Abstract
Objectives
We aimed to compare the inter-observer agreement between two experienced readers using supine versus combined supine/prone myocardial perfusion SPECT (MPS) in a large population.
Methods
1181 consecutive patients without known coronary artery disease (CAD) undergoing rest 201Tl/stress 99mTc-sestamibi MPS studies were evaluated. Visual reads were performed in 2 consecutive steps, with readers scoring the stress supine perfusion images during step 1 and rescoring the images using both supine/prone data during step 2. Visual summed stress scores (SSS) of 2 readers including regional scores in different vascular territories were compared.
Results
The specificity for both readers improved using combined supine/prone imaging (Reader 1: 92% vs. 86% [P=0.0002], Reader 2: 88% vs. 72% [P<0.0001]. The inter-observer correlation for SSS (0.90 vs. 0.84, P<0.0001) and inter-observer agreement for combined supine/prone reading (bias = 1.0, 95% confidence interval (CI) 0.9-1.2 vs. 3.1, 95% CI 2.8-3.4, P<0.0001) were significantly better than for supine-only reading. The overall correlation between SSS scores for two readers improved with supine/prone imaging for both genders, as well as in the left anterior descending and right coronary territories.
New Knowledge Gained
Combined supine/prone imaging improves overall inter-observer agreement as well as based on gender and vascular territories.
Conclusion
The inter-observer correlation and agreement significantly improves using two-position supine/prone versus supine-only imaging.
Keywords: Inter-observer Agreement, Coronary Artery Disease, Myocardial Perfusion SPECT, Visual Summed Stress Score, Supine-Prone SPECT
Introduction
Myocardial perfusion SPECT (MPS) is the most commonly used noninvasive stress imaging modality of choice for diagnosis of coronary artery disease (CAD) 1. The interpretation of MPS involves visual and semi-quantitative analysis of stress and rest perfusion images to identify differences in perfusion, which is inherently subjective in nature leading to significant inter-observer variability 2. Significant variations in analysis by different observers may lead to marked differences in clinical decision making; hence inter-observer agreement plays an important role in diagnostic performance of diagnostic test in addition to the accuracy of the test. Prior studies have demonstrated that combined supine and prone MPS acquisitions results in improved specificity without a significant decline in sensitivity 3,4.
The aim of the current study was to evaluate the inter-observer agreement for visual analysis of two expert readers using combined supine and prone MPS versus using supine analysis only in a large population. We hypothesized that prone imaging improves inter-observer agreement by identifying artifacts especially in the inferior territory.
Materials and Methods
Patient Population
The subjects with suspected CAD who were referred to the Nuclear Medicine Department of Cedars-Sinai Medical Center, Los Angeles, California, from November 1, 2001 to June 30, 2005 for rest and stress electrocardiography (ECG)-gated, performed in both supine and prone positions, were consecutively selected5. All patients with a prior history of CAD, known cardiomyopathy, left bundle branch block, pacemaker, or significant valve disease were excluded. However, patients with obesity were not excluded in our study, with 12% of patients having a BMI ≥ 35 and 5% of patients having a BMI ≥ 40. Based on these selection criteria, 1181 sequential studies were identified to form the evaluation group. This population consisted of two subgroups of patients: 713 patients with correlative angiography and 468 patients with a low likelihood (LLk) of CAD. In the angiography group, MPS and coronary angiography had to be performed within 60 days without a significant intervening event. The majority of the patients in the angiography group underwent MPS prior to cardiac catheterization (96%). The LLk group consisted of patients who did not have correlating coronary angiography available, but had a low pretest likelihood of CAD (<5%). The clinical characteristics are listed in Table 1. The data analyzed in this study have been selected retrospectively from the existing database at Cedars-Sinai Medical Center (Los Angeles, California). The retrospective use of clinical data in this study was approved by the Institutional Review Board at Cedars-Sinai and informed consent was obtained from all patients.
Table 1.
Baseline characteristics of the patients.
