Abstract
Introduction:
The Subaxial Injury Classification (SLIC) system and severity score has been developed to help surgeons in the decision-making process of treatment of subaxial cervical spine injuries. A detailed description of all potential scored injures of the SLIC is lacking.
Materials and Methods:
We performed a systematic review in the PubMed database from 2007 to 2014 to describe the relationship between the scored injuries in the SLIC and their eventual treatment according to the system score.
Results:
Patients with an SLIC of 1-3 points (conservative treatment) are neurologically intact with the spinous process, laminar or small facet fractures. Patients with compression and burst fractures who are neurologically intact are also treated nonsurgically. Patients with an SLIC of 4 points may have an incomplete spinal cord injury such as a central cord syndrome, compression injuries with incomplete neurologic deficits and burst fractures with complete neurologic deficits. SLIC of 5-10 points includes distraction and rotational injuries, traumatic disc herniation in the setting of a neurological deficit and burst fractures with an incomplete neurologic deficit.
Conclusion:
The SLIC injury severity score can help surgeons guide fracture treatment. Knowledge of the potential scored injures and their relationships with the SLIC are of paramount importance for spine surgeons who treated subaxial cervical spine injuries.
Keywords: Cervical spine, fractures, Subaxial Injury Classification, spinal cord injury
INTRODUCTION
The management of subaxial cervical spine trauma (SCST) has been facilitated following the publication of the Subaxial Injury and Classification (SLIC) and severity scale by the Spine Trauma Study Group.[1] The SLIC system is a classification and injury severity score based on the importance of three factors related to the management of cervical injuries: Morphology, neurological status and the integrity of the disco-ligamentous complex (DLC).[1] These three parameters are evaluated in isolation [Table 1 – the SLIC system], quantifying spinal cord injuries according to their severity.
Table 1.
The SLIC system severity score
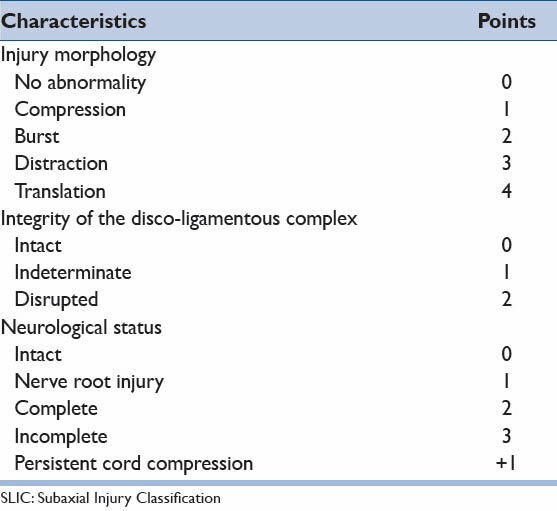
The SLIC classifies injuries as it follows:
Morphology: (0) no abnormality, (1) compression, (2) burst, (3) distraction, and (4) translation or rotation.
DLC (formed by the intervertebral disc, anterior and posterior longitudinal ligaments, interspinous ligaments, facet capsules, and ligamentum flavum): (0) intact, (1) indeterminate (isolated magnetic resonance imaging signal change or isolated widening of the spinous process) and (2) disrupted (widening of the disc, facet perch or locked).
Neurologic status: (0) intact, (1) root injury, (2) complete cord injury, (3) incomplete cord injury and (+1) continuous cord compression in the setting of neurological deficit.
The final summated score will suggest the potential treatment: 1-3 scored patients can be treated nonoperatively, patients with 4 points can be treated nonsurgically or surgically, according to surgeons’ preference and patients’ condition, and five or more points are referred to surgery, with the realignment, neurological decompression (if indicated), and stabilization.
Since its publication, many studies evaluating the SLIC system have been published.[2,3,4,5]. However, a detailed description of all potential scored injures of the SLIC is lacking. The purpose of this study is to describe the relationship between the scored injuries and their recommended treatment according to the SLIC system.
