Abstract
Psychiatric disorders are associated with long-term disability and huge social and economic costs. The possible influence of heavy metals exposure on public health remains a matter of concern. A recurring research question that persisted among researchers in neuropsychiatry has been “are psychiatric patients more likely to have a high body burden of lead or other heavy metals?” This is an update account on the role of lead and cadmium in psychiatry. This review, which has employed search words like “lead and cadmium in psychiatry”, “lead and cadmium in schizophrenia”, “lead and cadmium in psychosis” in citation indices such as PubMed, Google Scholar, Scirus, and Scopus. A total of 415 articles were found; 60 fulfiled the inclusion criteria. Evidence-based information suggests that lead and cadmium may be involved in psychiatry. Should environmental lead and cadmium be implicated in the etiogenesis of psychiatry given the characteristic high environmental pollution in Sub Sahara Africa, it is worthwhile for toxicologists and scientists in Sub-Sahara Africa to investigate if lead and cadmium can become additional biomarkers in the diagnosis of psychiatric disorders.
Keywords: Cadmium, Environmental health, Lead, Psychiatry
Introduction
Neurological diseases and disorders are rarely unidimensional or unifactorial. Even those diseases, whose etiologies seem closely linked to genetic predispositions, tend to be the product of multiple and intertwined risk factors, of which environmental chemical exposures may serve as one component.[1] Psychiatric conditions including madness, mania, melancholia, and schizophrenia spectrum disorders (SSDs) are mental illnesses of unknown etiology, typically diagnosed in adolescence or adulthood. These diseases, which lack definitive curative modality, are frequently associated with long-term disability and huge social and economic costs. According to Freeman (1984), areas with high population densities are associated with higher rates of criminality, mortality, social isolation, air pollution, and noise.[2] Rates of psychiatric disorders seem to correlate with urbanization. Following the Dohrenwend and Dohrenwend contribution on psychiatric disorders in urban settings,[3] other workers have shown higher overall rates in urban areas and specifically, somewhat higher rates for depression.[4,5,6,7,8] The breeder hypothesis assumes that various environmental factors cause illness. Urbanization is modestly but consistently associated with the prevalence of psychopathology.[9] Dekker et al. (2008)[10] confirmed that psychiatric disorders are more common in more urbanized areas in Germany. They opined that the urban-rural differences may be related to environmental risk factors. Van Os et al.[11] found a relation between psychotic symptoms and the lifetime prevalence of psychotic disorders, and between psychotic symptoms and urbanization.
The construct that low level of lead and cadmium exposure can damage the brain and increase the risk of psychiatric disorder — a leading cause of morbidity and disability — is of great concern to overall health. Exposure to lead is widely recognized as a major risk factor for several human diseases, and the structure of industrial ecological systems has made exposure to lead unavoidable for most people alive today.[12] The possible influence of low-level lead and indeed other heavy metals exposure on public health remains a matter of concern. Over thirty years ago, the research question that persisted among researchers in neuropsychiatry was “are psychiatric patients more likely to have a high body burden of lead or other heavy metals?” Although recent findings suggest involvement of toxic heavy metals in psychiatric illness. Research has shown evidence for this notion; however, the exact underlying factors are not fully understood. This is an updated account on the role of lead and cadmium in psychiatry.
An electronic and manual search of the terms search words like “lead and cadmium in psychiatry”, “lead and cadmium in schizophrenia”, “lead and cadmium in psychosis” in citation indices like PubMed, Google Scholar, Scirus, and Scopus. Articles were not discriminated by date of publication. Studies also had to be published in English and conducted with human subjects in most cases.
