Abstract
Background
We describe trends in childhood mortality in Kenya, paying attention to the urban–rural and intra-urban differentials.
Methods
We use data from the Kenya Demographic and Health Surveys (KDHS) collected between 1993 and 2008 and the Nairobi Urban Health and Demographic Surveillance System (NUHDSS) collected in two Nairobi slums between 2003 and 2010, to estimate infant mortality rate (IMR), child mortality rate (CMR) and under-five mortality rate (U5MR).
Results
Between 1993 and 2008, there was a downward trend in IMR, CMR and U5MR in both rural and urban areas. The decline was more rapid and statistically significant in rural areas but not in urban areas, hence the gap in urban–rural differentials narrowed over time. There was also a downward trend in childhood mortality in the slums between 2003 and 2010 from 83 to 57 for IMR, 33 to 24 for CMR, and 113 to 79 for U5MR, although the rates remained higher compared to those for rural and non-slum urban areas in Kenya.
Conclusions
The narrowing gap between urban and rural areas may be attributed to the deplorable living conditions in urban slums. To reduce childhood mortality, extra emphasis is needed on the urban slums.
Keywords: Infant mortality, Child mortality, Under five mortality, Urban slums, Sub-Saharan Africa
1. Introduction
Marked progress towards achieving the millennium development goal target of reducing mortality of children under the age of five years by two thirds between 1990 and 2015 has been experienced globally. A recent report by the United Nations Inter-agency Group for Child Mortality Estimation (UN-IGME) indicates that the number of deaths among children under five (U5) worldwide declined from 12 million deaths per year in 1990 to approximately seven million deaths per year in 2011. This translates to a 41% decline in U5 mortality from 87 per 1000 live births in 1990 to 51 per 1000 live births in 2011. However, this reduction was not uniform across countries and regions. The greatest reduction (of over 50%) was experienced in Eastern Asia, Northern Africa, Latin America and the Caribbean, South Eastern Asia and Western Asia. Sub-Saharan Africa (SSA) had the slowest rate of reduction at only 39%, and the highest rates of U5 mortality are still found in the region. One in nine children in SSA dies before they reach the age of five years (Inter-agency, 2012, United Nations, 2013). The regional disparities may be attributable to intra-urban disparities in health, environmental and social conditions (African Population and Health Research Center, 2002a, African Population and Health Research Center, 2002b, Magadi, 2004, Kimani-Murage and Ngindu, 2007, Fotso et al., 2009, Madise N. et al., 2012).
Rapid urbanization has been experienced globally. The world urban population crossed the 50% mark in 2009, and it is projected that increases in the world׳s population will be concentrated in urban areas of the less developed regions of the world including Africa (United Nations, 2010). For example, it is projected that the urban population will increase by 2.6 billion by 2050, and that most of the expected urban growth will be in urban areas of the least developed countries (United Nations, 2012). Whilst SSA has enjoyed sustained economic growth during the last one to two decades, the region still has the highest rate of poverty with 47.5% of the population living on only $1.25 a day, and accounts for 30% of the most poor in the world (World Bank, 2012/2013). Rapid growth of the urban population in a context marked by inadequate urban planning and limited service provision has led to the mushrooming of slums(Brockerhoff and Brennan, 1998, National Research Council, 2003, Cohen, 2006). As a result, the majority (62% in 2010) of urban residents in sub-Saharan Africa live in overcrowded slums and shantytowns (Unhabitat, 2008), characterized by very poor housing conditions, inadequate water and sanitation infrastructure, poor livelihood opportunities, and limited education, health and other social services (African Population and Health Research Center, 2002a, African Population and Health Research Center, 2002b, Magadi, 2004, Kimani-Murage and Ngindu, 2007).
Living conditions, health and lifestyle are associated with place of residence (Montgomery and Hewett, 2005, Sampson et al., 2002). For a long time, a comparative advantage of urban residence over rural residents with regards to health outcomes has been assumed because many conditions that influence health, including health care services, water and sanitation infrastructure, and good housing, have been more common in urban than in rural areas (Sastry, 1997, Lalou and LeGrand, 1997). However, the growth of slums settlements in many low income countries (Brockerhoff and Brennan, 1998, National Research Council, 2003, Cohen, 2006) has led to a larger proportion of urban residents now living in unfavorable conditions (Sastry, 2004). The substantial proportion of urban residents living under squalid conditions in slums puts into question the long held view of an urban advantage in health.
Previous studies show poor child health outcomes in Kenya. For example, high levels of child malnutrition have been documented with the national prevalence of stunting at 35% (Kenya National Bureau of Statistics (KNBS) and ICF Macro, 2009). Health care service utilization is also low and, according to the Kenya Demographic and Health Survey (KDHS) 2008/09, only 56% of children with acute respiratory infections (ARI) received care from a health care provider, while only 43% of women gave birth at a health facility (Kenya National Bureau of Statistics (KNBS) and ICF Macro, 2009). The urban population in Kenya is growing at a rapid rate of 4%; with the proportion of the urban population in Kenya estimated at 22% in 2010 (Unhabitat, 2008). Given the rapid growth of the urban population and the fact that the majority of urban residents in Kenya live in slums (Unhabitat, 2003), health indicators in urban slums are likely to determine urban health indicators and also national health indicators.
Evidence from the Kenya Demographic and Health Surveys conducted in 2008 indicates that while urban areas still fare better in some child health related outcomes, they fare worse in others. There is higher prevalence of delivery at a health facility in urban areas (75%) compared with rural areas (35%). Additionally, there is a lower prevalence of malnutrition in children aged less than five years in urban areas (26%) compared with rural areas (37%). Breastfeeding practices seem to be worse in urban areas compared with rural areas. For example, the median duration of exclusive breastfeeding is 0.6 months in urban areas compared with 1.0 months in rural areas. A similar proportion of children in urban areas are born with low birth weight as that in rural areas (6% vs. 5%, respectively), and have diarrhea (17% vs. 17%). Although a slightly higher proportion of children 12–23 months in urban areas (81%) and are reported to have received all basic vaccinations compared with rural areas (76%), a substantially higher proportion of children in rural areas (75%) have a vaccination card compared with urban areas (55%) (Kenya National Bureau of Statistics (KNBS) and ICF Macro, 2009). Poor health outcomes have been documented among the urban poor. Evidence has shown that urban poor children have a higher prevalence of diarrhea (31%) compared with their rural counterparts (17%). Again, urban poor children are less likely to be fully immunized (44%) compared with their rural counterparts (64%) (African Population and Health Research Center, 2002).
