Abstract
Background
It is unclear whether declines in cigarette smoking in the U.S. have resulted in a hardened population of “hardcore” smokers. We studied changes in nicotine dependence severity from 2002–2012, using data from the National Survey on Drug Use and Health.
Methods
We used generalized non-linear factor analysis to examine whether individual Nicotine Dependence Syndrome Scale (NDSS) items functioned differently over time, and whether average NDSS scores changed in a sample of 130,637 current smokers. We also examined trends for individual NDSS sub-scales and whether trends were moderated by tobacco consumption and socio-demographic factors.
Results
Consumption levels and dependence severity both declined over the study period. This decline was driven by priority (e.g., avoiding smoke-free locations) and tolerance dimensions of dependence, while drive (e.g., craving and smoking to relieve negative affect) and continuity (e.g., stability) of smoking did not change. Declines for tolerance were greatest among those without serious psychological distress and among middle-aged smokers. Drive and continuity increased among women and low income smokers.
Conclusions
We did not find evidence of hardening at the population level for smokers in the U.S., 2002–2012. However, there is evidence of hardening when considering drive and continuity-related nicotine dependence among women and low-income smokers, suggesting these sub-groups are experiencing greater severity of craving, smoking to relieve negative affect, and regularity of smoking despite reduced consumption.
Keywords: Nicotine, Dependence, Cigarette, Smoking, Trends
1. INTRODUCTION
The prevalence of cigarette smoking continues to decline in the U.S. (Substance Abuse and Mental Health Services Administration (SAMHSA), 2012). Reductions in smoking are likely the result of a combination of efforts, including public health, improved treatment, and changes in attitudes towards smoking (Cummings et al., 2009). There is concern that tobacco control efforts and concomitant reductions in smoking have resulted a “hardened” population of remaining smokers, who may have more difficulty quitting (National Cancer Institute, 2003; Warner and Burns, 2003).
Previous investigations of trends in nicotine dependence severity have primarily used cigarettes per day, or other measures of consumption, as a marker for dependence (Al-Delaimy et al., 2007; Goodwin et al., 2009; Hyland and Cummings, 2003). The majority of these studies have found either no change or declines in cigarettes per day over time, suggesting dependence severity is not increasing at the population level. However, changes in cigarettes per day and other consumption-based measures of dependence severity may be influenced by factors such as taxation and stigmatization, and thus may not adequately document whether or not dependence severity has increased over time (Hughes, 2003). O’Connor et al. (2006) improved on these previous studies by examining both cigarette consumption and serum cotinine levels from 1988–2002, finding declines in both measures. Contrarily, a more recent investigation found serum cotinine levels had not changed from 1988–2012 (Jarvis et al., In Press). Although studies of serum cotinine provide more objective measure of nicotine exposure, the studies do not capture other dimensions of dependence severity, such as tolerance, withdrawal and craving. Measures that capture both consumption and non-consumption dimensions of nicotine dependence severity may be better suited for accurately assessing change over time (Hughes, 2011).
Two population-based, retrospective birth-cohort studies used DSM measures of nicotine dependence to examine whether dependence increased with decreasing age of cohorts (Breslau et al., 2001 - DSM-III; Goodwin et al., 2009 - DSM-IV), with both finding evidence that smokers were becoming more dependent. These retrospective birth cohort studies have important limitations. For example, previous research has demonstrated differential recall bias between younger and older birth cohorts (Johnson and Schultz, 2005). Further, Hughes (2003) found that smokers in younger cohorts were more willing to label their nicotine addiction as dependence than older cohorts. The results may also be biased by differential mortality, whereby heavier smokers in older cohorts are more likely to have passed away than lighter smokers.
The purpose of the current investigation was to assess whether dependence levels changed among smokers in the general U.S. population from 2002–2012. This time period is particularly relevant, given the number of improvements in tobacco control efforts that occurred in the early-mid 2000s (e.g., smoke-free policies, increased tobacco taxation and price of cigarettes, FDA approval of varenicline). The study improved upon existing research on this topic in several important ways. First, we used serial cross-sectional data from the National Survey on Drug Use and Health to examine changes over time. Second, we used the Nicotine Dependence Syndrome Scale (NDSS; Shiffman et al., 2004), a measure that captures both consumption and non-consumption dimensions of nicotine dependence. In addition to examining trends based on this comprehensive assessment of dependence severity, we were also able to conduct analyses of trends for specific dimensions of dependence, using item-level and subscale analyses. We first conducted Item Response Theory and Differential Item Functioning analyses to examine changes in the performance of individual NDSS items over time, and to generate overall dependence severity factor scores. We then examined trends for the following NDSS sub-scales: drive (e.g., craving and smoking to reduce negative affect), priority (e.g., avoid places where smoking is restricted), tolerance, and continuity (e.g., smoking regularly throughout the day). We tested moderation of trends for overall dependence severity and NDSS sub-scales by factors related to nicotine dependence severity: daily cigarette consumption, other tobacco product use, sex, age, race/ethnicity, income, and serious psychological distress.
2. METHODS
We analyzed data from the National Survey on Drug Use and Health (NSDUH; formerly the National Household Survey on Drug Abuse), an annual nationally representative survey of the U.S. non-institutionalized population, ages 12 and older. This time period (2002–2012) was the longest period available with a consistent measure of nicotine dependence. Computer-assisted, face-to-face interviews were conducted each year by professionals from the Research Triangle Institute. Full details regarding the sampling procedures can be found at the SAMHSA Substance website (SAMHSA, 2013).
Important changes were made to the NSDUH sampling design during the 2002–2012 period. Subsequent to 2005, census tracts were used for the first stage of sampling rather than pre-defined geographical areas. First-stage sampling units had 50% overlap for each consecutive year from 2002–2004, and then again from 2004–2012 in order to improve consistency between samples (without overlapping respondents; SAMHSA, 2013). Our study was limited to current smokers (100+ cigarettes in their lifetime and at least once during the past 30 days). The sample sizes for each survey year were: 2002, n=12,757; 2003, n=12,967; 2004, n=12,599; 2005, n=12,434; 2006, n=11,978; 2007, n=11,934; 2008, n=11,617; 2009, n=11,470; 2010, n=11,343; 2011, n=11,169; 2012, n=10,412. The total sample size was n=130,637 smokers. The age distribution for smokers in this final combined sample was as follows: 12 to 17 years − 8.69%; 18 to 25 – 48.70%; 26 to 34 – 15.09%; 35 to 49 – 19.16%; 50 to 64 – 6.59%; 65 or older – 1.77%. Fifty-two percent were men; 72% were white/Caucasian, 9.5% were Black/African American, and 10.5% were Hispanic; and the median income category was $20,000–$49,000.
