Abstract
Background:
Craniovertebral surgeries require the anatomical knowledge of craniovertebral junction. The human occipital condyle (OC) is unique bony structure connecting the cranium and the vertebral column. A lateral approach like transcondylar approach (TA) requires understanding of the relationships between the OC, jugular tubercle, and hypoglossal canal. Hence, the aim of the present study was to analyze the morphological variations in OCs of dry adult human skull.
Materials and Methods:
The study was carried out on 142 OC of 71 adult human dry skulls (55 males and 16 females). Morphometric parameters such as length, width, thickness, intercondylar distances, and the distances from the OC to the foramen magnum, hypoglossal canal and jugular foramen were measured. In addition, the different locations of the hypoglossal canal orifices in relation to the OC and different shapes of the OC were also noted.
Results:
The average length, width and height of the OC were found to be 2.2, 1.1 and 0.9 cm. The anterior and posterior intercondylar distances were 2.1 and 3.9 cm, respectively. Maximum and minimum bicondylar distances were 4.5 and 2.6 cm, respectively. The intra-cranial orifice of the hypoglossal canal was found to be present in middle 1/3rd in all skulls (100%), and extra-cranial orifice of the hypoglossal canal was found to be in anterior 1/3rd (98%) in relation to OC. The oval shaped OC (22.5%) was the most predominant type of OC observed in these skulls.
Conclusion:
Occipital condyle is likely to have variations with respect to shape, length, width and its orientation. Therefore, knowledge of the variations in OC along with careful radiological analysis may help in safe TAs during skull base surgery.
Keywords: Hypoglossal canal, jugular foramen, occipital condyle, surgical anatomy, transcondylar approach
INTRODUCTION
Tumors at the craniovertebral junction (CVJ) are difficult to remove because of their location and complex anatomic relations. The stability of this CVJ depends largely on the morphometric parameters of the occipital condyles (OCs).[1] Each OC is oriented obliquely, so that its anterior end lies closer to the midline. The hypoglossal canal directed laterally and slightly forwards, and jugular foramen (JF) is lateral to each condyle. Despite the fact that variations in shapes of the OC, as well as the measurements and incidence, have been reported in the previous clinical and anatomical studies, it has been observed during the dissection that the pattern of the OC in the CVJ was not as simple as it had been reported by many authors.[2,3,4,5]
The condylar parts of the occipital bone flank the foramen magnum (FM). Tumors at the level of FM can be reached surgically by using ventral and dorsal approaches. As the ventral approach is dangerous and has a high rate of morbidity, the dorsal approach is mostly preferred at the CVJ.[6,7] In recent times, transcondylar approach (TA) has been used in surgeries to access lesions in areas close to the FM which is performed by piercing the OC above the occipital junction, below the hypoglossal canal through the direct path of the OC. The extent of bony removal for optimal exposure is unclear ranging from suboccipital craniotomy to total OC removal.[6,7,8,9,10] This approach decreases the depth of the surgical area and provides better visibility without brain retraction. Nevertheless, it is important to plan and calculate the bone extent to be resected.[11] Therefore, transcondylar surgical approaches need adequate information about the metric and nonmetric aspect of the OC for safe surgical outcome. The objective of the present study was to clarify the morphometric data of the OC and its surgical implications in TA.
MATERIALS AND METHODS
The study was performed on 142 OC of 71-adult human (55 male, 16 female) dry skulls. Metric and nonmetric study was performed in the collected specimens. The parameters examined for OC (bilaterally) were as below [Figures 1–3].
Figure 1.