MATERIALS AND METHODS
A review of the literature using the Medline database (National Library of Medicine) was performed. The key-word “SLIC system” was used, from 2007 to 2014. Articles related to the system and the potential scored injures were selected according to the purpose of our review. The summation of points of the three components (fracture morphology, DLC and neurological status) of the SLIC system can total between 1 to a maximum of 10 points. These 10 possibilities were analyzed in isolation, dividing them into three groups according to the proposed treatment – patients with three or less points (conservative management), patients with five or more points (surgical management) and patients with four points (managed potentially of both ways).
Regarding morphology, patients with “no abnormality” (including isolated spinous process fractures, laminar fractures or small nondisplaced facet fractures) and “compression or burst fractures” without neurological deficits or any disco-ligamentous injury can be score with less than 4 points and managed conservatively. If there is a disruption of the disco-ligamentous complex (2 points) than a burst fracture without a neurological deficit will be scored with 4 points.
Patients with distraction (three points) and rotational injuries (four points) will also have a disrupted DLC, receiving two extra points, and will be surgically managed, regardless of the neurological status.
Patients with normal morphology and extruded traumatic disc herniation will receive two points for DLC injury in addition to the scoring of their spinal cord injury.
RESULTS
Results are categorized according to the suggested treatment based on the SLIC system total score and summarized in the sections: Nonsurgical treatment [1-3 points - Table 2], Surgical or nonsurgical treatment [4 points - Table 3], and Surgical treatment [5-10 points - Table 4]. Figure 1 illustrates a case example treated according to the SLIC system.
Table 2.
Classification of the injures with a SLIC score of 0-3 points
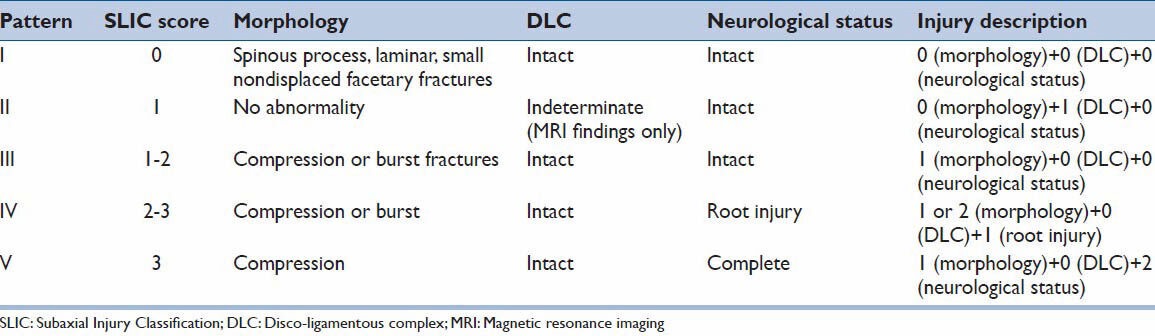
Table 3.
Classification of the injures with a SLIC score of 4 points
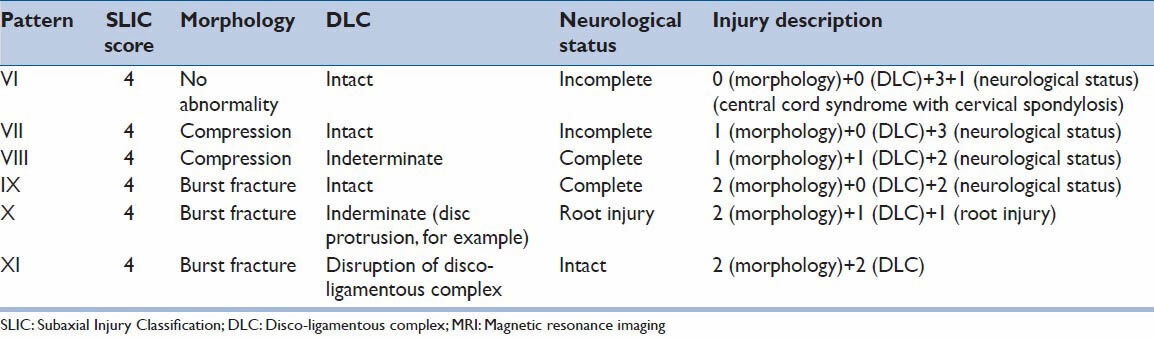
Table 4.
