Abstract
Introduction:
Basilar invagination (BI) is a congenital craniocervical junction (CCJ) anomaly represented by a prolapsed spine into the skull-base that can result in severe neurological impairment.
Materials and Methods:
In this paper, we retrospective evaluate the surgical treatment of 26 patients surgically treated for symptomatic BI. BI was classified according to instability and neural abnormalities findings. Clinical outcome was evaluated using the Nürick grade system.
Results:
A total of 26 patients were included in this paper. Their age ranged from 15 to 67 years old (mean 38). Of which, 10 patients were male (38%) and 16 (62%) were female. All patients had some degree of tonsillar herniation, with 25 patients treated with foramen magnum decompression. Nine patients required a craniocervical fixation. Six patients had undergone prior surgery and required a new surgical procedure for progression of neurological symptoms associated with new compression or instability. Most of patients with neurological symptoms secondary to brainstem compression had some improvement during the follow-up. There was mortality in this series, 1 month after surgery, associated with a late removal of the tracheal cannula.
Conclusions:
Management of BI requires can provide improvements in neurological outcomes, but requires analysis of the neural and bony anatomy of the CCJ, as well as occult instability. The complexity and heterogeneous presentation requires attention to occult instability on examination and attention to airway problems secondary to concomitant facial malformations.
Keywords: Basilar invagination, congenital craniocervical malformation, surgical treatment
INTRODUCTION
The craniocervical junction (CCJ) comprises the region located between the skull-base and the upper cervical spine (atlas and axis), along with its neural components (brainstem and spinal cord).[1] Its stability is mainly based on strong complex ligamentous and bony structures that are also responsible for the majority of axial rotation (at the atlantoaxial complex) and flexion-extension movements (at the occiput-C1 joint).[2,3,4,5,6] One of the most common CCJ anomalies is basilar invagination (BI), a radiographic finding represented by a prolapsed spine into the skull-base, diagnosed when the tip of the odontoid process is located at least 2 mm above of Chamberlain's line.[6] Different thresholds are also found in literature, such as 5 or 6.6 mm.[7,8] Many osseous anomalies are associated with BI, such as clivus and condyle hypoplasia, atlas assimilation and subaxial vertebral body fusion.[9] Tonsillar herniation is described as an associated neural finding that can lead to neurological impairment and can drive surgical treatment.[7,8]
In this paper, we review a case series of patients treated for symptomatic BI, discussing the different strategies required to manage this complex CCJ disease, as well as complications and patients’ neurological outcomes.
MATERIALS AND METHODS
A retrospective evaluation of a consecutive series of patients surgically treated for treatment of symptomatic BI between January 2009 and September 2013 by one of the authors (AFJ) was performed. Institutional Ethical Committee approval was obtained prior to the study (CAAE: 17337313.7.0000.5404).
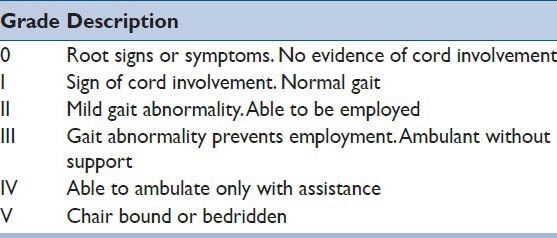
Clinical data included: Age, sex, follow-up, surgical indication, surgical complications, and neurological status before and after surgery. The pre- and post-operative functional status was classified according to the Nürick Scale [Table 1].[10]
Table 1.
Nürick scale for evaluation the neurological status
Radiological evaluations consisted in a craniocervical magnetic resonance (MR) and a computed tomography (CT) with sagittal and coronal reconstructions. A flexion and extension CT scan was also required when instability could not be clearly inferred based on static examinations.
Patients were diagnosed as having BI when the tip of the odontoid was located 2 mm above the Chamberlain's line on sagittal CT scan reconstructions.
Our protocol of treatment included foramen magnum decompression when tonsillar herniation was compressing the medulla or the spinal cord. In selected cases, craniocervical realignment and stabilization was performed in patients with static or dynamic atlanto-axial instability. Realignment consists of preoperative traction or direct C1-C2 manipulation or occipital C2 distraction [Figure 1].