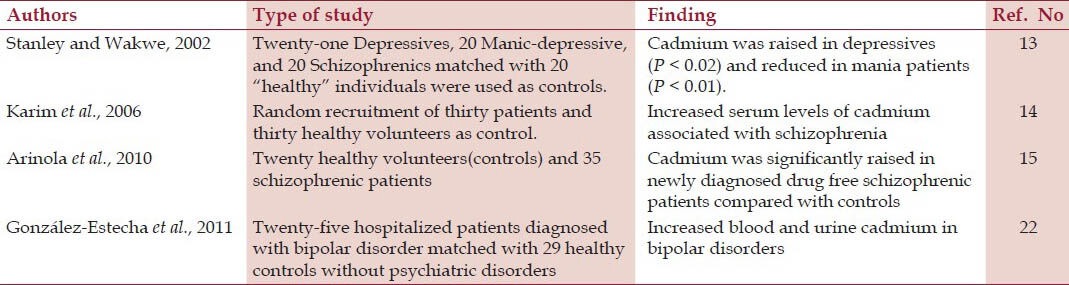
A total of 415 articles were found 60 met the inclusion criteria. Evidence based information suggest that lead and cadmium may be involved in psychiatry. The effects of lead and cadmium in psychiatry are shown on Tables 1 and 2, respectively. Three of these studies namely Stanley and Wakwe,[13] Karim et al.,[14] and Arinola et al.,[15] inspite of the poor record keeping are from developing nations. Various studies[13,14,15,16,17,18,19,20,21,22,23,24] using different research designs have implicated increased bone and blood lead levels with different forms of psychiatric conditions ranging from depression, schizophrenia, bipolar disorder, mood disorders, etc. All the studies associated depression, schizophrenia, and bipolar disorder with significant increases in the body burden of lead except Karim et al.[14] who noted non-significant increase in serum levels of lead in schizophrenia and suggested further studies. Stanley and Wakwe[13] indicated that lead was increased in depressives (P < 0.01) and schizophrenics (P < 0.05) but not in manic patients. Eum et al.[23] found increased depressive symptom scores and high phobic anxiety scores in association with increasing bone lead concentration among middle-age and elderly women. The effect of cadmium in psychiatry tended to follow the same trend with the effect of lead.
Table 1.
Effect of lead in psychiatry
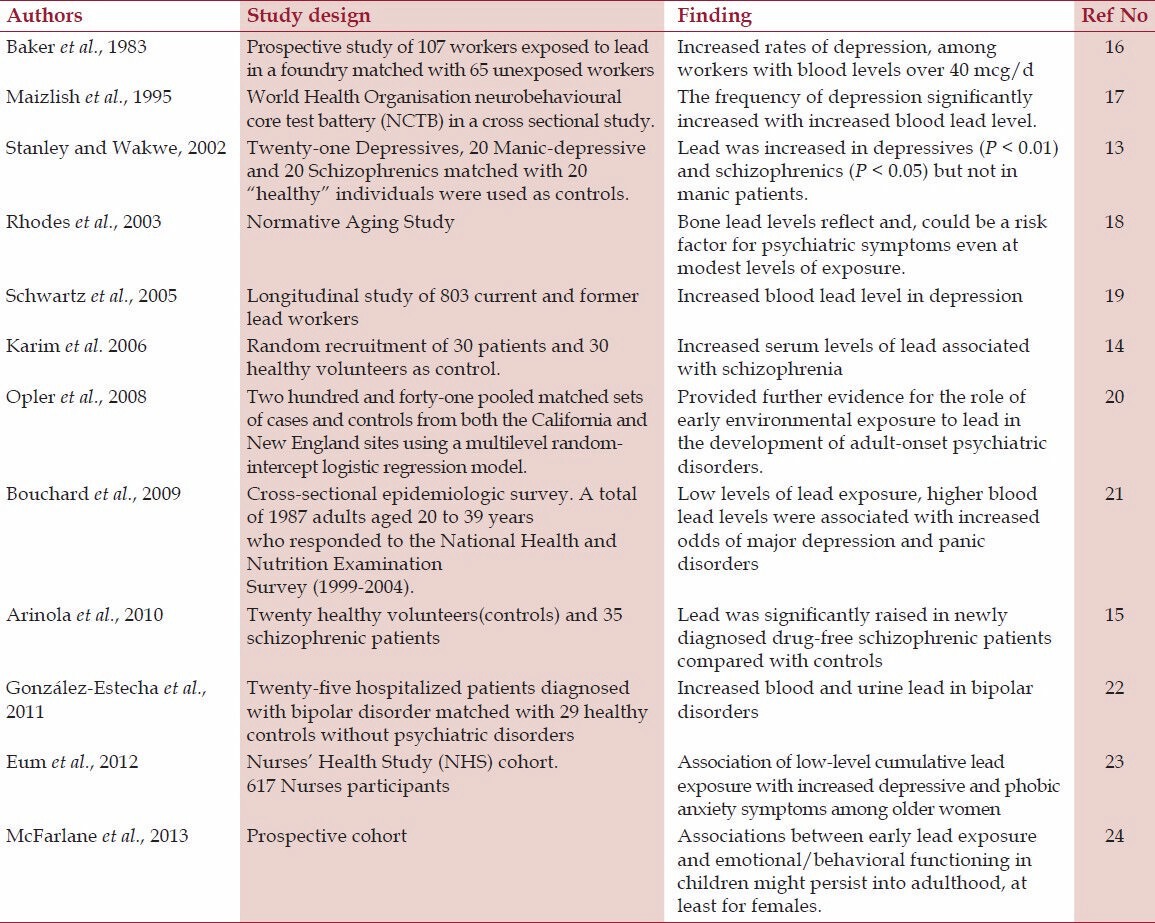
Table 2.
