Abstract
Objectives
To describe the development and application of an organizing research framework to guide COG Nursing research.
Data Sources
Research articles, reports and meeting minutes
Conclusion
An organizing research framework helps to outline research focus and articulate the scientific knowledge being produced by nurses in the pediatric cooperative group.
Implication for Nursing Practice
The use of an organizing framework for COG nursing research can facilitate clinical nurses’ understanding of how children and families sustain or regain optimal health when faced with a pediatric cancer diagnosis through interventions designed to promote individual and family resilience.
The Children’s Oncology Group (COG) is the sole National Cancer Institute (NCI)-supported cooperative pediatric oncology clinical trials group and the largest organization in the world devoted exclusively to pediatric cancer research. It was founded in 2000 following the merger of the four legacy NCI-supported pediatric clinical trials groups (Children’s Cancer Group [CCG], Pediatric Oncology Group [POG], National Wilms Tumor Study Group, and Intergroup Rhabdomyosarcoma Study Group). The COG currently has over 200 member institutions across North America, Australia, New Zealand and Europe and a multidisciplinary membership of over 8,000 pediatric, radiation, and surgical oncologists, nurses, clinical research associates, pharmacists, behavioral scientists, pathologists, laboratory scientists, patient/parent advocates and other pediatric cancer specialists. The COG Nursing Discipline was formed from the merger of the legacy CCG and POG Nursing Committees, and current membership exceeds 2000 registered nurses. The discipline has a well-developed infrastructure that promotes nursing involvement throughout all levels of the organization, including representation on disease, protocol, scientific, executive and other administrative committees (e.g., nominating committee, data safety monitoring boards). COG nurses facilitate delivery of protocol-based treatments for children enrolled on COG protocols, and Nursing Discipline initiatives support nursing research, professional and patient/family education, evidence-based practice, and a patient-reported outcomes resource center. The research agenda of the Nursing Discipline is enacted through a well-established nursing scholar program.
Keywords: Childhood cancer; Pediatric oncology nursing; Cooperative group; Nursing research; Clinical trial; Theoretical framework, Resilience
Historical Background of COG Nursing Discipline
Prior to the merger of the pediatric cooperative groups at the turn of the millennium, leaders of the CCG and POG Nursing Disciplines had begun to explore the feasibility of nursing research collaboration. A series of discussions held in conjunction with CCG and POG group meetings and Association of Pediatric Oncology Nurses (APON; currently the Association of Pediatric Hematology Oncology Nurses) conferences positioned nursing well for the merger by establishing mutual understanding that areas of shared interest outweighed differences across the two groups. CCG and POG nursing leaders recognized the opportunity for nursing to make unique scientific contributions within the COG, and agreed to undertake the first State of the Science Summit in Pediatric Oncology Nursing Research1.
A strength of both nursing groups was strong representation from advanced practice nurses (APNs) who were well integrated into the cooperative group structure, knowledgeable about cooperative group processes, and familiar with protocols2,3. However, the APNs lacked the expertise of doctorally prepared nurse scientists to successfully develop and lead nursing research within the cooperative group structure. At the same time, there was a very small cadre of doctorally prepared pediatric oncology nurse researchers available and they had limited experience working within the cooperative groups. These gaps in nursing intellectual capital led to the development of a research structure that paired APNs who were very familiar with cooperative group processes with doctorally prepared nurses who had expertise in the design and implementation of nursing research. The initial APN/PhD dyads focused on four areas of priority identified during the State of the Science Summit in Pediatric Oncology Nursing and included: neurocognitive effects of childhood cancer therapy4, fatigue and related symptoms5, coping effects of patients and families6, and self-care7. A second group of nursing scholar teams was added in 2005 after a second State of the Science Summit. These included nursing scholars focused on developing research in the areas of end of life/palliative care8, parent treatment decision making9 and complementary and alternative medicine10. Table 1 provides a timeline summarizing development of key COG Nursing Discipline activities.
Table 1.