Figure 1.
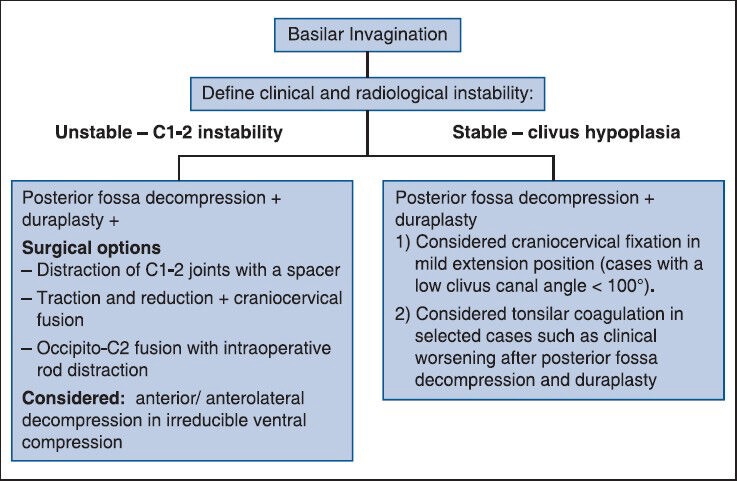
Surgical decision-making flow chart for patients with basilar invagination
Radiological data were used to assess the surgical procedure, technique of fixation used (when applied), and late radiological complications.
RESULTS
Twenty-six patients were included in this series. Age ranged from 15 to 67 years old (mean 38 and median of 38.5 years old). Ten patients were male (38%), and 16 (62%) were female. All patients had tonsillar herniation below the foramen magnum.
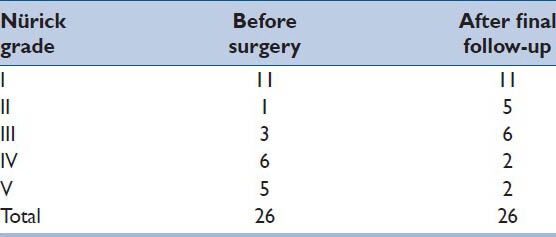
Follow-up ranged from 1 to 25 months (average of 9 and median of 6). Most of the patients had clinical improvement, as shown in Table 2, according to the Nürick grade system. Of note, some patients had also axial cervical pain with significant improvement after surgery, although this change did not alter the Nürick grade (11 patients with Nürick Grade I still Grade I, although they were satisfied with surgery, with less clinical symptoms). Eight patients improved one grade in the Nürick system and three improved within two grades.
Table 2.
Clinical evolution of the patients before surgery and after final follow-up assessment according to the Nürick grade system
All the patients underwent foramen magnum decompression, except patient 5, who underwent an occipitocervical fixation and fusion in mild extension. This patient only had symptoms upon cervical flexion and demonstrated a mild tonsillar herniation. He was clinically stable after 22 months of follow-up.
Nine patients underwent craniocervical instrumentation and fusion with concomitant foramen magnum decompression: Three patients for atlanto-axial instability secondary to evident lysthesis of the facet joints in static CT and/or MR imaging; four patients for abnormal subluxation detected on dynamic CT scan between C1 and C2 (increased atlanto-dens interval in flexion and extension) and two for severe craniocervical kyphosis (clivus-canal angle of <90°).
Six patients of our series were had surgery prior to presentation to our institution and underwent a revision surgical procedure for progression of their neurological symptoms. Four had developed new compression and instability after foramen magnum decompression. One had a prior craniocervical fixation without foramen magnum decompression in flexion with pseudarthrosis and failed instrumentation. Finally, one patient had a prior occipitocervical fusion without reduction of the anterior brainstem compression secondary to C1-C2 listhesis.
Minor complications included wound dehiscence in five patients: Three were treated with antibiotics only, one required surgical debridement besides antibiotics and one required a cranial flap due to poor skin coverage associated with prior surgical treatment (patient 13). One patient who underwent a transoral dens resection developed meningitis, even though a cerebrospinal fluid (CSF) leak was not noted during the procedure (patient 6), and was treated with antibiotics only without neurological compromise.