Effect of cadmium in psychiatry
Hanninen et al.[25] found a positive association between lead and depression in agreement with earlier finding among workers with present and past blood lead level <3.4 μmol/l[26] (not shown on the Table). Susser, et al.,[27] found association of exhaust plumes and psychiatry decades after pregnant women were exposed to exhaust plumes at a time lead was used in Callifonia.
The public health burden of psychiatric disorders such as depression and anxiety is tremendous — an estimated 450 million people worldwide suffer from psychiatric disorders.[28] Prenatal and neonatal lead and cadmium exposure have been documented to cause common and widespread neurological and psychological effects including depression, anxiety, mood disorders, schizophrenia, etc.[29] Lead, a potent neurotoxin, may affect numerous cell functions, including the release of neurotransmitters such as dopamine and serotonin.
Opler et al. in a a study of prenatal lead exposure and schizophrenia using the biomarker of exposure δ-aminolevulinic acid in archived maternal serum samples collected from subjects enrolled in the Childhood Health and Development Study (1959-1966) based in California, suggested a possible association between prenatal lead exposure and the development of schizophrenia in later life. Although there were limitations that hampered an outright conclusion in a follow-up investigation in 2008 by the same team, the results provided further evidence for the role of early environmental exposures in the development of adult-onset psychiatric disorders.[20]
Karim et al.[14] reported increased levels of serum cadmium in schizophrenia disordered patients. In the brain lead and cadmium cause lesions including decrease in total cortical volume, white matter,[30] enlargement of cerebroventricular system, changes in gray and white matter and abnormal laminar organization. Various biochemical factors make humans susceptible to neuropsychiatric diseases caused by exposures to a variety of toxic chemicals.[31] It has been postulated that exposure to environmental contaminants may play a role in the development of psychiatric disorder.[32]
The Human Brain and Metallotoxicology
The human brain is susceptible to a variety of toxic chemicals because of natural selection that favors brain structures promoting advanced brain functions such as long-term memory and rapid learning. The high fat content of brain also predisposes it to long-term storage of the same fat soluble toxic chemicals that accumulate in adipose tissue. The high rate of metabolism and high content of polyunsaturated fatty acids also makes it much more susceptible to free radical damage mediated by toxic chemicals, leading to increased damage to brain macromolecules like deoxyribonucleic acid, ribonucleic acid, proteins, cell organelles, and small molecules. The sulfur amino acids are also highest in these brains, making them exquisitely susceptible to exposure to heavy metals. All of these biochemical factors make humans extremely susceptible to neuropsychiatric diseases caused by exposures to a variety of toxic chemicals.[31]
Lead and cadmium in oxidative stress and psychiatry
The mechanism of lead- and cadmium-induced neurotoxicity that lead to neuropsychiatric disorder is not fully understood even in animal studies. However, one developmental hypothesis has it that environmental factors induce pathological changes in the brain before it reaches adult state.[33,34] The pathophysiology of neuropsychiatric disorder is poorly understood, although there is a notion that structural changes occur in the brain of patients with neuropsychiatric disorder. In the brain, lead and cadmium cause lesions including decrease in total cortical volume, white matter[30], enlargement of cerebroventricular system, changes in gray and white matter, and abnormal laminar organization.
González-Estecha et al.[22] finding of increased blood and urine levels of lead and cadmium in bipolar disorder may reflect a high past lead exposure in childhood and adolescence. These increased blood lead levels also indicate that oxidative stress may play a role in the pathophysiology of bipolar disorder, as suggested by a meta-analysis showing that oxidative stress markers are increased in bipolar disorder[35]. In the NHANES 1999-2004 study, persons with blood lead levels in the highest quintile (≥2.1 μg/dL) had a 2.3-fold increased risk of meeting DSM-IV criteria for major depression disorder and a 4.9-fold increased risk of panic disorder as those in the lowest quintile (0.7 μg/dL)[21].
