Abstract
Background: Maintaining the recent expansion of palliative care access in the United States is a recognized public health concern. Economic evaluation is essential to validate current provision and assess the case for new programs. Previous economic reviews in palliative care reported on programs across settings and systems; none has examined specifically the hospital consultative model, the dominant model of provision in the United States.
Objectives: To review systematically the economic evidence on specialist palliative care consultation teams in the hospital setting, to appraise this evidence critically, and to identify areas for future research in this field.
Data Sources: A meta-review (“a review of existing reviews”) was conducted of eight published systematic reviews and one relevant nonsystematic review. To identify articles published outside of the timeframe of these reviews, systematic searches were performed on the PubMed, CINAHL, and EconLit databases.
Study Selection: Articles were included if they compared the costs and/or cost effectiveness of a specialist hospital inpatient palliative care consultation for adult patients with those of a comparator.
Results: Ten studies were included and these demonstrate a clear pattern of cost-saving impact from inpatient consultation programs. Nevertheless, knowledge gaps still exist regarding the economic effects of these programs. Current evidence has been generated from the hospital perspective; health system costs, patient and caregiver costs, and health outcomes are typically not included.
Conclusions: Inpatient palliative care consultation programs have been shown to save hospitals money and to provide improved care to patients with serious illness. With a clear pattern of cost-saving using current methodology, it is timely to begin expanding the scope of economic evaluation in this field. Future research must address the measurement of both costs and outcomes to understand more fully the role that palliative care plays in enhancing value in health care. Relevant domains for such research are identified.
Introduction
Maintaining the recent expansion of palliative care access in the United States is a recognized public health concern, both to address insufficient provision in underserved regions and to develop national capacity in the context of aging populations and changing patterns of disease.1–5
Evidence-based research is required, systematically appraising the outcomes of programs and identifying the key processes and structures underpinning these outcomes.6–8 Payers and policymakers require evidence to validate current palliative care provision, to explore ways that this could be made more cost effective, and to assess the case for new programs.9
One essential component of such a research agenda is economic evaluation. Patients with serious illness and functional impairment account for a rapidly increasing share of medical expenditures in the United States and other high-income countries.5 Cost-effectiveness analysis of care provided to people with serious illness has been identified as fundamental to controlling long-term costs.10
Despite the acknowledged significance of economic analyses in evaluating and informing care provision, the economic literature on programs is small and disparate, reflecting the complexity of palliative care assessment.11 Where the clinical and economic impact of palliative care programs have been analyzed in previous systematic reviews, these have tended to report across different settings, diagnoses, levels of specialism, and national systems, highlighting patterns without focusing on specific programs or models of care.12–19
There has been no economic review focused on specialist hospital inpatient consultation, the dominant model of provision in the United States hospital setting. Nonspecific approaches have been logical given the disparate and formative nature of economic evaluation in palliative care. But as the numbers of programs and of evaluations grow, so does the need for more focused analysis. A review was therefore undertaken to collect systematically the economic evidence on this model specifically, to appraise critically the evidence, and to identify areas for future research in the field.
Methods
Identifying studies for consideration in our review was performed primarily by systematic meta-review (“a review of existing reviews”); instead of collating studies from databases, researchers considered studies included in already published reviews. For time periods not covered by already published reviews, a systematic database search was undertaken.
This was agreed among the authors as an appropriate method given the prior literature and our objectives. In the context of multiple relevant prior reviews, we did not feel that a full systematic review was justified: broadly considered, the economic evidence on palliative care programs has been assembled. What the prior reviews do not provide is a detailed examination of the economic evidence on any specific model of care delivery, or a critical assessment of that evidence. In systematically reviewing relevant previous reviews using clear criteria focusing specifically on economic evaluation of one model, we provide meaningful information that can guide decision making—the primary purpose of a systematic literature review in health care.20 Formal meta-analysis combining these results using statistical modeling is precluded by persistent differences in methods and approach in economic studies of palliative care.19
Reviews were identified by systematic searches on the PubMed, CINAHL, and EconLit databases. Relevant search terms for palliative care, review, and economics (e.g., palliative, hospice; review, systematic; economic*, cost*) were combined to search titles, abstract, and subject headings to July 31, 2013. A review was included the meta-review only if it reported (1) a systematic search strategy, (2) examining (but not necessarily limited to) inpatient hospital palliative care programs, (3) treating adult patients, and (4) identified outcomes of interest as including (but not necessarily limited to) economic analysis. Only English-language journal articles were considered.
The meta-review returned nine published reviews with a relevant focus,12–19,21 summarized in Table 1.
Table 1.
Systematic Reviews of Palliative Care Program Evaluations
| Ref # | Review | Number of included papers |
|---|---|---|
| (12) | Higginson et al., 2002, UK | 13 |
| (13) | Douglas et al., 2003, UK | 17 |
| (14) | Higginson et al., 2003, UK | 15a |
| (15) | Zimmermann et al., 2008, US | 7b |
| (21) | Smith and Cassel, 2009, USc | 21c |
| (16) | Higginson and Evans, 2010, UK | 59 |
| (17) | Simoens et al., 2010, BEL | 15 |
| (18) | El-Jawahri et al., 2011, US | 22 |
| (19) | Smith et al., 2014,d IRL | 46 |
Sixty-five included in total; 15 reported separately in economic analysis.
Twenty-two included in total; 7 reported separately in economic analysis.
