Summary
Background
Knowledge of the relation between health-system factors and child mortality could help to inform health policy in low-income and middle-income countries. We aimed to quantify modifiable health-system factors and their relation with provincial-level heterogeneity in under-5, infant, and neonatal mortality over time in Mozambique.
Methods
Using Demographic and Health Survey (2003 and 2011) and Multiple Indicator Cluster Survey (2008) data, we generated provincial-level time-series of child mortality in under-5 (ages 0–4 years), infant (younger than 1 year), and neonatal (younger than 1 month) age groups for 2000–10. We built negative binomial mixed models to examine health-system factors associated with changes in child mortality.
Findings
Under-5 mortality rate was heterogeneous across provinces, with yearly decreases ranging from 11·1% (Nampula) to 1·9% (Maputo Province). Heterogeneity was greater for neonatal mortality rate, with only seven of 11 provinces showing significant yearly decreases, ranging from 13·6% (Nampula) to 4·2% (Zambezia). Health workforce density (adjusted rate ratio 0·94, 95% CI 0·90–0·98) and maternal and child health nurse density (0·96, 0·92–0·99) were both associated with reduced under-5 mortality rate, as were institutional birth coverage (0·94, 0·90–0·98) and government financing per head (0·80, 0·65–0·98). Higher population per health facility was associated with increased under-5 mortality rate (1·14, 1·02–1·28). Neonatal mortality rate was most strongly associated with institutional birth attendance, maternal and child nurse density, and overall health workforce density. Infant mortality rate was most strongly associated with institutional birth attendance and population per health facility.
Interpretation
The large decreases in child mortality seen in Mozambique between 2000 and 2010 could have been partly caused by improvements in the public-sector health workforce, institutional birth coverage, and government health financing. Increased attention should be paid to service availability, because population per health facility is increasing across Mozambique and is associated with increased under-5 mortality. Investments in health information systems and new methods to track potentially increasing subnational health disparities are urgently needed.
Funding
Doris Duke Charitable Foundation and Mozambican National Institute of Health.
Introduction
Worldwide, deaths among children younger than 5 years decreased from an estimated 12 million to 6·6 million between 1990 and 2012.1 Sub-Saharan Africa saw a doubling of annual reductions in under-5 (ie, age 0–4 years) mortality rate between 1990–2000 and 2000–10. Mozambique, which has had one of the highest rates of under-5 mortality in the world, has made substantial progress towards achieving Millennium Development Goal 4 (MDG 4; to reduce the under-5 mortality rate by two-thirds between 1990 and 2015) target of 75 per 1000 livebirths; nationally, the under-5 mortality rate fell from 226 per 1000 livebirths in 1990 to 97 per 1000 livebirths reported in the 2011 Demographic and Health Survey (DHS).1,2 Worldwide, about 44% of child deaths occur during the neonatal period (before age 1 month) and this proportion is increasing because neonatal mortality is decreasing slower than is under-5 mortality.1 In Mozambique, neonatal deaths represented 23% of deaths before age 5 years in 1990 (neonatal mortality rate 53 per 1000 livebirths), increasing to 31% in 2011 (neonatal mortality rate 30 per 1000 livebirths). Similar to Mozambique, many countries have documented substantial reductions in under-5 mortality nationally; however, efforts are needed to identify effective strategies to further accelerate gains, especially for neonatal mortality. Strategies are also urgently needed to address potentially increasing regional disparities in health improvements within countries.2
More than 75% of deaths before age 5 years in Mozambique are caused by infectious, preventable diseases, with more than 60% attributable to malaria (42·3%), HIV (13·4%), and pneumonia (6·4%).3 Other major causes of death are diarrhoeal diseases, malnutrition, sepsis, and measles.4 For neonates, 35% of deaths are attributable to bacterial sepsis, and 10% to complications of pregnancy, labour, and delivery.4 Other major causes of death for neonates are fetal development disorders (6%), malaria (6%), hypoxia and asphyxia (6%), and pneumonia (4%).4 The Mozambican National Health Service is the primary provider of formal health services in the country, with more than 90% of the population outside of the capital city of Maputo seeking care from public-sector clinics. However, the system is understaffed and underfunded relative to the high burden of infectious and chronic diseases. Over the past decade, health-systems strengthening has been an important focus of efforts to achieve MDG 4, with particular attention paid to the role of human resources for health and the availability, access, and quality of safe delivery services.5 Several studies have examined the relation between health-system factors and under-5 mortality in low-income and middle-income countries, but few to none (to our knowledge) have used longitudinal designs with data resolutions below the national level.6-10
Individual-level determinants of under-5 mortality in low-income and middle-income countries are well known and include the mother’s level of education, age, place of residence, and access to water and sanitation; antenatal care; and the child’s place of birth and birthweight.11-14 Previous cross-national studies have shown high physician density, good access to water and sanitation, low government corruption, and high national incomes to be protective for national under-5 mortality, with out-of-pocket health expenditures a risk factor for under-5 mortality.8,15 Over the past decade, substantial effort and resources have been dedicated to improving the Mozambican health system, including workforce expansion, which has led to increases in health-worker density even while overall health expenditures (excluding vertical funds) have remained low (6·2% of gross domestic product [GDP] in 2009, or a per-head health expenditure of US$27).16-18
No previous studies have assessed the effect of changes in health-system factors on child mortality in under-5, infant, and neonatal age groups in Mozambique—knowledge that is crucial for guiding priority setting for resource allocation by the Ministry of Health and donors. In the present study, we examine subnational trends in child mortality and their relation to key variables related to health-system strength between 2000 and 2010, a period during which Mozambique saw large reductions in child mortality.
Methods
Data sources and outcomes
We estimated provincial-level under-5 (ages 0–4 years), infant (younger than 1 year), and neonatal (younger than 1 month) mortality from 2000 to 2010 in Mozambique using publicly available data from the 2003 and 2011 DHS19 and the 2008 Multiple Indicator Cluster Survey (MICS). Figure 1 shows the provincial structure of Mozambique.20 We merged these three datasets and used them to calculate the provincial-level probability of a child dying before their fifth birthday (under-5 mortality rate), before their first birthday (infant mortality rate), and in their first month of life (neonatal mortality rate; all expressed as deaths per 1000 livebirths) for each year of the 11-year period using direct life-table estimation methods21 that are reliant on full birth history data. The 2003 DHS provided provincial-level estimates for 2000–03; the 2008 MICS for 2000–08; and the 2011 DHS for 2000–10. The sample included 26 464 children in 2000, 20 936 children in 2005, and 10 697 children in 2010.
Figure 1. Political map of provinces and provincial capital cities of Mozambique.