The most likely mechanism of lead could be explained, at least in part, by some in vivo studies that suggest that lead exposure causes generation of reactive oxygen species and alteration of antioxidant defense systems[36]. Lead and cadmium have a high affinity for sulfhydryl groups[37]. Some antioxidants, such as N-Acetyl Cysteine (NAC) chelate lead and remove it from the bloodstream[38]. Reducing blood lead levels in bipolar disorder may contribute to an improvement in symptoms in bipolar disorder.
As for cadmium, González-Estecha et al.[22] observed a statistically significant increase in the bipolar group with respect to the control group. González-Estecha et al.[22] observed an increase in blood cadmium levels in manic phase patients compared to depressive phase patients. An association of lead and cadmium with homocysteine was observed in the NHANES 1999-2002 study as well as in other studies.[39,40] While lead and cadmium may affect homocysteine levels, it is also possible that homocysteine affects blood lead or cadmium levels.[39,40]
Lead and cadmium in mitochondrial dysfunction and psychiatric disorders
In patients with mitochondrial diseases, psychiatric symptoms have been reported. Fattal et al.[41] recorded 19 cases of mitochondrial diseases with comorbid psychiatric problems, including bipolar disorder, major depressive disorder, psychosis, anxiety disorders, and personality changes.
Lead and cadmium disrupt mitochondrial functions through many processes leading to energy metabolism and malfunctions in mitochondrial biochemical cascade, as suggested by several studies on the pathophysiology of bipolar disorder, major depressive disorder, and schizophrenia.[34,41,42,43] There is a correlation between mitochondrial dysfunction and psychiatric disorders. Evidence include impaired energy metabolism in the brain detected using results of magnetic resonance spectroscopy and electron microscopy, co-morbidity with mitochondrial disease, increased mitochondrial DNA (mtDNA) deletion in the brain, and association with mtDNA mutation/polymorphisims of nuclear-encoded mitochondrial genes.[44] Lead is asociated with significant loss in adult gray matter volume of the prefrontal cotex and the anterior cingulate cortex that control executive function, mood regulation, and decision-making. It is suggested that these atrophic changes may be the basis for cognitive and behavioral impairments associated with lead childhood exposure.
Lead and cadmium in neurochemical and hypothalamic — pituitary — adrenal (HPA) axis
In their study on “Childhood and Adult Socioeconomic Position, Cumulative Lead Levels, and Pessimism in Later Life”, Peters et al.[45] found no direct correlation between lead and depression, but an indirect correlation was found through lead's association with pessimism. This observation is congruent with other studies that found an association between cumulative low lead level and depression.
The etiologic mechanisms underpinning lead and emotional processing have not been fully elucidated.[46] It is not clear if psychological problems are caused directly by lead-induced brain damage or are secondary to conditions surrounding its effect on cognitive performance.[47] Lead is believed to affect the brain systems that regulate social/emotional functioning.[47] Physiologically, lead may alter the functioning of the hypothalamic-pituitary-adrenal (HPA) axis either directly or indirectly, the latter mediated by inducing alterations in neurochemical function.[48] Lead tends to interfere with the release of neurotransmitters by mimicking or inhibiting calcium-mediated processes.[48,49,50,51] Lead exposure is of particular interest because it is an established neurotoxin[52] with known effects on several brain systems implicated in depression and anxiety, including monoaminergic signaling[48] and the HPA axis.[48,53] Animal studies have demonstrated that lead exposure affects the hypothalamic-pituitary-adrenal (HPA) axis and can lead to permanent HPA axis dysfunction.[48,54,55] Cory- Slechta and colleagues proposed that alterations in the HPA axis due to lead exposure result in changes in glucocorticoid and catecholamine levels, with neuropsychiatric disorders such as depression as potential consequences.[53] Furthermore, lead affects levels and metabolism of serotonin,[54] and abnormalities in the serotonergic system are present in depression.[56] Lead also affects the mesocorticolimbic system[54], aberrances in which have also been linked to depression.[57,58]
In Nigeria, Lead and cadmium were found to be significantly increased in newly diagnosed drug-free schizophrenic patients compared with controls according to Arinola et al. (2010)[15]. Thus, a mechanism that will decrease blood lead level may be helpful in the management of schizophrenia[15]. González-Estecha et al.[22] found high blood lead levels in bipolar patients. It is speculated that reducing blood lead levels in psychiatric patients may contribute to an improvement in symptoms in psychiatric disorders. Hence, the strong association between high blood lead levels seen in aforementioned studies with schizophrenia, bipolar disorder, and mania should be noted and further investigations should be carried out, especially with the suggestion made by the Kanofsky and co-workers[59] that in some susceptible individuals—people predisposed to bipolar illness—a relatively high lead burden can tip their balance towards illness.