Not reported as a systematic review; 21 papers discussed in cost analysis.
Epub 2013, within the timeframe of the review.
Of these, eight systematic reviews variously focused primarily or exclusively on economic factors in palliative care provision13,17,19; reported economic impact as one outcome of interest separately alongside clinical and other factors14,15; or evaluated palliative care services without particular emphasis on economic considerations.12,16,18 An additional review, not reporting a systematic search strategy but with a highly relevant focus, was included in the meta-review following discussion among the authors.21 The reviews had a balance between different systems and perspectives in high-income countries with four written by teams based in the United Kingdom,12–14,16 three in the United States,15,18,21 and one each from Belgium17 and Ireland.19
The timeframe of these nine reviews provided full coverage of the relevant published literature to the end of 2011. To supplement these findings and identify papers published since 2011, systematic searches were performed on the PubMed, CINAHL, and EconLit databases. Key search terms from the clinical and economic domains (e.g., palliative, hospice; economic*, cost*) were combined to search titles, abstracts and subject headings from January 1, 2012 to July 31, 2013.
Study selection
All studies included in any of the nine relevant previous reviews and all studies returned by systematic database search were considered for inclusion in our review.
The lead author reviewed all unique titles/abstracts against the inclusion criteria; all deemed irrelevant or not meeting the criteria were removed, all others were read in full against the inclusion criteria. Where there was uncertainty about an articles's suitability for inclusion this was discussed with coauthors.
A study was included in our review only if it contained a credible economic evaluation of a specialist-led multidisciplinary palliative care consultation team to adult patients in the hospital inpatient setting, measuring and comparing the costs and/or cost effectiveness of this intervention against a usual care comparator. Only English-language journal articles were considered.
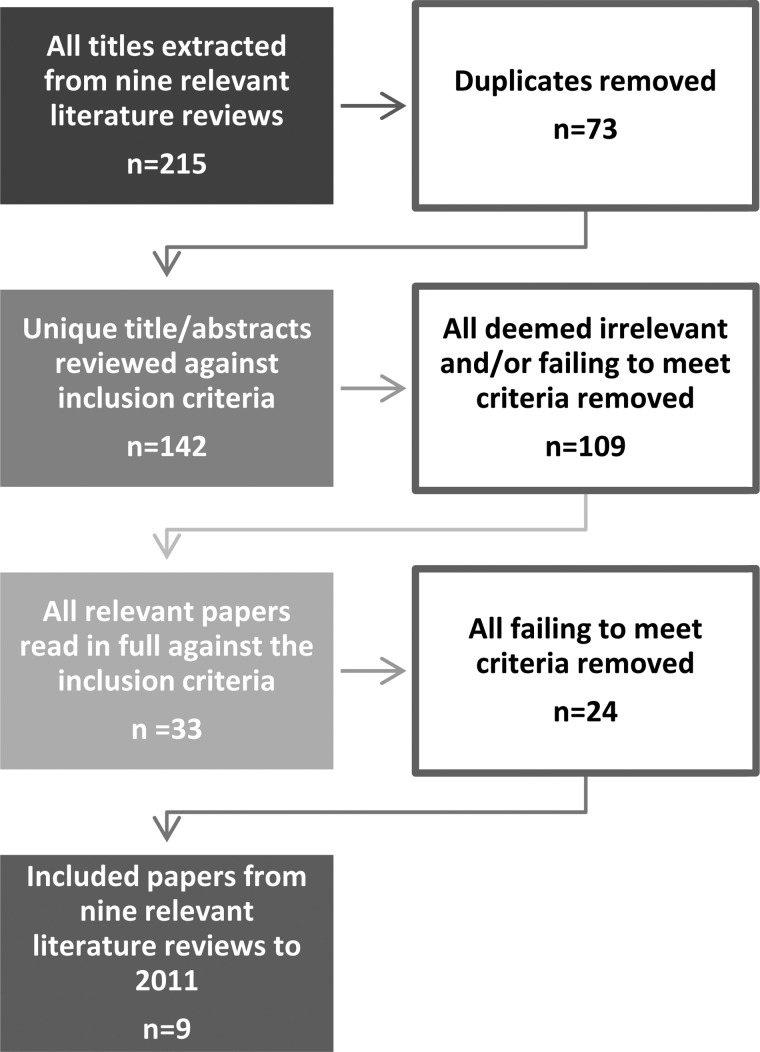
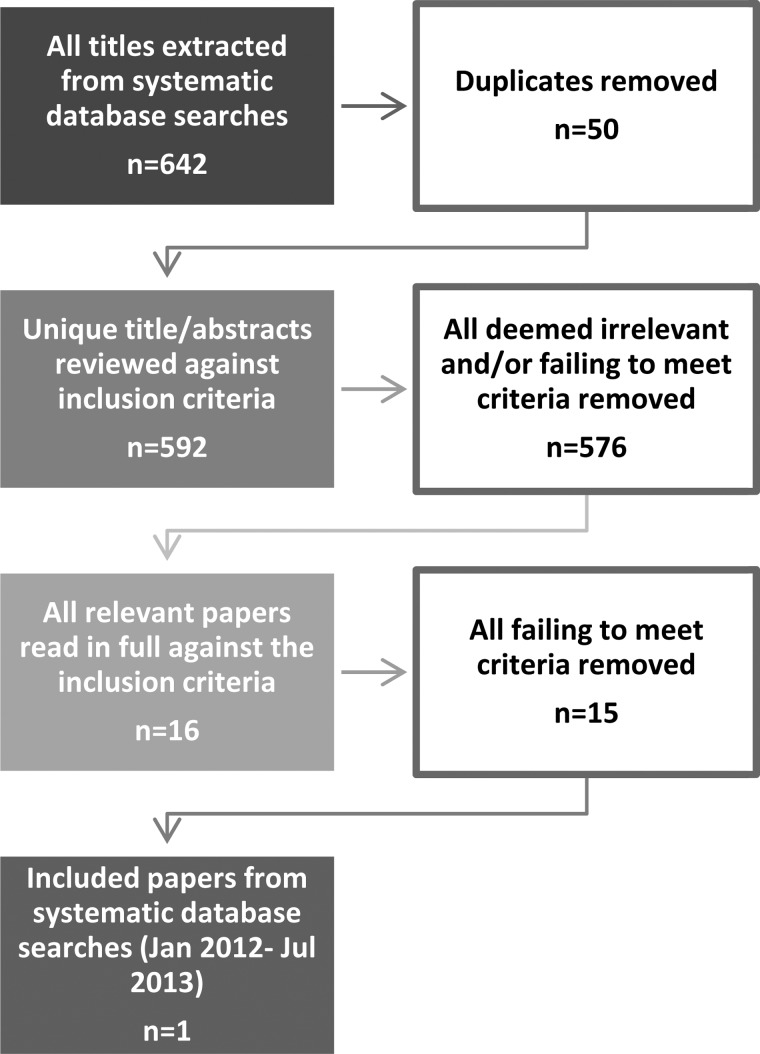
The rationale for these criteria were agreed among the authors, adapted from the gold standard guidelines for health economic evaluation.22 Drummond and Jefferson's22 full checklist for economic evaluations is far greater; these components were identified as constituting a fair bare minimum threshold in a field in which economic evaluation is at a very early stage. A full breakdown of the appraisal processes are illustrated in Figures 1 and 2.
FIG. 1.
Meta-review appraisal (to 2011).
FIG. 2.
Database search (January 2012 to July 2013).
Findings
Ten economic evaluations of specialist palliative consultation teams in a hospital setting were included in our review.23–33 These are summarized in Table 2.
Table 2.
Economic Evaluations of Specialist Inpatient Palliative Care Consultation Teams
| Ref # | Study | Hospital(s) ------------Team label | Design | Sample size Intervention/control | Principal diagnosisa | Outcomes of interest | Key findings |
|---|---|---|---|---|---|---|---|
| (23) | Cowan, 2004 | Hospital not categorized by authors ------------ Advanced Illness Assistance Team (AIA) |
Cohort | 164 PC patients 152 UC patients |