Explanatory factors
We selected explanatory variables on the basis of the existing scientific literature on the determinants of under-5 mortality in low-income and middle-income countries,6-14 along with WHO’s definition of the essential building blocks of health systems.22 We extracted provincial-level yearly time-series covariate data from several sources and had these data verified by the Ministry of Health before undertaking the final analyses. Data abstracted from the National Health Information System (Módulo Básico) were selected from indicators previously shown to be of high data quality.23 All data for population denominator were from population forecasts calculated from census projections from 1997 and 2007.24,25 We applied exchange rates, calculated yearly, from the Mozambique Central Bank to expenditure data to convert Mozambican meticals to US$.
Overall health-workforce density was defined as the number of physicians, nurses, midwives, medical assistants (clinical, surgery, and psychiatry technicians), and public health personnel per 100 000 people in each province per year. Data were obtained from the National Directorate of Human Resources. Physician and maternal and child health nurse densities were defined as the number of physicians or maternal and child health nurses per 100 000 people, respectively. Health providers who held primary appointments at Ministry of Health offices were excluded from calculations.
Service availability was captured by annual population per health facility, defined as the provincial population divided by the number of public-sector health facilities in the same year. Data were calculated by triangulation of the Módulo Básico to the National Infrastructure Survey 2007. We calculated percentage birth attendance coverage using reported institutional births over the estimated number of births based on fecundity and population demographic data. Data for institutional births were from the Módulo Básico.
Annual expenditures on health per head included provincial government recurrent expenditures and onbudget donor resources channelled through the common fund to complement provincial expenditures. We calculated per-head figures for government and donor expenditures separately, as well as combined. Both central funds managed directly by the Ministry of Health for health programmes, pharmaceutical and equipment procurement, and donor vertical funds were excluded because of unavailability of provincial-level data. All health expenditure variables were based on data from the Ministry of Health Budget Execution Reports 2000–10.26
Provincial-level GDP per head was the total annual production divided by the total population in each province. We estimated annual HIV prevalence in children younger than 5 years for each region in the country using official Ministry of Health statistics.27
Statistical analysis
Our analysis plan included univariate analyses of variables across time and provinces; initial scatterplots to visualise explanatory variables across strata of under-5, infant, and neonatal mortality to identify outliers and determine functional forms for variable parameterisation; analyses of crude time trends in under-5, infant, and neonatal mortality nationally and across provinces; and analyses of each explanatory variable and its effect on under-5, infant, and neonatal mortality after accounting for the confounding effect of time. We used Stata version 13 (StataCorp, College Station, TX, USA) for statistical analyses. We assessed associations for statistical significance at α=0·05 using two-tailed tests.
We excluded Maputo City from the associative analyses because of its unique sociodemographic and service-provision characteristics shown in table 1. All health financing and income variables (including GDP per head) were log10-transformed. For ease of interpretation, to increase statistical power, and because we noted no strong deviations from linearity, all other predictor variables were modelled as continuous. Crude analyses of the time trend in under-5 mortality showed provincial-level heterogeneity in intercepts, as well as the rate of change over time. Results of initial analyses to assess the assumption necessary for Poisson models (ie, that the mean and variance of the outcome variable are equal), suggested that the variance exceeded the mean. Thus, we fitted mixed-effects negative binomial regression with random intercepts for province and random slopes over time. Analyses of residual plots suggested no significant lack of model fit. We assessed the national time trends in under-5, infant, and neonatal mortality by including continuous time alone in the model. To examine trends for each province separately, we included interaction terms between province and continuous time. Multicollinearity between predictor variables of interest and low statistical power precluded the use of a fully adjusted multivariable model.
Table 1.
Provincial-level descriptive statistics and under-5, infant, and neonatal mortality rate, stratified by time period (2000–05 and 2006–10), for key health-system factors in Mozambique
| Under-5 mortality rate (per 1000 livebirths) |
Infant mortality rate (per 1000 livebirths) |
Neonatal mortality rate (per 1000 livebirths) |
Population per health facility |
Birth attendance (%) |
Health workforce density (per 100 000) |
Overall expenditure on health per head (US$) |