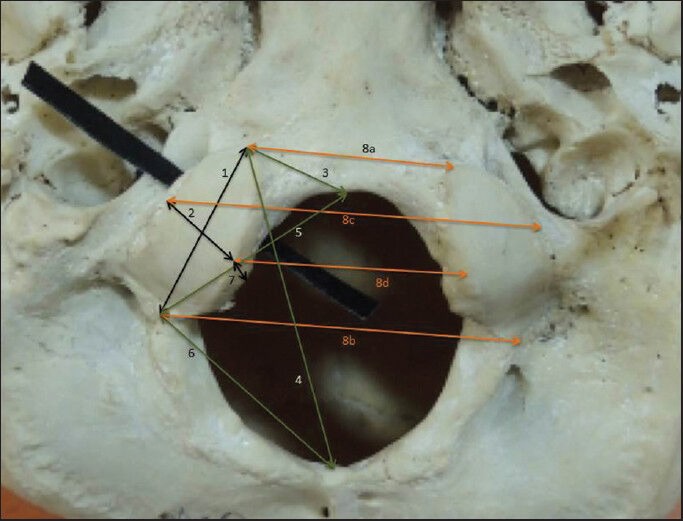
Some metric parameters of occipital condyle (OC). (1) Length of OC. (2) Width of OC. (3) Distance between the anterior tip of OC and basion. (4) Distance between the anterior tip of OC and opisthion. (5) Distance between posterior tip of OC and basion. (6) Distance between posterior tip of OC and opisthion. (7) Thickness of OC. (8a) Anterior intercondylar distance. (8b) Posterior intercondylar distance. (8c) Bicondylar distance is lateral. (8d) Bicondylar distance medial
Figure 3.
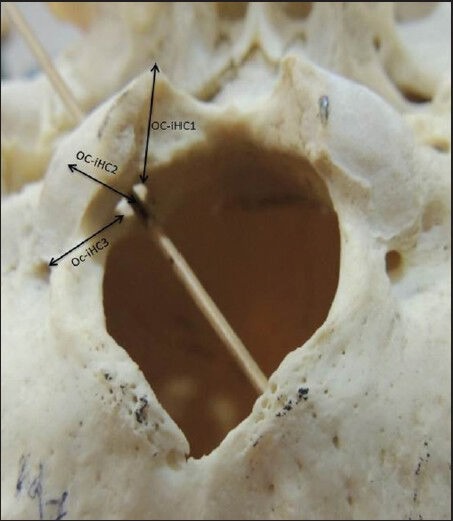
Metric parameters around intra-cranial end of the hypoglossal canal. Occipital condyle (OC-iHC1): Distance between OC and intra-cranial end of hypoglossal canal 1. OC-iHC2: Distance between OC and intra-cranial end of hypoglossal canal 2. OC-iHC3: Distance between OC and intra-cranial end of hypoglossal canal 3
Figure 2.
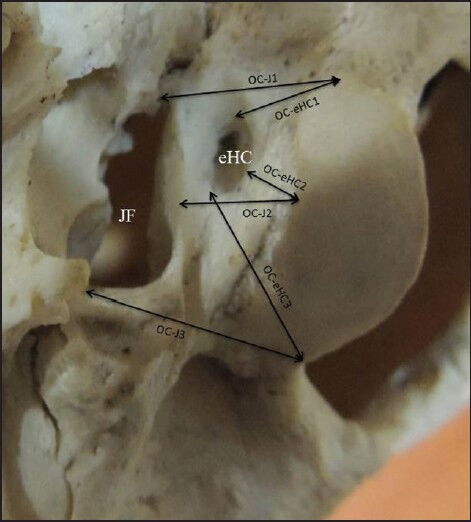
Metric parameters around hypoglossal canal and jugular foramen (JF). JF: Jugular foramen. eHC: Extra-cranial orifice of the hypoglossal canal. occipital condyle (OC-J1): Distance between OC and JF1. OC-eHC1: Distance between OC and extra-cranial end of hypoglossal canal 1. OC-eHC2: Distance between OC and extra-cranial end of hypoglossal canal 2. OC-J2: Distance between OC and JF2. OC-eHC3: Distance between OC and extra-cranial end of hypoglossal canal 3. OC-J3: Distance between OC and JF3
Length of occipital condyle
Width of occipital condyle
Distance between the anterior tip of occipital condyle and basion (OCAT-B)
Distance between the anterior tip of occipital condyle and opisthion (OCAT-O)
Distance between posterior tip of occipital condyle and basion (OCPT-B)
Distance between posterior tip of occipital condyle and opisthion (OCPT-O)
Distance between occipital condyle and jugular tubercle (OC-JT)
Thickness of occipital condyle (OC-TK)
Distance between occipital condyle and JF at three different places (OC-J1, OC-J2, and OC-J3)
Distance between occipital condyle and extra-cranial end of the hypoglossal canal at three different sites (OCAT-eHC1, OC-eHC2, OCPT-eHC3)
Distance between occipital condyle and intra-cranial end of the hypoglossal canal at three different sites (OCAT-iH1, OCPT-iHC2, OC-iHC3)
-
Intercondylar distance
- Anterior intercondylar distance (AID) between the anterior OC tips
- Posterior intercondylar distance (PID) between the posterior OC tips
- Bicondylar distance lateral (BC-L) — maximum distance between the lateral margins of the left and right condylar articular facets
- Bicondylar distance medial (BC-M) — maximum distance between the medial margins of the left and right condylar articular facets.