There was mortality in this series, 1 month after surgery associated with removal of a tracheal cannula. The patient was waiting a new tracheal cannula for hospital discharge. The head and neck department weaned her tracheotomy cannula, but she had a tracheal collapse some hours later, with acute respiratory failure.
Two illustrative cases are presented in Figures 2 and 3 and Table 3 content the general results of these series
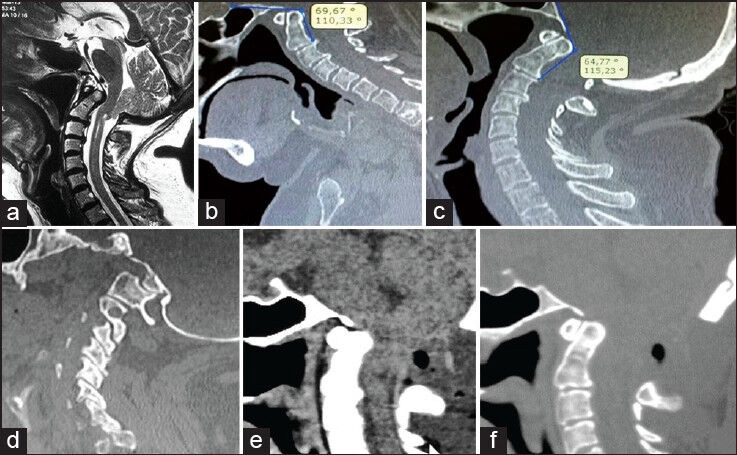
Figure 2.
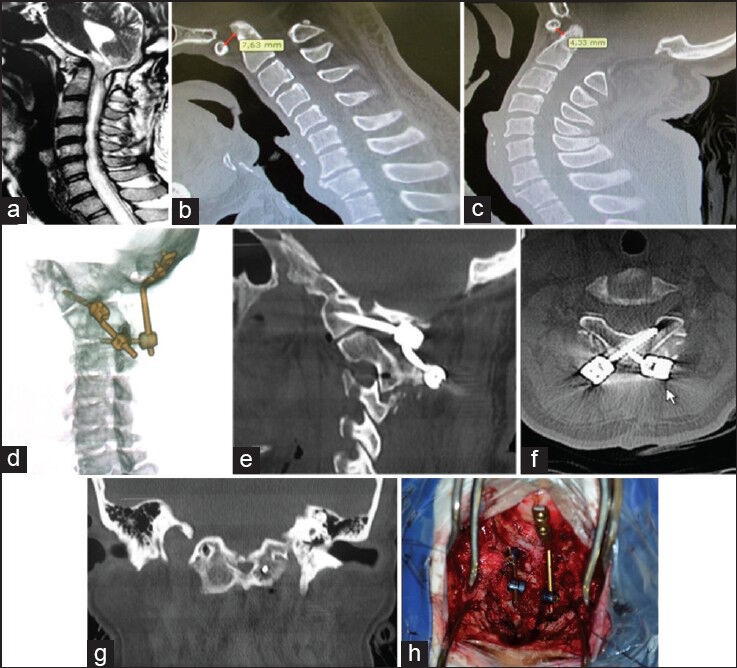
Illustrative case – Patient 9-presented with a severe neurological deterioration 3 years after a posterior fossa decompression for treatment a tonsillar herniation. (a) Sagittal T2 sequence magnetic resonance imaging showing odontoid compression over the brainstem and upper spinal cord. (b and c) Flexion and extension CT scan sagittal reconstructions showing atlanto-axial instability. (d) CT scan 3D reconstruction of a unilateral C1-C2 fusion and unilateral occipito-C2 fusion. (e) Note the C1 lateral mass screws and the fusion of the occipital condyle with C1. (f) Laminar screws at C2. (g) Coronal CT scan showing the left C1 screw in the lateral mass. (h) Intraoperative view of the final construction
Figure 3.