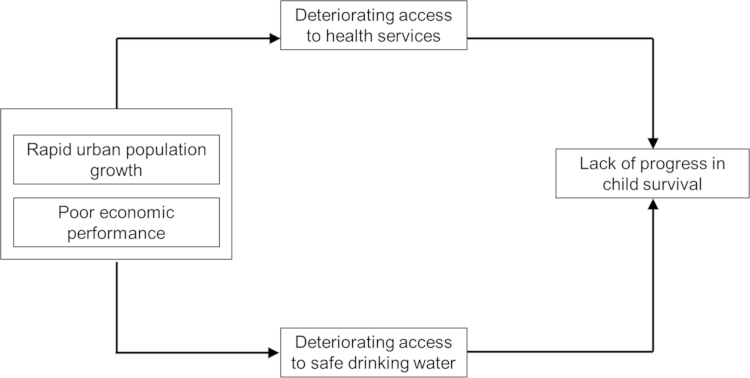
In this study, we examine trends in under-five mortality in Kenya, paying particular attention to the changes in urban–rural differentials over time. The study also draws on data collected in Nairobi slums to illustrate the within urban differentials using a place-based definition of the urban poor. To guide our interpretation, we draw on a conceptual framework develop by Fotso and colleagues (Fotso et al., 2007); which posits that rapid urbanization unmatched by similar rates of growth in the economy leads to poor access to water and sanitation infrastructure and limited health service utilization resulting in stagnating or worsening child mortality rates (Appendix 1). We also rely on an extensive pool of literature that demonstrates a strong association between health outcomes and neighborhood characteristics (or ‘neighborhood effects’), including residence in areas marked by pervasive poverty, limited land ownership, and poor access to services and amenities (Montgomery and Hewett, 2005, Sampson et al., 2002, Weeks et al., 2006, Fotso et al., 2012). For example, Weeks et al. (2006), observed spatial variability in child mortality rates within Accra, the capital city of Ghana, that was strongly associated with neighborhood ethnic concentrations and ethnic differences in socio-economic status. Fotso et al. (2012) examined how patterns of child growth are influenced by household poverty in urban poor settings in Kenya and concluded that different aspects of household poverty affect child growth differently. They also found that unexpectedly, household environmental index was not associated with child growth, implying that, in the urban slums, water and sanitation and other household living conditions do not affect children׳s growth patterns, possibly due to little variation in household amenities in these settings (Fotso et al., 2012). To explain the differences in mortality rate by area of residence, we compare urban–rural differences in various factors that are associated with childhood mortality such as adolescent child bearing, breastfeeding, immunization, use of insecticide treated nets (ITNs), childhood illnesses such as diarrhea, health care seeking for childhood illnesses, and access to improved sources of drinking water and sanitation (Fotso et al., 2007) (Kleinschmidt et al., 2009, Demombynes and Trommlerova, 2010, Demombynes and Trommlerova, 2010, Ndirangu et al., 2010, Kayode et al., 2012). For example, optimal breastfeeding is associated with a 13% reduction in under five mortality while ITNs are associated with a 7% reduction (Gareth et al., 2003). Further, Demombynes and Trommlerová attributed 58% of decline in infant mortality in Kenya to ownership of ITNs in malaria endemic areas and about 6% to improved access to sanitation facilities (Demombynes and Trommlerova, 2010, Demombynes and Trommlerova, 2010)
2. Data and methods
2.1. Data and sources
The study uses two data sources: (i) Secondary data collected through Demographic and Health Surveys (DHS) in Kenya in four panels (i.e. 1993, 1998, 2003 and 2008); and (ii) Data collected under the Nairobi Urban Health and Demographic Surveillance System (NUHDSS) between January 2003 and December 2010 (Emina et al., 2011).
2.2. Kenya demographic and health surveys data
The DHS are nationally-representative household surveys conducted in approximately 75 countries that provide data on a wide range of indicators including mortality, sexual and reproductive health, health status and health seeking and child nutrition. We reconstructed childhood mortality trends using data from the 1993, 1998, 2003, and 2008/09 KDHS. From each survey, births that occurred within 15 years preceding the date of survey were included in the analysis. The data therefore cover a 30-year period between 1979 and 2008, and are grouped into six cohorts (1979–1983, 1984–1988, 1989–1993, 1994–1998, 1999–2003 and 2004–2008) corresponding to six birth periods, as illustrated in Table 1. For example, births for the first cohort (1979–1983) are retrieved from the 1993 DHS (10–14 years preceding the survey), while those corresponding to the second cohort (1984–1988) are from the 1993 DHS (5–9 years preceding the survey) and the 1998 DHS (10–14 years preceding the survey). Mortality rates for each time period (except the first and the last) draw from data from multiple surveys, and yields estimates that are more robust than those from a single survey.
Table 1.
Number of births by five-year cohort and place of residence at birth; Kenya DHS 1993, 1998, 2003 and 2008/09.
| Period of birtha | 1979–1983 | 1984–1988 | 1989–1993 | 1994–1998 | 1999–2003 | 2004–2008 | Total |
|---|---|---|---|---|---|---|---|
| Time | 1 | 2 | 3 | 4 | 5 | 6 | |
| Data source | |||||||
| DHS 1993 | 121–180 months prior to the survey (N=5001) | 61–120 months prior to the survey (N=6130) | 1–60 months prior to the survey (N=5937) | 17,068 | |||
| DHS 1998 | 121–180 months prior to the survey (N=5003) | 61–120 months prior to the survey (N=5393) | 1–60 months prior to the survey (N=5485) | 15,881 | |||
| DHS 2003 | 121–180 months prior to the survey (N=4433) | 61–120 months prior to the survey (N=5032) | 1–60 months prior to the survey (N=5807) | 15,272 | |||
| DHS 2008 | 121–180 months prior to the survey (N=4406) | 61–120 months prior to the survey (N=5395) | 1–60 months prior to the survey (N=5961) | 15,762 | |||
| Total | 5001 | 11,133 | 15,763 | 14,923 | 11,202 | 5961 | 63,983 |
| Place of residence at birth | |||||||
| Urban | 516 | 1229 | 2402 | 2945 | 2521 | 1363 | 10,976 |
| Rural | 4485 | 9904 | 13,361 | 11,978 | 8681 | 4598 | 53,007 |
The data covers a period of 30 years – children born between 1979 and 2008.
2.3. Estimating mortality from the KDHS data
The outcome measures include infant mortality, child mortality and under five mortality. We estimated infant mortality rates (IMR) for children aged 0–11 months, child mortality rates (CMR) for children aged 12–59 months, and under-five mortality rates (U5MR) for children aged 0–59 months, by cohort and place of residence at birth (urban or rural), using the direct method based on the date of birth, survival status of the child, and the date of death or age at death (where this applied). Trends in mortality by area of residence were assessed using Cox regression. The place of residence at birth was reconstructed from the following variables: age of the index child, current place of residence of the mother, length of stay of the mother at the current place of residence, and previous place of residence of the mother. The residence at birth was taken to be the same as current place of residence if age of the child was less than the mother׳s duration of stay at the current residence and the same as the previous place of residence if age of the child was greater than the mother׳s duration of stay at the current residence. The data do not allow us to consider within urban movement so we only considered urban/rural residence. We did not use information on change of residence of the child since birth since only a negligible number of children (n=50; i.e. <0.1%) had changed residence from urban to rural or the other way round. All the analyses were conducted using STATA version 12.
2.4. Explanatory measures
We compare urban–rural differences in the following indicators: adolescent childbearing, median duration of exclusive breastfeeding, median duration of any breastfeeding, child immunization rates, use of insecticide treated nets (ITNs), percentage of children with diarrhea, percentage of children with acute respiratory infections (ARI) taken to health facilities, and improved access to drinking water and sanitation. Improved access to drinking water was defined as water from sources including piped water, bottled water, tube-well/borehole and protected wells and springs, while improved sanitation was defined as toilet facilities including toilets with a flush to sewer, septic tank or to a pit latrine, and ventilated improved pit latrines. The definition of the other indicators are described in detail in the guide to DHS statistics (Rutstein and Rojas, 2006).
2.5. Nairobi Urban Health and Demographic Surveillance System (NUHDSS) data
The NUHDSS is carried out in two urban slums (Korogocho and Viwandani) in Nairobi, Kenya by the African Population and Health Research Center (APHRC). The two slum areas are densely populated (63,318 and 52,583 inhabitants per square km, respectively), and are characterized by poor housing, lack of basic infrastructure, violence, insecurity, high unemployment rates, and poor health indicators (African Population and Health Research Center, 2002a, African Population and Health Research Center, 2002b, Mutua et al., 2011, Mutua et al., 2011). The NUHDSS involves a systematic recording of vital demographic events including births, deaths and migrations occurring among residents of all households in the surveillance area thrice a year since 2003. Individuals qualify to become Demographic Surveillance System (DSS) residents either through baseline enumeration, in-migration or birth (Emina et al., 2011). We limited our analysis to an open cohort of individuals observed within the NUHDSS area between 01 January 2003 and 31 December 2010 (n=36,952). We estimated their mortality rates by calculating the ratio of the number who died within the appropriate age interval (e.g. within one year of birth for infant mortality) and person years of exposure.