Classification of the injures with a SLIC score of 5 or more points
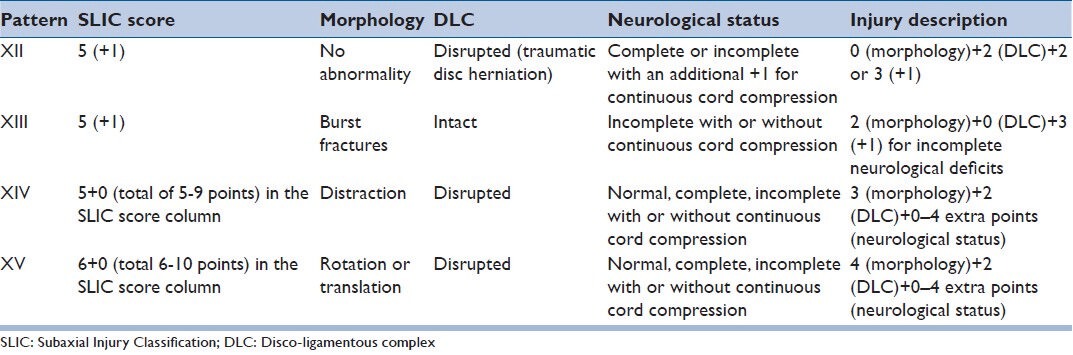
Figure 1.
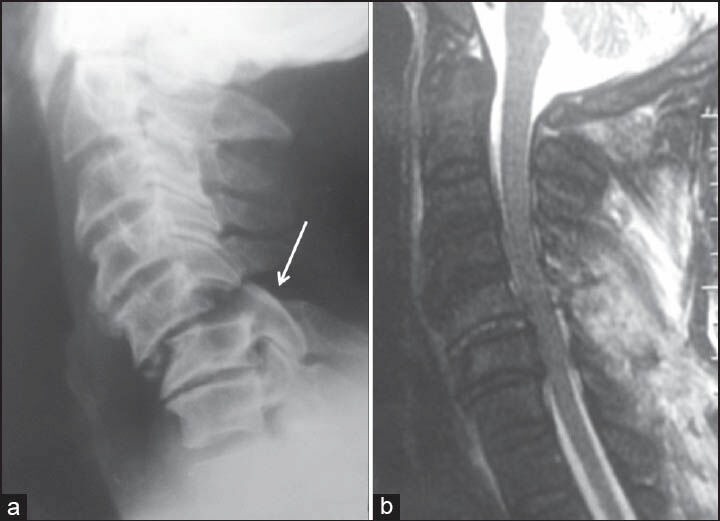
A 55-year-old man victim of fall from the height with normal neurological examination. (a) A distractive injury can be clearly seen at C5-C6 in a lateral X-ray with facet joints subluxation (bilateral perched facet joints). (b) A sagittal T2 sequence magnetic resonance imaging with hypersignal in the posterior cervical ligaments without signal changes in the spinal cord. The Subaxial Injury Classification score was: 3 points (distractive injury) + 2 points (disco-ligamentous complex injury) + 0 points (intact) = 5 points – surgical treatment was performed
Nonsurgical treatment – Subaxial Injury Classification 1-3 points [Table 2]
Most of the patients in this group are neurologically intact. Patients with isolated spinous process fractures, laminar fractures or small nondisplaced facet fractures are included in this group (I). Magnetic Resonance (MR) findings suggesting ligamentous injury may not be an indication for surgery (II) and also belong to nonsurgical treatment group. Patients with compression or burst fractures without neurological deficits can be score with less than 4 points if there is no disruption of the disco-ligamentous complex and also managed conservatively (III). Compression fractures are defined by loss of the height of the part or the entire vertebral body, as well as sagittal or coronal plane fractures and “tear-drop” injuries.[1,2] Sometimes, fractures of the posterior cervical elements can also be found, such as lamina or minimally displaced facet joints/lateral masses fractures.[1] Concomitant root injury in these cases does not preclude nonsurgical treatment according to the SLIC (IV). A rare clinical scenario of a compression fracture in a patient with a complete neurological deficits would result in a score of three points (V), being managed conservatively according to the system.[1,2]
Surgical or nonsurgical treatment – Subaxial Injury Classification 4 points [Table 3]
This borderline treatment group includes patients with central cord syndrome with cervical spondylotic compression without disc herniation (0 for morphology, 0 for DLC intact and 3 + 1 for neurological deficits with continuous compression) (VI). This group also includes a rare clinical scenario of compression fractures with intact DLC, incomplete neurological deficits or indeterminate DLC and complete neurological deficits (respectively, VII and VIII). Patients with burst fractures and complete deficits also are including, receiving 4 points (IX). The last two potential injury scores with 4 points is a patient with a burst fracture (2 points), indeterminate DLC injury (1 point) and root injury (1 point) (X) or a burst fracture, neuro intact with disrupted posterior ligamentous complex (XI).
Surgical treatment – Subaxial Injury Classification 5-10 points [Table 4]