Nursing Discipline Development Timeline
| Year | Development activity | Comments |
|---|---|---|
| 1955 | Pediatric cooperative groups funded by National Cancer Institute (NCI) | |
| 1979 | Nursing Committee established in Children’s Cancer Group (CCG) | |
| 1981 | Nursing Discipline established in Pediatric Oncology Group (POG) | |
| 1981–1997 | Nursing activities in the pediatric cooperative groups |
|
| 1997 | Initiation of intergroup nursing collaboration (independent of cooperative group merger) | |
| 2000 | Merger of 4 pediatric cooperative groups to form the Children’s Oncology Group (COG) |
|
| 2000 | Inaugural State of the Science in Pediatric Oncology Nursing Research |
|
| 2000-present | Nursing scholars |
|
| 2004 | Second State of the Science in Pediatric Oncology Nursing Research | Added 3 nursing scholar groups: Complementary and Alternative Medicine (CAM), Parent treatment decision making, End of life/Palliative care |
| 2006 | Developing Nurse-Led Interdisciplinary Research in the Cooperative Group Setting | Oncology Nursing Society invitational meeting for interdisciplinary cooperative group teams to develop a nurse-led research study concept. COG team focused on fatigue and related symptoms in Hodgkin Disease. |
| 2008–2012 | Nursing Research Traineeships | Nursing Discipline portion of COG Chair’s grant included funding for developing the next generation of nursing scholars. Three rounds of 2 year traineeships have been awarded to six trainees thus far. |
| 2000-present | Nursing Discipline Protocol Development |
|
| 2007-present | PRO-Resource Center | Nursing Discipline collaborated with Cancer Control Committee to develop a Patient Reported Outcomes (PRO) resource center to advance inclusion of pediatric PROs on disease trials. |
| 2009 | Strategic planning | With expansion of nursing scientists and growing cadre of young investigators, need to move from nursing scholar dyad approach to capitalize on growing network of pediatric oncology nursing scientists – nursing scholar network now open to all interested individuals. Monthly conference calls provide support and networking and identifying promising studies to move forward in group. |
| 2011 | Organizing framework adopted | Strategic planning yielded a number of suggestions including need for an organizing framework to define the focus of Nursing Discipline. |
| 2012 | Evidence-Based Practice initiative | Mentored opportunities for nurses to develop evidence summaries to inform clinical trials nursing practice. |
| 2013-ongoing | Areas for future focus | Current focus on research to inform effective delivery of patient/family education and reducing illness-related distress |
Development of an Organizing Framework for COG Nursing Research
In 2009, the COG Nursing Research Sub-Committee engaged in a strategic planning process that included a comprehensive review of the first decade of the nursing scholar program. During COG’s inaugural decade, nursing scholar teams had variable success in developing concepts for COG research protocols. Two of the 4 original teams successfully implemented COG studies, one as a freestanding protocol (ANUR0631) and one as an embedded aim in a therapeutic protocol (ACNS0331 – refer to Table 1). During this time, group-wide open meetings moved from a semi-annual to an annual schedule due to reduction in cooperative group funding, and changes in the study concept development process required that pilot work, for the most part, be completed outside of the cooperative group, with fully developed clinical trials given primary consideration for conduct within the COG. Since the majority of nursing scholars were young investigators, their programs of research were generally not mature enough to support large scale multi-site clinical trials. These changes needed to be weighed in the strategic planning process to ensure future COG Nursing research success.
The Nursing Research Sub-Committee co-chairs documented all nursing scholar team activities completed to date and conducted individual scholar interviews. Themes from these interviews were presented to the nursing scholars during a strategic planning session at the Fall 2009 group meeting. In general, scholars reported positive experiences within the cooperative group and were in agreement that APN-PhD synergy had been accomplished. However, nurse scientists new to cooperative group procedures identified the added time for cooperative group study concept development and approval (as compared to external funding mechanisms), and the cooperative group oversight required during study implementation and dissemination (as compared to studies conducted independently) as challenging. These challenges were balanced by the extensive expertise and support for multi-site protocol implementation and administrative support provided by the cooperative group. Nurse scientists now incorporate the added time needed for study development, implementation and dissemination to accommodate cooperative group approval processes into their study timelines.