2.1. Summary of analyses
2.1.1 Trends for general nicotine dependence severity
We used the Nicotine Dependence Syndrome Scale (Shiffman et al., 2004) as our primary measure of nicotine dependence. This measure has demonstrated strong psychometric properties as a multi-dimensional assessment of nicotine dependence (e.g., associations with dependence-relevant measures, prediction of withdrawal/urges to smoke/cessation, high internal reliability, and adequate test-retest reliability; Shiffman et al., 2004). We considered two options for analyzing trends for overall dependence severity. The first and simplest option was to generate summary NDSS scores for each smoker, and compare mean scores across years in the study. This approach had important limitations, such as the skewed nature of the variable’s distribution, and the inability to examine trends for individual symptoms over time [i.e., differential item functioning (DIF; Liu et al., 2013)].
In order to resolve these issues, we adapted integrated data analysis (IDA) methodology to our study aims, and used moderated nonlinear factor modeling (MNLFA) as our main analytic tool (Bauer and Hussong, 2009; Rose et al., 2013). This approach allowed us to do four things: 1) examine differential item functioning for individual items in 2003–2012 relative to 2002, 2) use this information to generate a psychometrically equivalent measure of nicotine dependence across 2002–2012, 3) generate nicotine dependence severity scores for each participant based on this psychometrically equivalent measure, and 4) examine whether both mean and variance for nicotine dependence severity changed from 2002–2012.
IDA is a general framework of methods for combining data from varying samples. This is achieved by creating psychometrically equivalent measures across studies. We achieved this goal by utilizing MNLFA, which is rooted in generalized linear modeling and item response theory (IRT; Bauer and Hussong, 2009). IRT is based on the assumption that items from a measure (in this case, NDSS) are representative of a range of ability (in this case nicotine dependence severity) for a single underlying, normally distributed latent factor (nicotine dependence). Our base model was a 2-PL IRT model (Embretson and Reise, 2000). In this model, each item in the measure has an item location parameter (the level of nicotine dependence severity represented by that item) and a discrimination parameter (each item’s ability to differentiate between those scoring higher and lower on nicotine dependence severity). These parameters can then be used with any given individual’s item responses to generate a factor score (each smoker’s nicotine dependence severity) for that individual.
MNLFA is able to extend on this base 2-PL IRT model in two important ways. First, the model can include estimates for the mean and variance of the factor scores. Second, one can include interaction terms for model parameters, allowing for a test of effect moderation by other key variables. For example, in the current investigation, this approach allowed us to examine whether item location and item discrimination were moderated by study year (i.e., testing item DIF), and whether mean factor score and variance were moderated by study year (i.e., testing whether overall nicotine dependence or variance in nicotine dependence varied by year, after accounting for DIF).
All analyses for the current investigation were conducted using MPlus (to generate initial parameter estimates), and SAS PROC NLMIXED (to conduct MNLFA modeling and generate nicotine dependence scores). NDSS responses for each item ranged from 1 to 5 (“not at all true” to “extremely true”). First, we dichotomized the items to fit the 2-PL IRT model. We re-coded each NDSS symptom to 0 or 1, based on whether the respondent reported the symptom was at least “somewhat true” of them. We used “somewhat true” as a cut-off because this translated to a “yes vs. no” response for whether the respondent had experienced the symptom. This approach is consistent with other non-consumption based measures of nicotine dependence (e.g., the DSM). We then conducted factor analyses on the NDSS symptoms in order to select items that best represented a single latent nicotine dependence factor for further analyses. We also wanted to limit our analyses to the most parsimonious number of symptoms possible, while maintaining an adequate representation of nicotine dependence. Our final selection of NDSS items are presented in Table 1.
Table 1.
Factor loadings for Nicotine Dependence Syndrome Scale items included in measure of overall nicotine dependence severity
| Symptom | Included in severity measure (yes/no) |
Factor loading: |
|---|---|---|
| After not smoking for a while, you need to smoke in order to feel less restless and irritable |
Yes | 0.60 |
| When you don’t smoke for a few hours, you start to crave cigarettes |
Yes | 0.72 |
| You sometimes have strong cravings for a cigarette where it feels like you’re in the grip of a force you can’t control |
Yes | 0.56 |
| You feel a sense of control over your smoking – that is, you can “take it or leave it” at any time |
No a | |
| You tend to avoid places that don’t allow smoking, even if you would otherwise enjoy them. |
Yes | 0.35 |
| Do you have any friends who do not smoke cigarettes? |
No b | --- |
| There are times when you choose not to be around your friends who don’t smoke because they won’t like it if you smoke |
No b | --- |
| Even if you are traveling a long distance, you would rather not travel by airplane because you would not be allowed to smoke |
Yes | 0.35 |
| You sometimes worry that you will run out of cigarettes |
Yes | 0.62 |
| You smoke cigarettes fairly regularly throughout the day |
Yes | 0.72 |
| You smoke about the same amount on weekends as on weekdays |
No c | --- |
| You smoke just about the same number of cigarettes from day to day |
Yes | 0.59 |
| It’s hard for you to say how many cigarettes you smoke per day because the number often changes |
No a | --- |
| It’s normal for you to smoke several cigarettes in an hour, then not have another one until hours later |
Yes | 0.32 |
| The number of cigarettes you smoke per day is often influenced by other things – how you are feeling, or what you are doing for example |
No c | --- |
| Your smoking is not affected much by other things. For example, you smoke about the same amount whether you’re relaxing or working, happy or sad, alone or with others |
No a | --- |
| Since you started smoking, the amount you smoke has increased |
Yes | 0.64 |
| Compared to when you first started smoking, you need to smoke a lot more now in order to be satisfied |
Yes | 0.68 |
| Compared to when you first started smoking, you can smoke much, much more now before you start to feel anything |
Yes | 0.53 |
Not included because of low factor loading (< 0.30)
Not included because skip pattern resulted in missing data for a portion of smokers
A similar symptom was included in the final measure
When calculating MNLFA models, we used adaptive Gaussi-Hermite quadrature, specifying 15 quadrature points and a maximum of 1000 iterations, and a gradient cut-off of 0.01. We considered DIF to be evident if both of two criterion were satisfied: 1) the DIF coefficient (i.e., the interaction between item location/discrimination and study year) for an item was statistically significant between study years (p < 0.05), and 2) the parameter estimate was greater than 0.2. We used the second criterion because with such a large sample size, even non-meaningful DIF was found to be highly statistically significant (even after accounting for multiple testing). We selected the cut-off of 0.2 because the parameter estimates have a scale of standardized units, and effect sizes < 0.2 are generally accepted to be small (Kirk, 1996). After testing DIF for each item, we generated a nicotine dependence score for each smoker, controlling for statistically significant DIF (i.e., each participant’s nicotine dependence score was based on an underlying latent construct that was equivalent across study years).
