Abstract
The goal of this paper is to synthesize available data to help guide policy and programmatic initiatives for families with substance abuse problems that are involved with the child welfare system, and identify gaps in the research base needed to further refine practices in this area. To date, Family Treatment Drug Court and newly developed home-based substance abuse treatment interventions appear the most effective at improving substance abuse treatment initiation and completion in child welfare populations. Research is needed to compare the efficacy of these two approaches, and examine cost and child well-being indicators in addition to substance abuse treatment and child welfare outcomes.
Keywords: Substance Abuse, Child Welfare, Treatment
INTRODUCTION
Over the past decade, there has been growing interest in the problem of substance abuse within the child welfare system. It is estimated that 60% – 70% of all substantiated child welfare cases, and 80% or more of parents whose children are placed in foster care, have substance use disorders (SUDs) (Osterling & Austin, 2008; Young, Boles, & Otero, 2007). Among child welfare cases, parental substance abuse is associated with higher rates of child re-victimization (Brook & McDonald, 2009; Ondersma, 2007), greater likelihood of out-of-home placement (DHHS, 1997; Smith, Johnson, Pears, Fisher, & DeGarmo, 2007), longer stays in care (Connell, Bergeron, Katz, Saunders, & Tebes, 2007; Vanderploeg, et al., 2007), and higher rates of termination of parental rights and child adoption (Connell, et al., 2007).
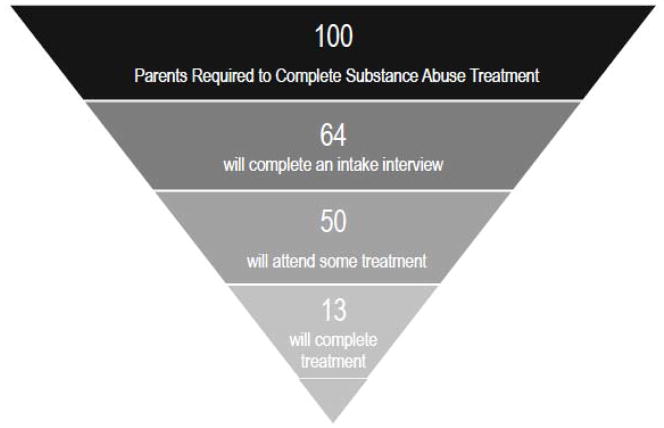
As depicted in Figure 1, there are many drop-off points for parents involved with the child welfare system in their attempts to access and finish substance abuse treatment (GAO, 1998). In 1998, the US General Accounting Office prepared a report for the US Senate Committee on Finance about the challenges facing foster care agencies serving children whose parents have SUDs. The report estimated that for each 100 parents required to receive substance abuse treatment as part of their service plan, 64% complete an intake for services, 50% attend some treatment, and only 13% complete treatment.
Figure 1. Drop-off Points for Parents involved in Child Welfare Accessing Substance Abuse Services.
There are many drop-off points in accessing substance abuse services for parents involved in child welfare. The data depicted above were generated from a report written by the US General Accounting Office (GAO) for the US Senate, Committee on Finance. In the survey conducted by the GAO, approximately 80% of parents of foster care children were required as part of their case plan to undergo substance abuse treatment. For each 100 parents required to receive treatment, 64% completed an intake, 50% participated in some treatment, and only 13% completed treatment.
Numerous demonstration projects have been initiated to improve treatment completion rates with foci at each stage depicted in the pyramid. The goal of this paper is to synthesize available data. To assure all available research was included in this review, computer-aided searches were conducted using PubMed and PsychInfo databases with the key words ‘child welfare’ or ‘child protection services’ crossed with the key words ‘substance abuse,’ ‘substance use disorders,’ and ‘addiction.’ References of prior review papers were also screened, and recipients of federally funded demonstration programs were contacted to obtain non-published data reporting the results of project evaluations. The review is limited to studies which included parents with substance use disorders who were involved with the child welfare system, and reported the effects of system or clinical interventions on one or more of the following substance abuse treatment outcomes: intake/assessment completion, treatment initiation, treatment completion, treatment success (e.g., sobriety); and/or one or more of the following child welfare outcomes: family reunification, child placement duration, and/or child re-victimization. Given the paucity of research in this area, when randomized controlled trials of a given intervention had not been conducted, results of studies utilizing non-random controls or presenting data from open treatment trials are reviewed as well.