2.6. Estimating mortality from the NUHDSS data
Based on their total survival time, we estimated the probability of dying at one year and 5 years of age respectively (infant, and under 5 mortality), and the probability of dying between 1 and 4 years of age (child mortality). During the observation period, 3691 deaths occurred in the DSS with 790 deaths occurring at between birth and exactly the age of one year, with a total cohort survival time of 12,540 person-years resulting in a probability of dying of 0.0691 (69.1 per 1000 live births). A total of 367 deaths occurred between birth and exactly the age of 5 with total cohort survival time of 11,510 person-years resulting in a probability of dying of 0.0959 (95.9 per 1000 live births). We then calculated mortality rates as the number of deaths divided by the number of population at risk during a certain period of time. The probability of death was derived from a life table (Appendix 3). We estimated IMR as the probability of a child born in a specific year dying at exactly the age of one, if subject to age-specific mortality rates of that period; CMR as the probability of a child born in a specific year dying at exactly the age of five, having survived up to age one, if subject to age-specific mortality rates of that period; and U5MR as the probability of a child born in a specific year dying at exactly the age of five, if subject to age-specific mortality rates of that period.
3. Results
3.1. Child mortality trends in Kenya by urban–rural place of residence: evidence from KDHS
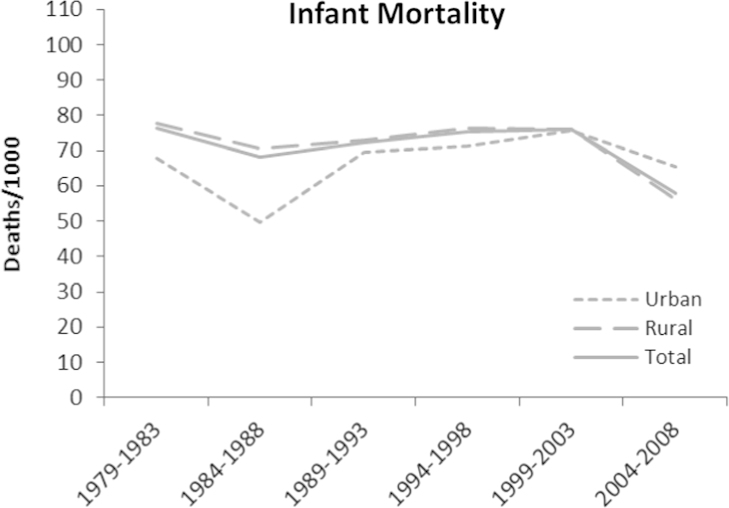
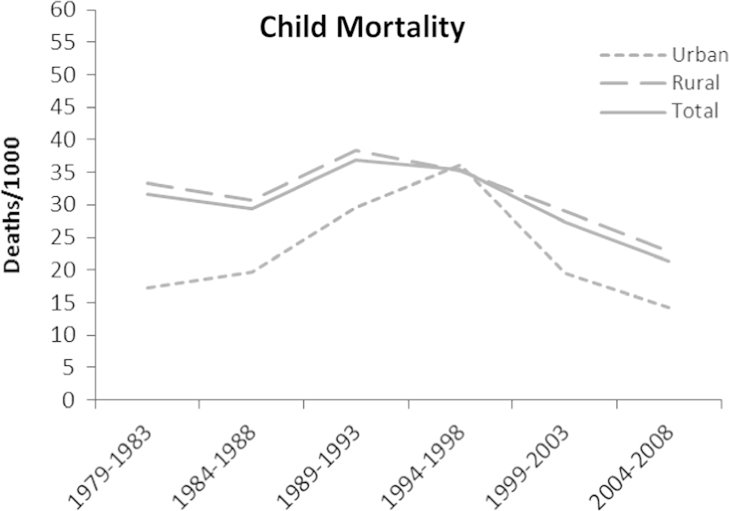
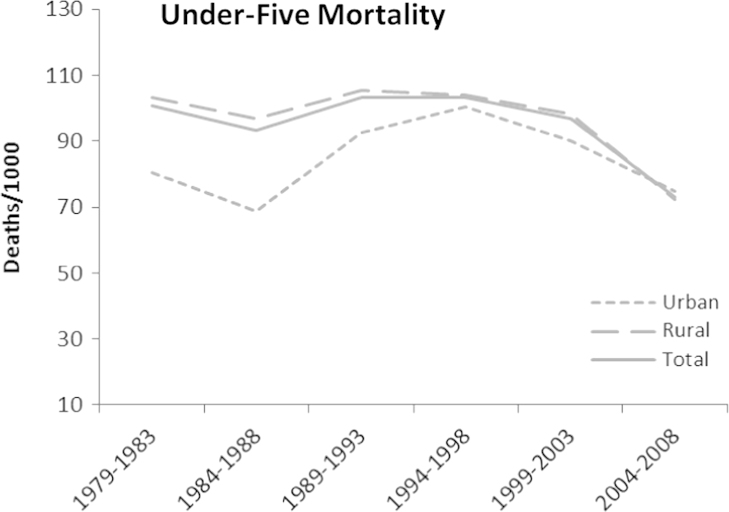
The KDHS generated a total of 63,983 live births, 53,007 in rural areas and 10,976 in urban areas (Table 1). The results show a general significant decline in all the forms of childhood mortality (infant, child and under five) over the 30 year period between 1979 and 2008 (Table 2). IMR declined from 76.5 (95% CI 69.5; 84.2) to 57.9 (95% CI 52.1; 64.4); CMR from 31.7 (95% CI 27.1; 37.2) to 21.3 (95% CI 16.7; 27.0); while U5MR declined from 100.7 (95% CI 92.7; 109.4) to 72.9 (95% CI 65.8; 80.8). The hazard ratios for IMR, CMR and U5MR for Kenya as a whole in 2004–2008 compared with 1979–1983 were 0.76, 0.73 and 0.78 respectively (p<0.05, respectively), indicating a reduction in childhood mortality rates over time. The hazard ratio for infant mortality reduced to 0.88 for the period 1984–1988, while for child mortality increased to 1.20 in the period 1989–1993 (p<0.05). For the other periods, though there seemed to be a reduction in the hazard ratio relative to 1979–1983, it was not statistically significant (Table 3). The pattern indicates that generally for IMR and U5MR, there was a decline in mortality from 1979–1983 to 1984–1988, an increase in the mid to late 1980s, a stall in the 1990s, then a decline in the 2000s. Child mortality shows a slightly different pattern with an increase from 1979–1983 until roughly around the period 1989–1993, then declining in the succeeding periods.
Table 2.