We then used separate linear regression models to examine whether NDSS factor scores for nicotine dependence changed over time, regressing dependence score on study year. We separately examined study year as both categorical and continuous variables, in order to calculate mean estimates for each year and examine linear trends over time.
2.1.2. Nicotine Dependence Sub-Scales
In addition to examining trends for overall dependence, we also examined trends for NDSS-subscales. Shiffman et al. (2004) divided NDSS items into 5 sub-scales: drive, priority, tolerance, continuity, and stereotypy. Due to similarities between continuity and stereotypy, these scales were combined in the current investigation. Items for “drive” (alpha = 0.82) included: 1) need to smoke to feel less irritable, 2) start to crave cigarettes when you don’t smoke for a few hours, 3) craving of cigarettes is like a strong force you can’t control, and 4) you feel a sense of control over your smoking (reverse coded?). Items for “priority” (alpha = 0.53) included: 1) Tend to avoid places that don’t allow smoking, and 2) when traveling long distances, tend to avoid traveling by airplane. Items for “tolerance” (alpha = 0.83) included: 1) amount of smoking has increased since started smoking, 2) need to smoke a lot more to be satisfied, and 3) need to smoke much more now before feeling anything. Items for “continuity” (alpha = 0.59) included: 1) smoke cigarettes fairly regularly throughout the day, 2) smoke same amount on weekends as on weekdays, 3) smoke same number of cigarettes from day to day, 4) number of cigarettes smoked per day often changes (reverse coded), 5) number of cigarettes smoked per day are influenced by other things (reverse coded), and 6) my smoking is not much affected by other things. Each item ranged in responses from 1 to 5 (“not at all true” to “extremely true”). Respondents’ sub-scale scores were calculated by averaging items for each scale, and then converting to standardized units. These standardized scales were then regressed on study-year as a continuous variable to examine linear changes in trends over time.
2.2 Moderation
We used linear regression to examine interactions between study year and moderator variables of interest in association with overall NDSS factor scores as well as scores for NDSS sub-scales. We examined moderation of linear changes in scores over time by the following variables: cigarette consumption (< 1–15, 16–25, and 26+ cigarettes per day), other tobacco product use (any past month use of smokeless tobacco, snuff, cigars, pipe tobacco, or chew), sex, age categories (12–17, 18–25, 26–34, 35–49, 50–64, and 65+ years) , race/ethnicity (Caucasian/European American, non-Hispanic; Black/African American, non-Hispanic; Native American/Alaska Native, non-Hispanic; Asian/Native Hawaiian/Pacific Islander, non-Hispanic; other, non-Hispanic, and Hispanic), and income (< $20,000 per year; $20,000–49,999; $50,000–74,999; and > $75,000). We also examined moderation by serious psychological distress (SPD), using Kessler’s K6 and standard cut-off scores (Kessler et al., 2003, 2005). When conducting tests for overall differences between variable sub-groups, alpha values were Sidak-adjusted to account for multiple testing. Post hoc comparisons between sub-groups also accounted for multiple comparisons using a Sidak correction.
3. RESULTS
3.1. Prevalence of smoking and proportion of heavy smokers
The prevalence of current cigarette smoking (100+ cigarettes in a lifetime, smoked at least once during the past month) consistently declined throughout 2002–2012, from 23.6% to 18.9%. Among those who smoked, the proportion of heavy smokers (25+ cigarettes per day) also declined, from 8.8% to 5.6%.