Government expenditure on health per head (US$) |
GDP per
head (US$) |
Regional HIV prevalence in children younger than 5 years |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| 2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
2000– 05 |
2006– 10 |
|
| Cabo Delgado | 197·7 (26·9) | 115·1 (31·1) | 148·2 (18·3) | 89·0 (21·8) | 54·4 (7·5) | 35·5 (7·5) | 15 844 (218) | 15 468 (592) | 29·9 (4·8) | 52·5 (10·2) | 31·5 (4·7) | 49·8 (8·7) | 2·3 (0·50) | 4·5 (1·1) | 2·0 (0·54) | 3·3 (0·93) | 144·1 (25·4) | 247·2 (33·1) | 0·83 (0·26) | 1·2 (0·08) |
|
| ||||||||||||||||||||
| Gaza | 142·3 (11·2) | 118·7 (13·2) | 80·5 (7·0) | 69·4 (6·6) | 31·6 (2·8) | 32·3 (4·7) | 10 528 (160) | 10 193 (725) | 51·9 (2·5) | 51·4 (8·4) | 42·5 (3·5) | 60·1 (5·2) | 2·9 (0·32) | 4·7 (0·81) | 2·6 (0·37) | 3·6 (0·65) | 185·1 (25·7) | 330·7 (54·2) | 2·6 (0·74) | 3·5 (0·20) |
|
| ||||||||||||||||||||
| Inhambane | 109·6 (12·5) | 76·4 (16·0) | 69·5 (6·0) | 49·4 (11·0) | 28·4 (1·3) | 21·2 (5·5) | 13 665 (591) | 12 213 (720) | 42·7 (1·4) | 45·6 (5·4) | 45·5 (7·5) | 71·2 (14·4) | 2·7 (0·43) | 5·0 (1·2) | 2·4 (0·25) | 3·6 (0·71) | 253·8 (64·7) | 520·0 (74·1) | 2·6 (0·74) | 3·5 (0·20) |
|
| ||||||||||||||||||||
| Manica | 153·2 (14·5) | 118·6 (12·1) | 98·1 (10·2) | 69·4 (10·2) | 32·4 (5·0) | 22·8 (3·4) | 15 168 (896) | 16 322 (291) | 50·9 (6·6) | 62·2 (4·9) | 39·2 (4·7) | 53·3 (2·0) | 2·3 (0·28) | 4·4 (0·46) | 2·2 (0·32) | 3·0 (0·40) | 152·9 (16·5) | 221·9 (22·9) | 2·8 (0·09) | 2·7 (0·22) |
|
| ||||||||||||||||||||
| Maputo City | 93·1 (5·5) | 85·5 (6·4) | 61·3 (2·9) | 63·6 (2·4) | 29·2 (2·3) | 32·5 (3·3) | 23 691 (1162) | 28 271 (2298) | 82·5 (6·6) | 74·5 (3·8) | 121·4 (7·3) | 146·0 (12·4) | 10·6 (1·4) | 18·3 (2·9) | 10·3 (1·2) | 17·1 (2·6) | 845·7 (91·0) | 1429·0 (227·4) | 2·6 (0·74) | 3·5 (0·20) |
|
| ||||||||||||||||||||
| Maputo Province | 107·1 (4·1) | 95·8 (3·5) | 72·8 (3·4) | 72·3 (2·6) | 36·6 (1·8) | 37·9 (2·6) | 12 020 (1487) | 15 300 (1165) | 39·9 (4·1) | 42·8 (5·0) | 43·7 (2·8) | 51·9 (2·0) | 3·0 (0·48) | 4·8 (0·91) | 2·8 (0·47) | 3·9 (0·89) | 846·6 (2·6) | 1185·6 (78·9) | 2·6 (0·74) | 3·5 (0·20) |
|
| ||||||||||||||||||||
| Nampula | 148·6 (32·5) | 79·2 (25·7) | 107·8 (24·5) | 55·6 (19·7) | 45·2 (14·7) | 20·2 (7·4) | 17 940 (608) | 20 317 (746) | 39·0 (4·9) | 53·9 (5·3) | 30·7 (5·3) | 48·3 (4·5) | 2·2 (0·42) | 3·8 (0·59) | 1·8 (0·40) | 2·5 (0·52) | 211·5 (29·2) | 315·5 (30·8) | 0·83 (0·26) | 1·2 (0·08) |
|
| ||||||||||||||||||||
| Niassa | 146·7 (20·3) | 106·3 (19·3) | 103·3 (11·0) | 71·3 (16·9) | 45·2 (7·9) | 34·5 (3·7) | 7620 (330) | 8788 (253) | 63·2 (9·7) | 82·8 (5·6) | 50·9 (10·9) | 64·7 (1·7) | 3·4 (0·65) | 5·5 (0·77) | 3·0 (0·56) | 4·4 (0·66) | 159·6 (24·4) | 219·3 (14·5) | 0·83 (0·26) | 1·2 (0·08) |
|
| ||||||||||||||||||||
| Sofala | 157·2 (26·7) | 91·5 (10·4) | 107·3 (20·4) | 62·8 (5·1) | 42·7 (6·4) | 32·5 (3·1) | 9895 (907) | 11 638 (308) | 45·5 (3·3) | 60·0 (7·3) | 59·1 (5·0) | 70·6 (7·2) | 4·5 (0·58) | 7·4 (1·4) | 4·2 (0·60) | 5·7 (1·2) | 338·8 (48·9) | 534·7 (60·5) | 2·8 (0·09) | 2·7 (0·22) |
|
| ||||||||||||||||||||
| Tete | 171·5 (14·3) | 141·4 (10·9) | 111·9 (10·7) | 92·0 (4·3) | 46·5 (4·5) | 42·8 (2·0) | 13 828 (459) | 17 302 (1571) | 45·4 (2·5) | 50·4 (3·4) | 40·2 (4·1) | 44·1 (2·4) | 2·3 (0·39) | 3·6 (0·69) | 2·2 (0·29) | 2·7 (0·38) | 216·5 (39·1) | 272·6 (13·5) | 2·8 (0·09) | 2·7 (0·22) |
|
| ||||||||||||||||||||
| Zambezia | 176·3 (10·3) | 152·7 (18·6) | 136·2 (6·7) | 109·5 (13·0) | 56·3 (5·5) | 43·9 (6·0) | 19 879 (917) | 20 484 (572) | 32·7 (3·9) | 46·8 (8·5) | 25·3 (0·30) | 39·6 (7·1) | 1·6 (0·24) | 2·9 (0·35) | 1·6 (0·24) | 2·0 (0·31) | 128·1 (21·7) | 209·0 (23·8) | 2·8 (0·09) | 2·7 (0·22) |
|
| ||||||||||||||||||||
| National average* | 145·8 (34·9) | 107·4 (28·4) | 99·7 (28·8) | 73·1 (20·1) | 40·8 (11·2) | 32·4 (8·9) | 14 553 (4557) | 16 027 (5446) | 47·5 (15·0) | 56·6 (13·3) | 48·2 (25·6) | 63·6 (28·9) | 3·4 (2·4) | 5·9 (4·3) | 3·2 (2·4) | 4·7 (4·2) | 316·6 (265·2) | 498·7 (409·7) | 2·2 (0·96) | 2·6 (0·96) |
Data are mean (SD), presented as annual figures averaged across period.
Data have been averaged across the 11 provinces without respect to provincial-level population denominators.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
The crude national-level under-5 mortality rate fell from 166·6 per 1000 livebirths (95% CI 162·2–171·2) in 2000 to 93·7 per 1000 livebirths (87·9–100·0) in 2010 (figure 2). Crude under-5 mortality differed greatly between provinces, as did decreases over time. Cabo Delgado had the highest provincial under-5 mortality rate for the 6-year period of 2000–05 (197·7 per 1000 livebirths), but this was reduced to 115·1 per 1000 livebirths for the years 2006–10 (table 1). By contrast, Zambezia and Tete provinces made little progress (table 1). Nationally, infant mortality fell from 115·3 per 1000 livebirths (95% CI 111·5–119·2) in 2000 to 63·9 per 1000 livebirths (59·5–68·7) in 2010 and neonatal mortality fell from 48·2 per 1000 livebirths (45·7–50·8) in 2000 to 30·4 per 1000 livebirths (27·3–33·8) in 2010 (figure 2). Crude neonatal mortality and its change over time were strongly heterogeneous across provinces, with Maputo City, Maputo Province, and Gaza showing increases in neonatal mortality between 2000–05 and 2006–10. By contrast, in Nampula neonatal mortality fell from 45·2 per 1000 livebirths in 2000–05 to 20·2 per 1000 livebirths in 2006–10 (table 1).
Figure 2. National-level time-series for child mortality in Mozambique, 2000–10.