Illustrative case – Patient 25-presented with cervical neck pain after moderate walking and signs of cord compression (hyperreflexia, a positive Babinski sign) without gait complaints. (a) Sagittal T2 sequence magnetic resonance imaging showing tonsillar herniation and syrinx in the cervical spinal cord. (b and c) Flexion and extension CT scan sagittal reconstructions showing atlanto-axial stability. The clivus canal angle changed from 110° in flexion through 115° in extension. (d) Sagittal CT scan showing a normal facet joints congruence despite an important clivus hipoplasia. (e and f) Postoperatory sagittal CT scan after posterior fossa decompression and dura mater expansion with fascia graft. The patient reported significant relief of cervical axial pain after 4 months of follow-up
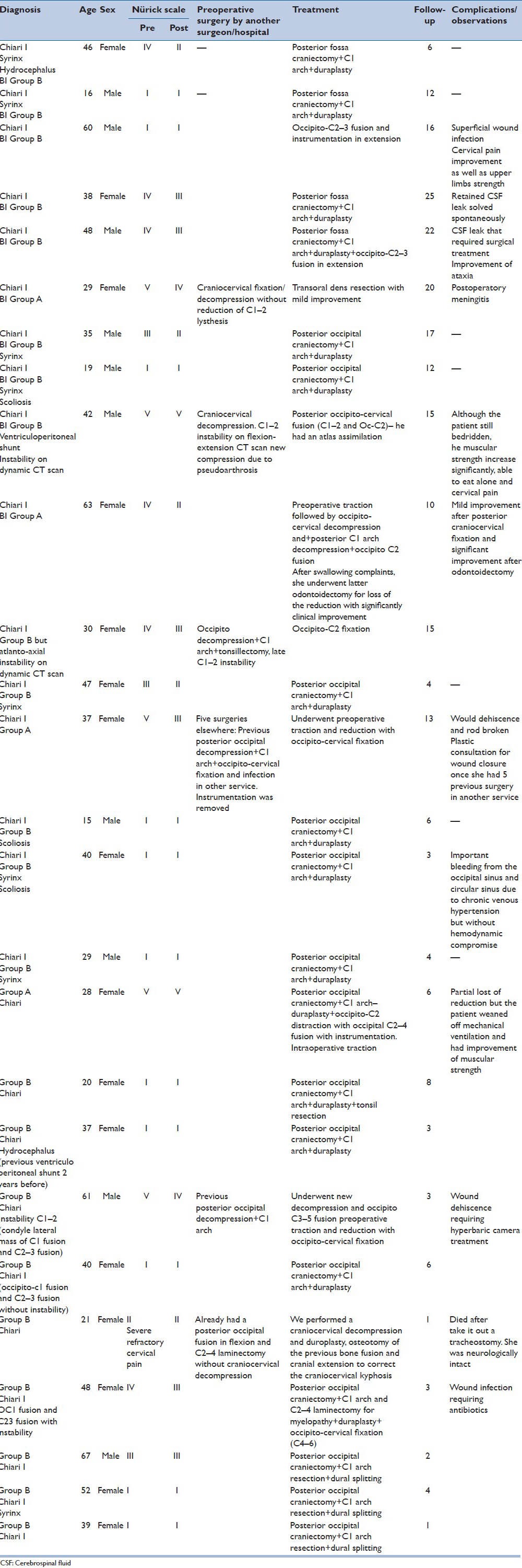
Table 3.
Clinical data of the 26 patients surgically treated for basilar invagination
DISCUSSION
Basilar invagination refers to a radiological finding secondary to a developmental anomaly of the occipital bone and upper cervical spine where the tip of the odontoid process is located at least 2 mm above Chamberlain's line.[6] It was described by Ackermann in 1790, in cretins from the Alps.[11] This neurodysplasia results in a prolapsed vertebral column into the skull-base that can lead to neural compression or craniocervical instability. Chiari I malformation (CMI) is commonly associated with BI. CMI is the most common CCJ malformation, represented by tonsillar herniation into the spinal canal and can be associated with BI in more than 90% of the cases.[7,9,12,13] In an analysis of 100 cases with CMI, Menezes and Traynelis have reported that 92 (92%) were associated with BI, and 34 (34%) had reducible ventral compression due to atlantoaxial instability which received craniocervical fixation concomitant to posterior fossa decompression.[9] Syrinx is presented in about 50% of the cases, probably due to the CSF blockade at the foramen magnum region.[14,15,16]
Management of BI, most of the times should be different than those cases of tonsillar herniation present in isolation. Goel proposed a classification for BI based on the presence (Group A) or absence (Group B) of clinical and radiological instability between C1 and C2.[6] The importance of this classification is that it helps surgeons to choose the best strategy to manage these patients.