3.2. Dependence trends
3.2.1 NDSS differential item functioning over time
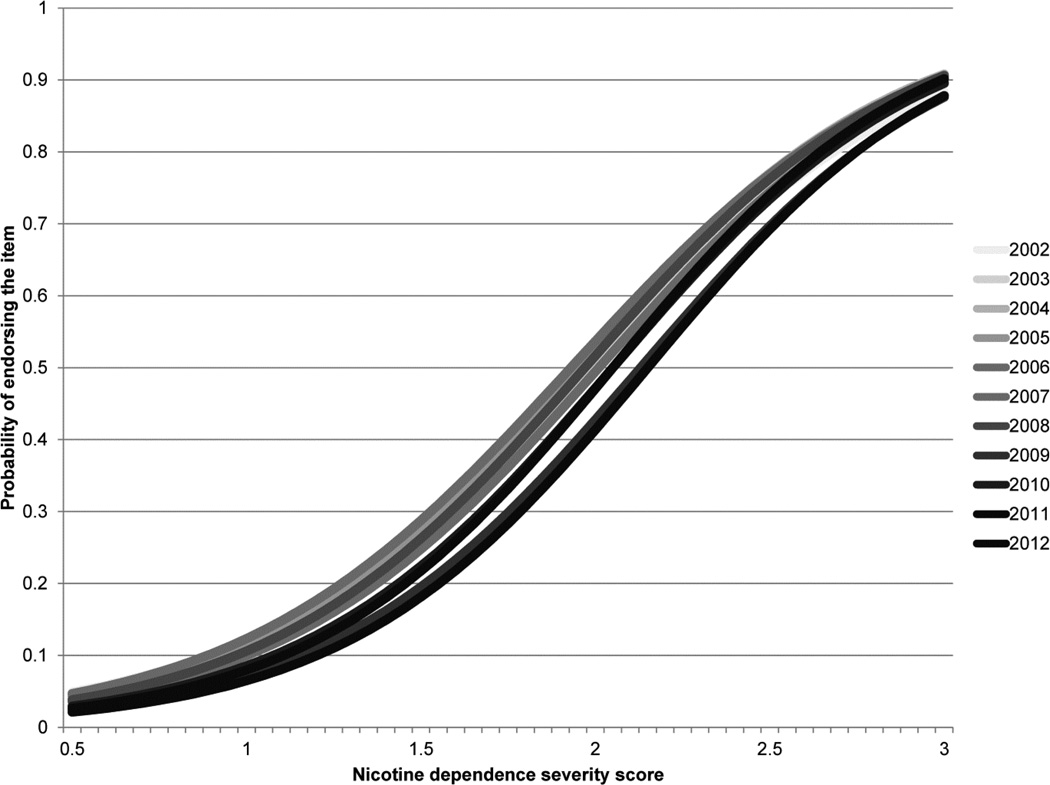
Table 1 displays our final selection of NDSS items, as well as factor loadings (range 0.32 to 0.72) for each item. A summary of findings for item DIF over time is presented in Table S11. Three items demonstrated consistent trends over time: 1) “After not smoking for a while, you need to smoke in order to feel less restless and irritable,” 2) You sometimes have strong cravings for a cigarette where it feels like you’re in the grip of a force you can’t control,” and 3) “Compared to when you first started smoking, you need to smoke a lot more now in order to be satisfied.” Figure 1 displays the item characteristic curves for this first item (need to smoke to feel less restless/irritable), 2002–2012 which became indicative of more severe nicotine dependence over time. A similar trend was found for the symptom “grip of a force you can’t control.” The opposite trend was found for the item, “need to smoke a lot more now to be satisfied” – this item became indicative of less severe dependence over time.
Figure 1.
Item characteristic curves (ICC) for the dependence symptom “smoke to relieve restlessness/irritability,” 2002–2012. Darker lines represent more recent years. The shift to the right over time demonstrates the symptom became indicative of greater levels of dependence severity over the study period.
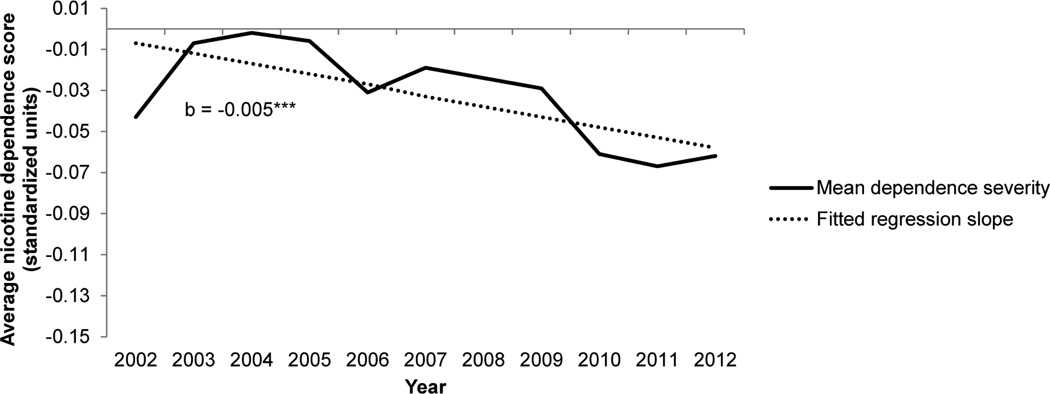
3.2.2. Trends for overall nicotine dependence severity, 2002–2012
We found evidence for a small decline in nicotine dependence severity (Figure 2). The slope for a linear time variable was −0.005 (95% CI = −0.007, −0.004). Over the study period, dependence level decreased by approximately 0.05 standardized units. There was no significant change in variability for the nicotine dependence severity measure over the study period.
Figure 2.
Change in nicotine dependence among current cigarette smokers, 2002–2012. Data source: National Survey on Drug use and Health. ***p < 0.001.
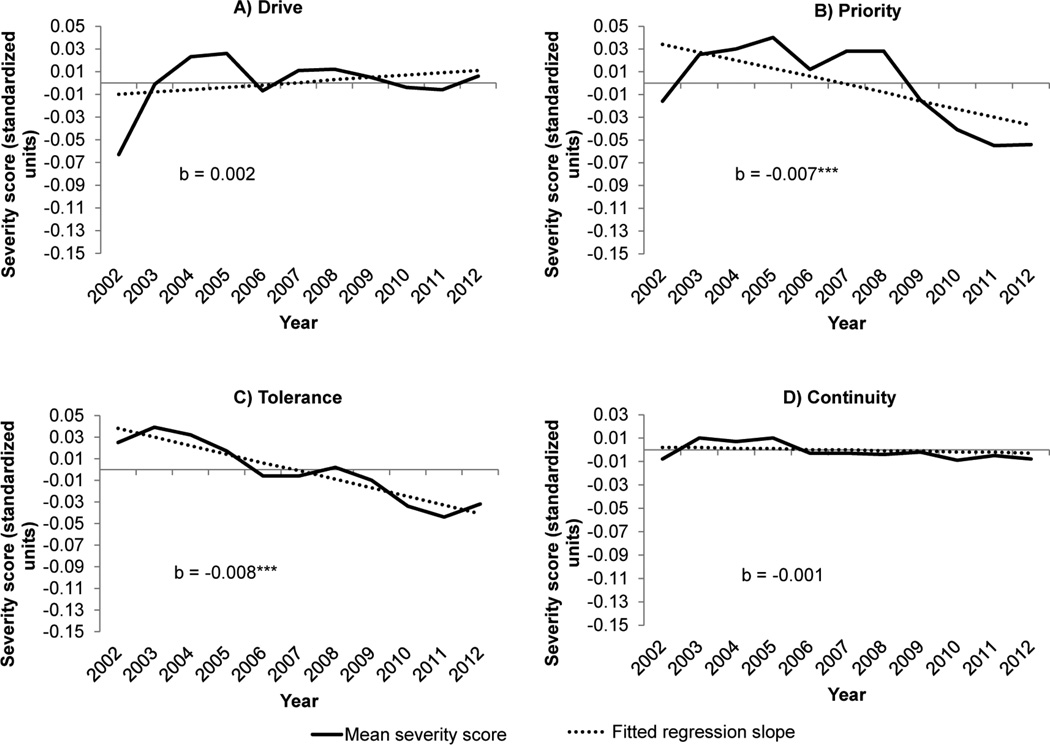
3.2.3 Trends for NDSS sub-scales, 2002–2012
The direction and significance of dependence severity trends varied over sub-scales. Mean scores for priority and tolerance decreased over the study period (b = −0.007, 95% CI = −0.009, −0.005; b = −0.008, 95% CI = −0.010, −0.006 for priority and tolerance, respectively). There was no change for the continuity or drive sub-scales (p > 0.05).