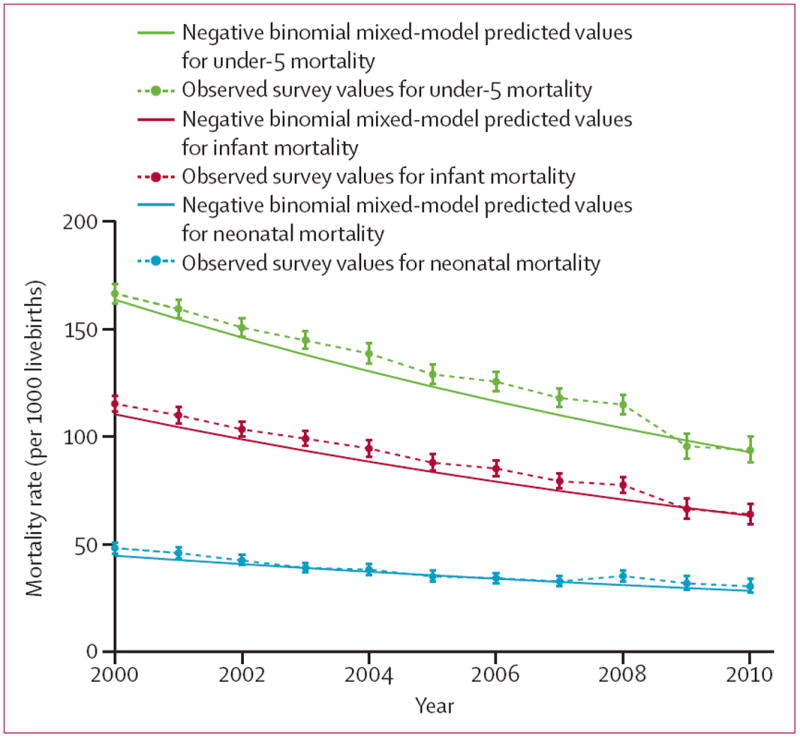
Error bars show 95% CIs for observed survey values.
Total population per health facility increased for eight of the 11 provinces between 2000–05 and 2006–10, with Maputo Province showing the greatest increase (table 1). The proportion of births attended by skilled professionals increased for nine of 11 provinces, with Cabo Delgado and Zambezia seeing very large increases (table 1). Every province showed improvement in health-workforce density over the study period, with Nampula, Inhambane, and Cabo Delgado seeing the greatest changes. Similarly, GDP and overall per-head expenditure on health increased for every province, with Cabo Delgado seeing the largest increase in overall health expenditure and Inhambane having the greatest increase in GDP (table 1).
Across all 11 provinces, under-5 mortality decreased by an average of 5·5% each year from 2000 to 2010, resulting in a 46·5% decrease over the entire 11-year period (figure 2; table 2). There was, however, statistically significant provincial-level heterogeneity in rates of change in under-5 mortality, with yearly decreases being as high as 11·1% (Nampula) and as low as about 2% (Maputo Province, 1·9%; Maputo City, 2·2%; figure 3). Across all provinces, infant mortality decreased by an average of 5·4% and neonatal mortality by 4·5% each year, resulting in a 45·8% reduction in infant mortality and a 39·4% reduction in neonatal mortality over the 11–year period (tables 3, 4). Seven of 11 provinces had significant decreases in neonatal mortality over the 11-year period, with yearly decreases as high as 13·6% for Nampula (table 4). Gaza, Maputo City, Maputo Province, and Tete did not have statistically significant changes in neonatal mortality over the 11-year period.
Table 2.
Mixed-effects negative binomial model of province-level and overall changes in under-5 mortality rate in Mozambique, 2000–10
| Rate ratio for province-level yearly change in under-5 mortality (95% CI) | p value | Overall percentage change in under-5 mortality rate, 2000–10 (95% CI) | |
|---|---|---|---|
| Cabo Delgado | 0·909 (0·895–0·923) | <0·0001 | –65·0% (–70·3 to –58·6) |
| Gaza | 0·964 (0·948–0·979) | <0·0001 | –33·4% (–44·2 to –20·4) |
| Inhambane | 0·933 (0·915–0·951) | <0·0001 | –53·5% (–62·4 to –42·6) |
| Manica | 0·955 (0·940–0·970) | <0·0001 | –39·9% (–49·5 to –28·5) |
| Maputo City | 0·978 (0·959–0·997) | 0·025 | –21·9% (–37·1 to –3·1) |
| Maputo Province | 0·981 (0·963–0·999) | 0·038 | –19·2% (–33·9 to –1·1) |
| Nampula | 0·889 (0·873–0·905) | <0·0001 | –72·7% (–77·6 to –66·8) |
| Niassa | 0·937 (0·922–0·953) | <0·0001 | –50·9% (–59·0 to –41·1) |
| Sofala | 0·911 (0·896–0·927) | <0·0001 | –64·0% (–70·0 to –56·6) |
| Tete | 0·964 (0·950–0·979) | <0·0001 | –33·1% (–43·1 to –21·3) |
| Zambezia | 0·978 (0·964–0·992) | 0·0022 | –22·0% (–33·4 to –8·6) |
| Overall | 0·945 (0·927–0·963) | <0·0001 | –46·5% (–56·6 to –34·0) |
Figure 3. Provincial-level time-series for child mortality in Mozambique, 2000–10.
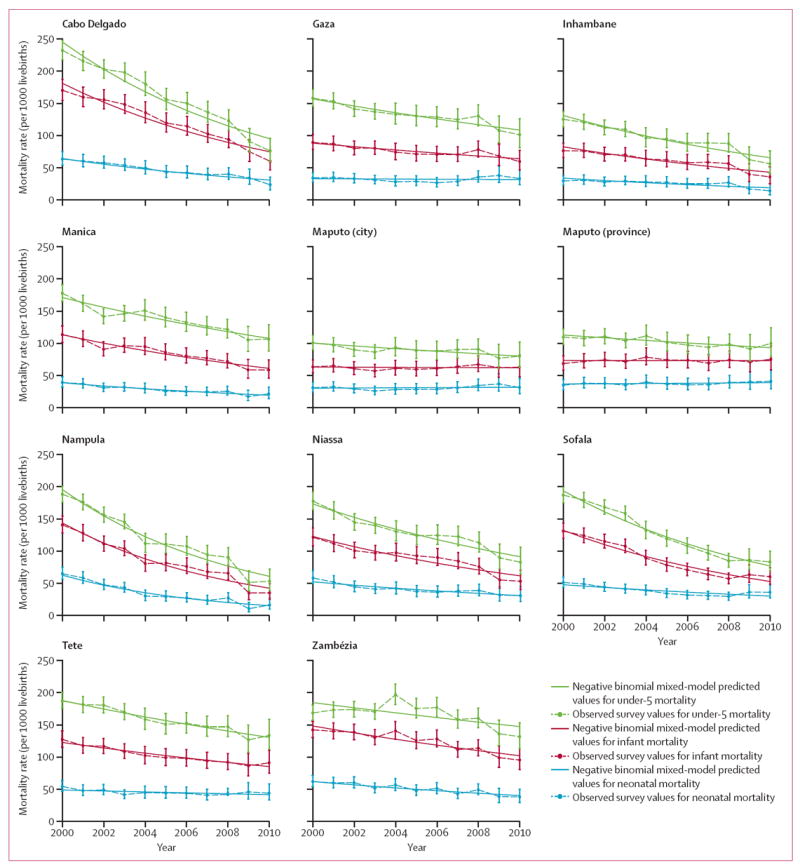
Error bars show 95% CIs for observed survey values.