Taken together, toxic heavy metals are found in the air we breathe, the food we eat, and the houses we live in. Toxic metal exposure can result in a wide array of common mental health disorders that may mimic many psychiatric “diseases” and thus lead to psychoactive prescription drug use or other unnecessary treatments. Many people are exposed to environmental lead in SSA. Attention should be given by practitioners to correctly diagnose lead-induced disorders manifesting themselves as neuropsychiatric illness. Since studies have shown that many of these complaints tended to be reversed on removal from lead exposure, attention should be given to a patient's work situation and detailed occupational history should be obtained that will identify practices resulting in lead exposure.
Unfortunately, the majority of clinicians dealing with patients who have mental health issues are unlikely to suspect heavy metal toxicity as a cause of their patient's problems due to a general lack of knowledge regarding this subject in the medical community. Unique biochemical, genetic, and nutritional factors can make certain people more susceptible to the effects of toxic heavy metals; thus, each case must be handled on an individual basis.
Although the number of practitioners trained in “functional” or “orthomolecular” medicine is increasing and these practitioners are very familiar with the diagnosis and treatment of problems associated with heavy metal toxicity[60], the case in developing nations is the opposite.
Recommendation
The none recognition of psychiatric disorders and their severity carries an enormous economic and social burden in the developing world especially Sub Saharan Africa SSA where the prevalence rates are feared to be higher than previously thought. Should environmental lead and cadmium be implicated in the etiogenesis of psychiatry given the characteristic high environmental pollution in SSA, it is worthwhile for toxicologists and scientists in SSA to investigate if lead and cadmium can become additional biomarkers in the diagnosis of psychiatric disorders.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Weiss B, Cory-Slechta D, Gilbert SG, Mergler D, Miller E, Miller C, et al. The new tapestry of risk assessment. Neurotoxicology. 2008;29:883–90. doi: 10.1016/j.neuro.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freeman H. 1st ed. London: Churchill Livingstone; 1984. Mental health and the environment. [Google Scholar]
- 3.Dohrenwend BP, Dohrenwend BS. Psychiatric disorders in urban settings. In: Caplan G, editor. American Handbook of Psychiatry. New York: Basic Books; 1974. pp. 424–47. [Google Scholar]
- 4.Mueller DP. The current status of urban-rural differences in psychiatric disorder: An emerging trend for depression. J Nerv Ment Dis. 1981;169:18–27. doi: 10.1097/00005053-198101000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Marsella AJ. Urbanization, mental health, and social deviancy. A review of issues and research. Am Psychol. 1998;53:624–34. doi: 10.1037//0003-066x.53.6.624. [DOI] [PubMed] [Google Scholar]
- 6.Neff JA. Urbanicity and depression reconsidered. The evidence regarding depressive symptomatology. J Nerv Ment Dis. 1983;171:546–52. doi: 10.1097/00005053-198309000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Verheij RA. Explaining urban-rural variations in health: A review of interactions between individual and environment. Soc Sci Med. 1996;42:923–35. doi: 10.1016/0277-9536(95)00190-5. [DOI] [PubMed] [Google Scholar]
- 8.Webb SD. Rural-urban differences in mental health. In: Freeman H, editor. Mental health and the environment. London: Churchill Livingstone; 1984. pp. 227–49. [Google Scholar]
- 9.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiat Scand. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- 10.Dekker J, Peen J, Koelen J, Smit F, Schoevers R. Psychiatric disorders and urbanization in Germany BMC Public Health. 2008;8:17. doi: 10.1186/1471-2458-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Os J, Hanssen M, Bijl RV, Vollebergh W. Prevalence of psychotic disorder and community level of psychotic symptoms: An urban-rural comparison. Arch Gen Psychiatry. 2001;58:663–8. doi: 10.1001/archpsyc.58.7.663. [DOI] [PubMed] [Google Scholar]