Cancer 27% Neurologic 18% Pulmonary 17% Cardiovasc. 12% Organ failure 7% Gastrointestinal 7% Chronic pain 6% Infection 4% Other 2% |
Hospital charges; LOS | Lower (∼7%) mean daily charges for PC than UC (p=0.006) For patients with LOS>7 days, PC reduces LOS |
| (24) | Penrod et al., 2006 | Two Veterans Administration (VA) facilities ------------ Palliative Care Consultation Team (PCCT) |
Cohort | 82 PC patients 232 UC patients |
Cancer 50% Infectious disease 10% Cardiovascular 7% Pulmonary 10% Gastrointestinal 7% Genitourinary 4% Other 12% |
Hospital costs; ICU | PC patients 42% less likely to be admitted to ICU Lower (∼22%) daily direct costs for PC than UC (p<0.0001) Laboratory & radiology also lower; no difference for pharmacy |
| (25) | Ciemins et al., 2007 | Large, private, not-for-profit medical center ------------ Palliative Care Consultation Service (PCCS) |
Cohort | 27 PC patients 128 UC patients |
Cancer 100% | Hospital costs | Lower (∼13%b) mean daily costs for PC than UC (p<0.01) Lower (∼16%) mean total costs for PC than UC (p<0.0001) |
| (26) | Bendaly et al., 2008 | Public hospital ------------ Palliative Care consultation (PCc) |
Cohort | 61 PC patients 55 UC patients |
Pulmonary disorders and/or MV 30% Cardiovascular disorders 23% Neoplasms 16% Infections with or without sepsis 15% Other 16% |
Hospital charges; LOS | Lower (∼16%) median total charges for PC than UC (p<0.001) No significant diference in LOS (p=0.57) |
| (27) | Gade et al., 2008 | Three managed care organization hospitals ------------ Interdisciplinary Palliative Care Service (IPCS) |
RCT | 275 PC patients 237 UC patients |
Cancer 27% CHF 9% MI 1% Other heart disease 3% COPD 13% Other pulmonary disease 1% ESRD 4% Organ failure 12% Stroke 9% Dementia 3%c |
Total health service costs 6 months postdischarge; symptom control, emotion/ spiritual support, satisfaction | Lower (∼32%) total mean health costs for PC than UC (p<0.001) Lower (∼23%) total mean health costs for PC than UC once IPCS staffing accounted for No difference in physical, emotional symptoms Improved satisfaction |
| (28) | Hanson et al., 2008 | Tertiary academic medical center ------------ Palliative Care Consultation Service (PCCS) |
Cohort | 104 PC patients 1,813 UC patients |
Cancer 61% Cardiopulmonary diseases 11% Neurologic diseases 5% Hepatic/renal failure 4% Acute infections 14%d |
Hospital costs, LOS | No difference in total variable costs (p=0.78) Lower (∼10%) daily variable costs for PC than UC (p=0.03) Larger proportional cost savings per day for PC where LOS is greater |
| (29) | Morrison et al., 2008 | Five community hospitals & three academic medical centers ------------ Palliative Care Consultation Team (PCCT) |
Cohort |
Live discharges 2630 PC patients 18,427 UC patients Hospital deaths 2278 PC patients 2124 UC patients |
Live discharge Cancer 29% Infection 4% Cardiovascular 19% Pulmonary 15% Gastrointestinal 7% Genitourinary 4% Other 22% Hospital death Cancer 19% Infection 11% Cardiovascular 24% Pulmonary 18% Gastrointestinal 9% Genitourinary 4% Other 14% |
Hospital costs |
Live discharges Lower total costs (∼14%; p=0.02), total costs per day (∼19%; p<0.001), total direct costs (∼15%; p=0.004), direct costs per day (∼21%; p<0.001) for PC than UC Hospital deaths Lower total costs (∼18%; p=0.001), total costs per day (∼22%; p<0.001), total direct costs (∼22%; p=0.003), direct costs per day (∼25%; p<0.001) for PC than UC |