Long-term child mortality trends by place of residence at birth; Kenya DHS 1993, 1998, 2003 and 2008/09. (infant mortality:0–11 months per 1000 live births; child mortality: 12–59 months per 1000 live births; under five mortality: 0–59 months per 1000 live births).
| Period of birth | 1979–1983 | 1984–1988 | 1989–1993 | 1994–1998 | 1999–2003 | 2004–2008 |
|---|---|---|---|---|---|---|
| Time | 1 | 2 | 3 | 4 | 5 | 6 |
| Infant mortality | ||||||
| Urban | 67.9 | 49.6 | 69.4 | 71.2 | 75.7 | 65.4 |
| (95% CIa) | (49.4; 92.9) | (39.3; 62.6) | (59.9; 80.4) | (62; 81.7) | (64.9; 88.1) | (51.7; 82.6) |
| Rural | 77.6 | 70.5 | 72.8 | 76.2 | 75.9 | 56.3 |
| (95% CI) | (70.1; 85.8) | (65.6; 75.7) | (68.5; 77.4) | (71.6; 81.2) | (70.7; 81.5) | (49.9; 63.4) |
| Total Kenya | 76.5 | 68 | 72.3 | 75.3 | 75.9 | 57.9 |
| (95% CI) | (69.5; 84.2) | (63.4; 72.8) | (68.3; 76.5) | (71.2; 79.7) | (71.1; 80.9) | (52.1; 64.4) |
| Rural/urban ratio | 1.14 | 1.42 | 1.05 | 1.07 | 1.00 | 0.86 |
| Child mortality | ||||||
| Urban | 17.3 | 19.6 | 29.5 | 36.2 | 19.5 | 14.2 |
| (95% CI) | (8.9; 33.6) | (13.3; 28.8) | (23.0; 38.0) | (29.1; 45.0) | (13.7; 27.8) | (7.5; 26.8) |
| Rural | 33.4 | 30.8 | 38.3 | 35.2 | 29.1 | 22.8 |
| (95% CI) | (28.4; 39.4) | (27.5; 34.6) | (34.8; 42.2) | (31.7; 39.1) | (25.4; 33.3) | (17.6; 29.5) |
| Total Kenya | 31.7 | 29.4 | 36.9 | 35.4 | 27.4 | 21.3 |
| (95% CI) | (27.1; 37.2) | (26.3; 32.8) | (33.7; 40.4) | (32.2; 38.9) | (24.1; 31.1) | (16.7; 27) |
| Rural/urban ratio | 1.93 | 1.57 | 1.30 | 0.97 | 1.49 | 1.61 |
| Under 5 mortality | ||||||
| Urban | 80.6 | 68.7 | 92.6 | 100.3 | 90.2 | 74.8 |
| (95% CI) | (60.4; 107.2) | (56.4; 83.5) | (81.4; 105.3) | (89.2; 112.9) | (78.1; 104.1) | (59.6; 93.6) |
| Rural | 103.1 | 96.8 | 105.3 | 104.1 | 98.1 | 72.5 |
| (95% CI) | (94.5; 112.4) | (91.1; 102.8) | (100; 110.9) | (98.6; 109.9) | (91.9; 104.6) | (64.6; 81.3) |
| Total Kenya | 100.7 | 93.4 | 103.3 | 103.4 | 96.7 | 72.9 |
| (95% CI) | (92.7; 109.4) | (88.1; 98.9) | (98.4; 108.4) | (98.4; 108.6) | (91.1; 102.5) | (65.8; 80.8) |
| Rural/urban ratio | 1.28 | 1.41 | 1.14 | 1.04 | 1.09 | 0.97 |
95% Confidence interval.
Table 3.
Cox regression models of mortality by area of residence and time; Kenya DHS 1993, 1998, 2003 and 2008/09.
| Urban |
Rural |
Overall |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio | p-Value | [95% CI] | HR | p-Value | [95% CI] | HR | p-Value | [95% CI] | |||||||
| Infant mortality | |||||||||||||||
| Time [Ref: 1 (1979–1983)] | |||||||||||||||
| 2 (1984–1988) | 0.73 | 0.123 | 0.49 | 1.09 | 0.90 | 0.128 | 0.79 | 1.03 | 0.88 | 0.048 | 0.78 | 1.00 | |||
| 3 (1989–1993) | 1.02 | 0.898 | 0.71 | 1.47 | 0.93 | 0.264 | 0.82 | 1.05 | 0.94 | 0.287 | 0.84 | 1.05 | |||
| 4 (1994–1998) | 1.05 | 0.801 | 0.73 | 1.50 | 0.98 | 0.717 | 0.86 | 1.11 | 0.98 | 0.718 | 0.87 | 1.10 | |||
| 5 (1999–2003) | 1.13 | 0.522 | 0.78 | 1.62 | 0.98 | 0.752 | 0.86 | 1.11 | 0.99 | 0.913 | 0.88 | 1.12 | |||
| 6 (2004–2008) | 0.97 | 0.899 | 0.65 | 1.46 | 0.73 | 0.000 | 0.62 | 0.86 | 0.76 | 0.000 | 0.66 | 0.89 | |||
| Child mortality | |||||||||||||||
| Time [Ref: 1 (1979–1983)] | |||||||||||||||
| 2 (1984–1988) | 1.06 | 0.854 | 0.56 | 2.02 | 1.01 | 0.931 | 0.85 | 1.20 | 1.00 | 0.961 | 0.85 | 1.19 | |||
| 3 (1989–1993) | 1.63 | 0.106 | 0.90 | 2.95 | 1.19 | 0.046 | 1.00 | 1.41 | 1.20 | 0.026 | 1.02 | 1.41 | |||
| 4 (1994–1998) | 2.00 | 0.020 | 1.11 | 3.58 | 1.07 | 0.448 | 0.90 | 1.27 | 1.13 | 0.133 | 0.96 | 1.34 | |||
| 5 (1999–2003) | 1.06 | 0.855 | 0.56 | 2.03 | 0.86 | 0.145 | 0.71 | 1.05 | 0.86 | 0.107 | 0.71 | 1.03 | |||
| 6 (2004–2008) | 0.86 | 0.720 | 0.37 | 1.99 | 0.74 | 0.041 | 0.56 | 0.99 | 0.73 | 0.022 | 0.56 | 0.96 | |||
| Under-five mortality | |||||||||||||||
| Time [Ref: 1 (1979–1983)] | |||||||||||||||
| 2 (1984–1988) | 0.83 | 0.306 | 0.59 | 1.18 | 0.96 | 0.464 | 0.86 | 1.07 | 0.94 | 0.277 | 0.85 | 1.05 | |||
| 3 (1989–1993) | 1.16 | 0.364 | 0.84 | 1.59 | 1.03 | 0.572 | 0.93 | 1.14 | 1.03 | 0.490 | 0.94 | 1.14 | |||
| 4 (1994–1998) | 1.24 | 0.178 | 0.91 | 1.69 | 1.01 | 0.782 | 0.91 | 1.13 | 1.03 | 0.535 | 0.93 | 1.14 | |||
| 5 (1999–2003) | 1.13 | 0.444 | 0.82 | 1.57 | 0.97 | 0.563 | 0.87 | 1.08 | 0.98 | 0.664 | 0.88 | 1.08 | |||
| 6 (2004–2008) | 1.01 | 0.972 | 0.70 | 1.46 | 0.75 | 0.000 | 0.65 | 0.87 | 0.78 | 0.000 | 0.68 | 0.89 | |||
A comparison of urban–rural differentials shows that there has been narrowing of the gap for IMR, and U5MR (Table 2; Fig. 1, Fig. 2, Fig. 3), with the rural–urban ratio on IMR and U5MR reversing in favor of rural areas. Generally, childhood mortality declined in both rural and urban areas, but the decline was more rapid in rural areas. IMR and U5MR were always higher in rural compared with urban areas but converged in the period 1999–2003 for IMR, and 2004–2008 for U5MR, with mortality being higher in urban areas thereafter. Child mortality showed a slightly different pattern whereby mortality in both rural and urban areas increased from the period 1979–1983 until the period 1989–1998, then declined in the succeeding periods. However, the gap between urban and rural areas seemed to have narrowed slightly. There was an overall downward trend in the hazard ratios for IMR, CMR and U5MR from 1979/83 to 2004/08; though there was an early increase in the hazard ratios for CMR and U5MR in the periods 1989/1993 and 1994/1998. The hazard ratios for IMR, CMR and U5MR for rural areas significantly reduced to 0.73, 0.74 and 0.75 in 2004–2008 compared to 1979–1983 (p<0.05, respectively), indicating a reduction in childhood mortality rates over time in rural areas but this was not the case for urban areas where the change was not significant. The hazard ratios for child mortality significantly increased in rural areas in the period 1989–1993 to 1.19 and doubled in urban areas in the period 1994–1998 relative to the period 1979–1983 (p<0.05) (Table 3). We also examined the rural–urban differential in mortality using the interaction between time and place of residence. We observed a decline in the hazard ratios for IMR and U5MR; however it was not statistically significant (Appendix 2).
