Abstract
Background
Primary pancreatic lymphoma is a rare tumour of the pancreas. Data on the role of endoscopic ultrasound guided fine needle aspiration for its diagnosis are scant.
Aim
To identify the frequency of occurrence, sonographic characteristics and cytological findings that are predictive of primary pancreatic lymphoma.
Methods
Pancreatic lymphoma cases were identified by retrospective review of solid pancreatic masses over 10-year period.
Results
12/2397 (0.5%) lesions were identified. Patients were predominantly white (92%) and male (58%). Mean largest dimension was 47.5 mm and 83.3% were located in the head. The mass appeared heterogeneous in 75% and peripancreatic lymphadenopathy was noted in 58%. None of the patients showed features of chronic pancreatitis or pancreatic ductal dilation. Rapid onsite analysis revealed atypical lymphocytes in 92%. Flow cytometry confirmed diagnosis in 75% of cases.
Conclusions
Primary pancreatic lymphoma is encountered in 0.5% of patients undergoing endoscopic ultrasound guided fine needle aspiration. A large heterogeneous mass, in the absence of chronic pancreatitis or pancreatic duct dilation that reveals atypical lymphocytes on fine needle aspiration is suggestive.
Keywords: EUS, Primary pancreatic lymphoma, EUS-FNA, Flow cytometry
1. Introduction
In the United States, it is estimated that 45,220 cases of pancreatic cancer will be diagnosed in 2013 with an estimated death in 38,460 individuals [1] more commonly from adenocarcinoma. However, solid pancreatic masses identified on imaging vary from adenocarcinoma in 85% to mass forming autoimmune pancreatitis, primary pancreatic lymphoma (PPL), neuroendocrine tumours and complex pancreatic cyst neoplasms. While the latter conditions are rare, treatment outcomes are vastly different.
Pancreatic involvement in lymphoma can be due to peripancreatic lymph node mass causing direct invasion of the parenchyma; intrinsic pancreatic mass lesion with or without discrete peripancreatic lymphadenopathy or secondary extranodal deposit [2]. Widely accepted criteria for diagnosis of PPL are (a) mass involving the pancreas with or without loco-regional lymph nodes, (b) absence of superficial/mediastinal lymph nodes, (c) absence of hepatic or splenic involvement and (d) normal leucocyte count [3]. Although previous history of haematological malignancy, young age, presence of B symptoms (fever, night sweats and weight loss), large size tumour, low CA19-9 level and absence of jaundice or diabetes mellitus are shown to indicate haematological malignancy in the pancreas [4], tissue diagnosis is imperative for appropriate treatment given the differing outcomes of therapy for these conditions.
EUS-FNA with its very high sensitivity and specificity has taken a central role in the management algorithm of solid pancreatic masses [5]. The objective of this study is to identify the frequency of occurrence, endosonographic characteristics and cytological findings of PPL in patients undergoing endoscopic ultrasound guided fine needle aspiration (EUS-FNA) of solid pancreatic masses.
2. Materials and methods
This study was executed by reviewing the Institutional Review Board approved database of all patients who underwent EUS-FNA of solid pancreatic masses over a period of 10 years. The data extracted included findings at EUS, rapid on site cytopathology evaluation (ROSE) and final diagnosis. Criteria for inclusion in the study were solid pancreatic masses and a final diagnosis of PPL. Excluded from analysis were pancreatic or retroperitoneal lymph node masses that were adherent or adjacent to the pancreas.