| Study Population | |
|---|---|
| Number | 1181 |
| Age (Years) | 57.6 ± 14.0 |
| Male (%) | 648 (55%) |
| Female (%) | 533 (45%) |
| Body Mass Index (BMI) | 28.1 ±7.2 |
| Diabetes Mellitus (%) | 204 (17%) |
| Hypertension (%) | 601 (51%) |
| Hyperlipidemia (%) | 549 (46%) |
| Smoking (%) | 69 (6%) |
| Family History (%) | 154 (13%) |
| Asymptomatic (%) | 532 (45%) |
| Typical Chest Pain (%) | 79 (7%) |
| Atypical Chest Pain (%) | 431 (36%) |
| Non-Anginal Chest Pain | 85 (7%) |
| Dyspnea (%) | 54 (5%) |
| Exercise SPECT | 577 (49%) |
| Adenosine SPECT | 604 (51%) |
| Ejection Fraction (%) | 63.3 ± 12.5 |
| Angiographic Subpopulation: | |
| Cath: 0-Vessel Disease | 291 (41%) |
| Cath: 1-Vessel Disease | 204 (29%) |
| Cath: 2-Vessel Disease | 149 (21%) |
| Cath: 3-Vessel Disease | 63 (9%) |
Exercise MPS protocol
Patients performed a symptom limited exercise treadmill test with the standard Bruce protocol. At near-maximum exercise, 99mTc-sestamibi (25-40 mCi based on patient weight) was injected intravenously. Treadmill exercise was continued at maximum workload for 1 minute and at one stage lower for 2 additional minutes when possible. 99mTc-sestamibi MPS acquisition was started 15 to 30 minutes after radiopharmaceutical injection.
Adenosine MPS protocol
Adenosine MPS was performed as previously described 6. Adenosine was infused at 140 μg · kg −1 · min−1 for 5 minutes. At the end of the second minute, 99mTc-sestamibi (25-40 mCi) was injected, and MPS acquisition was started approximately 60 minutes later. Whenever possible, during adenosine infusion, patients performed a low-level treadmill exercise, walking at 0% grade at 1 to 1.7 mph 7. With the latter protocol, imaging began 15 to 60 minutes after adenosine stress.
Image Acquisition and Reconstruction Protocols
The details of image acquisition and tomographic reconstruction have been previously described 8. All patients underwent separate-acquisition rest Tl-201/stress 99mTc-sestamibi dual-isotope MPS as previously described 9. Post-stress 99mTc-sestamibi acquisitions were performed beginning 15 to 60 minutes after injection, with 64 projections at 25 seconds per projection for supine 99mTc acquisition (~25-30 minutes), followed immediately by 32 projections at 15 seconds per projection for prone 99mTc acquisition (~extra 10-15 minutes depending on body habitus and intensity of gut activity). The rest Tl-201 acquisition were performed beginning 10 minutes after injection, with 35 seconds per projection. Images were acquired on a dual-detector camera (Forte or Vertex [Philips Medical Systems, Andover, Massachusetts] or e.cam [Siemens Medical Systems, Malvern, Pennsylvania]) equipped with high-resolution collimators. No attenuation or scatter correction was applied. Studies were reconstructed on the respective vendor platforms (Pegasys [Philips Medical Systems] or e.soft 2000 [Siemens Medical Systems]) by use of their commercial implementations of the iterative reconstruction. The reconstruction parameters were 12 iterations with Butterworth prefiltering (cutoff, 0.66 cycles per pixel for supine 99mTc and 0.55 cycles per pixel for prone 99mTc; order, 5). These parameters were optimized previously to provide optimal image quality for clinical scan reading 10. Gated images were only obtained for the supine position. Short-axis images were automatically generated 11. In minority of cases when the software failed to detect left ventricular contours, manual and visual assessment was needed for the derivation of the automated results by an experienced technologist. In addition, if patient motion was noted during review of raw projections, motion correction (MoCo) software was applied 12. After reconstruction, the images were transferred visual analysis using Cedars-Sinai QPS software 13.
Visual Analysis
Visual interpretation of MPS images was based on short axis, horizontal and vertical long-axis slices static images. Gated images were also provided for review. The myocardium was divided into 17 segments using QPS interactive 17-segment graph 13 according to the American Heart Association system 14. MPS images were scored independently by two expert cardiologists (Reader 1 with 30 years and Reader 2 with more than 10 years of clinical experience in nuclear cardiology as attending physicians) using a five-point scoring system (0-normal; 1-mildly decreased uptake; 2-moderately decreased uptake; 3-severely decreased uptake; and 4-absence of segmental uptake). Visual reading was performed in 2 consecutive steps with readers being provided with only supine data during the initial step, while being provided with supine and prone data during the second step. Readers could modify stress and rest scores in each step using the additional information they have been revealed. New defects on the prone images were considered as an artifact, however if a perfusion defect was present in both positions it was considered abnormal regardless of gender. The readers were blinded to quantitative computer results and clinical information.
During the first step, the readers scored 17 stress and rest segments using the 5-point scale described above. The readers were able to review stress and rest perfusion data, raw projection data and gated supine data 15. During the second scoring step, the readers could re-score the stress and rest studies based on additional prone data shown. During each step, the observer could also modify the default assignment of segments to the specific vascular territory as it is possible in QPS/QGS software.
