
|
| |||||
| Preference‡ | |||||
| Adolescents | 6 (33%) | 10 (56%) | 1 (5.5%) | 1 (5.5%) | <0.01 |
| Parents | 6(33%) | 10(56%) | 1 (5.5%) | 1 (5.5%) | |
|
| |||||
| NBPP specific‡ | |||||
| Adolescents | 5 (28%) | 11 (61%) | 1(5.5%) | 1(5.5%) | 0.01 |
| Parents | 3 (17%) | 13 (72%) | 1(5.5%) | 1(5.5%) | |
|
| |||||
| Easy to understand‡ | |||||
| Adolescents | 7 (39%) | 9 (50%) | 2 (11%) | 0(0%) | 0.36 |
| Parents | 3(17%) | 13(72%) | 2(11%) | 0(0%) | |
|
| |||||
| Functional‡ | |||||
| Adolescents | 4(22%) | 11 (61%) | 2(11%) | 1(5.5%) | <0.01 |
| Parents | 6 (33%) | 11(61%) | 0 (0%) | 1(5.5%) | |
|
| |||||
| Emotional‡a | |||||
| Adolescents | 13(72%) | 4 (22%) | 0(0%) | 1(5.5%) | <0.01 |
| Parents | 13(72%) | 4(22%) | 0(0%) | 1(5.5%) | |
Paired t test
Chi-square test or Fisher’s exact test
DISCUSSION
In 2006, the World Health Organization (WHO) developed the Orientation Program on Adolescent Health for Healthcare Providers to increase knowledge among physicians regarding the physical and emotional changes that occur during adolescence, and to improve/adapt health care services to young people’s special needs and concerns.(21,35) Persons in early- to mid-adolescence (10-17 years old) experience major biological and psychosocial transitions, including sexual maturation, growing independence, development of abstract reasoning, and increasing importance of peer acceptance.(21, 26) In this context, chronic impairments of the upper extremity that are primarily managed with elective reconstructive procedures, pose unique challenges when measuring treatment outcomes. Moreover, for relatively rare conditions, such as NBPP, that require unique and varied combinations of treatments from numerous specialists, investigations that comprehensively evaluate long-term outcomes with statistical and clinical significance can be extremely cumbersome to orchestrate, but are nonetheless essential in advancing the care of patients with these conditions.
The results of our study highlight several important themes worthy of further exploration and research. Through semi-structured interviews, we explored the functional/aesthetic ideals and practical logistical factors that influence quality of life among adolescents with NBPP and their families. Prior outcome tools to assess global QOL in both adults and children with upper extremity impairments have primarily focused on physician-derived measures to assess function, psychosocial impact, and pain.(25-27) The findings of our qualitative and quantitative assessment confirm the importance of these issues, but also revealed other patient and system dependent categories relevant to children and adolescents with complex upper extremity impairments, such as social impact and peer acceptance, aesthetic concerns and body image, physical therapy commitments, finances, and family dynamics.
Our quantitative results demonstrated that most adolescents experience a good QOL compared to normal control subjects, and that functional limitations were responsible for the greatest difference in outcome. Accordingly, improvement in functional ability and reduction of pain were the categories in which adolescents and parents expected the greatest improvement after treatment. We conducted a sensitivity analysis comparing CHQ and PODCI scores between adolescents with varying functional deficits, as measured by Narakas, Raimondi, and MRC, that revealed no statistically significant difference. This may imply that objective physical measurements alone are not sufficient to comprehensively evaluate functional impairment and global QOL among these patients.
With regards to adolescent/parent differences, we found that adolescents were generally more emotionally happy and self-confident with their physical condition than their parents. We also found that the relative contribution of contextual environmental or system dependent factors to global QOL were more prominent among adults compared to adolescents. This information is important for clinicians to consider when counseling patients and as adolescents grow older and become more autonomous in their decision making.