EUS was performed under moderate sedation after administration of intravenous meperidine, midazolam and diazepam using a linear array echoendoscope (Olympus UCT140, Olympus America Corp, Center Valley, PA). When a mass was identified, its size, echo features, involvement of adjacent vasculature, and presence of peripancreatic lymph nodes was documented. Fine needle aspiration (FNA) of the mass was performed with a standard FNA needle (Echotip, Cook Endoscopy, Winston-Salem, NC, USA; Expect™, Boston Scientific Corporation, Natick, MA, USA), the needle size was determined by endosonographer preference. ROSE was undertaken of air-dried smears with Diff-Quick staining (Dade Diagnostics, Miami, FL, USA) and additional FNA passes were made for flow cytometry or other ancillary studies as determined by the onsite cytopathologist. The number of passes required to establish onsite preliminary assessment was documented. Patients were then recovered in the endoscopy unit and discharged when stable. Follow-up telephone call was made 24 h after the procedure to assess for delayed complications.
2.1. Statistical analysis
The baseline characteristics of patients were summarized as median, interquartile range for continuous variables such as age, size and number of passes with the FNA needle. Categorical variables such as gender, race, clinical symptoms, were on the other hand expressed as frequencies and proportions. Procedure details including echo characteristics; pancreatic parenchymal appearance; calibre of pancreatic duct; presence or absence of peripancreatic lymphadenopathy was summarized. The frequency of occurrence of primary pancreatic lymphoma was determined with the denominator of the total number of EUS-FNA of solid pancreatic lesions and 95% confidence interval of population proportion was then calculated. The datasets were compiled using Microsoft Excel and SAS software, version 93 (SAS institute, Cary, NC, USA) was used to perform the analysis.
3. Results
3.1. Patient demographics and clinical details
Of 2397 patients who underwent EUS-FNA of solid pancreatic masses over the study period, 21 were identified to have a diagnosis of lymphoma. In 9/21 patients, there was ambiguity regarding the origin of the tumour mass at EUS, these were classified as secondary pancreatic lymphoma and excluded from the analysis. The remaining 12 patients were categorized to have PPL and constituted the study cohort. The frequency of PPL occurrence was 0.5% [95% CI 0.22–0.78]. Majority of patients were male (58.3%) and Caucasian (91.7%) with a median age of 65.5 years (IQR = 41–89). Clinical presentation included abdominal pain (91.7%), jaundice (25%), weight loss (16.7%), nausea and vomiting (8.3%) and B-grade symptoms (8.3%). One patient had a prior diagnosis of AIDS. All patients had identifiable mass lesions on CT scan.
3.2. EUS features
The mean largest dimension of the mass was 47.5 mm (SD = 21) and more than 80% were located in the head region with one each in the body and tail of pancreas. Echo features were heterogeneous 75% while the rest were uniformly hypoechoic. The margins were ill defined in all patients and vascular invasion was noted in 41.7%. The rest of the pancreatic parenchyma was unremarkable without features of chronic pancreatitis. The main pancreatic duct was not dilated in any patient and peripancreatic lymphadenopathy was noted in 58.3% (Table 1).
Table 1.
Endosonographic features, fine needle aspiration and final flow cytometry analysis of the study group (N = 12).
| Maximum size (mm) | Mean 47.5, SD: 21 |
|---|---|
| Number of passes | Median = 4, IQR = 1 – 6 |
| Location | |
| Head | 10 (83.4%) |
| Body | 1 (8.3%) |
| Tail | 1 (8.3%) |
| Vascular invasion | |
| Yes | 5 (41.7%) |
| None | 7 (58.3%) |
| EUS features | |
| Heterogeneous | 9 (75%) |
| Hypoechoic | 3 (25%) |
| Peripancreatic LN | |
| Yes | 7 (58.3%) |
| No | 5 (41.7%) |
| Dilated pancreatic duct | |
| Yes | 0 |
| None | 12 (100%) |
| ROSE | |
| Numerous lymphocytes | 9 (75%) |
| Atypical lymphocytes | 2 (16.7%) |
| Necrosis | 1 (83%) |
| Flow cytometry | |
| Conclusive | 9 (75%) |
| Inconclusive | 3 (25%) |
| Adequacy of material | |
| Yes | 9 (75%) |
| No | 3 (25%) |
| Repeat EUS | |
| Yes | 3 (25%) |
| No | 9 (75%) |
| Open biopsy | |
| Yes | 3 (25%) |
| No | 9 (75%) |
LN: lymph node; EUS: endoscopic ultrasound; ROSE: rapid on-site cytopathology diagnosis; SD: standard deviation; IQR: inter-quartile range.