The reproducibility analysis only evaluated stress scores since the additional prone images were only obtained during stress. Summed stress scores (SSS) were obtained by summing the 17 segment visual stress scores. A visual SSS score of ≥ 4 was considered positive, while SSS score of < 4 was considered normal 10. Furthermore, partial summed scores for each vascular territory were also obtained with SSS ≥ 2 being considered abnormal for any territory16. We chose to focus on SSS because supine and prone positions were used only during stress imaging, while rest images were obtained in supine position only. Furthermore, our population consisted of patients with suspected disease with low-likelihood of CAD and no known infarcts. In addition, we also wanted to focus on 99mTc-sestamibi studies, therefore the rest images obtained with 201Tl were not used at all in our analysis. All visual scores were recorded automatically and directly converted for the statistical analysis in a batch mode, eliminating manual transfer.
Conventional Coronary Angiography
Conventional invasive coronary angiography (ICA) was performed according to standard clinical protocols, within 60 days of the myocardial perfusion examination in 60% of our population. All coronary angiograms were analyzed using quantitative coronary arteriography (QCA) by an experienced cardiologist. A stenosis of 50% or greater narrowing of luminal diameter of the left main or 70% or greater narrowing of the other coronary arteries by ICA was considered significant and was used as the gold standard for the detection of obstructive CAD.
Statistical Analysis
Continuous variables were expressed as the means ± standard deviation (SD), and categorical variables were expressed as percentages (%). The inter-observer correlation between the two readers’ scores using supine versus combined supine/prone imaging were compared using Pearson correlation coefficient, and secondly using the Inter-class correlation coefficient (ICC) for absolute agreement 17. The inter-observer agreement between two readers using supine versus combined supine/prone imaging were compared by % positive, negative, and total agreement using Z-test and by Cohen's kappa coefficients. The Bland-Altman 95% confidence intervals (CI) and bias (based on Bland-Altman) were compared using the one-sample variance comparison test. Furthermore, we compared inter-observer correlation, Bland Altman plots, % agreement and the Cohen's kappa coefficients for supine and supine/prone reading when stratified based on gender and vascular territory. For all analyses, p values < 0.05 were considered statistically significant.
Results
Contours were manually adjusted in 12% of the supine cases and 14% of the prone cases, with majority of these adjustments (9% for supine and 11% for prone) involving alteration of the mitral valve plane only. Thirty-five percent of cases were considered abnormal by Reader 1 during Step 1, while 30% of cases were considered abnormal during the second step (p < 0.01). The average SSS score for all studies during Step 1 and 2 for Reader 1 were 3.5 ± 5.3 and 3.0 ± 5.2 (p < 0.0001), respectively. On the other hand, 49% of cases were considered abnormal (average SSS score for all studies was 6.6 ± 8.4) by Reader 2 during Step 1, while 34% of cases were considered abnormal during Step 2 (average SSS score for all studies was 4.1 ± 6.6) [p < 0.001].
Diagnostic Performance of Expert Readers Using Supine Only Versus Supine/Prone Combined Imaging
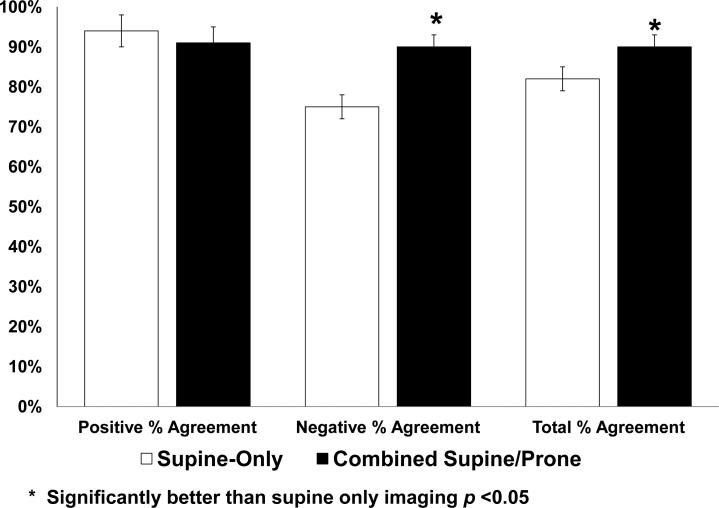
We compared the diagnostic performance of each experienced reader using supine imaging versus combined supine/prone imaging. The sensitivity for reader 1 did not significantly change for supine (74%) versus combined supine/prone (71%) [P = 0.26], however the specificity improved to 92% from 86% using combined imaging (P = 0.0002). The sensitivity for reader 2 decreased from 86% for supine only imaging compared to 74% for combined supine/prone imaging (P < 0.0001). The specificity similarly improved to 88% from 72% using combined imaging (P < 0.0001) (Figure 1).