This group may include patients with a traumatic disc herniation in the setting of a neurological deficit (XII). Burst fractures with incomplete deficits are also surgically treated, with a score of 5 or 6 points, the latter in cases of persistent cord compression (XIII). All the patients with distraction and rotational injures are included and referred for surgical treatment, regardless of the neurological status which can range for normal to incomplete deficits (XIV and XV). Distraction injures are characterized by anatomical dislocation in the vertical axis, whereas rotation injuries have horizontal displacement of one part with respect to the other.[1,2] Most of these patients will present with perched or locked unilateral or bilateral facet joints, unstable tear-drop fractures, and severe dislocations.
DISCUSSION
In a previous study of a retrospective case series of patients with subaxial cervical spine treated, high agreement rate in the SLIC score and the treatment chosen (nonsurgical or surgical) was demonstrated, with more than 90% of agreement between them.[3] There is also reported of excellent intra-observer and inter-observer agreement among surgeons with the SLIC score.[6] A prospective clinical study has demonstrated that the SLIC system was safe and effective in guide treatment regarding preservation of the neurological status in patients with SCST.[7] Due to the potential benefits of the score, accessing potential injuries scenarios, according to their score and potential treatment, is necessary to better understand the application of the SLIC system.
Nonsurgical group – Subaxial Injury Classification from 0 to 3 points
In this group are included patients with the spinous process (also known as Clay-Shoveler's fracture), laminar fractures, and small nondisplaced facet fractures. These fractures are stable, being treated with a cervical immobilization for comfort and pain reduction.[8,9] However, they can be viewed as a warning sign for more severe spinal injuries. Laminar fractures are also stable injuries in patients without neurologically deficits, but anecdotal cases of laminar fractures after direct trauma leading to neurological deficits are reported, with surgical treatment recommended if canal compression is present.[10]
Compression and burst fractures without neurological deficits can also be managed nonsurgically. Of note, some authors suggest radiological parameters associated with failure in conservative management of these injuries, such as more than 40% of height compression, kyphotic angulation higher than 15° or 20% of subluxation of one vertebra on another.[11,12] The SLIC did not address these risk factors, proposing conservative treatment for stable burst fractures without neurological deficits regardless of radiographic alignment.
Furthermore, in this group can be found compression or burst fractures with root injury. An attempt of conservative treatment can be accepted in such clinical scenarios. It should be note that in some burst fractures with severe radiculopathy involving motor and sensorial impairment, early surgery may be a better option, despite of the recommendation of conservative treatment in the SLIC score. The literature is, unfortunately, sparse regarding treatment of traumatic radiculopathy in the cervical spine.