3.3. Fine needle aspiration
FNA was performed with 22G needle in 833% and with 25G in others. One patient underwent EUS-FNA using a 19G needle following a failed procedure using a 22G needle. Median number of passes was four (IQR 1–6). Rapid onsite cytopathology revealed numerous atypical lymphocytes (Figs. 1 and 2) in 91.7% with one other showing necrosis. Flow cytometry confirmed lymphoma in 9 patients (75%). Three patients underwent repeat EUS-FNA with flow cytometry that was inconclusive; surgical biopsy established a definitive diagnosis of lymphoma in these patients. No complications were encountered with EUS-FNA.
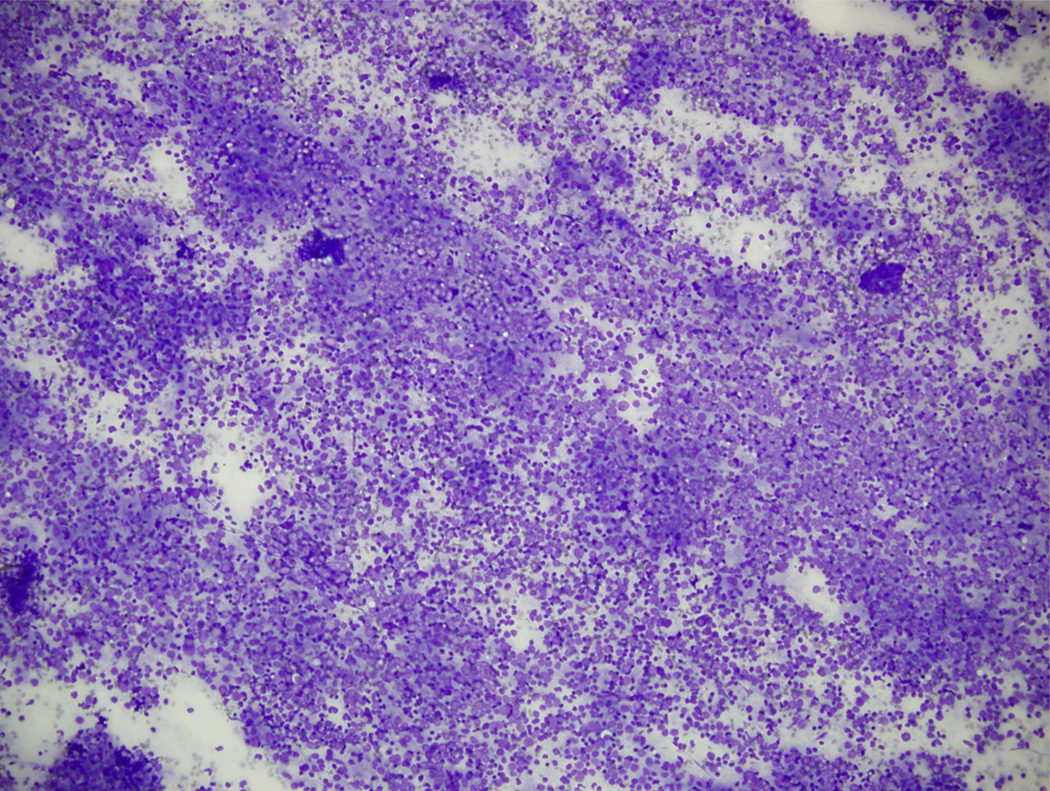
Fig. 1.
Low power (×10) rapid onsite evaluation reveals predominant distribution of atypical lymphocytes throughout field.