Figure 1.
Diagnostic performance of expert readers using supine only versus supine/prone combined imaging in the entire population (n = 1181).
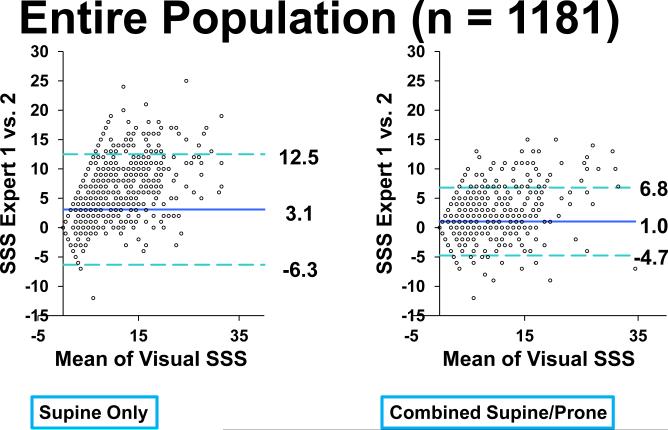
Comparison of Inter-Observer Correlation and Agreement for Stress Scores
The inter-observer correlation and agreement between the two readers using supine-only and supine/prone imaging is shown in Table 2. The inter-observer correlation for SSS was higher for supine/prone imaging (0.90 vs. 0.84, p < 0.0001) as compared to supine-only imaging. The negative agreement (regarding normal findings) and total agreement (regarding both positive and negative findings) for the supine/prone imaging was higher than supine-only imaging (Figure 2). In addition, the bias and 95% CI were smaller for the supine/prone imaging versus supine only imaging (p < 0.0001) [Figure 3]. The inter-observer agreement comparing positive and negative reads was also significantly better for supine/prone reading (kappa = 0.78) versus supine-only reading (kappa = 0.63) [p < 0.0001].
Table 2.
Inter-observer agreement and correlation using supine only and supine/prone imaging according to global, gender, and the vascular territory.
| Bias ± SD | 95% CI | R | κ | Bias ± SD | 95% CI | r | κ | |
|---|---|---|---|---|---|---|---|---|
| Supine-only | Supine/Prone | |||||||
| Global | ||||||||
| SSS | 3.1±0.1 | 2.8-3.4 | 0.84 | 0.63 | 1.0 ± 0.1* | 0.9-1.2* | 0.90* | 0.78* |
| Males | 3.8±0.2 | 3.4-4.2 | 0.86 | 0.64 | 1.5 ± 0.1* | 1.2-1.7* | 0.90* | 0.76* |
| Females | 2.2±0.2 | 1.9-2.6 | 0.75 | 0.56 | 0.5 ± 0.1* | 0.4-0.7* | 0.86* | 0.76* |
| Regional | ||||||||
| LAD SSS | 1.3±0.1 | 1.2-1.4 | 0.85 | 0.55 | 0.6 ± 0.1* | 0.5-0.7* | 0.89* | 0.70* |
| LCX SSS | 0.8±0.1 | 0.7-0.9 | 0.83 | 0.60 | 0.3 ± 0* | 0.2-0.4* | 0.84 | 0.69* |
| RCA SSS | 1.0±0.1 | 0.8-1.1 | 0.79 | 0.60 | 0.1 ± 0* | 0.0-0.2* | 0.86* | 0.77* |
Significantly better than supine only imaging p <0.01. SSS: Visual Summed Stress Score, LAD: Left Anterior Descending Artery, LCX: Left Circumflex Artery, RCA: Right Coronary Artery CI – Confidence Interval, r - Person's correlation coefficient, κ - Cohen-kappa coefficient.
Figure 2.
Diagnostic agreement between supine-only and combined supine/prone imaging.
Figure 3.
Differences of visual summed stress scores between supine-only and combined supine/prone imaging in the entire population (n = 1181).
We also assessed the correlation between our two expert readers based on presence of single vessel versus multi-vessel disease. There were 204 patients with single-vessel disease and 218 patients for multi-vessel disease (Table 1). Amongst patients with single vessel disease, correlations were 0.80 vs. 0.85 (P = 0.057) for supine and supine/prone imaging, respectively. Amongst patients with multi-vessel disease, correlations were 0.85 vs. 0.84 (P = 0.36) for supine and prone imaging, respectively. Although, there was a trend for improved correlation in single-vessel disease, there were no significant correlation differences amongst SSS scores for supine and prone imaging in patients with multi-vessel disease.