Scholars described facilitators and barriers of developing study concepts into protocols and listed the characteristics of a successful concept, which included having good fit with cooperative group priorities, being a common care problem and a mature idea with completed preliminary data, filling a key knowledge gap, being an elegantly simple idea/intervention and having a champion within the COG disease and/or discipline committee structure. Scholars described the components of a good scholar match and how to define their success in the group; i.e., with the same expectations for all researchers: successful funding and study conduct, and dissemination of findings. Scholars recognized the need to build capacity for the next generation of scholars through mentoring, outreach to doctoral students, and the critical importance of regular cooperative group meeting attendance. Scholars acknowledged that COG was the appropriate venue for Phase III intervention trials and that mechanisms were needed to support pre-COG pilot work. Recommendations included expanding the nursing scholar group to include new members, ensuring multidisciplinary representation, and facilitating the professional development of new PhDs by having the COG nursing scholars serve as a think tank, as well as a sounding board for scientific review and critique.
During the strategic planning session, three key questions were explored: (1) What is one thing we need to do to continue our success? (2) What area might we want to lead as a domain of expertise? and (3) How do we model interdisciplinary work? A key theme that emerged from this process was the need to identify a theoretical framework to help define the scope and sharpen the focus of nursing research within COG. Subsequent discussions highlighted both the promise and potential pitfalls of adopting a theoretical framework. Concerns included the need to align focus and language of the framework with cooperative group priorities, which could potentially exclude future nursing studies if they did not fit the framework. However, the consensus was that the potential gains in terms of advancing science overshadowed potential drawbacks. Terms such as “guiding framework” and “conceptual orientation” were used to describe the emerging picture of the type of organizing framework that would facilitate the focus of nursing research within the cooperative group. Values that guided the development of this framework are listed in Table 2.
Table 2.
Guiding values used to develop a framework for nursing research in the cooperative group.
|