- 12.Pruss-Ustun A, Fewtrell L, Landrigan PJ, Ayuso-Mateos JL. Lead Exposure. In: Lopez AD, Rodgers A, Murray CJ, editors. Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors. Geneva: World Health Organization; 2004. pp. 1495–552. [Google Scholar]
- 13.Stanley PC, Wakwe VC. Toxic trace metals in the mentally ill patients. Niger Postgrad Med J. 2002;9:199–204. [PubMed] [Google Scholar]
- 14.Karim P, Hossain MI, Nazmus Sadat AF, Nahar Z, Md Khalid Hossain MK, Hasnat A. Serum levels of cadmium, calcium, lead and iron in schizophrenic patients. Dhaka Univ J Pharm Sci. 2006;5:9–13. [Google Scholar]
- 15.Arinola G, Idonije B, Akinlade K, Ihenyen O. Essential trace metals and heavy metals in newly diagnosed schizophrenic patients and those on anti-psychotic medication. J Res Med Sci. 2010;15:245–9. [PMC free article] [PubMed] [Google Scholar]
- 16.Baker EL, Feldman RG, White RF, Harley JP. The role of occupational lead exposure in the genesis of psychiatric and behavioral disturbances. Acta Psychiatr Scand Suppl. 1983;303:38–48. doi: 10.1111/j.1600-0447.1983.tb00940.x. [DOI] [PubMed] [Google Scholar]
- 17.Maizlish NA, Parra G, Feo O. Neurobehavioural evaluation of Venezuelan workers exposed to inorganic lead. Occup Environ Med. 1995;52:408–14. doi: 10.1136/oem.52.6.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rhodes D, Spiro A, 3rd, Aro A, Hu H. Relationship of bone and blood lead levels to psychiatric symptoms: The normative aging study. J Occup Environ Med. 2003;45:1144–51. doi: 10.1097/01.jom.0000094995.23808.7b. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz BS, Lee BK, Bandeen-Roche K, Stewart W, Bolla K, Links J, et al. Occupational lead exposure and longitudinal decline in neurobehavioral test scores. Epidemiology. 2005;16:106–13. doi: 10.1097/01.ede.0000147109.62324.51. [DOI] [PubMed] [Google Scholar]
- 20.Opler MG, Buka SL, Groeger J, McKeague I, Wei C, Factor-Litvak P, et al. Prenatal exposure to lead, delta-aminolevulinic acid, and schizophrenia: Further evidence. Environ Health Perspect. 2008;116:1586–90. doi: 10.1289/ehp.10464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bouchard MF, Bellinger DC, Weuve J, Matthews-Bellinger J, Gilman SE, Wright RO, et al. Blood lead levels and major depressive disorder, panic disorder, and generalized anxiety disorder in US young adults. Arch Gen Psychiatry. 2009;66:1313–9. doi: 10.1001/archgenpsychiatry.2009.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.González-Estecha M, Trasobares EM, Tajima K, Cano S, Fernández C, López JL, et al. Trace elements in bipolar disorder. J Trace Elem Med Biol. 2011;25(Suppl 1):S78–83. doi: 10.1016/j.jtemb.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 23.Eum KD, Korrick SA, Weuve J, Okereke O, Kubzansky LD, Hu H, et al. Relation of cumulative low-level lead exposure to depressive and phobic anxiety symptom scores in middle-age and elderly women. Environ Health Perspect. 2012;120:817–23. doi: 10.1289/ehp.1104395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McFarlane AC, Searle AK, Van Hooff M, Baghurst PA, Sawyer MG, Galletly C, et al. Prospective associations between childhood low-level lead exposure and adult mental health problems: The port pirie cohort study. Neurotoxicology. 2013;39:11–7. doi: 10.1016/j.neuro.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 25.Hänninen H, Aitio A, Kovala T, Luukkonen R, Matikainen E, Mannelin T, et al. Occupational exposure to lead and neuropsychological dysfunction. Occup Environ Med. 1998;55:202–9. doi: 10.1136/oem.55.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanninen H, Mantere P, Hernberg S, Seppalainen AM, Kock B. Subjective symptoms in low-level exposure to lead. Neurotoxicology. 1979;1:333–47. [Google Scholar]