Compression fractures with complete neurological deficits would receive 3 points. Although this is a rare clinical scenario, conservative treatment is proposed in such situation as neither mechanical instability nor continuing neurological compression exists.
Borderline injury severity score – Subaxial Injury Classification of 4 – conservative or surgical treatment
The SLIC system suggests that patients with 4 points can be treated surgically or nonsurgically. One common clinical scenario of patients with 4 points is central cord syndrome in the context of cervical spondylosis (VI). Although fractures and dislocation can be present, these patients generally present normal computed tomography scan and without evident mechanical instability but with severe neurological deficits. Central cord syndrome is the most frequently encountered incomplete spinal cord injury, and nearly half of these patients have concomitant congenital or degenerative spinal stenosis with injuries during hyperextension.[13] Although most of these patients will have spontaneous recovery, many authors advocated surgery for relief of continuous cord compression, although time for surgery in such cases remains controversy.[14,15] In some surgical series, surgery for decompression is associated with better neurological improvement, being recommended as the treatment of choice in these patients.
Patients with compression morphology and incomplete (VII) or complete (VIII) neurological deficits can also add 4 points. As there is neither instability nor compression of the spinal canal, surgical benefits are limited compared to nonsurgical treatment.
Two other potential injuries with an SLIC of 4 points also deserve discussion: Burst fractures with complete neurological deficit (IX) and burst fractures with root injury secondary to disk protrusion and indeterminate DLC status (X). Finally, a patient can present with a burst fracture and DLC injury without neurological deficits, also having 4 points (XI).
Although conservative treatment can be an option for burst with complete deficits, many surgical series recommend early treatment with aggressive canal decompression, improving neurological outcomes and also offering immediate stabilization, even in patients with complete deficits.[9,16,17,18]
Surgical group – Subaxial Injury Classification ≥5
In this group, most of the patients have severe dislocations, distractive or rotational injuries and clear unstable lesions. For these patients, the benefits of surgical stabilization are clear.
Surgery for traumatic disc herniation (XII) in the setting of neurological deficits is a well-accepted procedure. Dai and Jia reported their experience with 24 patients with acute traumatic disc herniation.[17] The patients underwent an anterior cervical discectomy and fusion for cord decompression and spinal stabilization with marked neurological improvement. Traumatic disc herniation is also commonly found in fractures and dislocations, deserving special attention once anecdotal cases of neurological deterioration after closed reduction have been reported.[19,20]
Burst fractures with incomplete deficits with or without continuous compression (XIII) are also injuries that may benefits of early surgery, with canal decompression and stabilization.[16,18,21]
Surgical treatment of facet fractures and dislocations, in the past, prior to the advent of modern spinal instrumentation, was based on closed reduction and external orthoses with prolonged bedrest and its inherent morbidity and mortality. Today, these injuries are better managed with internal fixation, with early stability and rehabilitation. Regarding the choice of anterior versus posterior approaches for unstable lesions (XIV and XV), anterior approaches are generally recommended in the setting of severe vertebral body fracture with anterior compression and posterior approaches considered in posterior injury (facet joints, lateral mass, lamina), potential kyphosis deformity and severe misalignment. Combined approaches can also be performed, especially in complex cases.[22,23] The location of cord compression, anterior and/or posterior, will also guide surgical approach.