Nonmetric parameters
Shape of OC was classified into - S shaped, “eight” shaped, triangular, oval, kidney shaped, circular, two-portioned condyle and deformed condyle [Figure 4].
Based on the size, OC were classified as long, moderate and short according to length and wide, intermediate and narrow according to the width of the OC.
-
Relation of OC with hypoglossal canal was also noted. For location length of OC was divided into three equal parts [Figure 5].
- Location1 (anterior 1/3rd)
- Location 2 (middle 1/3rd)
- Location 3 (posterior 1/3rd).
Figure 4.
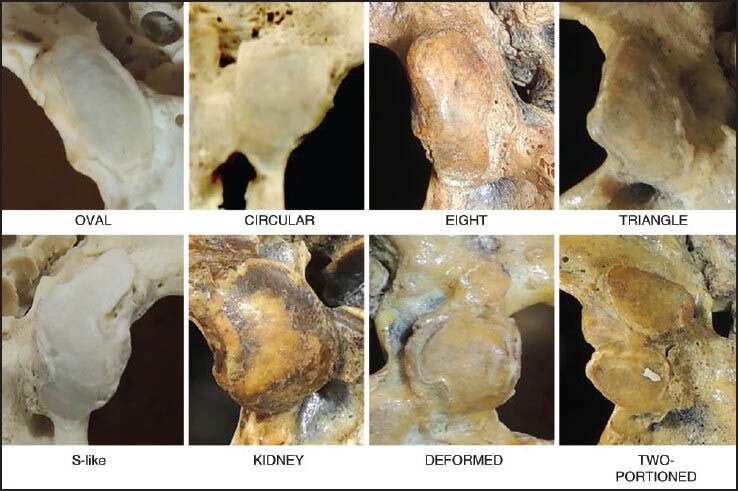
Different shapes of occipital condyle
Figure 5.
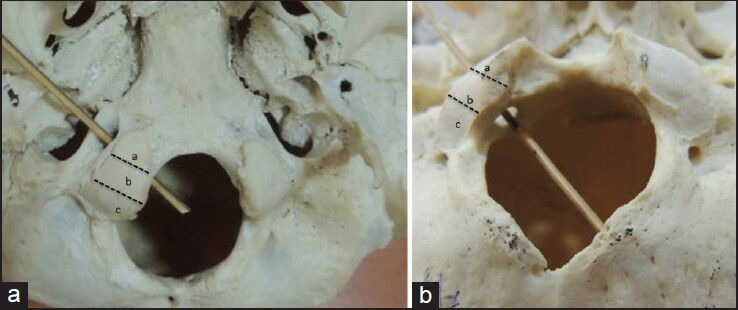
Location of the hypoglossal canal in relation to occipital condyle (OC). (a) Location 1 (anterior 1/3rd). (b) Location 2 (middle 1/3rd). (c) Location 3 (posterior 1/3rd). 5a: Extra-cranial hypoglossal canal related to anterior 1/3rd of OC. 5b: Intra-cranial hypoglossal canal related to middle 1/3rd of occipital condyle
All the measurements and frequencies of the data were tabulated and separated according to sex and skull side. All distances were measured using a digital sliding caliper (made in China), accurate to 0.01 mm. Descriptive statistics (mean, standard deviation [SD]) were evaluated for all the parameters collected from the skull measurements. For all the analyses, P < 0.05 was accepted as statistically significant, and statistical analysis was performed using IBM SPSS Statistics for Windows version 20.0, USA.