We also assessed the number of cases where the case was considered to be normal on supine, but scored as abnormal on supine/prone imaging. Reader 1 considered 765 studies as normal using supine imaging, 13 of which were considered as abnormal once prone imaging was added. Reader 2 considered 601 studies as normal, 9 of which were considered as abnormal once prone imaging was added. On the other hand, reader 1 considered 416 studies as abnormal using supine imaging, 71 of which were considered as normal once prone imaging was added. Reader 2 considered 580 studies as abnormal, 184 of which were considered as normal once prone imaging was added. Overall, the diagnosis was changed in 7.1% of cases using prone imaging for reader 1, and 16.3% of cases for reader 2 (these include all cases that were changed using combined supine/prone imaging, either to normal or abnormal). Furthermore, reader 1 re-classified only 3/215 cases of severe defects (defined as SSS > 7) as normal (defined as SSS <4) using prone imaging, while reader 2 re-classified 85/427 cases as normal using prone imaging.
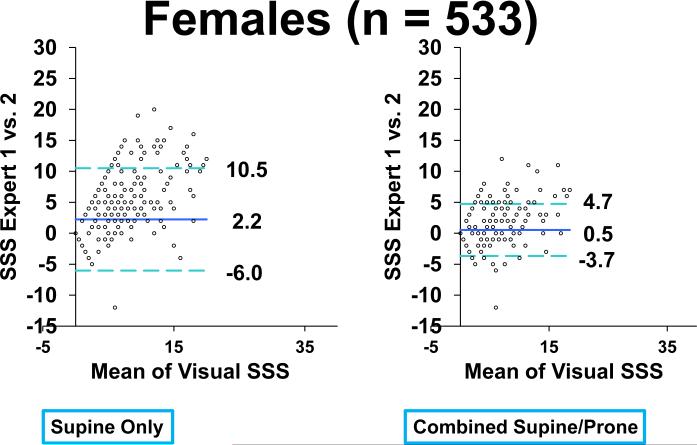
Comparison of Inter-Observer Correlation and Agreement for Stress Scores Based on Gender
The inter-observer correlations and agreements between the two readers using supine-only and supine/prone imaging stratified based on gender are shown in Table 2. The reader inter-observer correlations for both men and women were higher for supine/prone imaging (Female: 0.86 vs. 0.75, p < 0.0001; Male: 0.90 vs. 0.86, p = 0.0013) as compared to supine-only imaging. The reader bias, 95% CI were smaller for the supine/prone imaging for both males and females versus supine-only imaging (p < 0.0001) [Figure 4 and 5].
Figure 4.
Differences of visual summed stress scores between supine-only and combined supine/prone imaging in males (n = 648).
Figure 5.
Differences of visual summed stress scores between supine-only and combined supine/prone imaging in females (n = 533).
Reader 1 changed the diagnosis from abnormal to normal in 6.3% of cases in males and 5.6% of females (P = 0.61), while reader 2 changed the diagnosis from abnormal to normal in 13.3% of cases in males and 18.4% of females (P = 0.016).
Comparison of Inter-Observer Correlation and Agreement for Stress Scores Based on Vascular Territory
The inter-observer correlations and agreements between the two readers using supine-only and supine/prone imaging according to the vascular territory are shown in Table 2. The reader bias and 95% CI were smaller in all vascular territories when combined supine/prone imaging was used (Table 2). Furthermore, the inter-observer correlation for supine/prone reading was significantly better in left anterior descending (LAD) [0.89 vs. 0.85, p < 0.001] and right coronary territory (RCA) [0.86 vs. 0.79, p < 0.0001] as compared to supine-only reading, but was similar for left circumflex territory (LCX) [0.84 vs. 0.83, p = 0.42]. The Cohen-kappa coefficient was higher in all vascular territories for supine/prone reading (LAD: 0.70 vs. 0.55, p < 0.0001; LCX: 0.69 vs. 0.60, p < 0.001; RCA: 0.77 vs. 0.60, p < 0.0001) compared to supine-only reading.