3.3. Moderation analyses
Overall nicotine dependence severity was moderated by SPD and age, such that declines in severity were greatest among middle-aged smokers and those without SPD (Table 2). For the “drive” sub-scale (e.g., craving, smoking to reduce negative affect), the greatest increases were found among those who smoked 6 to 25 cigarettes per day. Drive increased among women, but not men, and among those with lower income, but not those with higher income. Priority (e.g., avoiding situations where smoking is not allowed) decreased among light smokers, remained constant among moderate smokers, and increased among the heaviest smokers. Tolerance decreased most among middle aged smokers and those without SPD. Continuity of smoking throughout the day/week increased among women and decreased among men. Continuity increased among those with low income but not among those with high income, and decreased among those without SPD but not among those with SPD. Continuity also decreased to the greatest amount among smokers aged 50–64 years.
Table 2.
Moderation of trends for overall dependence severity and individual NDSS sub-scales, 2002–2012
| Overall severity b (95% CI) |
Drive b (95% CI) |
Priority b (95% CI) |
Tolerance b (95% CI) |
Continuity b (95% CI) |
|
|---|---|---|---|---|---|
| Cigarettes per day | NS | NS | |||
| <1 to 5 | |||||
| Intercept | −0.59 (−0.61, −0.58) | −0.25 (−0.27, −0.24) | −0.60 (−0.61, −0.58) | ||
| Slope | 0.005 (0.003, 0.007)a | −0.004 (−0.007, −0.002)a | 0.004 (0.002, 0.007)a | ||
| 6 to 15 | |||||
| Intercept | 0.13 (0.11, 0.14) | −0.04 (−0.05, −0.02) | 0.11 (0.10, 0.13) | ||
| Slope | 0.014 (0.012, 0.017)b | −0.002 (−0.004, 0.001)ab | 0.014 (0.011, 0.016)b | ||
| 16 to 25 | |||||
| Intercept | 0.47 (0.45, 0.49) | 0.28 (0.26, 0.30) | 0.56 (0.55, 0.58) | ||
| Slope | 0.016(0.013, 0.019)b | 0.003 (0.000, 0.007)b | 0.008 (0.005, 0.012)a | ||
| 26+ | |||||
| Intercept | 0.66 (0.63, 0.69 | 0.80 (0.76, 0.83) | 0.61 (0.58, 0.64) | ||
| Slope | 0.006 (0.001, 0.012)ab | 0.007 (0.001, 0.013)b | 0.002 (−0.004, 0.008)a | ||
| Sex | NS | NS | NS | ||
| Men | |||||
| Intercept | −0.09 (−0.11, −0.08) | −0.05 (−0.06, −0.04) | |||
| Slope | −0.001 (−0.004, 0.001)a | −0.004 (−0.006, −0.002)a | |||
| Women | |||||
| Intercept | 0.07 (0.06, 0.09) | 0.06 (0.04, 0.07) | |||
| Slope | 0.007 (0.005, 0.010)b | 0.004 (0.001., 0.006)b | |||
| Age | NS | NS | |||
| 12 to 17 | |||||
| Intercept | 0.07 (0.04, 0.09) | 0.27 (0.23, 0.30) | −0.18 (−0.21, −0.15) | ||
| Slope | −0.006 (−0.011, −0.001)ab | −0.004 (−0.010, 0.002)ab | −0.006 (−0.012, 0.000)a | ||
| 18 to 25 | |||||
| Intercept | −0.06 (−0.08, −0.05) | 0.06 (0.04, 0.07) | 0.00 (−0.01, 0.01) | ||
| Slope | −0.003 (−0.005, −0.001)a | −0.003 (−0.006, −0.001)a | −0.001 (−0.004, 0.001)a | ||
| 26 to 34 | |||||
| Intercept | −0.08 (−0.10, −0.06) | −0.08 (−0.11, −0.06) | 0.00 (−0.02, 0.03) | ||
| Slope | −0.003 (−0.007, −0.001)ab | −0.003 (−0.008, 0.001)ab | −0.004 (−0.00, 0.008)ab | ||
| 35 to 49 | |||||
| Intercept | 0.10 (0.09, 0.12) | −0.01 (−0.03, −0.01) | 0.09 (0.07, 0.11) | ||
| Slope | −0.009 (−0.013, −0.006)ab | −0.011 (−0.015, −0.008)b | −0.002 (−0.006, 0.002)ab | ||
| 50 to 64 | |||||
| Intercept | 0.17 (0.13, 0.20) | −0.05 (−0.09, −0.01) | 0.11 (0.07, 0.15) | ||
| Slope | −0.013 (−0.018, −0.007)b | −0.014 (−0.020, −0.007)ab | −0.012 (−0.019, −0.005)b | ||
| 65+ | |||||
| Intercept | −0.04 (−0.10, 0.03) | −0.27 (−0.34, −0.19) | −0.10 (−0.18, −0.02) | ||
| Slope | 0.005 (−0.006, −0.016)ab | −0.006 (−0.018, 0.007)ab | 0.011 (−0.002, 0.023)ab | ||
| Annual Income | NS | NS | NS | ||
| <$20,000 | |||||
| Intercept | −0.02 (−0.04, 0.00) | −0.01 (−0.02, 0.01) | |||
| Slope | 0.007 (0.004, 0.010)a | 0.006 (0.002, 0.009)a | |||
| $20,000 to 49,999 | |||||
| Intercept | 0.02 (0.00, 0.04) | 0.04 (0.02, 0.05) | |||
| Slope | 0.003 (0.000, 0.005)ab | −0.002 (−0.005, 0.001)b | |||
| $50,000 to 74,999 | |||||
| Intercept | 0.01 (−0.02, 0.03) | 0.01 (−0.01, 0.04) | |||
| Slope | −0.002 (−0.007, 0.002)b | −0.001 (−0.006, 0.003)ab | |||
| ≥$75,000 | |||||
| Intercept | −0.10 (−0.12, −0.07) | −0.09 (−0.12, −0.07) | |||
| Slope | −0.002 (−0.007, 0.002)b | −0.005 (−0.009, 0.000)b | |||
| SPD | NS | NS | |||
| No | |||||
| Intercept | −0.03 (−0.04, −0.02) | −0.02 (−0.03, 0.00) | 0.01 (0.00, 0.02) | ||
| Slope | −0.011 (−0.012, −0.009)a | −0.014 (−0.016, −0.011)a | −0.007 (−0.009, −0.004)a | ||
| Yes | |||||
| Intercept | 0.20 (0.18, 0.22) | 0.28 (0.25, 0.30) | 0.23 (0.21, 0.26) | ||
| Slope | −0.005 (−0.008, −0.001)b | −0.004 (−0.009, 0.000)b | 0.002 (−0.002, 0.006)b |
Note: NS = non-significant overall interaction term, using a Sidak-corrected alpha of 0.0014. Bold slopes indicate statistically significant trends (p < 0.05). Within each variable, slopes that do not share a letter were significantly different from each other after adjusting for multiple comparisons. For race/ethnicity, C/EA = Caucasian/European American, B/AA = Black/African American, NA/AN = Native American/Alaskan Native, A/NH/PI = Asian/Native Hawaiian/ Pacific Islander, NH = non-Hispanic. SPD = serious psychological distress. All estimates are reported in standardized units.