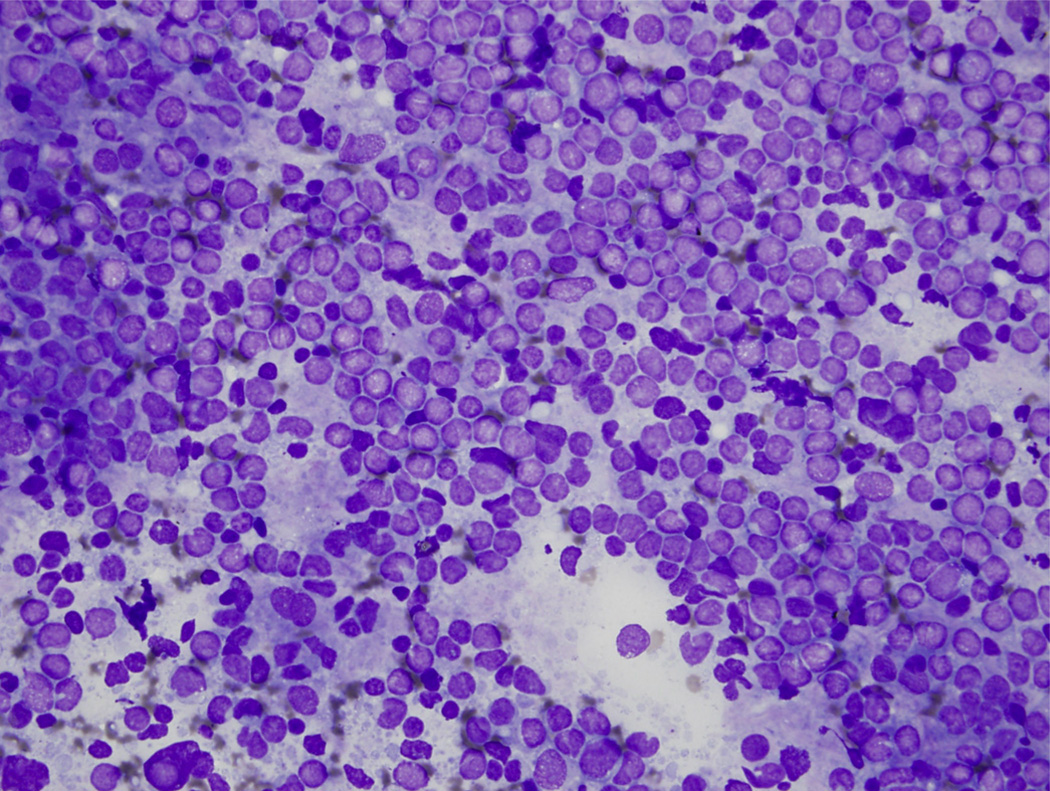
Fig. 2.
High power view (×40) shows numerous large monotonous lymphocytes with open chromatin admixed with small, dark, round, mature lymphocytes.
3.4. Final diagnosis and outcome
Eight of 12 patients (67%) were classified as Large B cell lymphoma, 3 (25%) as non-Hodgkin’s lymphoma, and one as small cell lymphocytic lymphoma. Except for one patient, all others underwent chemotherapy. At a median follow-up of 42 months (range, 13–84), one patient died of natural causes, six were in remission and others were lost to follow up.
4. Discussion
Pancreatic lymphoma can arise from the parenchyma or could be an extension from peripancreatic or retroperitoneal lymph node mass, making diagnosis by imaging difficult [6]. We used stringent criteria and excluded those lesions where there was ambiguity regarding the origin of the lesion, therefore, this constitutes a select cohort of patients with discrete pancreatic masses.