Patients with BI and C1-C2 instability can be treated with three posterior approaches described in the literature:
Preoperative traction with reduction followed by craniocervical fixation and fusion;[7]
C1-C2 direct joint manipulation with distraction of the joints and spacers for maintaining reduction[17] and
direct intraoperative distraction between the occipito and C2 using pedicle screws instrumentation.[18]
Anterior approaches are only used in patients with irreducible ventral compression as we performed in two of our patients (patients 6 and 10). Instability can be misdiagnosed in patients if flexion and extension radiological examination are not performed –3 (11%) patients of our series had instability detected on dynamic CT scan reconstruction. This assures our policy of performing dynamic CT scan reconstruction in flexion and extension in all patients with CMI or BI before surgery, especially in patients who underwent a posterior foramen magnum decompression. We have treated three patients with BI and C1-C2 lysthesis (Goel Group A).[19,20,21] Patients 15 and 16 received preoperative traction with reduction of C1-C2 instability followed by craniocervical fixation. In patient 9, an anterior approach was used once the patient had a previous craniocervical fusion without C1-C2 reduction and a persistent irreducible anterior brainstem compression.
Patients with BI secondary to clivus hypoplasia and without C1-C2 instability can be treated with posterior foramen magnum decompression — the most common treatment for patients in this group — based on the principle of increasing the posterior fossa volume.[6] In such cases, where instability is not present, treatment is similar to pure CMI, with controversies regarding the size of the craniectomy — a small versus a large suboccipital decompression — and the extension of the laminectomy to the cervical spine (C1, C2 or even C3).[15,22,23,24] Controversies regarding bone decompression with or without concomitant duraplasty or even tonsils resection to preservate the arachnoid are also found.[6,25,26] In our series, all the patients except one (patient 5) underwent a suboccipital bone decompression from below the inferior nucal line to the posterior and lateral edges of the foramen magnum, including the posterior arch of the atlas, followed by duraplasty with autologous graft (muscle fascia) without tonsil resection. It's our policy to perform duroplasty in all cases; although, we did not perform routine tonsils resection to avoid arachnoid scarring and late syrinx to CSF blockage. In cases of severe tonsillar herniation (tonsils displaced beyond C1), we then performed tonsil coagulation (two patients in this series). In selected cases (patients with severe craniocervical kyphosis), a posterior craniocervical decompression followed by craniocervical fixation in extended position in proposed to increase the clivus canal angle and decrease brainstem compression.[22] Two patients with BI secondary to clivus hypoplasia underwent craniocervical fusion in slight extension for a treatment of craniocervical kyphosis (clivus-canal angle of <90°). Both patients have substantial clinical improvement after surgery. Of note, one of these patients (patient 5) did not undergo posterior fossa decompression, once his symptoms were clearly exacerbated by head flexion. Despite that, he significantly improved of his complaints.
Although we performed nine craniocervical fixations in this series, we used C1 lateral mass screws in just one case (patient 13). This patient was operated previously, underwent a foramen magnum decompression, dural expansion, and tonsils coagulation, but developed a late C1-C2 instability with neurological deterioration.
Noteworthy, our craniocervical fixations were extended caudally up to the level of C3 with most of them being occipito-C2 fixations. In the out-patient clinics, we did not have significant complaints of head movement restrictions, probably because small constructions seem to do better than long ones.