| (30) | Penrod et al., 2010 | Five Veterans Administration (VA) facilities ------------ Palliative Care Consultation Team (PCCT) |
Cohort | 606 PC patients 2715 UC patients |
Cancer 62%e COPD 36% CHF 28% HIV/AIDS 3% |
Hospital costs, ICU use | PC patients 44% less likely to be admitted to ICU Lowerf daily direct costs for PC than UC (p<0.0001) Pharmacy, laboratory, & nursing also lower; no difference for radiology |
| (31) | Morrison et al., 2011 | A community hospital, two academic medical centers, and a safety-net hospital ------------ Palliative Care Consultation Team (PCCT) |
Cohort |
Live discharges 290 PC patients 1427 UC patients Hospital deaths 185 PC patients 149 UC patients |
Cancer 58% AIDS 2% CHF 12% COPD 2% Advanced liver disease 19% Prolonged ICU stay 6.9% |
Hospital costs, ICU use, LOS |
Live discharges Lower total costs (∼11%; p<0.05), total costs per day (∼18%; p<0.001) for PC than UC Lower laboratory (∼16%) & imaging (∼13%) costs though not statistically significant Slightly higher ICU LOS but significantly lower (∼42%; p<0.001) ICU cost per admission for PC than UC Hospital deaths Lower total costs (∼11%; p<0.05), total costs per day (∼9%; p<0.01) for PC than UC Lower pharmacy (∼21%; p<0.001) for PC than UC ; no difference for laboratory or imaging Lower ICU LOS (10.2 days against 13.8; p<0.01) for PC than UC; no significant cost difference |
| (33) | Whitford et al., 2013 | Integrated medical center comprising two hospitals ------------ Palliative Care Consult Service (PCCS) |
Cohort |
Live discharges 1177 PC patients 3531 UC patients Hospital deaths 300 PC patients 900 UC patients |
Live discharge Infectious 8% Neoplasm 21% Endocrine 2% Nervous 3% Circulatory 30% Respiratory 16% Digestive 8% Musculoskeletal 9% Other 3% Hospital death Infectious 4% Neoplasm 32% Endocrine 3% Nervous 4% Circulatory 23% Respiratory 10% Digestive 7% Musculoskeletal 3% Other 14% |
Hospital costs, incorporating ICU costs |
Live discharges Lower total costs (∼5%; p<0.05) for PC than UC Lower procedure costs; higher evaluation, imaging, pharmacy costs for PC than UC (no % or p value given) Hospital deaths Lower total costs (∼31%; p<0.05) for PC than UC Lower procedure, evaluation, imaging, laboratory, pharmacy costs for PC than UC (no % or p value given) |
For PC group at time of consultation.
There is inconsistency in reporting of cost difference as a percentage. Ciemins et al. use the cost of palliative care as the base cost in calculations, i.e., [%ΔC=((CPC – CUC)/CPC) x 100] while others (e.g., Hanson et al.) use the cost of usual care, i.e., [%ΔC=((CPC – CUC)/CUC)×100]. In this table and throughout the text all %ΔC have been calculated using the latter method.
Gade et al. report a diagnosis for 196 PC patients (=71.3%)
Primary diagnoses for all PC patients in overall sample (n=304); authors do not report corresponding figures for sub-sample in economic analysis (n=104).
Patients could have more than one advanced disease diagnosis; therefore does not add up to 100%.
No UC cost given so not possible to calculate proportional saving.
PC, palliative care; UC, usual care; LOS, length of stay; ICU, intensive care unit; RCT, randomized controlled trial; MV, mechanical ventilation; CHF, congestive heart failure; MI, myocardial infarction; COPD, chronic obstructive pulmonary disese; ESRD, end-stage renal disease; HIV/AIDS, human immunodeficiency virus/acquired immune deficiency syndrome.