Fig. 1.
Trends in infant mortality rate by place of residence at birth 1979–2008; Kenya DHS 1993, 1998, 2003, and 2008/09.
Fig. 2.
Trends in child mortality rates by place of residence at birth 1979–2008; Kenya DHS 1993, 1998, 2003, and 2008/09.
Fig. 3.
Trends in infant under five Mortality rates by place of residence at birth 1979–2008; Kenya DHS 1993, 1998, 2003, and 2008/09.
Examining the proximate determinants of child survival gives a mixed picture (Table 4). From 2003 to 2008, ITN usage substantially increased from 6% to 47%, and this could have had an impact on mortality from malaria. Since 1993, prevalence of diarrheal diseases among children slightly increased from 19% to 23% in 2008. The proportion of children with acute respiratory infections (ARI) who were taken to hospital decreased in urban areas (from 70% to 55%) but increased in rural areas (from 50% to 58%). Immunization coverage steadily decreased between 1993 (78%) and 2003 (52%) but increased in 2008 (68%). The results show a change or reversal in the ratio between urban and rural areas of various determinants of child mortality including adolescent childbearing (0.8–1.1), median duration of exclusive breastfeeding (1.0–0.5), child immunization (1.0–0.9), diarrhea morbidity (0.9–1.1) and health seeking for childhood illnesses (acute respiratory infections) (1.4–0.9), all in favor of rural areas.
Table 4.
Trends and urban–rural differentials in proximate determinants of infant and child mortality; Kenya DHS 1993, 1998, 2003 and 2008/09.
| 1993 | 1998 | 2003 | 2008/09 | |
|---|---|---|---|---|
| Adolescent child bearing (%)a | ||||
| Urban | 17.3 | 17.5 | 22.2 | 18.5 |
| Rural | 21.1 | 21.8 | 23.3 | 17.5 |
| Urban–rural ratio | 0.8 | 0.8 | 1.0 | 1.1 |
| Total | 20.5 | 20.9 | 23 | 17.7 |
| Median duration of exclusive breast feeding until six monthsb | ||||
| Urban | 0.5 | 0.5 | 0.5 | 0.6 |
| Rural | 0.5 | 0.5 | 0.5 | 1.1 |
| Urban–rural ratio | 1.0 | 1.0 | 1.0 | 0.5 |
| Total | 0.5 | 0.5 | 0.5 | 0.7 |
| Median duration of any breastfeedingc | ||||
| Urban | 19.6 | 18.9 | 20.3 | 19.5 |
| Rural | 21.5 | 21.5 | 22.3 | 22.5 |
| Urban–rural ratio | 0.9 | 0.9 | 0.9 | 0.9 |
| Total | 21.1 | 20.9 | 21.9 | 21.5 |
| Child immunizationd | ||||
| Urban | 80.9 | 58.3 | 53 | 62.9 |
| Rural | 77.7 | 59.8 | 51.5 | 69.9 |
| Urban–rural ratio | 1.0 | 1.0 | 1.0 | 0.9 |
| Total | 78.2 | 59.5 | 51.8 | 68.3 |
| Percentage of children with diarrhoeae | ||||
| Urban | 16.4 | 17.1 | 21.9 | 22.9 |
| Rural | 19.1 | 17.1 | 21.3 | 21.3 |
| Urban–rural ratio | 0.9 | 1.0 | 1.0 | 1.1 |
| Total | 18.8 | 17.1 | 21.4 | 21.9 |
| Percentage of children with ARI taken to H/Ff | ||||
| Urban | 70.1 | 73.9 | 65.5 | 54.7 |
| Rural | 50.3 | 54.0 | 50.3 | 57.7 |
| Urban–rural ratio | 1.4 | 1.4 | 1.3 | 0.9 |
| Total | 52.2 | 57.3 | 53 | 57.3 |
| Percentage of children who slept under an ITN last nightg | ||||
| Urban | 12.1 | 61.8 | ||
| Rural | 4.7 | 43.6 | ||
| Urban–rural ratio | 2.6 | 1.4 | ||
| Total | 6 | 46.7 | ||
| Access to improved source of drinking waterh | ||||
| Urban | 88.9 | 87.5 | 78.8 | 90.3 |
| Rural | 30.6 | 27.3 | 43.0 | 51.2 |
| Urban–rural ratio | 2.9 | 3.2 | 1.8 | 1.8 |
| Total | 41.8 | 41.6 | 52.0 | 61.3 |
| Access to improved toilet facilityi | ||||
| Urban | 52.2 | 54.0 | 50.8 | 85.4 |
| Rural | 7.6 | 7.8 | 9.0 | 37.1 |
| Urban–rural ratio | 6.9 | 6.9 | 5.6 | 2.3 |
| Total | 16.1 | 18.8 | 19.4 | 49.6 |
Percentage of women 15–19 years who are mothers or pregnant with their first child.
Median duration of exclusive breastfeeding (giving the child only breast milk in the last 24 h) as described in the Guide to DHS Statistics (Rutstein and Rojas, 2006).
Median duration of any breastfeeding (including exclusive breastfeeding, full breastfeeding, predominant breastfeeding and partial breastfeeding) as described in the Guide to DHS Statistics (Rutstein and Rojas, 2006).
Percentage of children 12–23 months who had received specific vaccines by the time of survey (according to vaccination card or mother׳s report).
Percentage of children under three years who had diarrhea in the last two weeks preceding the survey.
Percentage of children under three years who were ill with cough accompanied with rapid breathing duringthe two weeks preceding the survey, taken to a health facility.
Percentage of children under five years who slept under a mosquito net (treated or untreated).
Improved water sources include piped water sources, tubewell/borehole, protected wells and springs, and bottled water.
Improved facility includes toilets with a flush to sewer, septic tank or to a pit latrine.