Cross-System Collaboration
Project SAFE (Substance Abuse Family Evaluation) was initiated to facilitate cross-system and interagency collaboration (Young & Gardner, 2002). Project SAFE involved: 1) establishing collaborative relationship between child protection and adult mental health and addiction service systems; 2) implementing use of screening tool for protective service workers to determine if clients needed specialty substance abuse evaluation; 3) hiring a substance abuse specialist for each of regional child protection services offices to consult with workers; and 4) contracting with state-wide behavioral health consortium to provide drug testing, substance abuse assessments, and outpatient treatment - with these contracted services available to augment publicly funded substance abuse assessment and treatment resources.
Over five years, 5,776 parents were referred for substance abuse evaluations, and intakes were completed on 88% of those referred for specialty substance assessments. This represents a notable improvement over rate of intake completion previously reported in the literature (see Figure 1). Gains, however, were more modest in other tiers of the pyramid. Of clients referred for services, 41% attended some treatment, and only 19% of clients with SUDs referred for services, completed treatment.
Motivational Interviewing Approaches
Motivational interviewing (MI) is a collaborative, person-centered form of counseling that elicits and strengthens motivation for change which is widely used and supported in the substance abuse field (Miller & Rollnick, 2009). More than 200 clinical trials of MI have been published, and reviews and meta-analyses suggest MI is effective in non-child welfare populations in treating problem drinking, illicit drug use, concomitant mental and substance use disorders, and a range of other problematic behaviors and physical health problems. MI is a brief intervention, with most clinical trials being one to two sessions in length.
The efficacy of MI has been tested in two randomized studies with child welfare clients (Carroll, Libby, Sheehan, & Hyland, 2001; Mullins, Suarez, Ondersma, & Page, 2004). In the first study (Carroll, et al., 2001), 60 predominantly alcohol abusing clients were randomized to either standard intake or MI enhanced intake. Clients who received single session MI enhanced evaluation were significantly more likely to attend their first treatment session (59% vs. 29%). Treatment attendance fell off for both groups, and while proportion of clients to attend three or more sessions was greater for MI enhanced intake group (30% vs. 17%), the difference was not statistically significant, and rates of treatment completion were not reported.
The second study examining effectiveness of MI was conducted with clients referred to protective services due to prenatal drug use (Mullins, et al., 2004). It utilized a three session MI protocol, with one session completed at intake, one a week following, and the last one two months after intake. An educational video was used as a control condition. Seventy-one clients were randomized to the two conditions and there were no statistical differences between the two groups on subsequent substance abuse treatment attendance or urine tests of drug use. On average, clients in both groups attended approximately half the 16 treatment sessions, and had negative urine toxicology screens about half the time. Non-traditional alternative adjunctive treatments may be necessary to demonstrate a benefit of MI with child welfare populations.
Engaging Moms Program
The Engaging Moms (EM) Program was initially developed for mothers of cocaine-exposed infants involved with child welfare (Dakof, et al., 2003). EM is a manualized home-based 12-week intervention designed to promote maternal enrollment and retention in substance abuse services (Dakof, et al., 2003). EM interventions are guided by principals derived from Multidimensional Family Therapy and incorporate approaches focused at the individual and family level. EM specialists address barriers to treatment (e.g., transportation, child care), and therapeutic contacts focus on: 1) validating mother’s feelings about delivering a substance-exposed baby; 2) highlighting losses and missed opportunities as well as competencies and strengths; 3) helping mother understand her life situation as consequence of her difficult life circumstances; 4) instilling hope; and 5) strengthening bonds between mother and her family, natural supports, and children. EM specialists have bachelors or higher educational degrees, several years experience working in substance abuse field, and carry low caseloads of 8 clients each.
In an initial trial of EM program efficacy (Dakof, et al., 2003), a sample of 103 mothers of substance-exposed infants active with protective services were randomly assigned to EM or treatment as usual (TAU). Women in TAU received: 1) in-home psychosocial evaluation; 2) referral to a drug treatment program, 3) follow-up phone call within a day of the scheduled initial treatment appointment; and 4) whatever enrollment and retention interventions were provided by the drug treatment program they were attending. .EM services were initiated in two phases: 8 weeks focusing on treatment engagement, and 4 weeks focusing on treatment retention. Significantly more women assigned to EM Program completed a drug treatment program intake (88% vs. 46%) and received at least 4 weeks of services (67% vs. 38%). There were no differences between groups in terms of rates of treatment completion, however, with slightly over one-third of women in both conditions completing 90 days of treatment.