Reader 1 considered the SSS as abnormal in 25.4% of cases in LAD territory, 18% of cases in LCX territory, and 27.1% of cases in RCA territory. The abnormal studies were considered normal using prone imaging in 18.7% (56/300) of abnormal LAD cases, 19.7% (42/213) of abnormal LCX cases, and 25% (80/320) of RCA cases. When compared to the overall studies changed to normal by reader 1 (17.1%), only the numbers of normalized cases in the RCA were significant (P = 0.0013). Reader 2 considered the SSS as abnormal in 42.3% of cases in LAD territory, 30.2% of cases in LCX territory, and 36.7% of cases in RCA territory. The abnormal studies were considered normalized using prone imaging in 32.9% (164/499) of abnormal LAD cases, 42.3% (151/357) of abnormal LCX cases, and 40.2% (175/435) of RCA cases. When compared to the overall studies changed to normal by reader 2 (31.7%), only the number of normalized cases in the LCX and RCA were significant (P < 0.001).
Discussion
MPS is the most utilized non-invasive imaging modality and plays an important role in diagnosing significant cardiovascular disease, providing prognosis, as well as assessing the effectiveness of therapy 18. However, despite its overall effectiveness, interpretation of MPS is complex due to possible imaging artifacts including those related to patient and equipment. Attenuation artifact is one of the most common artifacts in MPS, typically related to breast in women and diaphragm in men 19. Hardware and software for attenuation and scatter correction are commercially available, however attenuation-correction systems add cost and are estimated to be available in only less than 5% of labs worldwide 20. Other artifacts, which can occur including patient motion artifacts and external activity interference. The 2-position imaging could possibly mitigate all the above artifacts. Quantitative combined supine/prone imaging has been shown to improve specificity and accuracy when compared to supine-only imaging 4,8. In our current study, we were again able to show improved specificity by both readers using combined supine/prone imaging, similar to what has been reported previously. It was noted that the reduction in false positive rate and improvement in specificity using combined supine/prone imaging were due to recognition of shifting breast attenuation artifacts 4. In addition, prone position has been shown to increase inferior and septal wall counts, reduce patient motion, and decrease diaphragmatic attenuation by lowering the diaphragm and allowing the heart to move closer to the chest wall 3,21.
Visual analysis of MPS, currently the recommended standard clinical practice 19, is dependent on a subjective interpretation of the data, which is also a major shortcoming of other non-invasive stress tests such as stress echocardiography. Previous studies have evaluated various factors affecting inter-observer agreement including image quality, reader's experience, standardization of image display, and computerized quantification 2,22–24. To our knowledge, this is a first study to compare inter-observer correlation, bias, confidence intervals, and diagnostic agreement between two-position supine/prone visual scoring as compared to supine-only visual scoring. In our study, the inter-observer correlation, agreement, bias, and 95% CI significantly improved when prone images were added.
We compared inter-observer correlation and agreement according to gender. Previous studies have demonstrated the disappearance of artifacts in the prone position, primarily due to the ability to generate higher counts from the inferior wall in prone position than when the patient is in the supine position 21,25. Although, inferior attenuation artifacts are more common in male patients 26, prone imaging has been shown to increase myocardial uptake in inferior segments in both men and women 8. In addition, if patient motion or interfering external activity causes artifacts only in one of the scans, the two-position imaging would allow reporting of the scan as normal. The combination of supine and prone imaging allows the reader to eliminate these common artifacts, possibly explaining the improvement in inter-observer correlation and agreement. Accordingly, the inter-observer correlation, agreement, bias, and 95% CI in our study improved in both genders when prone imaging were added.
In the pre-vessel analysis, the agreement and correlation improved in the LAD and RCA territory, likely due to the resolution of previously discussed artifacts. We also demonstrated that in the subset of studies that normalized using combined supine/prone imaging, the RCA territory was the one that was most commonly normalized, likely due to identification of inferior artifacts. The similar finding would be expected in the analysis of data with attenuation correction.
Prior studies have demonstrated that the level of reader's expertise plays an important role in interpretation reproducibility and accuracy 24,27. The readers in our study were experts from premier imaging centers with extensive experience in MPS interpretation, therefore it is feasible that the overall supine-only agreement would have been lower and potentially the improvement in agreement could be even higher in less experienced readers. The improvement in agreement will likely result in more uniform and standard care, which in addition to improvement in accuracy will lead to less unnecessary additional tests. Therefore, we recommend combined supine/prone imaging, when attenuation correction systems are not available.
This study has several limitations. The goal of the current study was to evaluate the effect of two-position supine/prone imaging on visual inter-observer reproducibility. Quantitative analysis was not used in this study. Prior studies have demonstrated that additional prone imaging at stress improves the specificity and accuracy for detection of coronary artery disease4,8. The large difference in number of abnormal images between our expert readers reflects the different reading styles of our expert physicians and illustrates the general limitation of visual reading. Finally, although we had a large patient population, the results were obtained on one camera system and using one supine-prone protocol. Further multicenter evaluation may be required in the future to confirm these results.