4. DISCUSSION
We did not find evidence of hardening among smokers in the U.S. from 2002–2012. Rather, nicotine dependence severity declined over this time period. This decline was primarily driven by symptoms related to priority (e.g., avoiding situations where one cannot smoke) and tolerance, while there was no evidence of change in drive (e.g., cravings or smoking to relieve negative affect) or continuity of smoking throughout the day/week. Declines in dependence severity were greater among those without serious psychological distress than those with, suggesting growing differences in dependence severity based on mental health status. Declines in severity were also greatest among middle-aged smokers. Contrary to general trends, women and low-income evidenced increased severity for both the drive and continuity dimensions of nicotine dependence, providing evidence of hardening among these sub-groups. When stratified by cigarettes per day, smokers in the U.S. exhibited increases in drive at all levels of nicotine consumption, and increases in continuity in all but the heaviest smokers.
Declining nicotine dependence severity has also been noted in studies using consumption-based measures of nicotine dependence (Al-Delaimy et al., 2007; Hyland and Cummings, 2003; O'Connor et al., 2006). These declines may also apply to non-consumption dimensions of nicotine dependence, suggesting hardening is not occurring at the population-level. However, declines in dependence were greater among those without serious psychological distress than among those with serious psychological distress, mirroring patterns for cigarette consumption (Lê Cook et al., 2014) and suggesting growing differences in dependence based on mental health status.
Declines in dependence severity were driven by items related to priority (e.g., avoiding situations where smoking is not allowed) and tolerance. As smoke-free policy becomes increasingly prevalent smokers may feel less inclined to try to avoid smoke-free places and rather adapt by reducing cigarette consumption (Hackshaw et al., 2010; Tauras, 2006). Declines in priority were most evident among the lightest smokers, while moderate smokers did not change priority, and the heaviest smokers actually increased priority. Increases in smoke-free policies may be driving the heaviest smokers to avoid greater numbers of smoke-free locations, although this mechanism is speculative.
Tolerance also declined over the study period. Symptoms of tolerance, as defined in the NDSS, are endorsed by those consuming greater numbers of cigarettes since they started smoking, or needing more cigarettes to produce a desired effect. In other words, tolerance is in essence based on the difference in number of cigarettes per day one originally smoked and the number of cigarettes per day one currently smokes. If average cigarettes per day have decreased, one would expect the difference between early smoking and current smoking to have decreased, and thus NDSS tolerance would have decreased as well. It follows, then, that tolerance as measured by the NDSS may be a less accurate marker of dependence in 2012 than 2002. Recent findings from Jarvis et al. (in press) further illustrate this point. The researchers conducted an investigation of NHANES Data from 1988–2012, and found that although average cigarettes per day had declined among smokers in the U.S., serum cotinine levels had not changed. The authors concluded smokers have compensated for fewer cigarettes per day by increasing their amount of nicotine intake from each cigarette. Therefore assessments of tolerance that are based on self-reported changes in amount of smoking may be increasingly less accurate than those based on biological markers of actual nicotine consumption.
This study did not find evidence of change over time in drive (e.g., craving, or smoking to relieve negative affect) or continuity of smoking for the overall population of smokers. In other words, despite declines in cigarettes per day there was no change in craving, smoking to relieve symptoms of negative affect, or regularity of smoking throughout the day/week. This finding explains why item-level analyses showed increased severity over time for drive-related items relative to other dependence symptoms (e.g., tolerance/priority), and why, when stratified by cigarettes per day, each category of consumption exhibited increased severity of drive and continuity (with the exception of the heaviest smokers for continuity). Consistent with Jarvis et al. (In Press), this study suggests smokers are becoming equally dependent on fewer cigarettes per day.