During additional strategic planning discussions, members noted that while the nursing scholars’ research spanned diverse areas within pediatric oncology, a common denominator was the human response to illness. Scholars recognized that their mutual goal was to improve the patient’s and family’s illness experience, and that they shared the belief that coping and even growth was possible throughout the illness trajectory. As the group interacted, members identified resilience as the collective outcome of interest, and noted that Dr. Joan Haase, a member of the nursing scholar group, had developed and tested a resilience model11. A small task force was subsequently convened to develop the organizing framework to guide nursing research within the COG. The 4-member task force worked over 6 months to develop a draft framework that was then presented to the nursing scholar group for consideration.
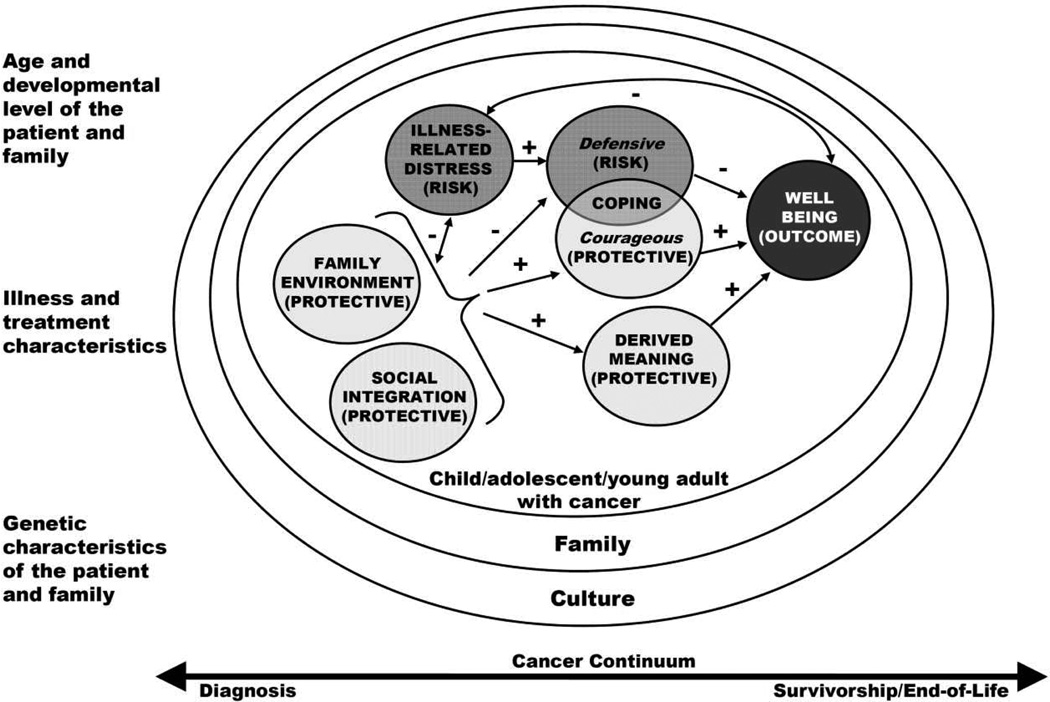
The Resilience in Individuals and Families Affected by Cancer12 (Figure 1) was adapted by the task force from the Resilience in Illness Model (RIM). The RIM was developed from a positive-health perspective that emphasizes the combined contributions of biological, behavioral and psychosocial factors to outcomes of resilience, disease prevention, and wellness13. RIM development and evaluation was accomplished through a series of mixed methods studies of pre-adolescents, adolescents, and young adults with chronic illness, primarily those having cancer11,14–16. Exploratory and confirmatory research indicates RIM well predicts resilience-related outcomes (R2 = 0.62 to 0.72)15. The RIM factors reflected in the COG Nursing research organizing framework are depicted within the inner circle that is focused on the individual. These factors include two risk factors (illness-related risk and defensive coping); four protective factors (family environment, social integration, courageous coping, and derived meaning), and one outcome factor (well-being). The well-being factor includes positive health outcomes such as global quality of life, resilience resolution and self-transcendence. The organizing framework was expanded to incorporate individual biological factors and family factors that are both impacted and have impact on resilience in the child and adolescent/young adult (AYA). Table 3 provides definitions and specific variables associated with each RIM factor incorporated in the COG Nursing research organizing framework. The list of RIM variables in column 3 are those used in the COG studies of interventions to promote AYA resilience; the list will certainly expand as COG Nursing scholars use the framework to guide studies that focus on, or include, physiologic variables, younger children and family units, diverse ethnic/racial groups, and different points on the cancer continuum. The organizing framework for COG Nursing research expanded RIM into an ecological model by adding the family, culture and cancer continuum constructs, as well as moderators (e.g., age and developmental level of the child and family, illness and treatment characteristics, and genetic characteristics of the child and family).
Figure 1. COG Nursing Research Organizing framework.
Adapted from Landier, W., M. Leonard, et al. (2013). "Children's Oncology Group's 2013 blueprint for research: nursing discipline." Pediatr Blood Cancer 60(6): 1031–1036 with permission.
Table 3.