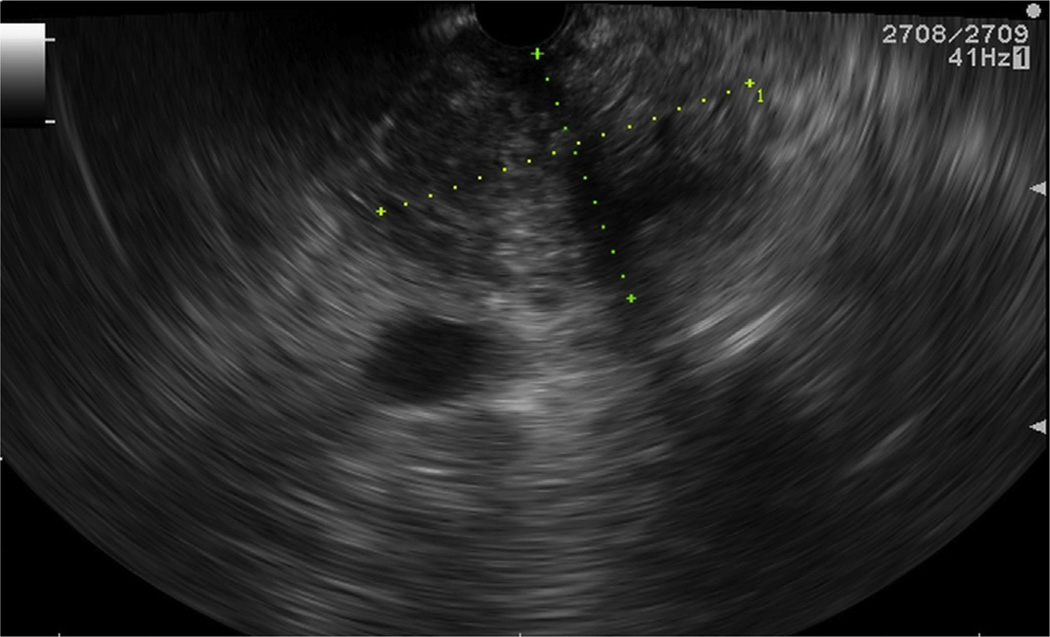
Our findings demonstrate that the echo features of the mass were predominantly heterogeneous (Fig. 3) with preponderance for the head of pancreas. While a prior study observed that a large, hypoechoic, pancreatic head mass on EUS was a feature of lymphoma, no other additional findings suggestive of PPL was reported [7]. A characteristic finding in our series was the lack of pancreatic ductal dilation in the presence of a large pancreatic head mass. This finding has been documented in two cross-sectional imaging studies where the pancreatic ductal diameter were reported to be minimally enlarged with the ratio of ductal diameter to width of the gland being <0.5 [8, 9]. Our study reaffirms these findings, as lymphomatous deposits arising within the pancreatic parenchyma pushes the pancreatic duct unlike ductal carcinoma that blocks the duct causing dilation.
Fig. 3.
Linear echoendoscopic view of heterogeneous pancreatic head mass.
Our study confirms the value of ROSE for preliminary evaluation of solid pancreatic masses. When a solid pancreatic mass is sampled at EUS and if preliminary assessment reveals a preponderance of atypical lymphoid cells without malignant or atypical ductal/acinar cells, then the probability of PPL must be strongly considered. In the absence of ROSE, however, a large heterogeneous mass with no evidence of ductal dilation should alert the endosonographer towards the possibility of lymphoma and additional FNA passes must be performed for flow cytometry and other ancillary studies. Although a core biopsy may be useful to establish a histological diagnosis in such a scenario, its utility was not evaluated in this study. In two prior reports, the addition of flow cytometry improved the diagnostic accuracy of cytology from 44 to 86% and from 267 to 867%, respectively [10, 11]. In the present study, flow cytometry established a diagnosis in 75% of cases.