Summary
Design and approach
All 10 studies are from the United States. Observational designs dominate with 9 cohort studies23–26,28–31,33 and 1 randomized controlled trial.27 Among observational studies there is a wide variation in size with 5 having intervention groups of between 27 and 164 patients,23–26,28 and 1 study having 4908 intervention patients.29
Nine of the studies restrict their perspective to the hospital and do not evaluate patient or caregiver outcomes.23–26,28–31,33 The remaining article analyzes total health care costs for 6 months postdischarge as well as some patient outcome measures but does not quantify the relationship between the two.27
While there is variation in terms of hospital type and the label given to multidisciplinary teams, the composition of those teams are broadly consistent. Six of the 10 evaluations were described as comprising at least a physician, a nurse, a social worker, and a chaplain23–28; in some cases these were also described as including a psychologist and/or an oncology nurse specialist and/or nursing assistants. Of the other 4, 2 were multisite studies in which all teams included a physician and nurse but not all included a social worker and chaplain,29,31 and another assessed a newly implemented service that initially comprised a physician and nurse before later incorporating a chaplain.33 The specific composition of the team was not described in one study,30 but is indicated to be consistent with a prior related study.24
A further source of potential variability between studies is the process and nature of referral. All consultation teams saw patients following referral from another team in the hospital but it is not possible to ascertain how comparable these processes were.
All studies addressed programs that treated a range of diagnoses, although following matching for economic evaluation one study was restricted to patients with cancer.25 Typically the study populations are patients near end of life; the survival rate during the study period for the intervention group varies between 0% and 80%, with a median of 55%.
Results
Overall costs
All 10 studies report that palliative care interventions result in lower costs than their usual care comparators. There are differences in study design, setting, intervention and population. Formal meta-analysis is also prevented by differences in approach to expressing costs; outcomes of interest are variously direct, variable and total costs, per diem and in toto.
Studies that report costs from the hospital perspective find statistically significant savings through palliative care in the 9%–25% range.24,25,28,29,31 The three studies that stratify by survivors and decedents report consistently higher costs for patients who died but an inconsistent treatment effect on costs between the two groups; two studies find similar differences in proportional savings (11%–20%) with slightly higher treatment impact for decedents29,31; the other reports a large discrepancy with a 5% cost-saving from palliative care for survivors and 31% for decedents.33
Of the two studies reporting hospital charges, one reported mean daily charges around 7% lower for palliative care23 and the other median total charges around 16% lower for palliative care.26 The only study to take a postdischarge health costs perspective finds costs for palliative patients 32% lower than those for usual care patients over 6 months.27 One study's reporting method precluded calculating a proportional difference.30
Ancillary costs
Where ancillary costs are reported separately, the results are inconsistent. Where statistically significant differences have been identified, costs are typically lower for palliative care interventions, but differences are not always identified. A study24 reports ancillary (laboratory and radiology) costs 43% lower and no difference in pharmacy; a larger follow-up study found differences in laboratory and pharmacy but not in imaging.30 Another study29 finds differences in pharmacy but not imaging; study31 finds no difference in pharmacy. Another study33 finds palliative care to be less costly across ancillary categories among patients who died, and different treatment effects by category for patients discharged alive.
ICU costs
Of the six studies to report ICU use as an outcome of interest, the results have a clear pattern toward lower use among palliative patients.24,27,29,30,33 One found no significant difference, possibly due to lack of power.28
Discussion
The findings of this review demonstrate that inpatient specialist palliative care consultation teams are consistently found to be less costly than usual care comparators in the range 9%–25% for hospital costs, while one study estimated a 32% reduction for all health care costs over 6 months postdischarge. These differences are statistically significant.
However, methodology to date has implications for our understanding of the role that palliative care plays in enhancing value in health care, where value is defined as the relationship between quality and cost. In assessing current provision and validating new programs, payers and policymakers are not only concerned with the immediate direct costs of providing hospital treatment. Specifically, questions remain as to whether reductions in hospital costs are passed on to other care settings or to family or informal caregivers, the effect of palliative care teams on hospice expenditures, and the effect of palliative care teams on overall health care expenditures.34,35 And ensuring that cost reduction does not reflect reduced quality of care is best achieved by a full cost-effectiveness analysis quantifying the relationship between cost effects and treatment efficacy.34
Knowledge gaps
From first principles, cost-effectiveness analysis in health care is defined as a “comparative analysis of alternatives in terms of both costs and consequences.”22
With regard to costs, the focus has been on the hospital “silo.” Seven examine only costs to the hospital providing care.24,25,28–31,33 while two use only hospital charges,23,26 generally considered a poor approximation of hospital costs.34 One study examines all health care costs postdischarge but not costs to patients, caregivers, or wider systems and society.27
With regard to consequences, there is no evidence base to date. No study has quantified the relationship between treatment efficacy and cost in a cost-effectiveness measure.
What is needed?
Limitations to the current literature reflect practical real-world challenges in both the collection of data and the measurement of intangible outcomes such as satisfaction with care among a rapidly changing and extremely sick patient population.8 However, with a clear pattern of hospital cost-saving using current methodology, it is timely to begin expanding the scope of economic evaluation in this field. The improvement of economic evaluation of palliative care teams requires that evaluators identify a greater proportion of relevant components in a full cost-effectiveness analysis, establish what is already known about these through existing datasets and published research, and considers the best way to measure and incorporate these in future.
Components of cost analysis
There are four major categories of resource use for cost-effectiveness analysis (CEA), summarized in Table 3.35
Table 3.