In isolated facet joint injuries with displacement, conservative treatment with closed reduction and external immobilization is associated with a high rate of cervical misalignment.[24,25,26,27] As such, these injuries should be referred for surgery, especially in patients with neurological deficits, in unilateral or bilateral perched/locked facet joints. These injuries can be managed by either anterior or posterior approaches, with similar outcomes.[28,29]
CONCLUSION
The SLIC injured severity score can help surgeons to guide surgical treatment. Patients without neurological deficits and minor bone injuries (spinous process, facet, lamina) without severe displacement can be treated conservatively, with a SLIC of <3 points, as well as compression and burst fractures without neurological deficits. Patients with an SLIC 4 can treated either conservatively or surgically, even though some injuries with an SLIC 4 may be preferentially referred for early surgery, such as patients with incomplete deficits and cervical spondylosis and patients with burst fractures and complete neurological deficits. Patients with an SLIC of >5 points generally have rotational or distractive injuries (such as facet fractures-dislocations and floating lateral mass), and should be referred for surgery regardless of their neurological deficits. Lastly, asymptomatic traumatic disc herniation with neurological deficit should also be treated surgically.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA, Jr, et al. The subaxial cervical spine injury classification system: A novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007;32:2365–74. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]
- 2.Dvorak MF, Fisher CG, Fehlings MG, Rampersaud YR, Oner FC, Aarabi B, et al. The surgical approach to subaxial cervical spine injuries: An evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976) 2007;32:2620–9. doi: 10.1097/BRS.0b013e318158ce16. [DOI] [PubMed] [Google Scholar]
- 3.Joaquim AF, Lawrence B, Daubs M, Brodke D, Patel AA. Evaluation of the Subaxial Injury Classification system. J Craniovertebr Junction Spine. 2011;2:67–72. doi: 10.4103/0974-8237.100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel AA, Dailey A, Brodke DS, Daubs M, Anderson PA, Hurlbert RJ, et al. Subaxial cervical spine trauma classification: The Subaxial Injury Classification system and case examples. Neurosurg Focus. 2008;25:E8. doi: 10.3171/FOC.2008.25.11.E8. [DOI] [PubMed] [Google Scholar]
- 5.Patel AA, Hurlbert RJ, Bono CM, Bessey JT, Yang N, Vaccaro AR. Classification and surgical decision making in acute subaxial cervical spine trauma. Spine (Phila Pa 1976) 2010;35:S228–34. doi: 10.1097/BRS.0b013e3181f330ae. [DOI] [PubMed] [Google Scholar]
- 6.Stone AT, Bransford RJ, Lee MJ, Vilela MD, Bellabarba C, Anderson PA, et al. Reliability of classification systems for subaxial cervical injuries. Evid Based Spine Care J. 2010;1:19–26. doi: 10.1055/s-0030-1267064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joaquim AF, Ghizoni E, Tedeschi H, da Cruz HY, Patel AA. Clinical results of patients with subaxial cervical spine trauma treated according to the SLIC score. J Spinal Cord Med. 2013 doi: 10.1179/2045772313Y.0000000143. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dellestable F, Gaucher A. Clay-shoveler's fracture. Stress fracture of the lower cervical and upper thoracic spinous processes. Rev Rhum Engl Ed. 1998;65:575–82. [PubMed] [Google Scholar]
- 9.Hirsh LF, Duarte LE, Wolfson EH, Gerhard W. Isolated symptomatic cervical spinous process fracture requiring surgery. Case report. J Neurosurg. 1991;75:131–3. doi: 10.3171/jns.1991.75.1.0131. [DOI] [PubMed] [Google Scholar]
- 10.Makan P. Neurologic compromise after an isolated laminar fracture of the cervical spine. Spine (Phila Pa 1976) 1999;24:1144–6. doi: 10.1097/00007632-199906010-00015. [DOI] [PubMed] [Google Scholar]