Organizing framework factors originally derived from the Resilience in Illness Model with definition and potential variables for study
| Factor | Definition | Variables | Examples of Potential Additional Variables |
|---|---|---|---|
| Illness-related Distress (Risk) | The degree of perceived illness-related uncertainty and disease and symptom-related distress |
|
Unmet information needs Patient reported outcomes measurement information system PROMIS) measures Depression/anxiety |
| Social Integration (Protective) | The degree to which the patient/family perceives a sense of connectedness with and support from friends and health care providers in the midst of having cancer. |
|
Patient/provider connectedness Patient/parent involvement in treatment decision making Trust in provider |
| Family Environment (Protective) | The degree to which the patient/family member perceives the family as adaptable, cohesive, effectively communicating, and having family strengths. |
|
Psychosocial Assessment Tool risk category Use of standardized family demographics for all COG studies |
| Defensive Coping (Risk) | The degree to which the patient/family member uses evasive and emotive coping strategies to deal with the cancer experience. |
|
|
| Courageous Coping (Protective) | The degree to which the patient/family member uses confrontive, optimistic, and supportant coping strategies to deal with the cancer experience. |
|
Activity during treatment |
| Derived Meaning (Protective) | The degree to which the patient/family member uses hope and spiritual perspective to derive meaning from the cancer experience. |
|
|
| Well-being | The process of identifying or developing resources and strengths to flexibly manage stressors to gain a positive outcome, a sense of confidence/mastery, self-transcendence, and self-esteem. |
|
Health related quality of life |
Scholars were asked to evaluate the framework for fit with their programs of research and to consider how the framework might inform their future research. Concerns voiced by scholars included the framework being too narrow and restrictive, an absence of biological indicators and mechanisms of injury and a focus on the psychosocial concepts of stress and coping. Scholars encouraged a broader view and also discussed ways the framework could be used to interpret the variable symptom patterns identified within specific disease groups. Scholars also encouraged broad definition of outcomes. The potential to identify a core set of measures that could be applied across studies was identified as an opportunity to build science and theory. Scholars discussed a number of potential nursing research priority areas and where each would fit. As the discussion progressed, it became clear that with the fine-tuning reflected in Figure 1, the framework could inform a broad group of research interests. The group also clarified that individual investigators might use other theoretical/conceptual frameworks to guide specific studies, to provide knowledge that would also inform components of the organizing framework.
During a subsequent discussion, one of the scholars presented an emerging research concept within the proposed organizing framework. While this researcher’s program of research was grounded in a different theoretical model, she identified how she could add measures and/or contribute findings to the organizing framework. Through this presentation, scholars were able to visualize how an organizing framework might help COG nursing leaders and grant reviewers better articulate the scientific knowledge being produced by nurses in the cooperative group. The framework was helpful in describing the kind of work nurses do. It outlined nursing’s focus and expertise and framed how nursing research is conducted.
After the organizing framework was endorsed by the nursing scholar group, presentations to the greater COG Nursing Discipline membership and other relevant COG committees were completed to obtain broader feedback. The organizing framework was well received. No changes to the framework were necessary after these presentations; explanatory text was added to the diagram to facilitate stand-alone understanding before posting to the Nursing Discipline website.
Application of the Organizing Framework in COG Nursing Research
There are multiple ways the organizing framework can be used to guide research. In 2001, potential intervention applications of RIM to enhance resilience and well-being in AYA with cancer were proposed during an APON pre-conference workshop11,17. Similar application approaches are being used with the COG organizing framework. Here, we identify four approach options. First, investigators could focus on descriptive and/or theory generating work for a single variable within any risk or protective factors (e.g., symptom clusters within illness-related distress) and use the framework to speak to the larger significance of their work. In such cases, investigators would likely use other frameworks to guide their focused work (e.g., symptom representation, motivational coping, communication theory). Second, investigators could focus on multiple mechanisms within a single factor (e.g., develop a model to specify factors that influence provider-patient connectedness) prior to developing interventions that strengthen social integration to ultimately enhance “downstream” protective and/or risk factors. A third option could be to target multiple factors in the model through a single intervention. An example of this option is ANUR0631, “Stories and Music for Adolescent/Young Adult Resilience During Transplant” (SMART I) (R01NR008583; U10CA098543; U10CA095861). This randomized clinical trial of a therapeutic music video intervention targeted all factors in RIM in a sample of AYA undergoing stem cell transplant. Results showed significant improvements in 3 protective factors and moderate, but non-significant improvement in 2 additional factors. A fourth approach option could be to target one or two factors in the model. The follow-up study for ANUR0631, “Stories through Music for Adolescent/Young Adults and Parents (SMART+P) during Treatment; ANUR 1131” provides an example of this approach (R01CA162181; U10CA098543; U10CA095861). This 2 group randomized controlled trial is in process in a dyadic sample of AYAs with high risk cancer and/or high palliative care needs and one parent. The SMART + P study aims to enhance the family protective factor and also target the middle (family) circle of the COG Nursing research organizing framework by adding a parent focused, nurse delivered intervention to the previously tested therapeutic music therapy intervention the AYA receives.