Components Belonging in the Numerator of a Cost-Effectiveness Analysis34
| Cost component | Use in evaluation of palliative care teams |
|---|---|
| Health care resources: The costs of tests, drugs, supplies, health care personnel and medical facilities, in providing intervention and in all subsequent interventions relevant to the disease or condition. | Health care resources have been partially included in the evaluations of palliative care teams to date: nine studies have used hospital costs only; Gade et al.27 incorporates all formal health care costs for a 6-month period. Future studies therefore need to expand their perspective in examining health care resources: Broaden perspective beyond hospital costs to incorporate all relevant health care costs paid by patients, their families and other payers, including pharmacy, formal caregivers. Lengthen perspective beyond initial hospital stay to incorporate all disease-relevant system costs following the initial intervention, both to hospitals and the health system, and to patients, families and other payers. |
| Non-health care resources: The costs of other consumption entailed in the intervention and follow-up, e.g., transport to and from hospital; child care bills while a parent receives treatment | Non-health care resources were not included in the evaluations of palliative care teams to date. There is no established literature on this area to provide indicative magnitudes of these costs and, by definition, there is no central dataset. It seems likely that these can only be measured and incorporated in CEA through well-designed original primary research projects. |
| Patient time: Time expended by the patient seeking, participating in, and undergoing an intervention | Patient time costs were not included in the evaluations of palliative care teams to date. There is only a limited literature on this area to estimate the magnitude of these costs. It seems likely that these can only be measured and incorporated in CEA through well-designed original primary research projects. |
| Informal caregiver time: Unpaid time spent by family members or volunteers to provide homecare | Informal caregiver time costs were not included in the evaluations of palliative care teams to date. There is only a limited literature on this area to estimate the magnitude of these costs. It seems likely that these can only be measured and incorporated in CEA through well-designed original primary research projects. |
CEA, cost-effectiveness analysis.
As this summary makes clear, current economic evaluation has excluded key components of the cost effects of palliative care teams. Increasing the scope and thus reliability of economic evaluation of palliative care teams requires addressing these shortfalls.
First, future studies need to expand their perspective in examining health care resources beyond the perspective of direct hospital costs. These studies need to incorporate all relevant health care costs paid by patients, their families, and other payers, including pharmacy, and formal caregivers, and incorporate all disease-relevant system costs (“total spend”) following the initial intervention, both to hospitals and the health system, and to patients, families, and other payers.
A full cost-effectiveness analysis would examine and incorporate non-health care system costs, such as hours lost from work, caregiver comorbidity, financial consequences of serious illness to families, and patient and family caregiver time. As our review shows, no evaluation of in-hospital consultation teams has included these costs. Given the lack of routine data collection in these domains, addressing these knowledge deficits may be best addressed by future primary research incorporating these domains in design.
Where future analysis remains focused on cost from the hospital perspective, our review highlights two particular priorities. First, studies to date have not analyzed in detail patient-level determinants of resource use. But factors such as socioeconomic status, functionality, and diagnosis may determine a high proportion of hospital costs in providing care to patients with serious illness.17,36,37 Identifying relevant patient-level factors may offer new and valuable information for understanding variations in cost and so delivering care that is both more appropriate to patient needs and less resource-intensive. However, few studies in any setting have attempted this.38,39 Second, the literature to date is skewed toward patients near end of life; as palliative treatment is increasingly introduced earlier in the care trajectory, it is important to develop evidence on treatment effects for patient groups with longer life expectancy at the time of consultation.
Future analysis will also be helped by more detailed cost reporting. Recent studies have tended to report both direct and total costs, per diem and in toto. This approach, alongside a definition of what each category comprises and how the figures were reached, is the best way to enable formal comparison and statistical analysis of results in future as well as to improve understanding of the data under discussion.
Approaches to estimating effectiveness
There is no consensus on methodology for measuring effectiveness in the economic evaluation of palliative care.
Standardized guidelines for health economics research in the United States identify the quality-adjusted life year (QALY) as the fundamental outcome measurement for all evaluations.35 However, equivalent guidelines specifically for palliative care have resisted this position.8,40 The QALY approach has been criticized as inappropriate for patients with serious illness and is an ongoing subject of debate among economists in this field.41–43
Evaluators must make their own decision in research design to identify the contextually appropriate measures of physiological and health-related quality of life (HRQL) effects to be incorporated in cost-effectiveness analysis. Given the emerging state of the field, initial approaches do not need to be methodologically complex to make a substantial contribution. An example of a simple approach was illustrated in a U.K. study of short-term palliative care for multiple sclerosis.44 The authors generated two cost-effectiveness planes, plotting the relationship of costs with patient outcomes (as measured by Palliative Care Outcome Scale [POS]-8) and caregiver burden (using Zaret Caregiver Burden [ZBI]-12).
In combining cost and effectiveness analysis for the same patient group the authors present more thorough and robust evidence to compare the impact of an intervention and a comparator. This ought to be the goal of an increasing number of studies in future.
Conclusion
The published evidence shows a clear pattern of specialist inpatient palliative care consultation teams reducing hospital costs. This finding is consistent with other reviews of the positive impact of palliative care programs on multiple outcomes across a range of settings.
By methodological norms in economic evaluation, the evidence base has been generated using a narrow approach. These limitations are defensible given practical challenges and available data but, with a clear pattern of cost saving using current methodology, it is timely to begin expanding the scope of economic evaluation in this field. The evidence now suggests that specialist inpatient palliative care both reduces costs and improves patient outcomes. Unifying this evidence in robust cost-effectiveness analysis will strengthen our understanding of the role that palliative care plays in enhancing value in health care.