Recovery Coaches
The Illinois Title IVE Alcohol and Other Drug Abuse Waiver Demonstration Project tested efficacy of recovery coaches in improving the outcomes of families with substance abuse problems who are involved in the child welfare system (Choi & Ryan, 2006; Ryan, Choi, Hong, Hernandez, & Larrison, 2008; Smith, 2009). Recovery coaches: 1) provide ongoing outreach and engagement (e.g., transportation to initial intake appointment); 2) assist in removing any barriers to treatment; 3) provide ongoing assessments and make linkages for mental health, parenting, housing, domestic violence and family support services; 4) coordinate alcohol and other drug use service planning efforts, arrange case conferences, participate in family meetings, and testify in court; 5) conduct urinalysis testing; and 6) provide standardized, regular (monthly) reporting to workers and the courts. Each recovery coach is responsible for 20–25 clients. Recovery Coach intervention is similar to EM program in goal and use of outreach and engagement strategies, but the EM program has significantly lower worker-client caseloads (e.g., 8 vs. 20–25), is more likely to implement family interventions, and less likely to directly monitor drug use through urinalysis.
Families were eligible for the Recovery Coach waiver demonstration project if they satisfied the following conditions: 1) child entered foster care between April 2000 and June 2004; 2) parent assessed in court building by Juvenile Court Assessment Program within 90 days of temporary custody hearing; and 3) parent met diagnostic criteria for a SUD. Substance abusing caregivers were randomly assigned to either TAU or TAU plus intensive case management in the form of a recovery coach.
A total of 931 parents participated in the study: 670 received TAU plus a recovery coach, and 261 received TAU. Follow-up data derived from protective service and Juvenile Court Assessment Program records were collected through December 31, 2005. Length of follow-up for study participants ranged from 1.5 to 5.5 years. Parents assigned recovery coach were more likely to engage in treatment (71% vs. 52%), and engaged in treatment significantly faster than parents assigned TAU. Recovery coach services were also associated with significantly fewer subsequent SEI births (15% vs. 21%), and fewer new allegations of abuse (25% vs. 31%), although family reunification rates were low for both groups (18% vs. 13%). Treatment completion data was only reported for demonstration group (Choi & Ryan, 2006) - 22% of the parents completed substance abuse treatment.
Parents who participated in this project were representative of a typical child welfare sample and had high rates of co-occurring problems that compromised treatment efficacy, including housing problems, histories of domestic violence, and co-occurring mental health problems. Substance abuse was the only presenting problem for only 8% of the cohort, while 30% of the parents had SUD plus one other problem, 35% had two additional problems, and 27% had three additional problems. The addition of any co-occurring problem was associated with a 50% lower likelihood of achieving family reunification.
This demonstration project only included parents who completed an initial substance abuse assessment and were found to meet criteria for a SUD. It improved case outcomes at next tier of the pyramid, with number of parents attending their first session of treatment increasing from approximately 50% to over 70%. Unfortunately, improvement in number of parents completing treatment was modest, and rates of re-victimization over the extended follow-up period were high for both groups, albeit lower for the demonstration group (25% vs. 31%).
Family Treatment Drug Courts
The first Family Treatment Drug Court (FTDC) was established in Reno Nevada in 1994 (CEBC, 2008). The target population was parents whose children were placed in protective services custody due to abuse or neglect related to substance abuse. As of 2009, there were 272 FTDCs nationwide, with approximately 20% of these established in 2008 (BJA, 2009). To date, there have been three large-scale studies published examining efficacy of FTDCs on child and parent outcomes (Boles, Young, Moore, & DiPirro-Beard, 2007; Green, Furrer, Worcel, Burrus, & Finigan, 2007; Worcel, Furrer, Green, Burrus, & Finigan, 2008).