RESULTS
Seventy-one skulls investigated in the present study comprised 55 males (77.4%) and 16 females (22.5%). The results obtained from the metric parameters are presented in Table 1. The OCAT-B, OC-TK, OCPT-JF2, OCPT-iHC3 were significantly different between right and left side of the male skull (P < 0.05), while in female skulls there was a significant difference between right and left side OCAT-B, OCPT-B, OCPT-O, OC-TK, OCAT-iHC1 (P < 0.05). Similarly, the left OC-iHC2 was significantly different in male and female skulls (P < 0.05). The mean intercondylar distances are presented in Table 2. There was no significant difference between male and female intercondylar measurements [Table 2].
Table 1.
Morphometric measurements of occipital condyle

Table 2.
Intercondylar distance of occipital condyle

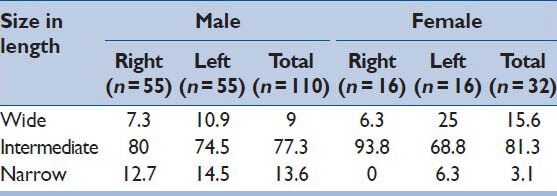
Occipital condyle was classified according to its length. The condyle of 2.2 ± 0.2 cm (i.e., mean length ± SD) (2–2.4 cm) was considered as moderate, the condyle shorter than 2 cm was considered as short and condyle longer than 2.4 cm was considered as long OC. Moderate length of OC was most common in both the sexes. Interestingly, males had long OC when compared to females [Table 3]. When we classified OC according to its width, the condyle of 1.1 ± 0.2 (i.e., mean length ± SD) (0.9-1.3 cm) was classified under intermediate, the condyle of 0.9 cm was classified as narrow and condyle >1.3 cm as wide OC. Intermediate type was common in both the sexes. Narrow type was more common (13.6%) in males, while in female skulls wide type was more common (5%) [Table 4].
Table 3.
Size of occipital condyle (%) according to length in males and females

Table 4.
Size of occipital condyle (%) according to the width in males and females
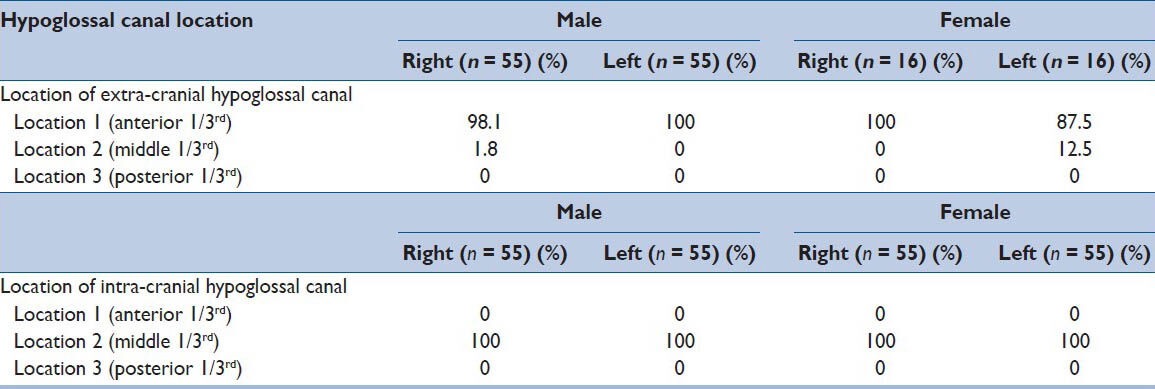
The locations of the intra-cranial and extra-cranial orifices of the hypoglossal canal in relation to the OC are represented in Table 5. It was found that the intra-cranial orifice of the hypoglossal canal was present in location 2 (middle 1/3rd) in 100% of OC for both genders. The extra-cranial orifice of the hypoglossal canal was found to be in a location 1 (anterior 1/3rd) in 98% and 93.7% for male and female. Only 1-2% was present in location 2. Direction of the hypoglossal canal in majority was antero-laterally and only in 2% cases it was directed transversely.