There is a consensus on the appropriate approach to measuring costs, and this paper identifies the relevant domains. There is no consensus on the appropriate approach to measuring outcomes, but it ought to be possible to generate evidence using different approaches and so strengthen the evidence base amidst methodological debate. Given the lack of routine data collection in these domains, addressing knowledge deficits may be best addressed by future primary research.
Where future analysis remains focused on cost from the hospital perspective, research priorities should include the patient-level determinants of cost difference between palliative and usual care, and the economic impact of treatments earlier in the care trajectory.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Center to Advance Palliative Care: Analysis of U.S. Hospital Palliative Care Programs 2010 Snapshot. 2010. www.capc.org/news-and-events/releases/analysis-of-us-hospital-palliative-care-programs-2010-snapshot.pdf/file_view (Last accessed June13, 2014)
- 2.Davies E, Higginson I: The Solid Facts: Palliative Care. Copenhagen: World Health Organization, Regional Office for Europe, 2004 [Google Scholar]
- 3.Davies E, Higginson I: Better Palliative Care for Older People. Copenhagen: World Health Organization, Regional Office for Europe, 2004 [Google Scholar]
- 4.Goldsmith B, Dietrich J, Du Q, Morrison RS: Variability in access to hospital palliative care in the United States. J Palliat Med 2008;11:1094–1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meier DE: Increased access to palliative care and hospice services: Opportunities to improve value in health care. Milbank Q 2011;89:343–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldstein NE, Morrison RS: The intersection between geriatrics and palliative care: A call for a new research agenda. J Am Geriatr Soc 2005;53:1593–1598 [DOI] [PubMed] [Google Scholar]
- 7.Gelfman LP, Du Q, Morrison RS: An update: NIH research funding for palliative medicine 2006 to 2010. J Palliat Med 2013;16:125–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Higginson IJ, Evans CJ, Grande G, Preston N, Morgan M, McCrone P, Lewis P, Fayers P, Harding R, Hotopf M, Murray SA, Benalia H, Gysels M, Farquhar M, Todd C; MORECare: Evaluating complex interventions in end of life care: The MORECare statement on good practice generated by a synthesis of transparent expert consultations and systematic reviews. BMC Med 2013;11:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meier DE, Beresford L: Palliative care cost research can help other palliative care programs make their case. J Palliat Med 2009;12:15–20 [DOI] [PubMed] [Google Scholar]
- 10.Smith TJ, Hillner BE: Bending the cost curve in cancer care. N Engl J Med 2011;364:2060–2065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gomes B, Harding R, Foley KM, Higginson IJ: Optimal approaches to the health economics of palliative care: Report of an international think tank. J Pain Symptom Manage 2009;38:4–10 [DOI] [PubMed] [Google Scholar]
- 12.Higginson IJ, Finlay I, Goodwin DM, Cook AM, Hood K, Edwards AG, Douglas HR, Norman CE: Do hospital-based palliative teams improve care for patients or families at the end of life? J Pain Symptom Manage 2002;23:96–106 [DOI] [PubMed] [Google Scholar]
- 13.Douglas HR, Halliday D, Normand C, Corner J, Bath P, Beech N, Clark D, Hughes P, Marples R, Seymour J, Skilbeck J, Webb T: Economic evaluation of specialist cancer and palliative nursing: A literature review. Int J Palliat Nurs 2003;9:424–428 [DOI] [PubMed] [Google Scholar]
- 14.Higginson IJ, Finlay IG, Goodwin DM, Hood K, Edwards AG, Cook A, Douglas HR, Normand CE: Is there evidence that palliative care teams alter end-of-life experiences of patients and their caregivers? J Pain Symptom Manage 2003;25:150–168 [DOI] [PubMed] [Google Scholar]
- 15.Zimmermann C, Riechelmann R, Krzyzanowska M, Rodin G, Tannock I: Effectiveness of specialized palliative care: A systematic review. JAMA 2008;299:1698–1709 [DOI] [PubMed] [Google Scholar]
- 16.Higginson IJ, Evans CJ: What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J 2010;16:423–435 [DOI] [PubMed] [Google Scholar]
- 17.Simoens S, Kutten B, Keirse E, Berghe PV, Beguin C, Desmedt M, Deveugele M, Léonard C, Paulus D, Menten J: The costs of treating terminal patients. J Pain Symptom Manage 2010;40:436–448 [DOI] [PubMed] [Google Scholar]
- 18.El-Jawahri A, Greer JA, Temel JS: Does palliative care improve outcomes for patients with incurable illness? A review of the evidence. J Support Oncol 2011;9:87–94 [DOI] [PubMed] [Google Scholar]
- 19.Smith S, Brick A, O'Hara S, Normand C: Evidence on the cost and cost-effectiveness of palliative care: A literature review. Palliat Med 2014;28:130–150 [DOI] [PubMed] [Google Scholar]
- 20.Centre for Reviews and Dissemination, University of York: Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health Care. York: CRD, University of York, 2009 [Google Scholar]