- 27.Susser ES, Brown AS, Gorman JM. Washington: American Psychiatric Press; 1999. Prenatal Exposures in Schizophrenia; pp. 89–112. [Google Scholar]
- 28.World Health Organization. Mental Health: New Understanding. Geneva: New Hope; 2001. The World Health Report. [Google Scholar]
- 29.Arena JM, Drew RN. Toxicology-Symptoms-Treatment, Fifth Edition. 3rd Ed. Charles C. Thomas-Publisher, Springfield Il, 1986; & Merritt's Textbook of Neurology. 9th Ed., Williams and Wilkins, Baltimore & Clinical Management of Poisoning; 1995. Poisoning 1995; p. 753. [Google Scholar]
- 30.van der Schot AC, Vonk R, Brans RG, van Haren NE, Koolschijn PC, Nuboer V, et al. Influence of genes and environment on brain volumes in twin pairs concordant and discordant for bipolar disorder. Arch Gen Psychiatry. 2009;66:142–51. doi: 10.1001/archgenpsychiatry.2008.541. [DOI] [PubMed] [Google Scholar]
- 31.Shaw W. The unique vulnerability of the human brain to toxic chemical exposure and the importance of toxic chemical evaluation and treatment in orthomolecular psychiatry. J Orthomol Med. 2010;25:125–34. [Google Scholar]
- 32.Shih RA, Hu H, Weisskopf MG, Schwartz BS. Cumulative lead dose and cognitive function in adults: A review of studies that measured both blood lead and bone lead. Environ Health Perspect. 2007;115:483–92. doi: 10.1289/ehp.9786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rapoport JL, Addington AM, Frangou S, Psych MR. The neurodevelopmental model ofschizophrenia: Update 2005. Mol Psychiatry. 2005;10:434–49. doi: 10.1038/sj.mp.4001642. [DOI] [PubMed] [Google Scholar]
- 34.Rapoport JL, Giedd JN, Gogtay N. Neurodevelopmental model of schizophrenia: Update 2012. Mol Psychiatry. 2012;17:1228–38. doi: 10.1038/mp.2012.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Andreazza AC, Kauer-Sant’Anna M, Frey BN, Bond DJ, Kapczinski F, Young LT, et al. Oxidative stress markers in bipolar disorder: A meta-analysis. J Affect Disord. 2008;111:135–44. doi: 10.1016/j.jad.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 36.Vaziri ND. Mechanisms of lead-induced hypertension and cardiovascular disease. Am J Physiol Heart Circ Physiol. 2008;295:H454–65. doi: 10.1152/ajpheart.00158.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hsu PC, Guo YL. Antioxidant nutrients and lead toxicity. Toxicology. 2002;180:33–44. doi: 10.1016/s0300-483x(02)00380-3. [DOI] [PubMed] [Google Scholar]
- 38.Gurer H, Ercal N. Can antioxidants be beneficial in the treatment of lead poisoning? Free Radic Biol Med. 2000;29:927–45. doi: 10.1016/s0891-5849(00)00413-5. [DOI] [PubMed] [Google Scholar]
- 39.Schafer JH, Glass TA, Bressler J, Todd AC, Schwartz BS. Blood lead is a predictor of homocysteine levels in a population-based study of older adults. Environ Health Perspect. 2005;113:31–5. doi: 10.1289/ehp.7369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guallar E, Silbergeld EK, Navas-Acien A, Malhotra S, Astor BC, Sharrett AR, et al. Confounding of the relation between homocysteine and peripheral arterial disease by lead, cadmium and renal function. Am J Epidemiol. 2006;163:700–8. doi: 10.1093/aje/kwj090. [DOI] [PubMed] [Google Scholar]
- 41.Fattal O, Budur K, Vaughan AJ, Franco K. Review of the literature on major mental disorders in adult patients with mitochondrial diseases. Psychosomatics. 2006;47:1–7. doi: 10.1176/appi.psy.47.1.1. [DOI] [PubMed] [Google Scholar]
- 42.Tosic M, Ott J, Barral S, Bovet P, Deppen P, Gheorghita F, et al. Schizophrenia and oxidative stress: Glutamate cysteine ligase modifier as a susceptibility gene. Am J Hum Genet. 2006;79:586–92. doi: 10.1086/507566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sarandol A, Sarandol E, Eker SS, Erdinc S, Vatansever E, Kirli S. Major depressive disorder is accompanied with oxidative stress: Short-term antidepressant treatment does not alter oxidative-antioxidative systems. Hum Psychopharmacol. 2007;22:67–73. doi: 10.1002/hup.829. [DOI] [PubMed] [Google Scholar]
- 44.Jou SH, Chiu NY, Liu CS. Mitochondrial dysfunction and psychiatric disorders. Chang Gung Med J. 2009;32:370–9. [PubMed] [Google Scholar]