Table 5.
Locations of intra-cranial and extra-cranial orifices of the hypoglossal canal relative to the occipital condyle
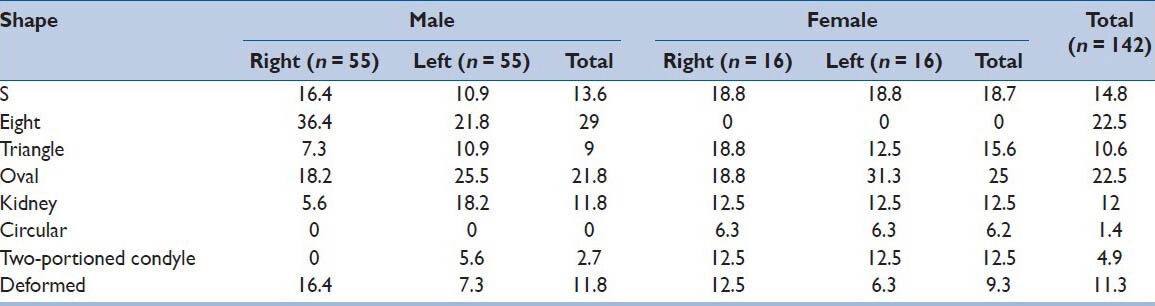
The shape of OC was classified into eight types. The most common type was oval both in males and females (21.8% and 25%, respectively), whereas the most unusual type in male was two-portioned (2.7%), whereas in female it was circular (6.2%). Other types are shown in [Figure 4 and Table 6]. Of a total of 142 OC oval and eight types OC were most common, followed by circular type. The symmetrical shape was found in 62%, and asymmetrical shape was found in 38%.
Table 6.
The rates of different occipital condyle shape
DISCUSSION
Anomalies of CVJ are of interest not only to an anatomist, but also to the clinicians because many of these deformities produce clinical symptoms. The most frequently reported lesions in this region are extra and intradural tumors, vertebral artery lesions, rheumatoid disease and malformations of the craniocervical junction, synovial cysts, infections, syringobulbia and intrinsic lesions (mostly demyelination).[12] Lesions located anterior to CVJ have posed a surgical challenge causing high mortality and morbidity.[13] Many surgical approaches and their several modifications have been developed to approach these lesions safely and effectively. Most of the craniovertebral approaches necessitate either partial or complete resection of the OC.[14,15,16,17,18] The type and size of the lesion along with its location designate which technique is to be used.
In the present study, the mean length of the OC was found to 2.2 ± 0.2 cm. This measured length is comparable to what was found by previous author as 2.3 cm.[15,16,19,20] but Dowd et al.[21] got the value as 3 cm, which was more than our study. The length of the OC is an important surgical issue. The results of partial condylectomy in short type are different from the results obtained in long type OC. The same amount of partial condylectomy may cause greater occipitocervical instability in short OC, whereas the long condyle may require more extensive resection for optimal visualization. In our study, we found short OC in 9.2% of the skulls. These results are in agreement with other investigators’ findings,[11,16,22] who observed short OC in 8.6%, 5%, and 7%, respectively. In our study, we also observed that women tend to have shorter OC than men, suggesting that women undertaking partial condylectomy with extensive condyle resection may be more vulnerable to atlanto-occipital instability than men, undertaking the same procedure.
The OC mean width was found to be 1.1 ± 0.2 cm. This measured width was in agreement with the results obtained by previous authors who reported the width as 1–1.4 cm.[14,15,16,19,23,24] Width of OC is also of surgical importance as one should know how much medially the condyle can be resected. In the present study, 11.3% were narrow, and males tend to have narrow OC than female. The thickness of OC also matters during condylectomy as one should know how deep OC has to be drilled. It was found to be 0.9 ± 0.1 cm. This was in agreement with the previous authors[16,20] who reported it as 0.9 cm and but the result obtained by Oliver[23] was 0.8 cm.