Characteristics of FTDCs vary somewhat from court to court. In general, they include: 1) substance abuse evaluation services available within the courthouse and frequently completed immediately following the initial dependency hearing; 2) regular, often weekly, court hearings to monitor parents’ treatment compliance; 3) provision of substance abuse treatment and adjunctive wrap around services, often in the form of recovery coaches and other individualized services; 4) frequent drug testing; and 5) rewards, sanctions, and intensity of judicial surveillance linked to service compliance (Boles, et al., 2007). Controls included in prior published FTDC efficacy studies were historical controls -- parents who were seen in dependency court prior to initiation of FTDC program (Boles, et al., 2007; Green, Rockhill, & Furrer, 2007), overflow cases --parents referred to FTDC but who were unable to receive services because program was at capacity (Green, Rockhill, et al., 2007), or propensity matched controls (Worcel, et al., 2008).
FTDCs are associated with faster and greater rates of substance abuse treatment initiation (Green, Furrer, et al., 2007; Worcel, et al., 2008), longer duration of treatment (Green, Furrer, et al., 2007; Worcel, et al., 2008), and in two of the three studies, greater likelihood of treatment completion (Boles, et al., 2007; Green, Furrer, et al., 2007; Worcel, et al., 2008). FTDCs have also been associated consistently with fewer days in out-of-home placement for children (Boles, et al., 2007; Worcel, et al., 2008), and higher rates of family reunification (Boles, et al., 2007; Green, Furrer, et al., 2007; Worcel, et al., 2008). Rates of treatment entry are between 80%–90% for FTDC cases, as compared to 55%–60% for controls. Also, while only about one-third of controls complete treatment, treatment completion rates are approximately two-thirds among FTDC cases. In one study, days in out-of-home care decreased significantly from 495 to 403 (Worcel, et al., 2008), and in the second study that reported this outcome, days in out of home care decreased significantly from 993 to 642 (Boles, et al., 2007). Across the three studies, rates of reunification range from 42% to 69% for FTDC cases, and 27% to 44% for control cases, with reunification approximately twice as likely if parents completed at least one treatment cycle (Green, Rockhill, et al., 2007). FTDC case outcomes are strongly linked with treatment compliance (Green, Furrer, et al., 2007). FTDC parents who complete treatment quickly have almost a 90% chance of reunification, and are approximately nine times more likely to have their children returned than FTDC cases that are noncompliant. In contrast, likelihood of reunification is predicted less strongly by treatment indicators with comparison cases.
While FTDC is associated with much greater entry and treatment completion rates than TAU or recovery coach interventions used independently from drug courts, no consistent benefit of FTDC has been demonstrated with regard to re-entry into care or new substantiated reports of maltreatment. Boles and colleagues (2007) reported non-significant differences between FTDC cases and controls on rates of re-entry into care, with 23% (83/362) of FTDC cases, and 11% (5/47) of controls re-entering care within 24 months of family reunification. Green and colleagues (2007) reported a similar pattern of findings, with rates of new substantiated reports of abuse (FTDC: 23% vs. Control: 14%, ns).
In one jurisdiction, to enhance FTDC case outcomes, a small-scale (N=62) randomized trial was conducted comparing FTDC with standard intensive case management/recovery coach services to FTDC with Engaging Moms (EM) Program specialists (Dakof, et al., 2010). As discussed previously, EM is a 12-week program designed to promote maternal enrollment in substance abuse services and enhance retention using principals derived from Multidimensional Family Therapy. The two approaches are very similar, except EM specialists have lower caseloads and do more therapeutic services with immediate and extended family (Dakof, Cohen, & Duarte, 2009; Dakof, et al., 2003). Outcomes of both groups were similar on measures of substance use, mental health, parenting practices, and family functioning. EM cases, however, were significantly more likely to have positive permanency outcomes, as defined as reunification with sole custody or joint custody, or permanent guardianship with family members without termination of the mother’s parental rights (FTDC+EM: 77% vs. FTDC+ICM: 55%). This preliminary study suggests the importance of working with extended family and natural supports to optimize permanency outcomes for children.
Home-Based Substance Abuse Interventions
Traditional substance abuse services are hospital- or office-based. Recently, Swenson, Henggler and colleagues (Swenson, et al., 2009) reported initial data on an alternative integrated treatment model of substance abuse services for parents with children six and older who are involved with protective services– the Building Stronger Families (BSF) program. BSF integrates Multisystemic Therapy (MST) and Reinforcement based treatment (RBT) for adult substance abuse to provide home-based drug and alcohol treatment. MST is an empirically validated home- and community-based treatment for families of school-aged children with multiple complex treatment needs, and RBT is an empirically validated incentive-based treatment for adults with addictive disorders.