Table 3.
Mixed-effects negative binomial model of province-level and overall changes in infant mortality rate in Mozambique, 2000–10
| Rate ratio for province-level yearly change in infant mortality (95% CI) | p value | Overall percentage change in infant mortality rate, 2000–10 (95% CI) | |
|---|---|---|---|
| Cabo Delgado | 0·915 (0·899–0·930) | <0·0001 | –62·5% (–69·0 to –54·6) |
| Gaza | 0·968 (0·948–0·989) | 0·003 | –29·9% (–44·5 to –11·4) |
| Inhambane | 0·937 (0·915–0·959) | <0·0001 | –51·4% (–62·7 to –36·7) |
| Manica | 0·940 (0·921–0·959) | <0·0001 | –49·3% (–59·5 to –36·7) |
| Maputo City | 0·998 (0·975–1·02) | 0·89 | –1·8% (–24·2 to 27·0) |
| Maputo Province | 0·999 (0·978–1·02) | 0·97 | –0·43% (–21·5 to 26·4) |
| Nampula | 0·884 (0·865–0·903) | <0·0001 | –74·4% (–79·7 to –67·6) |
| Niassa | 0·933 (0·914–0·952) | <0·0001 | –53·5% (–62·7 to –42·1) |
| Sofala | 0·912 (0·893–0·931) | <0·0001 | –63·8% (–71·0 to –54·7) |
| Tete | 0·964 (0·947–0·982) | <0·0001 | –33·2% (–45·4 to –18·3) |
| Zambezia | 0·963 (0·947–0·980) | <0·0001 | –33·7% (–44·9 to –20·4) |
| Overall | 0·946 (0·923–0·966) | <0·0001 | –45·8% (–57·2 to –31·4) |
Table 4.
Mixed-effects negative binomial model of province-level and overall changes in neonatal mortality rate in Mozambique, 2000–10
| Rate ratio for province-level yearly change in neonatal mortality (95% CI) | p value | Overall percentage change in neonatal mortality rate, 2000–10 (95% CI) | |
|---|---|---|---|
| Cabo Delgado | 0·928 (0·903–0·954) | <0·0001 | –55·9% (–67·5 to –40·2) |
| Gaza | 0·995 (0·964–1·03) | 0·78 | –4·9% (–33·0 to 35·1) |
| Inhambane | 0·942 (0·909–0·977) | 0·00012 | –48·0% (–65·0 to –22·8) |
| Manica | 0·933 (0·902–0·966) | <0·0001 | –53·3% (–67·9 to –31·9) |
| Maputo City | 1·00 (0·973–1·04) | 0·77 | 5·4% (–26·4 to 51·0) |
| Maputo Province | 1·01 (0·976–1·04) | 0·71 | 6·3% (–23·1 to 47·1) |
| Nampula | 0·864 (0·835–0·894) | <0·0001 | –80·0% (–86·2 to –70·9) |
| Niassa | 0·948 (0·921–0·975) | <0·00025 | –44·7% (–59·7 to –24·1) |
| Sofala | 0·954 (0·927–0·983) | 0·00019 | –40·1% (–56·7 to –17·2) |
| Tete | 0·984 (0·958–1·01) | 0·24 | –16·5% (–38·0 to 12·4) |
| Zambezia | 0·958 (0·933–0·983) | 0·00011 | –37·9% (–53·3 to –17·3) |
| Overall | 0·955 (0·932–0·979) | 0·00027 | –39·4% (–53·8 to –20·7) |
Overall health-workforce density and maternal and child health nurse density were both significantly associated with changes in under-5 and neonatal mortality over time, whereas physician density was not (although all three variables had similar directions and point estimates for effect size). Each ten additional health workers per 100 000 people was associated with a 5·8% (95% CI 1·6–9·9) decrease in under-5 mortality and an 8·1% (0·9–14·7) decrease in neonatal mortality. Each ten additional maternal or child health nurses per 100 000 people was associated with a 4·1% (0·1–8·0) decrease in under-5 mortality and an 8·6% (1·7–14·9) decrease in neonatal mortality (table 5). Infant mortality was not significantly related to any health workforce variables.
Table 5.
Mixed-effects negative binomial regression models of factors associated with provincial-level* changes in under-5, infant, and neonatal mortality rate in Mozambique, 2000–10
| Adjusted rate ratio† for under-5 mortality rate (95% CI) | p value for under-5 mortality rate | Adjusted rate ratio† for infant mortality rate (95% CI) | p value for infant mortality rate | Adjusted rate ratio† for neonatal mortality rate (95% CI) | p value for neonatal mortality rate | |
|---|---|---|---|---|---|---|
|
Health workforce
| ||||||
| Health-workforce density (10-unit change per 100 000) | 0·94 (0·90–0·98) | 0·0074 | 0·96 (0·91–1·01) | 0·095 | 0·92 (0·85–0·99) | 0·028 |
| Physician density (1-unit change per 100 000) | 0·96 (0·90–1·03) | 0·26 | 0·98 (0·91–1·06) | 0·65 | 1·00 (0·89–1·13) | 0·98 |
| Maternal and child health nurse density (10-unit change per 100 000) | 0·96 (0·92–0·99) | 0·045 | 0·97 (0·92–1·02) | 0·20 | 0·91 (0·85–0·98) | 0·015 |
|
| ||||||
|
Health-service
delivery
| ||||||
| Population per health facility (5000-person change) | 1·14 (1·02–1·28) | 0·03 | 1·16 (1·01–1·33) | 0·03 | 1·16 (0·99–1·36) | 0·07 |
| Institutional birth attendance coverage (10% change) | 0·94 (0·90–0·98) | 0·0046 | 0·94 (0·89–0·99) | 0·026 | 0·91 (0·85–0·98) | 0·008 |
|
| ||||||
|
Health financing
| ||||||
| Overall health expenditure per head (10-times change, US$) | 0·87 (0·70–1·09) | 0·23 | 0·88 (0·67–1·15) | 0·33 | 1·13 (0·74–1·72) | 0·57 |
| Government expenditure on health per head (10-times change, US$) | 0·80 (0·65–0·98) | 0·028 | 0·81 (0·64–1·03) | 0·092 | 1·08 (0·74–1·58) | 0·69 |
| Donor common fund expenditure on health per head (10-times change, US$) | 1·03 (0·99–1·08) | 0·18 | 1·03 (0·98–1·10) | 0·25 | 1·02 (0·94–1·12) | 0·60 |
|
| ||||||
|
Other variables
| ||||||
| Regional HIV prevalence in children younger than 5 years (%) | 1·05 (0·98–1·11) | 0·16 | 1·05 (0·97–1·13) | 0·21 | 0·94 (0·95–1·03) | 0·18 |
| GDP per head (10-times change, US$) | 0·92 (0·62–1·36) | 0·67 | 0·91 (0·56–1·46) | 0·69 | 0·82 (0·48–1·42) | 0·49 |
Excludes Maputo City.