The OC converge ventrally. The anterior and PIDs were found to be 2.1 ± 0.3 and 3.9 ± 0.3 cm, respectively. These measured distances when compared to the results obtained by[16,19,20] was almost similar for AID as 2.1, 2.2, 2.0 cm, but the PID in our study was less when compared with the[16,19,20] who reported 4.1, 4.4, and 4.1 cm respectively. In the present study, the maximum distance between two OC (BC-L) and minimum distance (BC-M) was noted, which was found to be 4.5 ± 0.45 and 2.6 ± 0.33 cm. This wide difference between the anterior and PIDs leads the OC to have different anterior and posterior angles. The anteroposterior orientation and narrow intercondylar space would require a more bony removal.
The average distance between the OCAT-B was 1.2 ± 0.2 cm, and OCPT-B was 2.7 ± 0.2 cm. These measured distances are comparable to the results obtained by Naderi et al.[16] who reported them as 1.0 and 2.8 cm respectively and by Fetouh et al.[20] as 1.6 cm and 2.7 cm respectively. The distance between the OCAT-O and OCPT-O was 3.9 ± 0.3 and 2.8 ± 0.2 respectively in the present study. This was in agreement with Naderi et al.[16] who reported them as 3.9 and 2.6 cm respectively and Fetouh et al.[20] who reported it as OCAT-O as 5 cm and OCPT-O as 2.7 cm. The distance between the posterior tip of OC and the opisthion is important as it represents the width of surgical exposure in suboccipital craniotomy and larger the distance better is the access for the posterolateral approach.
Incomplete TA posterior half of the OC is drilled away. This resection leads to exposure of the hypoglossal canal, which forms the anterior limit of the condyle. If resection extends superior and inferior to this canal, most of the jugular tubercle (JT) and the entire condyle are removed.[7] So, the configuration and orientation of the OC with the locations of the intra - and extra-cranial orifices of the hypoglossal canal, JF and JT is important as they may get affected during TA.
In the present study, the orifice of the hypoglossal canal was in agreement with the result recorded by previous authors.[7,16,20] There was no hypoglossal canal orifice in the location 3 (posterior 1/3rd). During resection of the OC posterior one-third is resected. The length of posterior one-third of the OC can be calculated from the total length of OC. The total length of the OC in the present study ranged from 1.5 to 3.2 cm, hence the distance between the posterior edge of OC and intra-cranial orifice ranged from 0.5 to 1 cm with an average of 0.75 cm. This is nearly similar to that reported by Wen et al.,[7] the average distance between the posterior edge of the OC and the intra-cranial orifice of the hypoglossal canal is 0.84 cm (range: 0.6–1 cm). In a study conducted by Fetouh et al.[20] the averaged distance ranged from 0.4 to 0.7 cm from intra-cranial orifice and Naderi et al.[16] reported as 0.4-0.7 cm. On the other hand, Muthukumar et al.[15] and Kizilkanat[19] reported that the distance from the intra-cranial end of the hypoglossal canal to the posterior margin of the OC as 1.2 cm. In our study, we also observed gender differences in the presence of extra-cranial orifice of the hypoglossal canal. Females had presence of extra-cranial orifice in location 2 more as compared to males. Hence, the exact location of the intra-cranial and extra-cranial orifices of the hypoglossal canal is important during condylectomy. Too dorsally located intra-cranial orifice of the hypoglossal canal may complicate and limit the TA. Hence, the distance of inner and outer openings of the hypoglossal canal from the borders of OC serves an important surgical guide in extension of condylar drilling. The distance between OCPT-eHC3 is also important, while drilling the condyle and in the present study it was 1.5 ± 0.2 cm.