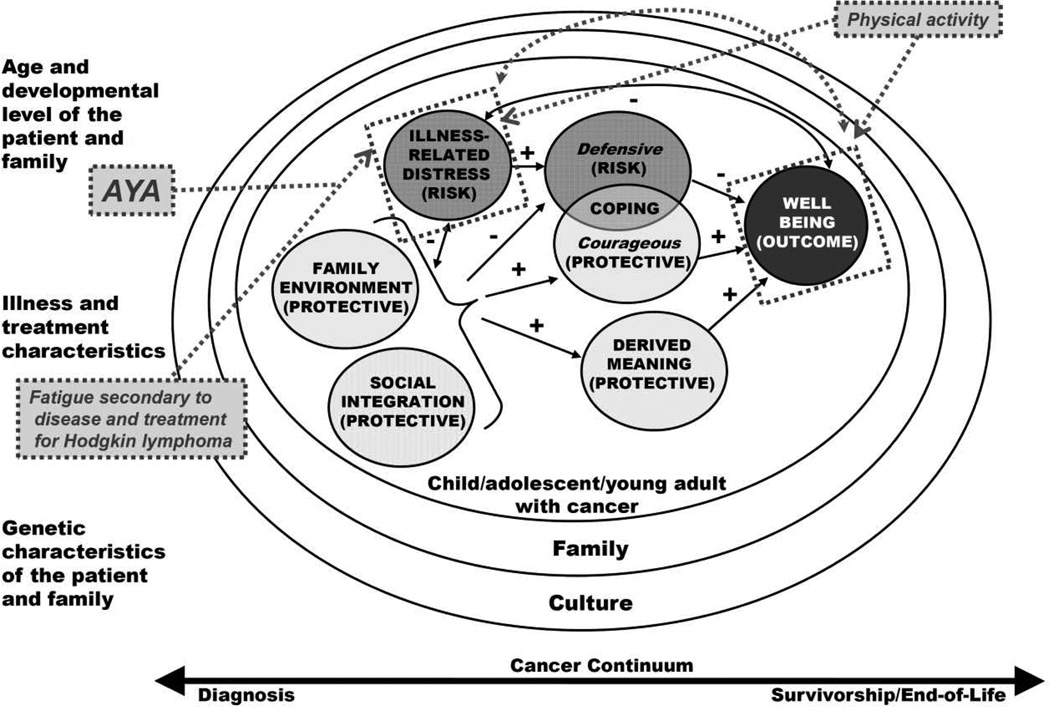
The organizing framework has also informed COG Nursing Research Traineeships. These biennial traineeships, funded by the Nursing Discipline portion of the Chair’s grant, are designed to support the development of young investigators. Traineeship calls are purposefully focused on areas of research in which the discipline leadership wishes to generate interest and focus. Applicants are asked to include how their proposed study is linked to the framework. Figure 2 demonstrates how one trainee’s study, designed to explore the relationship between self-reported fatigue and physical activity in survivors of Hodgkin disease treated as AYA on COG AHOD0331, was linked to aspects of the organizing framework18.
Figure 2. Example of research trainee’s study linkages to the COG Nursing Resarch Organizing Framework.
Used with permission from Catherine Macpherson PhD RN
Since its adoption, the COG Nursing Discipline’s organizing framework has shaped the Discipline’s research agenda by guiding the development of new knowledge through a focus on understanding ways that children and families sustain or regain optimal health when faced with a pediatric cancer diagnosis, and by grounding the Discipline’s research in positive health constructs that set the stage for the development and testing of interventions to promote resilience. The COG Nursing Discipline’s current research agenda, informed by the organizing framework, is described in detail in the Children’s Oncology Group’s 2013 Blueprint for Research: Nursing Discipline12.