As shown in Table 2, almost all the patients classified as Nurick Grade II or more had some degree of the neurological improvement during follow-up. Most patients with Nurick Grade I had improvement in pain symptoms, although the score remains the same. This was a limitation of our retrospective study, which could be solved using others outcome instruments, but it is our perception that patients are satisfied with surgery after hospital discharge.
There was mortality in this series 1 month after surgery associated with management of the tracheal cannula. It is important to remember that patients with severe craniocervical malformations can also have craniofacial abnormalities that can lead to difficult airways. An experienced team on difficult airways is mandatory when managing these patients to avoid catastrophic complications such as this.
Although anterior decompression use is decreasing, some patients with persistent symptoms can benefits from it. Patient 6 had a prior craniocervical fixation at another facility without correction of C1-C2 lysthesis and symptomatic anterior compression remained, so we decided to perform a transoral decompression of the dens with some significant neurological improvement. Patient 10 also had an anterior decompression for persistent symptomatic anterior compression after posterior occipital-C2 fixation and swallowing problems, despite a good craniocervical arthrodesis. She was eating without problems in the last follow-up consultation.
CONCLUSION
Management of congenital craniocervical anomalies requires a deep analysis of the neural and bony anatomy of the CCJ. Surgical treatment has a high rate of morbidity and morbidity, especially in previously treated patients in nonreferral centers, although the benefits of surgery overweight the risks. Treatment should be individualized based on the patient anatomy, presence or absence of instability and surgeon's experience. Most of the times, BI is managed differently than isolated CMI, especially regarding atlanto-axial instability. Attention to the principles above has proven to be helpful in improving surgical results in the treatment of these patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Dickman CA, Lekovic GP. Biomechanical considerations for stabilization of the craniovertebral junction. Clin Neurosurg. 2005;52:205–13. [PubMed] [Google Scholar]
- 2.Joaquim AF, Ghizoni E, Rubino PA, Anderle DV, Tedeschi H, Rhoton AL, Jr, et al. Lateral mass screw fixation of the atlas: Surgical technique and anatomy. World Neurosurg. 2010;74:359–62. doi: 10.1016/j.wneu.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Joaquim AF, Cavalcante RA, Rodrigues IJ, Mudo ML. Occipito-C2 laminar screws fixation for treatment of chronic C1-2 instability. J Bras Neurocirugía. 2011;22:186–9. [Google Scholar]
- 4.Joaquim AF, Patel AP. Occipito cervical trauma: Evaluation, classification and treatment. Contemp Spine Surg. 2010;11:1–5. [Google Scholar]
- 5.Joaquim AF, Patel AP. C1 and C2 spine trauma: Evaluation, classification and treatment. Contemp Spine Surg. 2010;11:1–7. [Google Scholar]
- 6.Goel A. Basilar invagination, Chiari malformation, syringomyelia: A review. Neurol India. 2009;57:235–46. doi: 10.4103/0028-3886.53260. [DOI] [PubMed] [Google Scholar]
- 7.Smith JS, Shaffrey CI, Abel MF, Menezes AH. Basilar invagination. Neurosurgery. 2010;66:39–47. doi: 10.1227/01.NEU.0000365770.10690.6F. [DOI] [PubMed] [Google Scholar]
- 8.Smoker WR. Craniovertebral junction: Normal anatomy, craniometry, and congenital anomalies. Radiographics. 1994;14:255–77. doi: 10.1148/radiographics.14.2.8190952. [DOI] [PubMed] [Google Scholar]
- 9.Menezes AH, Traynelis VC. Anatomy and biomechanics of normal craniovertebral junction (a) and biomechanics of stabilization (b) Childs Nerv Syst. 2008;24:1091–100. doi: 10.1007/s00381-008-0606-8. [DOI] [PubMed] [Google Scholar]