- 21.Smith TJ, Cassel JB: Cost and non-clinical outcomes of palliative care. J Pain Symptom Manage 2009;38:32–44 [DOI] [PubMed] [Google Scholar]
- 22.Drummond MF, Jefferson TO: Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996;313:275–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cowan JD: Hospital charges for a community inpatient palliative care program. Am J Hosp Palliat Care 2004;21:177–190 [DOI] [PubMed] [Google Scholar]
- 24.Penrod JD, Deb P, Luhrs C, Dellenbaugh C, Zhu CW, Hochman T, Maciejewski ML, Granieri E, Morrison RS: Cost and utilization outcomes of patients receiving hospital-based palliative care consultation. J Palliat Med 2006;9:855–860 [DOI] [PubMed] [Google Scholar]
- 25.Ciemins EL, Blum L, Nunley M, Lasher A, Newman JM: The economic and clinical impact of an inpatient palliative care consultation service: A multifaceted approach. J Palliat Med 2007;10:1347–1355 [DOI] [PubMed] [Google Scholar]
- 26.Bendaly EA, Groves J, Juliar B, Gramelspacher GP: Financial impact of palliative care consultation in a public hospital. J Palliat Med 2008;11:1304–1308 [DOI] [PubMed] [Google Scholar]
- 27.Gade G, Venohr I, Conner D, McGrady K, Beane J, Richardson RH, Williams MP, Liberson M, Blum M, Della Penna R: Impact of an inpatient palliative care team: A randomized control trial. J Palliat Med 2008;11:180–190 [DOI] [PubMed] [Google Scholar]
- 28.Hanson LC, Usher B, Spragens L, Bernard S: Clinical and economic impact of palliative care consultation. J Pain Symptom Manage 2008;35:340–346 [DOI] [PubMed] [Google Scholar]
- 29.Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, Spragens L, Meier DE; Palliative Care Leadership Centers' Outcomes Group: Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 2008;168:1783–1790 [DOI] [PubMed] [Google Scholar]
- 30.Penrod JD, Deb P, Dellenbaugh C, Burgess JF, Jr, Zhu CW, Christiansen CL, Luhrs CA, Cortez T, Livote E, Allen V, Morrison RS:P Hospital-based palliative care consultation: Effects on hospital cost. J Palliat Med 2010;13:973–979 [DOI] [PubMed] [Google Scholar]
- 31.Morrison RS, Dietrich J, Ladwig S, Quill T, Sacco J, Tangeman J, Meier DE: Palliative care consultation teams cut hospital costs for Medicaid beneficiaries. Health Aff (Millwood) 2011;30:454–463 [DOI] [PubMed] [Google Scholar]
- 32.Economic and Social Research Institute (ESRI): Clinical Coding. February16, 2012. www.esri.ie/health_information/hipe/clinical_coding/ (Last accessed June13, 2014)
- 33.Whitford K, Shah ND, Moriarty J, Branda M, Thorsteinsdottir B: Impact of a palliative care consult service. Am J Hosp Palliat Care 2014;31:175–182 [DOI] [PubMed] [Google Scholar]
- 34.Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL: Methods for the Economic Evaluation of Health Care Programmes, 3rded Oxford: Oxford University Press, 2005 [Google Scholar]
- 35.Gold MR: Cost-Effectiveness in Health and Medicine. New York/Oxford: Oxford University Press, 1996 [Google Scholar]
- 36.Tibi-Levy Y, Le Vaillant M, de Pouvourville G: Determinants of resource utilization in four palliative care units. Palliat Med 2006;20:95–106 [DOI] [PubMed] [Google Scholar]
- 37.Gomez-Batiste X, Tuca A, Corrales E, Porta-Sales J, Amor M, Espinosa J, Borràs JM, de la Mata I, Castellsagué X; Grupo de Evaluación-SECPAL: Resource consumption and costs of palliative care services in Spain: A multicenter prospective study. J Pain Symptom Manage 2006;31:522–532 [DOI] [PubMed] [Google Scholar]
- 38.Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA: Determinants of medical expenditures in the last 6 months of life. Ann Intern Med 2011;154:235–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Groeneveld I, Murtagh F, Kaloki Y, Bausewein C, Higginson I: Determinants of Healthcare Costs in the Last Year of Life. The Annual Assembly of American Academy of Hospice and Palliative Medicine & Hospice and Palliative Nurses Association; New Orleans, LA: March14, 2013 [Google Scholar]
- 40.Preston NJ, Short V, Hollingworth W, McCrone P, Grande G, Evans C, et al. . MORECare research methods guidance development: Recommendations for health economic evaluation in palliative and end of life care research [abstract]. Palliat Med 2012;26:541. [DOI] [PubMed] [Google Scholar]
- 41.Normand C: Measuring outcomes in palliative care: Limitations of QALYs and the road to PalYs. J Pain Symptom Manage 2009;38:27–31 [DOI] [PubMed] [Google Scholar]
- 42.Round J: Is a QALY still a QALY at the end of life? J Health Econ 2012;31:521–527 [DOI] [PubMed] [Google Scholar]
- 43.Normand C: Setting priorities in and for end-of-life care: Challenges in the application of economic evaluation. Health Econ Policy Law 2012;7:431–439 [DOI] [PubMed] [Google Scholar]
- 44.Higginson IJ, McCrone P, Hart SR, Burman R, Silber E, Edmonds PM: Is short-term palliative care cost-effective in multiple sclerosis? A randomized phase II trial. J Pain Symptom Manage 2009;38:816–826 [DOI] [PubMed] [Google Scholar]