- 11.Hadley MN, Walters BC, Grabb PA, Oyesiku NM, Przybylski GJ, Resnick DK, et al. Guidelines for the management of acute cervical spine and spinal cord injuries. Clin Neurosurg. 2002;49:407–98. [PubMed] [Google Scholar]
- 12.Lemons VR, Wagner FC., Jr Stabilization of subaxial cervical spinal injuries. Surg Neurol. 1993;39:511–8. doi: 10.1016/0090-3019(93)90038-3. [DOI] [PubMed] [Google Scholar]
- 13.Aarabi B, Koltz M, Ibrahimi D. Hyperextension cervical spine injuries and traumatic central cord syndrome. Neurosurg Focus. 2008;25:E9. doi: 10.3171/FOC.2008.25.11.E9. [DOI] [PubMed] [Google Scholar]
- 14.Waters RL, Adkins RH, Sie IH, Yakura JS. Motor recovery following spinal cord injury associated with cervical spondylosis: A collaborative study. Spinal Cord. 1996;34:711–5. doi: 10.1038/sc.1996.129. [DOI] [PubMed] [Google Scholar]
- 15.Wilkinson HA. Central cord syndrome. J Neurosurg. 2002;97:158–9. doi: 10.3171/spi.2002.97.1.0158a. [DOI] [PubMed] [Google Scholar]
- 16.Aebi M, Zuber K, Marchesi D. Treatment of cervical spine injuries with anterior plating. Indications, techniques, and results. Spine (Phila Pa 1976) 1991;16:S38–45. doi: 10.1097/00007632-199103001-00008. [DOI] [PubMed] [Google Scholar]
- 17.Dai L, Jia L. Central cord injury complicating acute cervical disc herniation in trauma. Spine (Phila Pa 1976) 2000;25:331–5. doi: 10.1097/00007632-200002010-00012. [DOI] [PubMed] [Google Scholar]
- 18.Goffin J, Plets C, Van den Bergh R. Anterior cervical fusion and osteosynthetic stabilization according to Caspar: A prospective study of 41 patients with fractures and/or dislocations of the cervical spine. Neurosurgery. 1989;25:865–71. [PubMed] [Google Scholar]
- 19.Farmer J, Vaccaro A, Albert TJ, Malone S, Balderston RA, Cotler JM. Neurologic deterioration after cervical spinal cord injury. J Spinal Disord. 1998;11:192–6. [PubMed] [Google Scholar]
- 20.Maiman DJ, Barolat G, Larson SJ. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1986;18:542–7. doi: 10.1227/00006123-198605000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Lambiris E, Zouboulis P, Tyllianakis M, Panagiotopoulos E. Anterior surgery for unstable lower cervical spine injuries. Clin Orthop Relat Res. 2003;411:61–9. doi: 10.1097/01.blo.0000068185.83581.cf. [DOI] [PubMed] [Google Scholar]
- 22.Cybulski GR, Douglas RA, Meyer PR, Jr, Rovin RA. Complications in three-column cervical spine injuries requiring anterior-posterior stabilization. Spine (Phila Pa 1976) 1992;17:253–6. doi: 10.1097/00007632-199203000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Johnson MG, Fisher CG, Boyd M, Pitzen T, Oxland TR, Dvorak MF. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine (Phila Pa 1976) 2004;29:2815–20. doi: 10.1097/01.brs.0000151088.80797.bd. [DOI] [PubMed] [Google Scholar]
- 24.Bucholz RD, Cheung KC. Halo vest versus spinal fusion for cervical injury: evidence from an outcome study. J Neurosurg. 1989;70:884–92. doi: 10.3171/jns.1989.70.6.0884. [DOI] [PubMed] [Google Scholar]
- 25.Della Torre P, Rinonapoli E. Halo-cast treatment of fractures and dislocations of the cervical spine. Int Orthop. 1992;16:227–31. doi: 10.1007/BF00182699. [DOI] [PubMed] [Google Scholar]
- 26.De Smet L, Vercauteren M, Verdonk R, Claessens H. Severe acute cervical spine injuries. Conservative treatment. Acta Orthop Belg. 1984;50:512–20. [PubMed] [Google Scholar]
- 27.Rockswold GL, Bergman TA, Ford SE. Halo immobilization and surgical fusion: Relative indications and effectiveness in the treatment of 140 cervical spine injuries. J Trauma. 1990;30:893–8. [PubMed] [Google Scholar]
- 28.Brodke DS, Anderson PA, Newell DW, Grady MS, Chapman JR. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech. 2003;16:229–35. doi: 10.1097/00024720-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Kwon BK, Fisher CG, Boyd MC, Cobb J, Jebson H, Noonan V, et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1–12. doi: 10.3171/SPI-07/07/001. [DOI] [PubMed] [Google Scholar]