Adjusted rate ratios from mixed-effects negative binomial models adjusted for time trend in mortality (2000–10) by use of random intercepts for province and random slope for time.
A larger population per health facility was strongly and consistently associated with higher under-5 mortality over time: each additional 5000 individuals per health facility was associated with a 14% (95% CI 1·5–27·9) increase in under-5 mortality. Institutional birth attendance was also strongly associated with under-5 mortality, with each 10% increase in coverage associated with a 6·1% (1·9–10·1) decrease in under-5 mortality over time. We noted similar directions and effect sizes for infant and neonatal mortality, although population per health facility was not significantly associated with neonatal mortality (p=0·07; table 5).
Each 10-times increase in per-head government expenditure on health was associated with a 20% (95% CI 2·3–34·8) decrease in under-5 mortality, but was not significantly associated with infant or neonatal mortality. Provincial-level GDP, regional HIV prevalence in children younger than 5 years, and other health-financing variables (overall expenditures and donor-funded expenditures) were not significantly associated with changes in under-5, infant, or neonatal mortality over time (table 5).
Discussion
This study is the first analytical assessment of the effects of changes in health-system factors on child mortality in Mozambique. Mozambique has made impressive strides towards achievement of MDG 4 in the past 11 years. However, behind these impressive national-level gains hides substantial heterogeneity in crude and modelled under-5 mortality, and infant and neonatal mortality, at the provincial level (panel). In 2010, Zambezia (131·7 per 1000 livebirths) and Tete (133·3) had roughly 2·5 times the crude child mortality of Inhambane (55·9) or Nampula (52·8). Neonatal mortality shows even stronger disparities, with five of 11 provinces showing decreases of more than 40% (and up to 80%), but four provinces showing no significant improvements over the 11-year period. Subnational disparities in child mortality suggest the need for a more nuanced approach in the post-MDG era, with inequities in health within countries explicitly acknowledged and taken into account in goal setting and the planning of health policy. New methods for investigating population-level trends in health indicators are urgently needed to extend subnational analyses to the district level,28 a level of disaggregation difficult to achieve with existing designs of large-scale community surveys (DHS and MICS).
The findings from our longitudinal subnational study corroborate the results of previous large, cross-national studies exploring health-facility factors and their relation to under-5 mortality, showing that higher health workforce densities and skilled birth attendance coverage are related to lower under-5 and neonatal mortality.8,15,29 Our finding that the effect sizes of increases in overall public-sector health-workforce density, maternal and child health nurse density, and institutional birth attendance coverage were strongly associated with reductions in neonatal mortality should be of particular interest to policy makers—these variables represent opportunities for future resource allocation if decreasing neonatal mortality is a priority.
Encouragingly, every province in Mozambique had increases in health-workforce density and only one province (Gaza) did not increase birth attendance coverage between 2000 and 2010. In 2011, 98% of primary health facilities were implementing the Integrated Management of Childhood Illnesses strategy as the main child survival strategy, which was introduced in 1999. In addition to new vaccine introduction (hepatitis B and Haemophilus influenzae type b), third-dose diphtheria, pertussis, and tetanus coverage has increased from an estimated 68% in 1999 to 76% in 2012.30 Despite these increases, Mozambique continues to rank among the lowest countries worldwide in terms of health worker to population density,31 which as we have shown varies dramatically across the country. This scarcity of trained human resources is compounded by insufficient resources to train and retain health workers in the public sector,32 as well as brain drain and internal migration of qualified health workers from the National Health Service.33 Efforts to address the scarcity of trained public-sector health workers, as well as to ensure their rational distribution, deserve renewed attention, especially in view of our findings that provinces with higher densities of health workers achieved greater reductions in under-5 mortality. For example, Tete Province continues to have among the highest under-5, infant, and neonatal mortality in Mozambique and had only a 10% increase in health-worker density over the study period, contrasting with a national increase of 32%. Massive long-term investments are needed to sustainably increase the capacity of health training centres, with commensurate political will to address funding and policy constraints to workers’ entry into the National Health Service.32,34 Strategies to promote equitable distribution of health workers within Mozambique are needed to maximise the return on investments in workforce expansion, and could include incentives to maintain health professionals in the public sector working in neglected areas through increased salaries and improved working conditions.
Of the significant predictors identified through our models, only population per health facility was trending in the wrong direction over the 11-year period: eight of 11 provinces had increases in population served per facility, which was a significant predictor of increased child death. Although expensive and time-consuming, the need for continued investment in the expansion of health infrastructure to meet existing and future population needs is clear. In the interim, innovative approaches to rapidly decrease the absolute or effective number of people served by each health facility are needed. Such approaches could include improvement of networks between community, primary, and referral facilities; investments in trained and salaried community health workers; and operations research to optimise patient flow through facilities.
By contrast with our assumption and results from previous cross-national studies,15 we did not identify an association between GDP per head or overall health expenditures and under-5 mortality. The relation between per-head GDP and health has generated controversial (and still unresolved) debates, centred on the potential for reverse causality and the effects of subnational income inequality on health not captured through crude measures of per-head GDP.35 Recent study findings suggest a very small to null association between increases in per-head GDP and reductions in early childhood undernutrition across countries36—results that support our findings in the present study.
However, we did note a significant association between increased government health financing and decreased under-5 mortality over the 11-year period. Increased government budget resources reflect the expansion of the national health system to support salaries and other health-facility running costs. Donor common fund resources represent a precious, but still limited, supplement to existing government resources, especially for disadvantaged provinces. Moreover, common fund resources might be non-significant in our analyses because they are often targeted to the acquisition of equipment, biotechnology, and drugs, which are often centralised at the national level and therefore excluded from the present study. Overall, our findings suggest that, in settings where access to services remains poor, economic improvement might not necessarily translate into health improvements unless increased resources are channelled into equitable and sustained expansion of public health services.
Further contrary to our assumption, HIV prevalence was not related to changes in under-5 mortality over time. This finding could be a result of our use of regional prevalence of HIV among children younger than 5 years rather than provincial-level data, which could have resulted in inflated variances and undermined our ability to detect an effect even if one was present. Additionally, the widespread introduction of combination antiretroviral therapy and programmes to prevent mother-to-child transmission during the same time period as our study (2000–10) might have hindered our ability to detect an association between HIV and under-5 mortality.