Finally, when comparing the CHQ and PODCI, we found that both adolescents and parents preferred the PODCI survey over the CHQ due to its shorter time to completion, easier understanding, and better ability to address NBPP specific functional issues. Overall, the CHQ is better in addressing family dynamics and emotional adjustment/psychological coping mechanisms, and the PODCI is better in addressing functional limitations and aesthetics. Both addressed pain and peer acceptance and neither addressed financial impact or PT/OT time commitment. The PODCI also has the added benefit of assessing patient expectations and providing a dialogue for medical decision making. Given that functional deficits and aesthetics are responsible for the majority of differences in QOL scores and also represented the highest code frequency in our qualitative analysis, this crudely suggests that the PODCI may be more sensitive and more accurate than the CHQ in measuring QOL in adolescents with NBPP. Finances and time commitment were not big contributors in our qualitative analysis, however clinicians should be cognizant of these factors and their impact on outcome during the shared decision making process with their patients.
Several factors limit the results and interpretations of our study. Because qualitative research is open ended and subjective in nature, it is especially prone to investigator bias.(15-19) Our study was also limited by recall bias among participants and subjective biases among interviewers. Preconceived notions of potential hypotheses generated from the data may influence the way interview guides are written and the way the interviewer directs the discussion. Similarly, these same biases may affect how passages and codes are selected, interpreted, and incorporated into the final manuscript. To reduce these limitations, we used a semi-structured interview guide and ensured that each interview guide was independently coded by two members of the study team with conflicts resolved by team consensus.
Our study was also limited by a small sample size and selection bias toward more happy and functionally competent patients able to arrange transportation to accommodate study participation. Although sample size less likely limited the results and conclusions found in our qualitative analysis, it may have affected our ability to determine quantitative effects. We conducted a post-hoc power analysis to determine the minimum sample sizes to achieve 80% power for each category of effect size. For minimum effect sizes our study would have required a sample size of 60 adolescent-parent pairs, whereas for medium and large effect sizes our study would have required sample sizes of 16 and 6 subject pairs, respectively. Thus, for our sample size of 18 subject pairs, we had > 80% power to detect medium and large effect sizes but not small ones.
Despite the above limitations, this study makes a unique and significant contribution to the existing literature on NBPP. In summary, this is the first study to examine quality of life and patient expectations in the NBPP population using both qualitative and quantitative methods. It is also the first study to evaluate adolescents and the varying perspectives between adolescents and their parents or health care proxies. The findings of our study may be used to guide further research regarding the influence of patient expectations and system dependent factors on outcomes for complex pediatric upper extremity reconstructive surgery patients.
Supplementary Material
Acknowledgments
Supported in part by a Clinical Research Grant from the American Society of Surgery of the Hand (to Dr. Lee Squitieri) and by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Dr. Kevin C. Chung).
Footnotes
Level of Evidence: Prognostic, IV
References
- 1.Chung KC, Yang LJ, McGillicuddy JE, editors. Practical Management of Pediatric and Adult Brachial Plexus Palsies. 1. London, England: Elsevier Saunders; 2012. [Google Scholar]