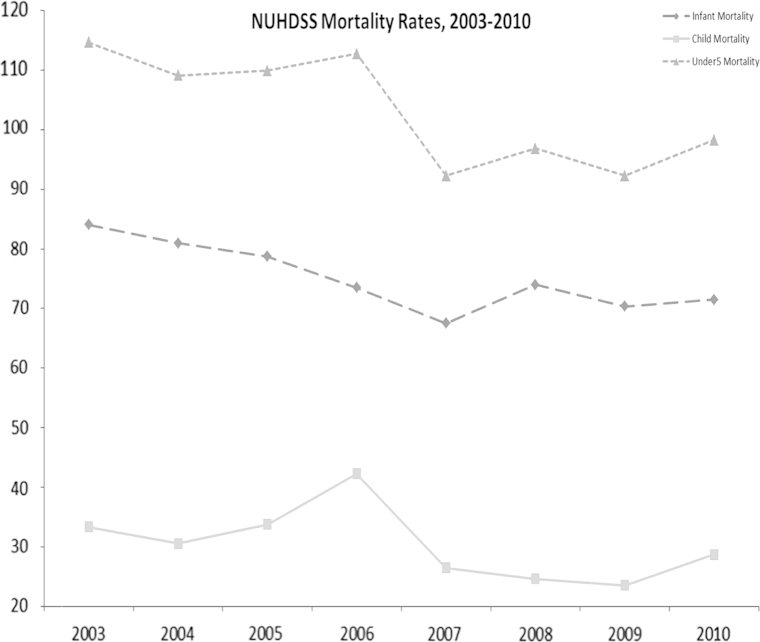
3.2. Child mortality trends in the urban slums according to NUHDSS
An open cohort of 36,952 individuals was included in the analysis from the NUHDSS. As shown on Table 5 and Fig. 4, a remarkable overall decline in all levels of childhood mortality was observed in the urban slums: infant mortality declined from 82.8 (95% CI 69.0; 99.3) in 2003 to 67.4 (95% CI 55.4; 81.8) in 2008 and 56.8 (95% CI 47.1; 68.4) in 2010, child mortality declined from 33.3 (95% CI 25.5; 43.5) in 2003 to 23.1 (95% CI 16.7; 31.9) in 2008 and 23.9 (95% CI 17.8;32.0) in 2010 while under five mortality declined from 113.4 (95% CI 97.7; 131.3) in 2003 to 88.9 (95% CI 75.4;104.7) in 2008 and 79.3 (95% CI 67.9; 92.5) in 2010.
Table 5.
Childhood mortality rates, NUHDSS 2003–2010.
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | |
|---|---|---|---|---|---|---|---|---|
| IMR | 82.8 | 79.0 | 76.7 | 71.1 | 64.9 | 67.4 | 61.9 | 56.8 |
| (95% CI) | (69.0; 99.3) | (65.0; 95.9) | (63.2; 93.1) | (58.7; 86.2) | (53.1; 79.1) | (55.4; 81.8) | (51.4; 74.4) | (47.1; 68.4) |
| CMR | 33.3 | 30.4 | 33.4 | 41.6 | 25.9 | 23.1 | 22.5 | 23.9 |
| (95% CI) | (25.5; 43.5) | (22.6; 40.7) | (25.3; 43.9) | (32.7; 52.8) | (19.1; 35.2) | (16.7; 31.9) | (16.5; 30.6) | (17.8; 32.0) |
| U5MR | 113.4 | 107.0 | 107.6 | 109.8 | 89.1 | 88.9 | 83.0 | 79.3 |
| (95% CI) | (97.7; 131.3) | (91.2; 125.3) | (92.0; 125.5) | (94.8; 127.0) | (75.6; 104.9) | (75.4; 104.7) | (71.0; 97.0) | (67.9; 92.5) |
Fig. 4.
Infant, child and under five mortality rates in Nairobi urban slums, 2003–2010; NUHDSS.
Table 6 shows a comparison of mortality rates per 1000 live births between urban slums, urban as a whole, rural and Kenya as a whole for the period 2004–2008. In line with our expectation, higher average mortality rates were registered for the urban slums compared with all other parts of Kenya. IMR was highest in urban slums (75) compared with urban as whole (65), rural (56) and Kenya as a whole (58). Child mortality was also highest in urban slums (32) compared with urban as whole (14), rural (23) and Kenya as a whole (21). U5MR was very high in the urban slums (104) compared with 75, 72.5 and 73 for the urban as whole, rural and Kenya as a whole, respectively.
Table 6.
Comparison of mortality rates in the urban slums with other parts of Kenya for the period 2004–2008; Kenya DHS 2008/09.
| Urban slums | Urban | Rural | Kenya | |
|---|---|---|---|---|
| Infant mortality | 75 | 65 | 56 | 58 |
| Child mortality | 32 | 14 | 23 | 21 |
| Under 5 mortality | 104 | 75 | 72.5 | 73 |
4. Discussion
This study shows that overall childhood mortality in Kenya has declined over the thirty-year period from 1979 to 2008. However, the decline has not been consistent, the trends show a decline in infant and under five mortality rates from the 1970s to the 1980s, a stall or an increase from the 1980s to the 1990s, and then a decline in the 2000s. The study also indicates a narrowing of the gap in childhood mortality between urban and rural areas. The narrowing of the gap seems to be mainly due to a more rapid decline in childhood mortality in rural areas. The results show that while the ratio between mortality in rural areas compared with urban areas has reduced for child mortality, it has actually reversed for IMR and U5MR. The findings from the two slums in Nairobi included in this study also illustrate the downward trend in childhood mortality, although the rates in urban slums remain high compared with indicators at national level for both urban and rural areas.
Our results are similar to those found by other researchers in the context of Kenya and sub-Saharan Africa. A study by Demombynes and Trommlerová indicated that among 20 countries with recent DHS data in sub-Saharan Africa, the average annual rate of decline in U5MR is 4.2% while that for IMR is 3.6%. Kenya had the fastest rate of decline in IMR among the 20 countries examined, at a decline rate of 7.6% per year between 2003 and 2008, while the decline in U5MR is also among the highest at 8.4% (Demombynes and Trommlerova, 2010, Demombynes and Trommlerova, 2010). The decline in Kenya observed in our study and by Demombynes and Trommlerová may be attributable to public health interventions including malaria prevention initiatives such as use of insecticide treated nets (ITNs) in malaria endemic areas, HIV prevention and treatment initiatives, and improved access to water and sanitation (Kleinschmidt et al., 2009, Demombynes and Trommlerova, 2010, Demombynes and Trommlerova, 2010, Ndirangu et al., 2010). Our study showed an improvement in various factors related to child survival particularly in the use of insecticide treated nets; a 10-fold increase in rural areas and a five-fold increase in urban areas. Using a Oaxaca-Blinder decomposition analysis of changes in infant mortality, the study by Demombynes and Trommlerová attributed 58% of decline in infant mortality in Kenya to ownership of ITNs in malaria endemic areas and about 6% to improved access to sanitation facilities (Demombynes and Trommlerova, 2010, Demombynes and Trommlerova, 2010). The increase in childhood mortality, particularly infant and under five mortality from the 1980s to the 1990s in this study may be attributed to HIV (Zaba et al., 2003, Ikamari, 2004). It is also important to note that the rates of mortality observed may be an under-estimation given that there is usually a bias introduced by interviewing living mothers (usually the case for DHS), as HIV positive women and their children are more likely to die (Hallett et al., 2010, Walker et al., 2012). Hallett and colleagues estimate that standard cross-sectional survey statistics underestimate the true IMR and U5MR mortality by 6.7% and 9.8%, respectively (Hallett et al., 2010).
The seemingly lower decline in childhood mortality in urban areas leading to a narrowing of the gap or a reversal between the magnitude of rates in rural versus urban may be attributed to the fact that most urban residents in Kenya now live in slum areas characterized by poor water and environmental sanitation, limited livelihood opportunities, inadequate health services and poor health outcomes including poor vaccination coverage and high HIV prevalence (African Population and Health Research Center, 2002a, African Population and Health Research Center, 2002b, Kimani-Murage and Ngindu, 2007, Madise N. et al., 2012). Evidence from 22 countries in sub-Saharan countries using DHS data collected between 1990s and 2000s indicates an association between urban U5 mortality, urban population growth, and trends in access to safe drinking water and in immunization coverage. Higher urban U5 mortality was documented in countries with higher urban population growth, while lower mortality was documented in countries with higher levels of safe drinking water and immunization coverage (Fotso et al., 2007). Another study involving 47 developing countries using DHS data indicates that in a substantial number of countries, there is higher level of stunting and U5 mortality in urban areas than in rural areas (Van de Poel et al., 2007). Bocquier and colleagues in a recent analysis of DHS data from 18 African countries observed that after controlling for known demographic and socio-economic correlates of U5 mortality, the urban advantage in U5 mortality is largely reduced or reversed. They concluded that what may matter most with regards to child survival is access to services and economic opportunities rather than place of residence (Bocquier et al., 2011).