Conclusion
The inter-observer correlation, confidence interval, bias and diagnostic agreement significantly improves when prone images are considered in addition to supine myocardial perfusion images.
Acknowledgements
This research was supported in part by grants R01HL089765 from the National Heart, Lung, and Blood Institute/National Institutes of Health (NHLBI/NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NHLBI. Cedars-Sinai Medical Center receives royalties for the quantitative assessment of function, perfusion, and viability, a portion of which is distributed to some of the authors of this manuscript (DB, GG, PS). We would like to thank Dr. Caroline Kilian and Arpine Oganyan for proof reading the text, Mr. Jim Gerlach for quality controls of the data and Ms. Heidi Gransar for the statistical analysis.
Abbreviations
- MPS
Myocardial Perfusion SPECT
- CAD
Coronary Artery Disease
- SSS
Summed Stress Score
References
- 1.Underwood SR, Anagnostopoulos C, Cerqueira M, Ell PJ, Flint EJ, Harbinson M, et al. Myocardial perfusion scintigraphy: the evidence. Eur. J. Nucl. Med. Mol. Imaging. 2004;31:261–291. doi: 10.1007/s00259-003-1344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danias PG, Ahlberg AW, Travin MI, Mahr NC, Abreu JE, Marini D, et al. Visual assessment of left ventricular perfusion and function with electrocardiography-gated SPECT has high intraobserver and interobserver reproducibility among experienced nuclear cardiologists and cardiology trainees. J Nucl Cardiol. 2002;9:263–270. doi: 10.1067/mnc.2002.121233. [DOI] [PubMed] [Google Scholar]
- 3.Berman DS, Kang X, Nishina H, Slomka PJ, Shaw LJ, Hayes SW, et al. Diagnostic accuracy of gated Tc-99m sestamibi stress myocardial perfusion SPECT with combined supine and prone acquisitions to detect coronary artery disease in obese and nonobese patients. J Nucl Cardiol. 2006;13:191–201. doi: 10.1007/BF02971243. [DOI] [PubMed] [Google Scholar]
- 4.Slomka PJ, Nishina H, Abidov A, Hayes SW, Friedman JD, Berman DS, et al. Combined quantitative supine-prone myocardial perfusion SPECT improves detection of coronary artery disease and normalcy rates in women. J Nucl Cardiol. 2007;14:44–52. doi: 10.1016/j.nuclcard.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 5.Arsanjani R, Xu Y, Dey D, Vahistha V, Shalev A, Nakanishi R, et al. Improved accuracy of myocardial perfusion SPECT for detection of coronary artery disease by machine learning in a large population. J Nucl Cardiol. 2013 doi: 10.1007/s12350-013-9706-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amanullah AM, Kiat H, Friedman JD, Berman DS. Adenosine technetium-99m sestamibi myocardial perfusion SPECT in women: diagnostic efficacy in detection of coronary artery disease. J. Am. Coll. Cardiol. 1996;27:803–809. doi: 10.1016/0735-1097(95)00550-1. [DOI] [PubMed] [Google Scholar]
- 7.Berman DS, Kang X, Hayes SW, Friedman JD, Cohen I, Abidov A, et al. Adenosine myocardial perfusion single-photon emission computed tomography in women compared with men. Impact of diabetes mellitus on incremental prognostic value and effect on patient management. J. Am. Coll. Cardiol. 2003;41:1125–1133. doi: 10.1016/s0735-1097(03)00085-8. [DOI] [PubMed] [Google Scholar]
- 8.Nishina H, Slomka PJ, Abidov A, Yoda S, Akincioglu C, Kang X, et al. Combined supine and prone quantitative myocardial perfusion SPECT: method development and clinical validation in patients with no known coronary artery disease. J. Nucl. Med. 2006;47:51–58. [PubMed] [Google Scholar]
- 9.Berman DS, Kiat H, Friedman JD, Wang FP, van Train K, Matzer L, et al. Separate acquisition rest thallium-201/stress technetium-99m sestamibi dual-isotope myocardial perfusion single-photon emission computed tomography: a clinical validation study. J. Am. Coll. Cardiol. 1993;22:1455–1464. doi: 10.1016/0735-1097(93)90557-h. [DOI] [PubMed] [Google Scholar]
- 10.Hayes SW, De Lorenzo A, Hachamovitch R, Dhar SC, Hsu P, Cohen I, et al. Prognostic implications of combined prone and supine acquisitions in patients with equivocal or abnormal supine myocardial perfusion SPECT. J. Nucl. Med. 2003;44:1633–1640. [PubMed] [Google Scholar]