Our study has several important limitations. First, the use of DHS and MICS data limited subnational analyses to the provincial level, masking potential district-level heterogeneity in mortality outcomes. Second, the use of these data sources also limited the statistical power of our analyses, precluding the use of rigorous multi variable analyses. Third, survey teams, methods, and implementation might differ between community survey types (DHS vs MICS) or DHS surveys done at different times, in addition to recall or other reactive biases of respondents. Together, these issues could lead to bias in our estimates of mortality estimates extracted by use of retrospective full birth history data. In the present study, most estimates of under-5 mortality matched well over time—that is, overlapping estimates of under-5 mortality were similar for DHS data from 2003, DHS data from 2011, and MICS data from 2008. However, we noted that Inhambane and Nampula had consistently lower estimates of under-5 mortality from the DHS 2011 than from either the DHS 2003 or the MICS. We anticipate that combining these overlapping estimates provides the best estimate of the truth, but we hypothesise that the estimates from DHS 2011 for Inhambane and Nampula are spuriously low on the basis of our in-country experience. More generally, the fact that these community surveys show large discrepancies and represent the only data source for under-5, and other, mortality estimates available for decision making is concerning and suggests the need for new approaches in the future. A further limitation is the absence of data for potential explanatory variables of interest, including causes of child death and health service coverage, which could help to account for the relative differences in changes in mortality estimates over time within provinces. Because these data are generally available only intermittently through community surveys, they could not be included without multiple imputation efforts. As a result, the potential exists for confounding in our assessment of the relation between mortality estimates and health-system factors.
Despite these limitations, our study has some notable strengths. Using both community surveys and routine Ministry of Health data sources, we were able to include a range of potential explanatory variables to address an important and relevant question for countries striving to structure their health systems to accelerate improvements in population health, including decreased under-5, infant, and neonatal mortality. Furthermore, the longitudinal and subnational nature of the analysis allowed us to describe improvements over time, and estimate associations between health-system factors and rates of change in child mortality across meaningful administrative units in Mozambique.
Overall, our findings show that Mozambique made substantial progress in the reduction of child, infant, and neonatal mortality between 2000 and 2010. However, national success masks continued inequalities at the subnational level. Some of the improvements in child mortality seem to be attributable to the expansion of the national health system, particularly improvements in public-sector human resources for health, increased institutional birth coverage, and increased government health expenditures. A significant predictor of child death that warrants further attention in Mozambique, and potentially in other low-income and middle-income countries, is the number of individuals served by each health facility. New and different methods to accurately estimate trends in under-5 mortality at subprovincial levels are urgently needed to track and target health disparities within low-income and middle-income countries.
Panel: Research in context.
Systematic review
We searched PubMed and Google Scholar for English and Portuguese reports, published between 1966 and 2014, of longitudinal studies examining the effect of changes in health-system factors on child mortality in low-income and middle-income countries similar to Mozambique. Search terms used included “health systems”, “health systems strengthening”, “systems”, “workforce”, “human resources”, “HIV”, and “under-5 mortality”, “infant mortality”, “neonatal mortality”, “MDG4”, and “child death”. Most previous studies are cross-national in nature and few (if any) use data resolution below the national level. Existing cross-national studies8,15,29 suggested that health workforce densities and skilled birth attendance were associated with lower under-5 and neonatal mortality rates.
Interpretation
The results of our study show that Mozambique made impressive progress in reducing deaths among children younger than 5 years between 2000 and 2010, with all provinces showing significant reductions. Infant mortality has fallen significantly in eight of 11 provinces, and neonatal mortality has fallen significantly in seven of 11 provinces, showing the continuing (and in some cases widening) gaps in health status between provinces. Our analyses suggest that these large gains in child mortality were most strongly related to improvements in public-sector health workforce density, institutional birth coverage, and increases in government financing for health. These findings add to increasing evidence from other longitudinal cross-national studies8,15,29 that emphasises the fundamental importance of public-sector human resources underlying improvements in population health.
Acknowledgments
This work was supported by the African Health Initiative of the Doris Duke Charitable Foundation and the Mozambican National Institute of Health. KS was supported by a grant from the Fogarty International Center (US National Institutes of Health [NIH]; K02TW009207). QFF was supported by the International AIDS Research and Training Program through a grant from the Fogarty International Center (D43 TW000007). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Contributors
QFF, BHW, JP, SG, and KS formulated the research question and analysis plan. QFF and BHW did the data analysis, with creative input from KS. QFF drafted first version of the report, with creative input from BHW and KS. LA provided support for the analysis of expenditure data. All authors read and approved the final report.
Declaration of interests
We declare no competing interests.
References
- 1.UNICEF, WHO, World Bank, UN. Levels and trends in child mortality report 2012—estimates developed by the UN interagency group for child mortality estimates. New York: United Nations Children’s Fund; 2013. [Google Scholar]
- 2.Ministério de Saúde. Inquérito demográfico e de saúde 2011. Maputo, Mozambique: Instituto Nacional de Estatística and Ministério da Saúde Maputo; 2013. [Jan 23, 2014]. http://measuredhs.com/pubs/pdf/PR14/PR14.pdf. [Google Scholar]
- 3.Mazive E, Nhapure G, Duce P, et al. Mortalidade em Moçambique inquérito nacional sobre causas de mortalidade, 2007/8. Maputo, Mozambique: Instituto Nacional de Estatística; 2009. [Google Scholar]
- 4.Mozambique National Institute of Statistics, US Census Bureau, MEASURE Evaluation, US Centers for Disease Control and Prevention. Mortality in Mozambique: results from a 2007–2008 postcensus mortality survey. Chapel Hill: MEASURE Evaluation; 2012. [Google Scholar]