The current study showed that although there has been a decline in childhood mortality in the two slum settings, the levels remain high. The average rates observed in urban slums for the period 2004–2008 in this study are generally higher than for rural areas, urban areas as a whole, and Kenya as a whole observed in the same period. The high levels of childhood mortality rates in urban slums, coupled with an increase in the proportion of urban residents residing in slums, may explain the reason why rates in urban areas as a whole remain high despite the rapid decline in rural areas. The current study shows that there has been a change or reversal in the ratio of various determinants of childhood mortality between urban and rural areas including adolescent child bearing, median duration of exclusive breastfeeding, child immunization, diarrhea morbidity and health seeking for childhood illnesses (acute respiratory infections), all in favor of rural areas. This may further explain the narrowing of the gap in childhood mortality. Consistent with the literature on neighborhood effects on health (Montgomery and Hewett, 2005, Sampson et al., 2002), this change may be a result of poor health conditions including health care and social services, water and environmental sanitation and housing that have been documented in urban slum settings in sub-Saharan Africa (African Population and Health Research Center, 2002a, African Population and Health Research Center, 2002b, Magadi, 2004, Kimani-Murage and Ngindu, 2007).
A key strength of this study is being able to examine trends in childhood mortality over a long period of time (30-year period). Additionally, being able to use data collected in urban slum settings to explain trends seen in urban areas is also a key strength. This is particularly important because we were able to have a place-based definition of the urban poor, as opposed to using characteristics such as household wealth to define the urban poor as used in many studies. A key limitation is the wide confidence intervals, particularly for the urban rates, so that several of the comparisons are not statistically significant. This may be occasioned by few cases in the urban areas. Another limitation is that we do not have data for slum settings for the period 1979–2003 as we do for the other parts of the country. Therefore, we could only compare rates for the period 2004–2008 between urban slums and other parts of the country. Other limitations relate to using mother׳s self-reports in the estimations for example of date of birth and date of death of the child. The mother could have misreported these dates particularly if the child has died. There is also likelihood of age heaping particularly at age 12 months which is common, and which may have led to underestimation of infant mortality.
In conclusion, this study indicates a significant decline in childhood mortality over the last three decades, more marked in rural areas compared to urban areas. This has led to a narrowing of the gap between childhood mortality rates in rural compared with urban areas. This study indicates that despite a decline in childhood mortality in urban slums, the rates remain high. The deplorable conditions observed in the urban slums (African Population and Health Research Center, 2002a, African Population and Health Research Center, 2002b, Magadi, 2004, Kimani-Murage and Ngindu, 2007) may explain the slower decline in childhood mortality in urban areas as majority of urban residents now live in slum areas. These results suggest that efforts to reduce child mortality should prioritize resource-poor urban settings, particularly in provision of services (Bocquier et al., 2011). However, there is need for further studies to carefully examine which factors have played the key role in the improvement in child health indicators and the narrowing of the gap between rural and urban areas, paying special attention to factors in slum settings which this study was not able to establish.
Acknowledgments
Analysis and writing time was supported through a grant from the Bill and Melinda Gates Foundation (Grant OPP1021893) and core funding for APHRC from The William and Flora Hewlett Foundation (Grant no. 2009-4051) and the Swedish International Cooperation Agency (SIDA) (Reference no. 2011-001578). Elizabeth Kimani is a Wellcome Trust Fellow (Research Grant no. 097146/Z/11/Z). We acknowledge free access of the DHS data and funding for the DHS from the USAID. We are grateful to Dr. Catherine Kyobutungi of APHRC for her careful review of the manuscript.
Appendix A1
See Fig. A1 and Table A2, Table A3.
Table A2.
Cox regression models (HR and p-value) of mortality urban–rural differences over time; Kenya DHS 1993, 1998, 2003 and 2008/09.
| Variable | Infant mortality |
Child mortality |
Under 5 mortality |
|||
|---|---|---|---|---|---|---|
| HR | p-Value | HR | p-Value | HR | p-Value | |
| Residence [Ref: Urban] | ||||||
| Rural | 1.15 | 0.422 | 1.95 | 0.058 | 1.29 | 0.109 |
| Time [Ref: 1 (1979–1983)] | ||||||
| 2 (1984–1988) | 0.73 | 0.123 | 1.13 | 0.762 | 0.84 | 0.361 |
| 3 (1989–1993) | 1.02 | 0.896 | 1.73 | 0.133 | 1.16 | 0.378 |
| 4 (1994–1998) | 1.05 | 0.798 | 2.14 | 0.035 | 1.25 | 0.183 |
| 5 (1999–2003) | 1.13 | 0.517 | 1.18 | 0.671 | 1.17 | 0.361 |
| 6 (2004–2008) | 0.98 | 0.908 | 0.94 | 0.896 | 1.03 | 0.862 |
| Residence×time interaction | ||||||
| Rural – 2 (1984–1988) | 1.24 | 0.314 | 0.81 | 0.616 | 1.10 | 0.606 |
| Rural – 3 (1989–1993) | 0.91 | 0.627 | 0.66 | 0.263 | 0.87 | 0.419 |
| Rural – 4 (1994–1998) | 0.93 | 0.718 | 0.49 | 0.058 | 0.81 | 0.214 |
| Rural – 5 (1999–2003) | 0.87 | 0.473 | 0.75 | 0.470 | 0.83 | 0.286 |
| Rural – 6 (2004–2008) | 0.75 | 0.196 | 0.76 | 0.584 | 0.71 | 0.102 |
Table A3.
Life tables for childhood mortality, NUHDSS 2003–2010.
| Appendix A3a: Life table for infant and under five mortality rates, NUHDSS 2003–2010 | |||||||
|---|---|---|---|---|---|---|---|
|
Interval |
Total |
Deaths |
Failure |
Error |
95% Conf. Interval |
||
| 0 | 1 | 12,540 | 790 | 0.0691 | 0.0024 | 0.0645 | 0.0739 |
| 1 | 2 | 12,582 | 211 | 0.0844 | 0.0026 | 0.0795 | 0.0896 |
| 2 | 3 | 12,434 | 78 | 0.0901 | 0.0026 | 0.0851 | 0.0954 |
| 3 | 4 | 12,077 | 53 | 0.094 | 0.0027 | 0.0889 | 0.0994 |
| 4 | 5 | 11,510 | 25 | 0.0959 | 0.0027 | 0.0908 | 0.1014 |
|
Appendix A3b: Life table for child mortality rates, NUHDSS 2003–2010 | |||||||
|
Interval |
Total |
Deaths |
Failure |
Error |
95% Conf. interval |
||
| 1 | 2 | 12,582 | 211 | 0.0165 | 0.0011 | 0.0144 | 0.0189 |
| 2 | 3 | 12,434 | 78 | 0.0226 | 0.0013 | 0.0202 | 0.0253 |
| 3 | 4 | 12,077 | 53 | 0.0268 | 0.0014 | 0.0242 | 0.0298 |
| 4 | 5 | 11,510 | 25 | 0.0289 | 0.0015 | 0.0261 | 0.0319 |
Fig. A1.
Conceptual framework on urban population growth, access to water and health services, and child mortality. .
Source: Fotso et al. (2007).