- 11.Germano G, Kavanagh PB, Su HT, Mazzanti M, Kiat H, Hachamovitch R, et al. Automatic reorientation of three-dimensional, transaxial myocardial perfusion SPECT images. J. Nucl. Med. 1995;36:1107–1114. [PubMed] [Google Scholar]
- 12.Matsumoto N, Berman DS, Kavanagh PB, Gerlach J, Hayes SW, Lewin HC. Quantitative assessment of motion artifacts and validation of a new motion-correction program for myocardial perfusion SPECT. J. Nucl. Med. 2001;42:687–694. [PubMed] [Google Scholar]
- 13.Germano G, Kavanagh PB, Slomka PJ, Van Kriekinge SD, Pollard G, Berman DS. Quantitation in gated perfusion SPECT imaging: the Cedars-Sinai approach. J Nucl Cardiol. 2007;14:433–454. doi: 10.1016/j.nuclcard.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 14.Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539–542. doi: 10.1161/hc0402.102975. [DOI] [PubMed] [Google Scholar]
- 15.Wolak A, Slomka PJ, Fish MB, Lorenzo S, Acampa W, Berman DS, et al. Quantitative myocardial perfusion SPECT: comparison of three state-of-the-art software packages. J Nucl Cardiol. 2008;15:27–34. doi: 10.1016/j.nuclcard.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 16.Xu Y, Fish M, Gerlach J, Lemley M, Berman DS, Germano G, et al. Combined quantitative analysis of attenuation corrected and non-corrected myocardial perfusion SPECT: Method development and clinical validation. J Nucl Cardiol. 2010;17:591–599. doi: 10.1007/s12350-010-9220-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 18.Burrell S, MacDonald A. Artifacts and pitfalls in myocardial perfusion imaging. J Nucl Med Technol. 2006;34:193–211. quiz 212–214. [PubMed] [Google Scholar]
- 19.Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, et al. Single photon-emission computed tomography. J Nucl Cardiol. 2010;17:941–973. doi: 10.1007/s12350-010-9246-y. [DOI] [PubMed] [Google Scholar]
- 20.Germano G, Slomka PJ, Berman DS. Supine acceptance of a conventional imaging position may make you less prone to success. J Nucl Cardiol. 2010;17:16–18. doi: 10.1007/s12350-009-9187-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kiat H, Van Train KF, Friedman JD, Germano G, Silagan G, Wang FP, et al. Quantitative stress-redistribution thallium-201 SPECT using prone imaging: methodologic development and validation. J. Nucl. Med. 1992;33:1509–1515. [PubMed] [Google Scholar]
- 22.Wackers FJ, Bodenheimer M, Fleiss JL, Brown M. Factors affecting uniformity in interpretation of planar thallium-201 imaging in a multicenter trial. The Multicenter Study on Silent Myocardial Ischemia (MSSMI) Thallium-201 Investigators. J. Am. Coll. Cardiol. 1993;21:1064–1074. doi: 10.1016/0735-1097(93)90226-q. [DOI] [PubMed] [Google Scholar]
- 23.Hendel RC, Parker MA, Wackers FJ, Rigo P, Lahiri A, Zaret BL. Reduced variability of interpretation and improved image quality with a technetium 99m myocardial perfusion agent: comparison of thallium 201 and technetium 99m-labeled tetrofosmin. J Nucl Cardiol. 1994;1:509–514. doi: 10.1007/BF02939973. [DOI] [PubMed] [Google Scholar]
- 24.Golub RJ, Ahlberg AW, McClellan JR, Herman SD, Travin MI, Mather JF, et al. Interpretive reproducibility of stress Tc-99m sestamibi tomographic myocardial perfusion imaging. J Nucl Cardiol. 1999;6:257–269. doi: 10.1016/s1071-3581(99)90037-5. [DOI] [PubMed] [Google Scholar]
- 25.Segall GM, Davis MJ. Prone versus supine thallium myocardial SPECT: a method to decrease artifactual inferior wall defects. J. Nucl. Med. 1989;30:548–555. [PubMed] [Google Scholar]
- 26.DePuey EG, Rozanski A. Using gated technetium-99m-sestamibi SPECT to characterize fixed myocardial defects as infarct or artifact. J. Nucl. Med. 1995;36:952–955. [PubMed] [Google Scholar]
- 27.Golub RJ, McClellan JR, Herman SD, Travin MI, Kline GM, Aitken PW, et al. Effectiveness of nuclear cardiology training guidelines: a comparison of trainees with experienced readers. J Nucl Cardiol. 1996;3:114–118. doi: 10.1016/s1071-3581(96)90003-3. [DOI] [PubMed] [Google Scholar]