As many parents involved with child welfare meet criteria for Posttraumatic Stress Disorder (PTSD), BSF clinicians are also trained in evidence-based PTSD treatments (Swenson, et al., 2009). This is important, as individuals participating in substance abuse treatment studies that have co-occurring PTSD have greater impairment at baseline, post-treatment, and at follow-up (Najavits, et al., 2007). While there has been concern in the field that trauma-focused interventions would promote adverse consequences in substance abusing populations (e.g., symptom exacerbation), implementing PTSD treatment in substance abuse treatment programs has been found to lead to greater reduction in substance use and clinical symptomatology (Hien, et al., 2009), and there is no evidence that it promotes adverse consequences (Killeen, et al., 2008).
BSF clinicians provide substance abuse, mental health, parenting, case management, and other services as needed, with 24/7 on-call services available to address crises that emerge after hours. Given intervention intensity, BSF clinicians carry only four to six cases at a time with treatment lasting about six months. The goals of BSF are to eliminate parental substance misuse, address factors associated with child maltreatment, and keep children living with their families (parents or relatives) whenever possible. Family safety plans are developed with protective service workers and BSF clinician, ideally with collaboration from members of the family’s natural ecology. Breathalyzer and urine drug testing is conducted randomly in home a minimum of three times per week for the duration of treatment. Within BSF, there is an understanding that relapse is a part of recovery process. Decisions to remove children from their parents’ homes are not based on results of any particular drug test, but on parent adherence to safety plans and willingness to engage in substance abuse treatment. In a study of treatment feasibility with 54 families, 87% of the parents referred for BSF treatment initiated services, 93% of those who began treatment services completed the BSF program, and 75% of the parents retained custody of their children throughout the duration of treatment. Overall, 86% of cases were discharged successfully with sustained sobriety, stable mental health, safe and secure housing, and placement permanency for children (Swenson, et al., 2009).
Family Based Recovery (FBR) is a second home-based integrated substance abuse and family support treatment model that was developed for parents of infants and young children (Vanderploeg, et al., 2009). It is similar to BSF in that it integrates reinforcement-based treatment for adult substance abuse, frequent in-home urine toxicology testing, and family-based treatment strategies. Given the young age of the children, it also incorporates attachment-based parent-child psychotherapy approaches (Lieberman, 2005). To date, data are available for the first 158 parents served by FBR. The clients served had multiple co-occurring problems: 45% had psychiatric diagnoses; 46% experienced domestic violence; 27% had childhood histories of sexual abuse; 35% had past criminal convictions; and 65% had children who had positive toxicology tests at birth. Utilizing family safety plans developed with protective service workers, FBR team, and members of family’s natural ecology, 64% of the infants and young children remained safely at home throughout the intervention.
Summary
A number of policies and practices have been implemented to enhance the delivery of substance abuse services for parents involved with the child welfare system. Establishment of cross system collaborations and stationing a substance abuse specialist in child welfare offices appears a successful strategy for increasing intake rates, but not treatment engagement or completion. Motivational interviewing (MI), a highly effective approach for enhancing treatment initiation and completion in general substance abusing populations, improved treatment entry, but failed to be associated with enhanced treatment completion rates within child welfare samples when combined with traditional treatment approaches. Outreach and engagement strategies like those used by the Engaging Moms Program and Recovery Coach interventions likewise have been found to improve substance abuse treatment initiation in child welfare populations. When implemented independently these programs do not optimize treatment completion rates, but are very effective at improving substance abuse treatment completion rates when combined with Family Treatment Drug Courts (FTDC).
To date, FTDC and newly developed home-based substance abuse treatment interventions appear to be the most effective at improving outcomes at each level of the pyramid depicted in Figure 1. The high rates of re-entry into care after reunification reported among FTDC cases, however, highlights the need for more work in this area.
Additional research on the short- and long-term efficacy of the home-based substance abuse treatment models is clearly warranted. A key feature of the home-based programs is the delivery of empirically validated substance abuse treatment and monitoring of client progress through tri-weekly toxicology screens in the home – not referring out for these services. Another key feature is that clinicians and protective service workers develop safety plans with family members and extended supports in the parents network allowing children to be maintained at home in the majority of cases while the parent engages in substance abuse treatment. Given the many poverty-related concrete barriers to accessing substance abuse services that exist for parents involved with child welfare (e.g., no phone, limited cell phone minutes, no car, no child care), bringing state-of-the-art substance abuse services to parents where they live appears a very promising strategy for optimizing substance abuse treatment outcomes for parents, and minimizing the separation and traumatic loss experiences of children.