References
- African Population and Health Research Center . APHRC; Nairobi: 2002. Population and Health Dynamics in Nairobi Informal Settlements. [Google Scholar]
- African Population and Health Research Center . Occasional Study Report 1. APHRC; Nairobi: 2002. Health and livelihood needs of residents of informal settlements on Nairobi city. [Google Scholar]
- Bocquier P., Madise N.J., Zulu E.M. Is there an urban advantage in child survival in sub-saharan Africa? Evidence from 18 countries in the 1990s. Demography. 2011;48(2):531–558. doi: 10.1007/s13524-011-0019-2. [DOI] [PubMed] [Google Scholar]
- Brockerhoff M., Brennan E. The poverty of cities in developing regions. Popul. Dev. Rev. 1998;24:75–114. [Google Scholar]
- Cohen B. Urbanization in developing countries: current trends, future projections, and key challenges for sustainability. Technol. Soc. 2006;28(1–2):63–80. [Google Scholar]
- Demombynes, G., S.K. Trommlerova, 2010. What has driven the decline of infant mortality in Kenya?. Policy Research Working Paper No. WPS 60572010, World Bank.
- Emina J. Monitoring of health and demographic outcomes in poor urban settlements: evidence from the Nairobi urban health and demographic surveillance system. J. Urban Health. 2011;88(Suppl. 2):S200–S218. doi: 10.1007/s11524-011-9594-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fotso J.C. Progress towards the child mortality millennium development goal in urban sub-Saharan Africa: the dynamics of population growth, immunization, and access to clean water. BMC Public Health. 2007;7:218. doi: 10.1186/1471-2458-7-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fotso J.C. What does access to maternal care mean among the urban poor? Factors associated with use of appropriate maternal health services in the slum settlements of Nairobi, Kenya. Matern. Child Health J. 2009;13(1):130–137. doi: 10.1007/s10995-008-0326-4. [DOI] [PubMed] [Google Scholar]
- Fotso J.C. Child growth in urban deprived settings: does household poverty status matter? At which stage of child development? Health Place. 2012;18(2):375–384. doi: 10.1016/j.healthplace.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gareth J. How many child deaths can we prevent this year? Lancet. 2003;362(9377):65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- Hallett T.B. Measuring and correcting biased child mortality statistics in countries with generalized epidemics of HIV infection. Bull. World Health Organ. 2010;88(10):761–768. doi: 10.2471/BLT.09.071779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikamari L.D. An Upsurge in early childhood mortality in Kenya: a search for explanations. Afr. J. Health Sci. 2004;11(1–2):9–20. doi: 10.4314/ajhs.v11i1.30774. [DOI] [PubMed] [Google Scholar]
- Inter-agency U.N. Group for Child Mortality Estimation, Levels & Trends in Child Mortality – Report. The UN Inter-agency Group for Child Mortality Estimation; New York: 2012. [Google Scholar]
- Kayode G.A., Adekanmbi V.T., Uthman O.A. Risk factors and a predictive model for under-five mortality in Nigeria: evidence from Nigeria demographic and health survey. BMC Pregnancy Childbirth. 12. 20122012:10. 10. doi: 10.1186/1471-2393-12-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenya National Bureau of Statistics (KNBS) and ICF Macro, 2009. Kenya Demographic and Health Survey 2008–09. KNBS and ICF Macro, Calverton, Maryland.
- Kimani-Murage E.W., Ngindu A.M. Quality of water the slum dwellers use: the case of a Kenyan slum. J. Urban Health. 2007;84(6):829–838. doi: 10.1007/s11524-007-9199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinschmidt I. Marked increase in child survival after four years of intensive malaria control. Am. J. Trop. Med. Hyg. 2009;80(6):882–888. [PMC free article] [PubMed] [Google Scholar]
- Lalou R., LeGrand T.K. Child mortality in the urban and rural sahel. Popul.: Engl. Sel. 9. 19971997:147–168. 147–168. [Google Scholar]
- Madise N. J. Are slum dwellers at heightened risk of HIV infection than other urban residents? Evidence from population-based HIV prevalence surveys in Kenya. Health Place. 2012;18(5):1144–1152. doi: 10.1016/j.healthplace.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magadi M. Maternal and child health among the urban poor in Nairobi, Kenya. Afr. Popul. Stud. 2004;19:179–198. [Google Scholar]
- Montgomery M., Hewett P. Urban poverty and health in developing countries: household and neighborhood effects. Demography. 2005;42(3):397–425. doi: 10.1353/dem.2005.0020. [DOI] [PubMed] [Google Scholar]
- Mutua M.K., Kimani-Murage E., Ettarh R.R. Childhood vaccination in informal urban settlements in Nairobi, Kenya: Who gets vaccinated? BMC Public Health. 2011;11(1):6. doi: 10.1186/1471-2458-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Research Council . Cities Transformed: Demographic Change and Its Implications in the Developing World. The National Academies Press; Washington, DC: 2003. [Google Scholar]
- Ndirangu J. Decline in early life mortality in a high HIV prevalence rural area of South Africa: evidence of HIV prevention or treatment impact? AIDS. 2010;24(4):593–602. doi: 10.1097/QAD.0b013e328335cff5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutstein S.O., Rojas G. ORC Macro; Calverton, MD: 2006. Guide to DHS Statistics. Demographic and Health Surveys. [Google Scholar]
- Sampson R.J., Morenoff J.D., Gannon-Rowley T. Neighborhood effects: social processes and new directions in research. Annu. Rev. Sociol. 2002;28:443–478. [Google Scholar]
- Sastry N. What explains rural–urban differentials in child mortality in Brazil? Soc. Sci. Med. 1997;44(7):989–1002. doi: 10.1016/s0277-9536(96)00224-9. [DOI] [PubMed] [Google Scholar]
- Sastry N. Trends in socioeconomic inequalities in mortality in developing countries: the case of child survival in Sao Paulo, Brazil. Demography. 2004;41(3):443–464. doi: 10.1353/dem.2004.0027. [DOI] [PubMed] [Google Scholar]
- Unhabitat . UNHABITAT; Nairobi: 2003. Slums of the World. The Face of Urban Poverty in the New Millennium? Global Urban Observatory. [Google Scholar]
- Unhabitat . State of the World׳s Cities 2010/2011: Bridging the Urban Divide. UNHABITAT; Nairobi: 2008. [Google Scholar]
- United Nations, 2010. World Urbanization Prospects: The 2009 Revision. Department of Economic and Social Affairs, Population Division, United Nations, New York.
- United Nations, 2012. World Urbanization Prospects: The 2011 Revision. Department of Economic and Social Affairs, Population Division, United Nations, New York.
- United Nations, 2013. The Millenium Development Goals Report 2013, United Nations, New York.
- Walker N., Hill K., Zhao F. Child mortality estimation: methods used to adjust for bias due to AIDS in estimating trends in under-five mortality. PLoS Med. 2012;9(8):e1001298. doi: 10.1371/journal.pmed.1001298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks J.R. Ethnic residential patterns as predictors of intra-urban child mortality inequality in Accra, Ghana. Urban Geogr. 2006;27(6):526–548. doi: 10.2747/0272-3638.27.6.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank . The World Bank; Washington DC: 2012/2013. African Development Indicators. [Google Scholar]
- Zaba B, Marston M, Floyd S. United Nations Population Division; New York: 2003. The Effect of HIV on Child Mortality Trends in Sub-Saharan Africa. [Google Scholar]
- Van de Poel E., O׳Donnell O., Van Doorslaer E. Are urban children really healthier? Evidence from 47 developing countries. Soc. Sci. Med. 2007;65(10):1986–2003. doi: 10.1016/j.socscimed.2007.06.032. [DOI] [PubMed] [Google Scholar]