- 2.Hale HB, Bae DS, Waters PM. Current Concepts in the Management of Obstetric Brachial Plexus Birth Palsy. J Hand Surg Am. 2010;35A(2):322–331. doi: 10.1016/j.jhsa.2009.11.026. [DOI] [PubMed] [Google Scholar]
- 3.Waters PM. Comparison of the Natural History, the Outcome of Microsurgical Repair, and the Outcome of Operative Reconstruction in Brachial Plexus Birth Palsy. J Bone Joint Surg Am. 1999;81:649–659. doi: 10.2106/00004623-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 4.McNeely PD, Drake JM. A Systematic Review of Brachial Plexus Surgery for Birth-Related Brachial Plexus Injury. Pediatr Neurosurg. 2003;38:57–62. doi: 10.1159/000068045. [DOI] [PubMed] [Google Scholar]
- 5.Bae DS, Waters PM, Zurakowski D. Classification Systems Measuring Active Motion in Brachial Plexus Birth Palsy. J Bone Joint Surg Am. 2003;85A(9):1733–1738. doi: 10.2106/00004623-200309000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Ho ES, Curtis CG, Clarke HM. Pediatric Evaluation of Disability Inventory: It is Application to Children with Obstetric Brachial Plexus Palsy. J Hand Surg Am. 2006;31A(2):197–202. doi: 10.1016/j.jhsa.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 7.Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating Patient-Based Outcome Measures for Use in Clinical Trials. Health Technol Assess. 1998;2(14):1–74. [PubMed] [Google Scholar]
- 8.Chow A, Mayer EK, Darzi AW, Athanasiou T. Patient-Reported Outcome Measures: The Importance of Patient Satisfaction in Surgery. Surgery. 2009;146(3):435–43. doi: 10.1016/j.surg.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 9.Mancuso CA, Sculco TP, Wickiewicz TL, et al. Patients’ Expectations of Knee Surgery. J Bone Joint Surg Am. 2001;83(7):1005–1012. doi: 10.2106/00004623-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Beaton DE, Clark JP. Qualitative Research: A Review of Methods with Use of Examples from the Total Knee Replacement Literature. J Bone Joint Surg Am. 2009;91(Suppl 3):107–112. doi: 10.2106/JBJS.H.01631. [DOI] [PubMed] [Google Scholar]
- 11.Vitale MG, Levy DE, Moskowitz AJ, et al. Capturing Quality of Life in Pediatric Orthopaedics: Two Recent Measures Compared. J Pediatr Orthop. 2001;21(5):629–635. [PubMed] [Google Scholar]
- 12.Huffman GR, Bagley AM, James MA, Lerman JA, Rab G. Assessment of Children with Brachial Plexus Birth Palsy Using the Pediatric Outcomes Data Collection Instrument. J Pediatr Orthop. 2005;25(3):400–404. doi: 10.1097/01.bpo.0000151055.62356.1b. [DOI] [PubMed] [Google Scholar]
- 13.Bae D, Waters PM, Zurakowski D. Correlation of Pediatric Outcomes Data Collection Instrument with Measures of Active Movement in Children with Brachial Plexus Birth Palsy. J Pediatr Orthop. 2008;28(5):584–592. doi: 10.1097/BPO.0b013e31817bb88b. [DOI] [PubMed] [Google Scholar]
- 14.Giacomini MK, Cook DJ for the Evidence-Based Medicine Working Group. Users’ Guides to the Medical Literature, XXIII: Qualitative Research in Health Care A. Are the Results of the Study Valid? JAMA. 2000;284:357–362. doi: 10.1001/jama.284.3.357. [DOI] [PubMed] [Google Scholar]
- 15.Shauver MJ, Chung KC. A Guide to Qualitative Research in Plastic Surgery. Plast Reconstr Surg. 2010;126:1089–1097. doi: 10.1097/PRS.0b013e3181e60624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giacomini MK, Cook DJ for the Evidence-Based Medicine Working Group. Users’ Guides to the Medical Literature, XXIII: Qualitative Research in Health Care B. What Are the Results and How Do They Help Me Care for My Patients? JAMA. 2000;284:478–482. doi: 10.1001/jama.284.4.478. [DOI] [PubMed] [Google Scholar]