Future Directions and Conclusions
Significant advances have been made in the past decade. Research is needed to compare the efficacy of FTDC and the newer integrated home-based substance abuse treatment models. Outcome research to date has only focused on substance abuse treatment and child welfare outcomes. In the future it will be important to also examine cost and child well-being indicators. Through rigorous evaluation, the system of care for families involved with child welfare can be further improved.
Acknowledgments
This work was supported by the National Center for PTSD, VA CT. The authors thank Dr. Johari Massey for her research support, and also wish to thank the children and families they have worked with for the unique clinical insights they have provided regarding the needs of this population.
References
- BJA. Drug Court Clearinghouse Project at American University: Summary ofJuvenile/Family Drug Court Activity by State and County. Washington, D.C: Bureau of Justice; 2009. [Google Scholar]
- Boles S, Young N, Moore T, DiPirro-Beard S. The Sacramento Dependency Drug Court: development and outcomes. Child Maltreat. 2007;12(2):161–171. doi: 10.1177/1077559507300643. [DOI] [PubMed] [Google Scholar]
- Brook J, McDonald T. The impact of parental substance abuse on the stability of family reunifications from foster care. Children and Youth Services Review. 2009;31(2):193–198. [Google Scholar]
- Carroll K, Libby B, Sheehan J, Hyland N. Motivational interviewing to enhance treatment initiation in substance abusers: an effectiveness study. Am J Addict. 2001;10(4):335–339. doi: 10.1080/aja.10.4.335.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CEBC. Reno Family Drug Court - Summary. Califorinia Evidence-Based Clearinghouse for Child Welfare. 2008 from http://www.cachildwelfareclearinghouse.org/program/30#contact.
- Choi S, Ryan J. Completing substance abuse treatment in child welfare: the role of co-occurring problems and primary drug of choice. Child Maltreat. 2006;11(4):313–325. doi: 10.1177/1077559506292607. [DOI] [PubMed] [Google Scholar]
- Connell C, Bergeron N, Katz K, Saunders L, Tebes J. Re-referral to child protective services: the influence of child, family, and case characteristics on risk status. Child Abuse Negl. 2007;31(5):573–588. doi: 10.1016/j.chiabu.2006.12.004. [DOI] [PubMed] [Google Scholar]
- Dakof G, Cohen J, Duarte E. Increasing family reunification for substance abusing mothers and their children: Comparing two drug court interventions. Juvenile and Family Court Journal. 2009;60:11–23. [Google Scholar]
- Dakof G, Cohen J, Henderson C, Duarte E, Boustani M, Blackburn A, et al. A randomized pilot study of the Engaging Moms Program for family drug court. J Subst Abuse Treat. 2010;38(3):263–274. doi: 10.1016/j.jsat.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakof G, Quille T, Tejeda M, Alberga L, Bandstra E, Szapocznik J. Enrolling and Retaining Mothers of Substance-Exposed Infants in Drug Abuse Treatment. Journal of Consulting & Clinical Psychology. 2003;71(4):764–772. doi: 10.1037/0022-006x.71.4.764. [DOI] [PubMed] [Google Scholar]
- DHHS. National study of protective, preventive, and reunification services delivered to children and their families. Washington, D.C: U.S. Department of Health and Human Services; 1997. [Google Scholar]
- GAO. Foster care: Agencies face challenges securing stable homes for children of substance abusers. Washington, D.C: U.S. General Accounting Office; 1998. [Google Scholar]
- Green B, Furrer C, Worcel S, Burrus S, Finigan M. How effective are family treatment drug courts? Outcomes from a four-site national study. Child Maltreat. 2007;12(1):43–59. doi: 10.1177/1077559506296317. [DOI] [PubMed] [Google Scholar]
- Green B, Rockhill A, Furrer C. Does substance abuse treatment make a difference for child welfare case outcomes? A statewide longitudinal analysis. Children and Youth Services Review. 2007;29:460–463. [Google Scholar]