In procedures like extreme lateral infrajugular transcondylar–transtubercular exposure drilling of JT is required. The JT is deeply placed and requires extradural drilling in order to avoid any damage to the lower cranial nerves. Significant injury to adjacent neurovascular structures can occur if the anatomy of this structure is not fully understood. The mean distance of OC-JT was found to be 2 ± 0.2 cm in the present study. During condylectomy, care should be taken not to approach the jugular canal as important cranial nerves lie long with venous structure. The distance between OC and JF at various places was noted, and minimum distance found was 0.8 ± 0.2 cm at OC-JF2.
Many previous studies reported different classifications for the shapes of the OC.[14,23,25] We followed the classification of Naderi et al.[16] The oval shaped OC was found to be the most common type which was in agreement with Naderi et al.[16] However, Fetouh et al.[20] found kidney shape to be most common. Among the different types of OC, the triangular, the deformed and kidney shaped types may require more extensive condylectomy to reach the ventral lesions. In the present study, males showed triangular and kidney shaped more in comparison to females. Symmetry of the OC does not pose any difficulty in flexion, extension and lateral bending, but asymmetrical facets will give rise to altered kinematics in the atlanto-occipital joint.
These measurements can be helpful for neurosurgeons for performing lateral transcondylar surgical approaches for reaching lesions in the middle and posterior part of the cranial base. Understanding the pathology of these abnormalities and their treatment is simplified if one has the knowledge of bony anatomy, biomechanics and embryology of this region. Therefore, the assessment of morphometric of OC is essential.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Vishteh AG, Crawford NR, Melton MS, Spetzler RF, Sonntag VK, Dickman CA. Stability of the craniovertebral junction after unilateral occipital condyle resection: A biomechanical study. J Neurosurg. 1999;90:91–8. doi: 10.3171/spi.1999.90.1.0091. [DOI] [PubMed] [Google Scholar]
- 2.Das S, Suri R, Kapur V. Unusual occipital condyles of the skull: An osteological study with clinical implications. Sao Paulo Med J. 2006;124:278–9. doi: 10.1590/S1516-31802006000500009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peyton WT, Peterson HO. Congenital deformities in the region of the foramen magnum: Basilar impression. Radiol. 1942;38:131–44. [Google Scholar]
- 4.Suhardja A, Agur AM, Cusimano MD. Anatomical basis of approaches to foramen magnum and lower clival meningiomas: Comparison of retrosigmoid and transcondylar approaches. Neurosurg Focus. 2003;14:e9. doi: 10.3171/foc.2003.14.6.9. [DOI] [PubMed] [Google Scholar]
- 5.Terasaka S, Day JD, Fukushima T. Extended transbasal approach: Anatomy, technique, and indications. Skull Base Surg. 1999;9:177–84. doi: 10.1055/s-2008-1058144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.al-Mefty O, Borba LA, Aoki N, Angtuaco E, Pait TG. The transcondylar approach to extradural nonneoplastic lesions of the craniovertebral junction. J Neurosurg. 1996;84:1–6. doi: 10.3171/jns.1996.84.1.0001. [DOI] [PubMed] [Google Scholar]
- 7.Wen HT, Rhoton AL, Jr, Katsuta T, de Oliveira E. Microsurgical anatomy of the transcondylar, supracondylar, and paracondylar extensions of the far-lateral approach. J Neurosurg. 1997;87:555–85. doi: 10.3171/jns.1997.87.4.0555. [DOI] [PubMed] [Google Scholar]
- 8.George B, Dematons C, Cophignon J. Lateral approach to the anterior portion of the foramen magnum. Application to surgical removal of 14 benign tumors: Technical note. Surg Neurol. 1988;29:484–90. doi: 10.1016/0090-3019(88)90145-0. [DOI] [PubMed] [Google Scholar]