Despite the lack of hardening for the overall population of smokers, there was some evidence of hardening among specific sub-groups. We found increases in the drive and continuity dimensions of dependence severity among women, and among low-income smokers. Women and low-income smokers have a commonality, in that stress and negative affect are salient factors related to smoking in both groups (Back et al., 2008; McKee et al., 2003; Perkins et al., 2012, 2013; Saladin et al., 2012; Siahpush et al., 2003; Siahpush and Carlin, 2006; Weinberger and McKee, 2012). These dimensions of dependence warrant particular attention, as they are strongly related to difficulty with smoking cessation (Sledjeski et al., 2007; Sterling et al., 2009). Further, women and low-income smokers had higher drive and continuity in 2002 than men and higher income smokers, respectively, indicating that sex and income differences in craving/smoking to relieve negative affect and continuity of smoking have increased over time.
Changes over time found in this study were small in effect size. Converting standardized units to percentiles, changes over time were generally in the range of 2–10 percentile points (results not shown). This does not imply that the effects are not meaningful. Effect sizes in this range are consistent with those for related tobacco statistics over the same time period, such as changes in smoking prevalence and consumption levels. Further, when applied across the entire population of U.S. smokers there may be important public health implications of changes in the small effect-size range for tobacco use variables (Lightwood and Glantz, 1997).
There are limitations of this study. Due to the advanced statistical methods applied in these analyses, we were unable to apply the NSDUH survey weights to our estimates. Thus, estimates for each individual year may be slightly different than they would be if we had applied weights. However, the large sample size (over 130,000) suggests that this study’s conclusions, particularly for trends over time, are indeed representative of the general U.S. population. As previously noted, it is unclear how our conclusions may have changed with a more expansive time-period. For example, hardening of the smoking population may have occurred leading up to 2002, but then tapered off from 2002–2012. The NSDUH sampling methodology changed over the study period (as outlined in Methods), and it is unclear how these changes may have influenced the analyses. Our assessment of cigarettes per day was limited to categories rather than a continuous measure based on available data in the NSDUH survey. Finally, it is unclear whether these findings extend to treatment-seeking samples. Previous research suggests that nicotine dependence may be increasing, rather than decreasing, among cigarette smokers seeking help for quitting (Irvin et al., 2003). Studies on both population and treatment seeking samples are needed to continue understanding the changing dimensions of cigarette smoking in the U.S.
Despite these limitations, the current investigation added to existing literature on nicotine dependence trends, showing dependence severity did not increase from 2002–2012 among the general population of U.S. smokers. Particular sub-groups of smokers may warrant increasing attention: those with poor mental health/psychiatric co-morbidity, women, and those of low SES. Despite declines in cigarette consumption, smokers may be becoming equally dependent on fewer cigarettes per day, demonstrating an increasingly greater disconnect between actual number of cigarettes smoked and level of nicotine dependence severity, particularly when considering smoking to relieve craving/symptoms of negative affect, and continuity of smoking throughout the day/week.
Supplementary Material
Figure 3.
Severity scores for NDSS sub-scales, 2002 vs. 2012. Drive consisted of items related to craving and smoking to relieve symptoms of negative affect. Priority consisted of items related to avoiding situations in which smoking was not allowed. Tolerance consisted of items related to increased number of cigarettes since stated smoking. Continuity consisted of items related to regularity of smoking throughout the day and week. Data source: National Survey on Drug use and Health. ***p < 0.001.
Highlights.
We did not find evidence of increased dependence severity among cigarette smokers in the U.S., 2002–2012
Differences in dependence severity based on mental health status grew over the study period
Severity of symptoms related to craving, smoking to relieve negative affect, and continuity (i.e., regularity) of smoking increased among women and low-income smokers
Acknowledgments
Role of Funding Source
Funding for this study was provided by NIMH (T32MH01423539, PI: Dr. Heping Zhang) and NIDA (P50DA03394502, PI: Dr. Sherry McKee; DA029834, PI: Dr. Jennifer Rose). NIMH and NIDA had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Author Disclosures:
Contributors
PHS led the design of the study, conducted the analyses, and wrote the first draft of the manuscript. JSR provided consulting on the statistical analyses, and assisted with study design. GAG, SHS, and CMM also contributed to the study design. All authors substantially contributed to and approved of the final draft of the manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
REFERENCES
- Al-Delaimy WK, Pierce JP, Messer K, White MM, Trinidad DR, Gilpin EA. The California Tobacco Control Program’s effect on adult smokers: (2) daily cigarette consumption levels. Tob. Control. 2007;16:91–95. doi: 10.1136/tc.2006.017061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back SE, Waldrop AE, Saladin ME, Yeatts SD, Simpson A, McRae AL, Upadhyaya HP, Contini Sisson R, Spratt EG, Allen J. Effects of gender and cigarette smoking on reactivity to psychological and pharmacological stress provocation. Psychoneuroendocrinology. 2008;33:560–568. doi: 10.1016/j.psyneuen.2008.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer DJ, Hussong AM. Psychometric approaches for developing commensurate measures across independent studies: traditional and new models. Psychol. Methods. 2009;14:101–125. doi: 10.1037/a0015583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Johnson EO, Hiripi E, Kessler RC. Nicotine dependence in the united states: prevalence, trends, and smoking persistence. Arch. Gen. Psychiatry. 2001;58:810–816. doi: 10.1001/archpsyc.58.9.810. [DOI] [PubMed] [Google Scholar]
- Cummings KM, Fong GT, Borland R. Environmental influences on tobacco use: evidence from societal and community influences on tobacco use and dependence. Annu. Rev. Clin. Psychol. 2009;5:433–458. doi: 10.1146/annurev.clinpsy.032408.153607. [DOI] [PubMed] [Google Scholar]
- Embretson SE, Reise SP. Item response theory. Psychology Press. 2000 [Google Scholar]