- Hien D, Wells E, Jiang H, Suarez-Morales L, Campbell A, Cohen L, et al. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. J Consult Clin Psychol. 2009;77(4):607–619. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killeen T, Hien D, Campbell A, Brown C, Hansen C, Jiang H, et al. Adverse events in an integrated trauma-focused intervention for women in community substance abuse treatment. J Subst Abuse Treat. 2008;35(3):304–311. doi: 10.1016/j.jsat.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman A, Van Horn P. “Don't hit my mommy!”: A Manual for Child-Parent Psychotherapy with Young Witnesses of Family Violence. Washington, DC: Zero to Three Press; 2005. [Google Scholar]
- Miller W, Rollnick S. Ten things that motivational interviewing is not. Behav Cogn Psychother. 2009;37(2):129–140. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- Miller W, Rose G. Toward a theory of motivational interviewing. Am Psychol. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullins S, Suarez M, Ondersma S, Page M. The impact of motivational interviewing on substance abuse treatment retention: a randomized control trial of women involved with child welfare. J Subst Abuse Treat. 2004;27(1):51–58. doi: 10.1016/j.jsat.2004.03.010. [DOI] [PubMed] [Google Scholar]
- Najavits L, Harned M, Gallop R, Butler S, Barber J, Thase M, et al. Six-month treatment outcomes of cocaine-dependent patients with and without PTSD in a multisite national trial. J Stud Alcohol Drugs. 2007;68(3):353–361. doi: 10.15288/jsad.2007.68.353. [DOI] [PubMed] [Google Scholar]
- NCSACW. National Center on Substance Abuse and Child Welfare. from http://www.ncsacw.samhsa.gov.
- Ondersma S. Introduction to the First of Two Special Sections on Substance Abuse and Child Maltreatment. Child Maltreat. 2007;12:3–6. [Google Scholar]
- Osterling K, Austin M. Substance abuse interventions for parents involved in the child welfare system: evidence and implications. J Evid Based Soc Work. 2008;5(1–2):157–189. doi: 10.1300/J394v05n01_07. [DOI] [PubMed] [Google Scholar]
- Ryan J, Choi S, Hong J, Hernandez P, Larrison C. Recovery coaches and substance exposed births: an experiment in child welfare. Child Abuse Negl. 2008;32(11):1072–1079. doi: 10.1016/j.chiabu.2007.12.011. [DOI] [PubMed] [Google Scholar]
- Smith D, Johnson A, Pears KC, Fisher P, DeGarmo D. Child maltreatment and foster care: unpacking the effects of prenatal and\ postnatal parental substance use. Child Maltreat. 2007;12(2):150–160. doi: 10.1177/1077559507300129. [DOI] [PubMed] [Google Scholar]
- Smith M. Illinois DCFS IV-E AODA Waiver: The Recovery Coach Project. Paper presented at the Southern Illinois Methamphetamine and other Drugs Awareness Conference.2009. [Google Scholar]
- Swenson C, Schaeffer C, Tuerk E, Henggeler S, Tuten M, Panzarella P, et al. Adapting Multisystemic Therapy for Co-Occurring Child Maltreatment and Parental Substance Abuse: The Building Stronger Families Project. Emotional & Behavioral Disorders in Youth. 2009:3–8. [Google Scholar]
- Vanderploeg J, Connell C, Caron C, Saunders L, Katz K, Tebes J. The impact of parental alcohol or drug removals on foster care placement experiences: a matched comparison group study. Child Maltreat. 2007;12(2):125–136. doi: 10.1177/1077559507299292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderploeg J, Connell C, Hanson K, Adnopoz J, Hawke J, Steinberg K, et al. Family-Based Recover Program: Quality Assurance Findings from a Statewide, Multi-Site Intervention for Children Affected by Parental Substance Abuse. Paper presented at the A System of Care for Children's Mental Health: Expanding the Research Base.2009. [Google Scholar]
- Worcel S, Furrer C, Green B, Burrus S, Finigan M. Effects of Family Treatment Drug Courts on Substance Abuse and Child Welfare Outcomes. Child Abuse Review. 2008;17:427–443. [Google Scholar]
- Young N, Boles S, Otero C. Parental substance use disorders and child maltreatment: overlap, gaps, and opportunities. Child Maltreat. 2007;12(2):137–149. doi: 10.1177/1077559507300322. [DOI] [PubMed] [Google Scholar]
- Young N, Gardner S. Navigating the Pathways: Lessons and Promising Practices in Linking Alcohol and Drug Services with Child Welfare. U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Center for Substance Abuse Treatment; 2002. [Google Scholar]