- 17.Mays N, Pope C. Qualitative Research in Health Care: Assessing Quality in Qualitative Research. BMJ. 2000;320:50–52. doi: 10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pope C, Ziebland S, Mays N. Qualitative Research in Health Care: Analysing Qualitative Data. BMJ. 2000;320:114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shauver MJ, Aravind M, Chung KC. A Qualitative Study of Recovery from Type III-B and Type III-C Tibial Fractures. Ann Plast Surg. 2011;66:73–79. doi: 10.1097/SAP.0b013e3181d50eba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aravind M, Shauver MJ, Chung KC. A Qualitative Study of the Decision Making Process for Patients with Severe Lower Leg Trauma. Plast Reconstr Surg. 2010;126:2019–2029. doi: 10.1097/PRS.0b013e3181f4449e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Augutis M, Levi R, Asplund K, Berg-Kelly K. Psychosocial Aspects of Traumatic Spinal Cord Injury with Onset During Adolescence: A Qualitative Study. J Spinal Cord Med. 2007;30(Suppl 1):S55–S64. doi: 10.1080/10790268.2007.11753970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clark JP, Hudak PL, Hawker GA, et al. The Moving Target: A Qualitative Study of Elderly Patients’ Decision-Making Regarding Total Joint Replacement Surgery. J Bone Joint Surg Am. 2004;86A:1366–1374. [PubMed] [Google Scholar]
- 23.Kotsis SV, Chung KC. A Qualitative Assessment of Rheumatoid Hand Surgery in Various Regions of the World. J Hand Surg Am. 2005;30A:649e1–649e10. doi: 10.1016/j.jhsa.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 24.Squitieri L, Larson BP, Chang KW, Yang LJ, Chung KC. Medical Decision-Making Among Adolescents with Neonatal Brachial Plexus Palsy and their Families: A Qualitative Study. Plast Reconstr Surg. doi: 10.1097/PRS.0b013e31828bd52b. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.James MA. Use of the Medical Research Council Muscle Strength Grading System in the upper extremity. J Hand Surg Am. 2007;32:154–156. doi: 10.1016/j.jhsa.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 26.Marcus JR, Clarke HM. Management of Obstetrical Brachial Plexus Palsy Evaluation, Prognosis, and Primary Surgical Treatment. Clin Plast Surg. 2003;30(2):289–306. doi: 10.1016/s0094-1298(02)00100-1. [DOI] [PubMed] [Google Scholar]
- 27.Raimondi P. Evaluation of Results in Obstetric Brachial Plexus Palsy: The Hand. Presented at the International Meeting on Obstetric Brachial Plexus Palsy; Heerlen, The Netherlands. 1993. [Google Scholar]
- 28.Child Health Questionnaire (CHQ): Scoring and Interpretation Manual. Cambridge, MA: HealthActCHQInc; 2008. [Google Scholar]
- 29.Raat H, Mangunkusumo RT, Landgraf JM, et al. Feasibility, Reliability, and Validity of Adolescent Health Status Measurement by the Child Health Questionnaire Child form (CHQ-CF): Internet Administration Compared with the Standard Paper Version. Qual Life Res. 2007;16:675–685. doi: 10.1007/s11136-006-9157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hunsaker FG, Cioffi DA, Amadio PC, et al. The American Academy of Orthopaedic Surgeons Outcomes Instruments. J Bone Joint Surg Am. 2002;84A(2):208–215. doi: 10.2106/00004623-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Wren TA, Sheng M, Hara R, et al. Agreement Among Three Instruments for Measuring Functional Health Status and Quality of Life in Pediatric Orthopaedics. J Pediatr Orthop. 2007;27(2):233–40. doi: 10.1097/01.bpb.0000242436.65940.1a. [DOI] [PubMed] [Google Scholar]
- 32.McCarthy ML, Silberstein CE, Atkins EA, et al. Comparing the Reliability and Validity of Pediatric Instruments for Measuring Health and Well-Being of Children with Spastic Cerebral Palsy. Dev Med Child Neurol. 2002;44(7):468–76. doi: 10.1017/s0012162201002377. [DOI] [PubMed] [Google Scholar]
- 33.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 34.Narakas AO. Obstetrical Brachial Plexus Injuries. In: Lamb DW, editor. The Paralyzed Hand. New York, NY: Churchill Livingstone; 1987. [Google Scholar]
- 35.World Health Organization (WHO) Orientation Programme on Adolescent Health for Health-Care Providers Module B: Meaning of Adolescence. Geneva, Switzerland: WHO Department of Child and Adolescent Health and Development; 2006. [4/24/12]. at: http://www.who.int/maternal_child_adolescent/documents/9241591269/en/index.html. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