- Goodwin RD, Keyes KM, Hasin DS. Changes in cigarette use and nicotine dependence in the United States: evidence From the 2001–2002 Wave of the National Epidemiologic Survey of Alcoholism and Related Conditions. Am. J. Public Health. 2009;99:1471–1477. doi: 10.2105/AJPH.2007.127886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackshaw L, McEwen A, West R, Bauld L. Quit attempts in response to smoke-free legislation in England. Tob. Control. 2010;19:160–164. doi: 10.1136/tc.2009.032656. [DOI] [PubMed] [Google Scholar]
- Hughes JR. Those Who Continue To Smoke: Is Achieving Abstinence Harder And Do We Need To Change Our Interventions? Bethesda: U.S. Department Of Health And Human Services, Public Health Service National Institutes Of Health, National Cancer Institute; 2003. The evidence for hardening. Is the target hardening? [Google Scholar]
- Hughes JR. The hardening hypothesis: is the ability to quit decreasing due to increasing nicotine dependence? A review and commentary. Drug Alcohol Depend. 2011;117:111–117. doi: 10.1016/j.drugalcdep.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Cummings KM. In: Those Who Continue to Smoke: Is Achieving Abstinence Harder and Do We Need to Change our Interventions? Bethesda: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 2003. Changes in measures of nicotine dependence using cross-sectional and longitudinal data from COMMIT; pp. 61–70. [Google Scholar]
- Irvin JE, Hendricks PS, Brandon TH. The increasing recalcitrance of smokers in clinical trials II: pharmacotherapy trials. Nicotine Tob. Res. 2003;5:27–35. doi: 10.1080/1462220031000070534. [DOI] [PubMed] [Google Scholar]
- Jarvis MJ, Giovino GA, O'Connor RJ, Kozlowski LT, Bernert JT. Variation in nicotine intake in U.S. cigarette smokers over the past 25 years: evidence from NHANES surveys. Nicotine Tob. Res. In Press doi: 10.1093/ntr/ntu120. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Schultz L. Forward telescoping bias in reported age of onset: an example from cigarette smoking. Int. J. Methods Psychiatr. Res. 2005;14:119–129. doi: 10.1002/mpr.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand ST, Manderscheid RW, Walter EE, Zaslavski AM. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk RE. Practical significance: a concept whose time has come. Educ. Psychol. Meas. 1996;56:746–759. [Google Scholar]
- Lê Cook B, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA. 2014;311:172–182. doi: 10.1001/jama.2013.284985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightwood JM, Glantz SA. Short-term economic and health benefits of smoking cessation myocardial infarction and stroke. Circulation. 1997;96:1089–1096. doi: 10.1161/01.cir.96.4.1089. [DOI] [PubMed] [Google Scholar]
- Liu LC, Hedeker D, Mermelstein RJ. Modeling nicotine dependence: an application of a longitudinal IRT model for the analysis of adolescent nicotine dependence syndrome scale. Nicotine Tob. Res. 2013;15:326–333. doi: 10.1093/ntr/nts125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Maciejewski PK, Falba T, Mazure CM. Sex differences in the effects of stressful life events on changes in smoking status. Addiction. 2003;98:847–855. doi: 10.1046/j.1360-0443.2003.00408.x. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Smoking and Tobacco Control Monograph No 15. Bethesda: U.S. Department of Health and Human Services, Public Health, National Institutes of Health Service, National Cancer Institute; 2003. Those Who Continue To Smoke: Is Achieving Abstinence Harder And Do We Need To Change Our Interventions? [Google Scholar]
- O'Connor RJ, Giovino GA, Kozlowski LT, Shiffman S, Hyland A, Bernert JT, Caraballo RS, Cummings KM. Changes in nicotine intake and cigarette use over time in two nationally representative cross-sectional samples of smokers. Am. J. Epidemiol. 2006;164:750–759. doi: 10.1093/aje/kwj263. [DOI] [PubMed] [Google Scholar]
- Perkins KA, Giedgowd GE, Karelitz JL, Conklin CA, Lerman C. Smoking in response to negative mood in men versus women as a function of distress tolerance. Nicotine Tob. Res. 2012;14:1418–1425. doi: 10.1093/ntr/nts075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA, Karelitz JL, Giedgowd GE, Conklin CA. Negative mood effects on craving to smoke in women versus men. Addict. Behav. 2013;38:1527–1531. doi: 10.1016/j.addbeh.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose JS, Dierker LC, Hedeker D, Mermelstein R. An integrated data analysis approach to investigating measurement equivalence of DSM nicotine dependence symptoms. Drug Alcohol Depend. 2013;129:25–32. doi: 10.1016/j.drugalcdep.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saladin ME, Gray KM, Carpenter MJ, LaRowe SD, DeSantis SM, Upadhyaya HP. Gender differences in craving and cue reactivity to smoking and negative affect/stress cues. Am. J. Addict. 2012;21:210–220. doi: 10.1111/j.1521-0391.2012.00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. Methodology Reports. 2013 http://www.samhsa.gov/data/Methodological_Reports.aspx.accessed on October 31 2013>.
- SAMHSA. Results from the 2011 National Survey on Drug Use and Health: Summary of national findings. Rockville, MD: NSDUH Series H-44; 2012. [Google Scholar]
- Shiffman S, Waters AJ, Hickcox M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 2004;6:327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Siahpush M, Borland R, Scollo M. Smoking and financial stress. Tob. Control. 2003;12:60–66. doi: 10.1136/tc.12.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M, Carlin JB. Financial stress, smoking cessation and relapse: results from a prospective study of an Australian national sample. Addiction. 2006;101:121–127. doi: 10.1111/j.1360-0443.2005.01292.x. [DOI] [PubMed] [Google Scholar]
- Sledjeski EM, Dierker LC, Costello D, Shiffman S, Donny E, Flay BR. Predictive validity of four nicotine dependence measures in a college sample. Drug Alcohol Depend. 2007;87:10–19. doi: 10.1016/j.drugalcdep.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Sterling KL, Mermelstein R, Turner L, Diviak K, Flay B, Shiffman S. Examining the psychometric properties and predictive validity of a youth-specific version of the Nicotine Dependence Syndrome Scale (NDSS) among teens with varying levels of smoking. Addict. Behav. 2009;34:616–619. doi: 10.1016/j.addbeh.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauras JA. Smoke-free air laws, cigarette prices, and adult cigarette demand. Econ. Inq. 2006;44:333–342. [Google Scholar]
- Warner KE, Burns DM. Hardening and the hard-core smoker: concepts, evidence, and implications. Nicotine Tob. Res. 2003;5:37–48. doi: 10.1080/1462220021000060428. [DOI] [PubMed] [Google Scholar]
- Weinberger AH, McKee SA. Gender differences in smoking following an implicit mood induction. Nicotine Tob. Res. 2012;14:621–625. doi: 10.1093/ntr/ntr198. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.