- 10.Nurick S. The natural history and the results of surgical treatment of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95:101–8. doi: 10.1093/brain/95.1.101. [DOI] [PubMed] [Google Scholar]
- 11.Ackermann JF. Gotha: In Der Ettingerschen Buchhandlung; 1790. Über die Kretinen, eine besondere Menschenabart in den Alpen. [Google Scholar]
- 12.Chiari H. Über Veränderungen des Kleinhirns infolge von Hydrocephalie des Grosshirns. Dtsch Med Wschenschr. 1891;17:1172–5. [Google Scholar]
- 13.Chiari H. Über veränderungen des kleinhirns, des pons und der medulla oblongata in folge von congenitaler hydrocephalie des grosshirns. Dtsch Akad Wiss. 1895;63:71–125. [Google Scholar]
- 14.Menezes AH. Evaluation and treatment of congenital and developmental anomalies of the cervical spine. Invited submission from the joint section meeting on disorders of the spine and peripheral nerves, March 2004. J Neurosurg Spine. 2004;1:188–97. doi: 10.3171/spi.2004.1.2.0188. [DOI] [PubMed] [Google Scholar]
- 15.da Silva JA, dos Santos AA, Jr, Melo LR, de Araújo AF, Regueira GP. Posterior fossa decompression with tonsillectomy in 104 cases of basilar impression, Chiari malformation and/or syringomyelia. Arq Neuropsiquiatr. 2011;69:817–23. doi: 10.1590/s0004-282x2011000600018. [DOI] [PubMed] [Google Scholar]
- 16.Oldfield EH, Muraszko K, Shawker TH, Patronas NJ. Pathophysiology of syringomyelia associated with Chiari I malformation of the cerebellar tonsils. Implications for diagnosis and treatment. J Neurosurg. 1994;80:3–15. doi: 10.3171/jns.1994.80.1.0003. [DOI] [PubMed] [Google Scholar]
- 17.Goel A: Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1:281–6. doi: 10.3171/spi.2004.1.3.0281. [DOI] [PubMed] [Google Scholar]
- 18.Jian FZ, Chen Z, Wrede KH, Samii M, Ling F. Direct posterior reduction and fixation for the treatment of basilar invagination with atlantoaxial dislocation. Neurosurgery. 2010;66:678–87. doi: 10.1227/01.NEU.0000367632.45384.5A. [DOI] [PubMed] [Google Scholar]
- 19.Goel A. Instability and basilar invagination. J Craniovertebr Junction Spine. 2012;3:1–2. doi: 10.4103/0974-8237.110115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kothari M, Goel A. Transatlantic odonto-occipital listhesis: the so-called basilar invagination. Neurol India. 2007;55:6–7. doi: 10.4103/0028-3886.30416. [DOI] [PubMed] [Google Scholar]
- 21.Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated cases. J Neurosurg. 1998;88:962–8. doi: 10.3171/jns.1998.88.6.0962. [DOI] [PubMed] [Google Scholar]
- 22.Henderson FC, Wilson WA, Mott S, Mark A, Schmidt K, Berry JK, et al. Deformative stress associated with an abnormal clivo-axial angle: A finite element analysis. Surg Neurol Int. 2010;1:30. doi: 10.4103/2152-7806.66461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sahuquillo J, Rubio E, Poca MA, Rovira A, Rodriguez-Baeza A, Cervera C. Posterior fossa reconstruction: A surgical technique for the treatment of Chiari I malformation and Chiari I/syringomyelia complex — Preliminary results and magnetic resonance imaging quantitative assessment of hindbrain migration. Neurosurgery. 1994;35:874–84. doi: 10.1227/00006123-199411000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Taricco MA, Melo LR. Retrospective study of patients with Chiari: Malformation submitted to surgical treatment. Arq Neuropsiquiatr. 2008;66:184–8. doi: 10.1590/s0004-282x2008000200008. [DOI] [PubMed] [Google Scholar]
- 25.Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, et al. Chiari I malformation redefined: Clinical and radiographic findings for 364 symptomatic patients. Neurosurgery. 1999;44:1005–17. doi: 10.1097/00006123-199905000-00042. [DOI] [PubMed] [Google Scholar]
- 26.Batzdorf U. Chiari I malformation with syringomyelia. Evaluation of surgical therapy by magnetic resonance imaging. J Neurosurg. 1988;68:726–30. doi: 10.3171/jns.1988.68.5.0726. [DOI] [PubMed] [Google Scholar]