The limitations of this study include its retrospective design and its inherent pitfalls. Moreover, this is a small series from a tertiary centre that reflects the rarity of this condition. In three patients with inconclusive diagnosis who underwent repeat EUS-FNA and eventually an open surgical biopsy, the use of a 19G or a dedicated core biopsy needle may have established a diagnosis. Presently, we use the 19G needle to procure specimen for flow cytometry when a diagnosis of PPL is suspected. Also, we do not have clinical follow-up on all patients as they were referred back to outside facilities for subsequent chemotherapy.
In conclusion, our study demonstrates that the presence of a large heterogeneous mass lesion in the head of pancreas without associated features of chronic pancreatitis or pancreatic ductal dilation that on ROSE reveals abundant atypical lymphocytes is suggestive of primary pancreatic lymphoma. EUS-FNA with flow cytometry establishes a definitive diagnosis in the majority of patients.
Footnotes
Conflict of interest statement
Jayapal Ramesh, Shantel Hebert-Magee, Hwasoon Kim, Jessica Trevino had no conflict of interest. Shyam Varadarajulu is a Consultant for Olympus America and Boston Scientific Corporation.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA: A Cancer Journal for Clinicians. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 2.Zucca E, Roggero E, Bertoni F, et al. Primary extranodal non-Hodgkin’s lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Annals of Oncology. 1997;8:727–737. doi: 10.1023/a:1008282818705. [DOI] [PubMed] [Google Scholar]
- 3.Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. British Journal of Surgery. 1961;49:80–89. doi: 10.1002/bjs.18004921319. [DOI] [PubMed] [Google Scholar]
- 4.Rock J, Bloomston M, Lozanski G, et al. The spectrum of hematologic malignancies involving the pancreas: potential clinical mimics of pancreatic adenocarcinoma. American Journal of Clinical Pathology. 2012;137:414–422. doi: 10.1309/AJCPCXW7QUG9EFTO. [DOI] [PubMed] [Google Scholar]
- 5.Puli SR, Bechtold ML, Buxbaum JL, et al. How good is endoscopic ultrasoundguided fine-needle aspiration in diagnosing the correct etiology for a solid pancreatic mass? A meta-analysis and systematic review. Pancreas. 2013;42:20–26. doi: 10.1097/MPA.0b013e3182546e79. [DOI] [PubMed] [Google Scholar]
- 6.Battula N, Srinivasan P, Prachalias A, et al. Primary pancreatic lymphoma: diagnostic and therapeutic dilemma. Pancreas. 2006;33:192–194. doi: 10.1097/01.mpa.0000227910.63579.15. [DOI] [PubMed] [Google Scholar]
- 7.Khashab M, Mokadem M, DeWitt J, et al. Endoscopic ultrasound-guided fineneedle aspiration with or without flow cytometry for the diagnosis of primary pancreatic lymphoma – a case series. Endoscopy. 2010;42:228–231. doi: 10.1055/s-0029-1243859. [DOI] [PubMed] [Google Scholar]
- 8.Van Beers B, Lalonde L, Soyer P, et al. Dynamic CT in pancreatic lymphoma. Journal of Computer Assisted Tomography. 1993;17:94–97. doi: 10.1097/00004728-199301000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Merkle EM, Bender GN, Brambs HJ. Imaging findings in pancreatic lymphoma: differential aspects. AJR: American Journal of Roentgenology. 2000;174:671–675. doi: 10.2214/ajr.174.3.1740671. [DOI] [PubMed] [Google Scholar]
- 10.Ribeiro A, Pereira D, Escalón MP, et al. EUS-guided biopsy for the diagnosis and classification of lymphoma. Gastrointestinal Endoscopy. 2010;71:851–855. doi: 10.1016/j.gie.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 11.Al-Haddad M, Savabi MS, Sherman S, et al. Role of endoscopic ultrasoundguided fine-needle aspiration with flow cytometry to diagnose lymphoma: a single center experience. Journal of Gastroenterology and Hepatology. 2009;24:1826–1833. doi: 10.1111/j.1440-1746.2009.06005.x. [DOI] [PubMed] [Google Scholar]