- 45.Peters JL, Kubzansky LD, Ikeda A, Spiro A, 3rd, Wright RO, Weisskopf MG, et al. Childhood and adult socioeconomic position, cumulative lead levels, and pessimism in later life: The VA Normative Aging Study. Am J Epidemiol. 2011;174:1345–53. doi: 10.1093/aje/kwr269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rajan P, Kelsey KT, Schwartz JD, Bellinger DC, Weuve J, Sparrow D, et al. Lead burden and psychiatric symptoms and the modifying influence of the delta-aminolevulinic acid dehydratase (ALAD) polymorphism: The VA Normative Aging Study. Am J Epidemiol. 2007;166:1400–8. doi: 10.1093/aje/kwm220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lidsky TI, Schneider JS. Lead neurotoxicity in children: Basic mechanisms and clinical correlates. Brain. 2003;126:5–19. doi: 10.1093/brain/awg014. [DOI] [PubMed] [Google Scholar]
- 48.Virgolini MB, Chen K, Weston DD, Bauter MR, Cory-Slechta DA. Interactions of chronic lead exposure and intermittent stress: Consequencesfor brain catecholamine systems and associated behaviours and HPA axis function. Toxicol Sci. 2005;87:469–82. doi: 10.1093/toxsci/kfi269. [DOI] [PubMed] [Google Scholar]
- 49.Cory-Slechta DA, Garcia-Osuna M, Greenamyre JT. Lead induced changes in NMDA receptor complex binding: Correlations with learning accuracy and with sensitivity to learning impairments caused by MK-801 and NMDA administration. Behav Brain Res. 1997;85:161–74. doi: 10.1016/s0166-4328(96)00174-x. [DOI] [PubMed] [Google Scholar]
- 50.Wright RO, Tsaih SW, Schwartz J, Spiro A, 3rd, McDonald K, Weiss ST, et al. Lead exposure biomarkers and mini-mental status exam scores in older men. Epidemiology. 2003;14:713–8. doi: 10.1097/01.EDE.0000081988.85964.db. [DOI] [PubMed] [Google Scholar]
- 51.Weisskopf MG, Proctor SP, Wright RO, Schwartz J, Spiro A, 3rd, Sparrow D, et al. Cumulative lead exposure and cognitive performance among elderly men. Epidemiology. 2007;18:59–66. doi: 10.1097/01.ede.0000248237.35363.29. [DOI] [PubMed] [Google Scholar]
- 52.Bressler J, Kim KA, Chakraborti T, Goldstein G. Molecular mechanisms of lead neurotoxicity. Neurochem Res. 1999;24:595–600. doi: 10.1023/a:1022596115897. [DOI] [PubMed] [Google Scholar]
- 53.Cory-Slechta DA, Virgolini MB, Rossi-George A, Thiruchelvam M, Lisek R, Weston D. Lifetime consequences of combined maternal lead and stress. Basic Clin Pharmacol Toxicol. 2008;102:218–27. doi: 10.1111/j.1742-7843.2007.00189.x. [DOI] [PubMed] [Google Scholar]
- 54.Cory-Slechta DA, Virgolini MB, Thiruchelvam M, Weston DD, Bauter MR. Maternal stress modulates the effects of developmental lead exposure. Environ Health Perspect. 2004;112:717–30. doi: 10.1289/ehp.6481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rossi-George A, Virgolini MB, Weston D, Cory-Slechta D. A Alterations in glucocorticoid negative feedback following maternal Pb, prenatal stress and the combination: A potential biological unifying mechanism for their corresponding disease profiles. Toxicol Appl Pharmacol. 2009;234:117–27. doi: 10.1016/j.taap.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Moore DP, Jefferson JW. handbook of medical psychiatry. Philadelphia: Mosby Inc; 2004. Major depressive disorder (DSM-IVTR #296.2-296.3) handbook of medical psychiatry; pp. 89–112. [Google Scholar]
- 57.Martin-Soelch C. Is depression associated with dysfunction of the central reward system? Biochem Soc Trans. 2009;37:313–7. doi: 10.1042/BST0370313. [DOI] [PubMed] [Google Scholar]
- 58.Naranjo CA, Tremblay LK, Busto UE. The role of the brain reward system in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2001;25:781–823. doi: 10.1016/s0278-5846(01)00156-7. [DOI] [PubMed] [Google Scholar]
- 59.Kanofsky JD, Rosen WA, Ryan PB, Decina P, Fieve RR, Kanofsky PB. Lead levels in the hair of bipolar patients and normal controls. Med Hypotheses. 1986;20:151–5. doi: 10.1016/0306-9877(86)90121-0. [DOI] [PubMed] [Google Scholar]
- 60.Heavy Metal Toxicity. 2011. [Last accessed on 2013 Jul 14]. Available from: at http://www.lef.org/