- 5.Travis P, Bennett S, Haines A, et al. Overcoming health-systems constraints to achieve the Millennium Development Goals. Lancet. 2004;364:900–06. doi: 10.1016/S0140-6736(04)16987-0. [DOI] [PubMed] [Google Scholar]
- 6.Masanja H, de Savigny D, Smithson P, et al. Child survival gains in Tanzania: analysis of data from demographic and health surveys. Lancet. 2008;371:1276–83. doi: 10.1016/S0140-6736(08)60562-0. [DOI] [PubMed] [Google Scholar]
- 7.Wang L. Determinants of child mortality in LDCs: empirical findings from demographic and health surveys. Health Policy. 2003;65:277–99. doi: 10.1016/s0168-8510(03)00039-3. [DOI] [PubMed] [Google Scholar]
- 8.Muldoon KA, Galway LP, Nakajima M, et al. Health system determinants of infant, child and maternal mortality: a cross-sectional study of UN member countries. Global Health. 2011;7:42. doi: 10.1186/1744-8603-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anand S, Bärnighausen T. Human resources and health outcomes: cross-country econometric study. Lancet. 2004;364:1603–09. doi: 10.1016/S0140-6736(04)17313-3. [DOI] [PubMed] [Google Scholar]
- 10.Stuckler D, Basu S, McKee M. Drivers of inequality in Millennium Development Goal progress: a statistical analysis. PLoS Med. 2010;7:e10000241. doi: 10.1371/journal.pmed.1000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macassa G, Ghilagaber G, Charsmar H, Walander A, Sundin Ö, Soares J. Geographic differentials in mortality of children in Mozambique: their implications for achievement of Millennium Development Goal 4. J Health Popul Nutr. 2012;30:331–45. doi: 10.3329/jhpn.v30i3.12297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alberto SA, Machado CJ, do Nascimento Rodrigues R. Associação Brasileira de Estudos Populacionais. Belo Horizonte, Brasil: 2010. [Jan 23, 2014]. Fatores associados à mortalidade infantil em Moçambique, 1998 a 2003. http://www.abep.nepo.unicamp.br/encontro2010/docs_pdf/tema_4/abep2010_2631.pdf. [Google Scholar]
- 13.Machavane CA, Muanamoha R. Dissertations of University Eduardo Mondlane. Maputo, Mozambique: Scientific Repository of Mozambique; 2013. [Jan 23, 2014]. Factores de risco de mortalidade infantil na regiao norte de mocambique: avaliacao de diferenciais neonatal e pos-neonatal. http://www.saber.ac.mz/handle/10857/4013. [Google Scholar]
- 14.Millard AV. A causal model of high rates of child mortality. Soc Sci Med. 1994;38:253–68. doi: 10.1016/0277-9536(94)90395-6. [DOI] [PubMed] [Google Scholar]
- 15.Houweling TAJ, Kunst AE, Looman CWN, Mackenbach JP. Determinants of under-5 mortality among the poor and the rich: a cross-national analysis of 43 developing countries. Int J Epidemiol. 2005;34:1257–65. doi: 10.1093/ije/dyi190. [DOI] [PubMed] [Google Scholar]
- 16.Ministério da Saúde. Relatório da revisão do sector de Saúde. Maputo, Moçambique: Ministério da Saúde; 2012. [Jan 23, 2014]. http://www.healthsystems2020.org/content/resource/detail/96661/ [Google Scholar]
- 17.Direcção de Planificação e Cooperação. Relatório da avaliação conjunta anual do desempenho do sector de saúde—2011. Maputo, Moçambique: Ministério de Saúde, Direcção de Planificação e Cooperação; 2012. [Jan 23, 2014]. http://www.internationalhealthpartnership.net/fileadmin/uploads/ihp/Documents/Country_PagesMozambique/Mozambique%20JAR%202011.pdf. [Google Scholar]
- 18.Direcção de Recursos Humanos. Relatorio anual—2011. Maputo, Moçambique: Ministério da Saúde; 2012. [Google Scholar]
- 19.MEASURE DHS. [Jan 23, 2014];Demographic and Health Surveys. http://www.dhsprogram.com/
- 20.UNICEF. Statistics and monitoring: Multiple Indicator Cluster Survey. [Jan 23, 2014];United Nations Children’s Fund, 2012. http://www.uniceforg/statistics/index_24302.html.
- 21.O’Donnell O, Doorslaer EV, Wagstaff A, Lindelow M. WBI Learning Resources Series. Washington, DC: World Bank; 2008. Analyzing health equity using household survey data: a guide to techniques and their implementation. [Google Scholar]
- 22.WHO. Everybody’s business—strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: World Health Organization; 2007. [Google Scholar]
- 23.Gimbel S, Micek M, Lambdin B, et al. An assessment of routine primary care health information system data quality in Sofala Province, Mozambique. Popul Health Metr. 2011;9:12. doi: 10.1186/1478-7954-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Instituto Nacional de Estatistica. Projecções anuais da população total, urbana e rural (2007–2040) por Provincia. Maputo, Moçambique: Instituto Nacional de Estatistica, Direcção de Estatísticas Demográficas, Vitais e Sociais; 2010. [Google Scholar]
- 25.Instituto Nacional de Estatistica. Projecções Anuais da População por Província e Área de Residência, 1997–2015 (Revisto 2004) Maputo, Moçambique: Instituto Nacional de Estatistica, Direcção de Estatísticas Demográficas, Vitais e Sociais; 2004. [Google Scholar]
- 26.Direcção de Administração e Finanças. Relatórios de execução orçamental de 2000 ate 2010. Maputo, Moçambique: 2011. [Jan 23, 2014]. http://www.dno.gov.mz/docs/orc_estado/execucao/Relatorio_Execucao_Jan_Dez_OE2011.pdf. [Google Scholar]
- 27.Instituto Nacional de Saúde, Instituto Nacional de Estatística. Vigilância epidemiológica do HIV e seu impacto demográfico em Moçambique. Maputo: Grupo Técnico Multisectorial de Combate ao HIV/SIDA; 2009. [Google Scholar]
- 28.Victora C, Black R, Boerma J, Bryce J. Measuring impact in the Millennium Development Goal era and beyond: a new approach to large-scale effectiveness evaluations. Lancet. 2011;377:85–95. doi: 10.1016/S0140-6736(10)60810-0. [DOI] [PubMed] [Google Scholar]
- 29.Farahani M, Subramanian S, Canning D. The effect of changes in health sector resources on infant mortality in the short-run and the long-run: a longitudinal econometric analysis. Soc Sci Med. 2009;68:1918–25. doi: 10.1016/j.socscimed.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 30.GAVI Alliance. Mozambique DTP3 / immunisation coverage. Geneva: GAVI Alliance; 2014. [June 3, 2014]. http://www.gavialliance.org/country/mozambique/ [Google Scholar]
- 31.WHO. The world health report 2006: working together for health. Geneva: World Health Organization; 2006. [Google Scholar]
- 32.Stuckler D, Basu S, Gilmore A, et al. An evaluation of the International Monetary Fund’s claims about public health. Int J Health Serv. 2010;40:327–32. doi: 10.2190/HS.40.2.m. [DOI] [PubMed] [Google Scholar]
- 33.Sherr K, Mussa A, Chilundo B, et al. Brain drain and health workforce distortions in Mozambique. PLoS One. 2012;7:e35840. doi: 10.1371/journal.pone.0035840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ooms G, Schrecker T. Expenditure ceilings, multilateral financial institutions, and the health of poor populations. Lancet. 2005;365:1821–23. doi: 10.1016/S0140-6736(05)66586-5. [DOI] [PubMed] [Google Scholar]
- 35.Deaton A. Health, inequality, and economic development. J Econ Lit. 2003;41:113–58. [Google Scholar]
- 36.Vollmer S, Harttgen K, Subramanyam MA, Finlay J, Klasen S, Subramanian SV. Association between economic growth and early childhood undernutrition: evidence from 121 Demographic and Health Surveys from 36 low-income and middle-income countries. Lancet Glob Health. 2014;2:e225–34. doi: 10.1016/S2214-109X(14)70025-7. [DOI] [PubMed] [Google Scholar]