- 9.Bertalanffy H, Seeger W. The dorsolateral, suboccipital, transcondylar approach to the lower clivus and anterior portion of the craniocervical junction. Neurosurgery. 1991;29:815–21. doi: 10.1097/00006123-199112000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Tedeschi H, Rhoton AL., Jr Lateral approaches to the petroclival region. Surg Neurol. 1994;41:180–216. doi: 10.1016/0090-3019(94)90123-6. [DOI] [PubMed] [Google Scholar]
- 11.Barut N, Kale A, Turan Suslu H, Ozturk A, Bozbuga M, Sahinoglu K. Evaluation of the bony landmarks in transcondylar approach. Br J Neurosurg. 2009;23:276–81. doi: 10.1080/02688690902814725. [DOI] [PubMed] [Google Scholar]
- 12.Cross J, Coles A. Suppliers of advanced neuro embolization coils. Adv Clin Neurosci Rehabil. 2002;2:16–7. [Google Scholar]
- 13.Babu RP, Sekhar LN, Wright DC. Extreme lateral transcondylar approach: Technical improvements and lessons learned. J Neurosurg. 1994;81:49–59. doi: 10.3171/jns.1994.81.1.0049. [DOI] [PubMed] [Google Scholar]
- 14.Bozbuga M, Oztürk A, Bayraktar B, Ari Z, Sahinoglu K, Polat G, et al. Surgical anatomy and morphometric analysis of the occipital condyles and foramen magnum. Okajimas Folia Anat Jpn. 1999;75:329–34. doi: 10.2535/ofaj1936.75.6_329. [DOI] [PubMed] [Google Scholar]
- 15.Muthukumar N, Swaminathan R, Venkatesh G, Bhanumathy SP. A morphometric analysis of the foramen magnum region as it relates to the transcondylar approach. Acta Neurochir (Wien) 2005;147:889–95. doi: 10.1007/s00701-005-0555-x. [DOI] [PubMed] [Google Scholar]
- 16.Naderi S, Korman E, Citak G, Güvençer M, Arman C, Senoglu M, et al. Morphometric analysis of human occipital condyle. Clin Neurol Neurosurg. 2005;107:191–9. doi: 10.1016/j.clineuro.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 17.Schwaber MK, Netterville JL, Maciunas R. Microsurgical anatomy of the lower skullbase – a morphometric analysis. Am J Otol. 1990;11:401–5. [PubMed] [Google Scholar]
- 18.Spektor S, Anderson GJ, McMenomey SO, Horgan MA, Kellogg JX, Delashaw JB., Jr Quantitative description of the far-lateral transcondylar transtubercular approach to the foramen magnum and clivus. J Neurosurg. 2000;92:824–31. doi: 10.3171/jns.2000.92.5.0824. [DOI] [PubMed] [Google Scholar]
- 19.Kizilkanat E. Morphometry of the hypoglossal canal, occipial condyle and foramen magnum. Neurosurg Q. 2006;16:121–5. [Google Scholar]
- 20.Fetouh FA, Awadalla AM. Morphometric analysis of the occipital condyle and its surgical implications in transcondylar approach. The pan arab neurosurgery society. about 15 p. http://panarabjn.org/wp-content/uploads/2013/03 .
- 21.Dowd GC, Zeiller S, Awasthi D. Far lateral transcondylar approach: Dimensional anatomy. Neurosurgery. 1999;45:95–9. doi: 10.1097/00006123-199907000-00023. [DOI] [PubMed] [Google Scholar]
- 22.Natsis K, Piagkou M, Skotsimara G, Piagkos G, Skandalakis P. A morphometric anatomical and comparative study of the foramen magnum region in a Greek population. Surg Radiol Anat. 2013;35:925–34. doi: 10.1007/s00276-013-1119-z. [DOI] [PubMed] [Google Scholar]
- 23.Olivier G. Biometry of the human occipital bone. J Anat. 1975;120:507–18. [PMC free article] [PubMed] [Google Scholar]
- 24.Ozer MA, Celik S, Govsa F, Ulusoy MO. Anatomical determination of a safe entry point for occipital condyle screw using three-dimensional landmarks. Eur Spine J. 2011;20:1510–7. doi: 10.1007/s00586-011-1765-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guidotti A. Morphometrical considerations on occipital condyles. Anthropol Anz. 1984;42:117–9. [PubMed] [Google Scholar]