Conclusions/Future Directions
The adoption of an organizing framework to guide COG Nursing research is indicative of the transformational change in the Nursing Discipline that has occurred since the merger of the pediatric cooperative groups in 2000. Other indicators of discipline maturity include a recent initiative to develop evidence summaries to translate nursing research into nursing practice, even as COG nurses continue to have a key role in both the development of and effective translation of medical research from “bench to bedside.” Indeed, the majority of pediatric cancer treatment innovations are delivered to patients and families through the hands of a bedside clinical nurse. At the same time, nurses participate in and lead key COG committees, and constitute the largest COG membership category. The successful integration of the Nursing Discipline within the COG, and the resilience-focused organizing framework that has been established to explore and address key gaps in knowledge related to the experience of individuals and families affected by pediatric cancer, may be useful in facilitating collaborative nursing research across cooperative clinical trials groups as cooperative group nursing moves forward within the National Clinical Trials Network (NCTN).
Acknowledgement
COG Nursing Discipline activities reported here were supported by the following grants: 5-U01-CA-13539-28; 5-U10-CA-30969-19; U10CA98543; R13-CA86138; U10CA095861; R01NR008583; R01CA162181
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Katherine Patterson Kelly, Co-chair, Children’s Oncology Group Nursing Research Subcommittee, Nurse Scientist, Children’s National Medical Center, Assistant Clinical Professor, George Washington University, Washington DC, USA.
Mary C. Hooke, Co-chair, Children’s Oncology Group Nursing Research Subcommittee, Assistant Professor, University of Minnesota School of Nursing, Minneapolis, MN, USA.
Kathleen Ruccione, Co-Director, HOPE Program, Children’s Center for Cancer and Blood Diseases, Children’s Hospital Los Angeles, Professor of Clinical Pediatrics, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA.
Wendy Landier, Chair, Children’s Oncology Group Nursing Discipline, Clinical Director, Center for Cancer Survivorship, Assistant Professor, Department of Population Sciences, City of Hope Comprehensive Cancer Center, Duarte, CA, USA.
Joan Haase, Holmquist Professor in Pediatric Oncology Nursing, Co-Director, IUPUI Signature Center: Research in Palliative and End-of-Life Communication and Training, Indiana University School of Nursing, Indianapolis, IN, USA.
References
- 1.Hinds PS, DeSwarte-Wallace J. Positioning nursing research to contribute to the scientific mission of the Pediatric Oncology Cooperative Group. SeminOncol Nuri. 2000;16(4):251–252. doi: 10.1053/sonu.2000.16575. [DOI] [PubMed] [Google Scholar]
- 2.Ruccione KS, Hinds PS, Wallace JD, Kelly KP. Creating a novel structure for nursing research in a cooperative clinical trials group: the Children's Oncology Group experience. Semin Oncol Nurs. 2005;21(2):79–88. doi: 10.1016/j.soncn.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Hinds PS, Baggott C, DeSwarte-Wallace J, et al. Online exclusive: functional integration of nursing research into a pediatric oncology cooperative group: finding common ground. Oncol Nurs Forum. 2003;30(6):E121–E126. doi: 10.1188/03.onf.e121-e126. [DOI] [PubMed] [Google Scholar]
- 4.Moore IM, Espy KA, Kaufmann P, et al. Cognitive consequences and central nervous system injury following treatment for childhood leukemia. Semin Oncol Nurs. 2000;16(4):279–290. doi: 10.1053/sonu.2000.16582. discussion 291-279. [DOI] [PubMed] [Google Scholar]
- 5.Hockenberry-Eaton M, Hinds PS. Fatigue in children and adolescents with cancer: evolution of a program of study. Semin Oncol Nurs. 2000;16(4):261–272. doi: 10.1053/sonu.2000.16577. discussion 272-268. [DOI] [PubMed] [Google Scholar]
- 6.Hinds PS. Fostering coping by adolescents with newly diagnosed cancer. Semin Oncol Nurs. 2000;16(4):317–327. doi: 10.1053/sonu.2000.16590. discussion 328–334. [DOI] [PubMed] [Google Scholar]
- 7.Dodd MJ, Miaskowski C. The PRO-SELF Program: a self-care intervention program for patients receiving cancer treatment. Semin Oncol Nurs. 2000;16(4):300–308. doi: 10.1053/sonu.2000.16586. discussion 308–316. [DOI] [PubMed] [Google Scholar]
- 8.Nuss SL, Hinds PS, LaFond DA. Collaborative clinical research on end-of-life care in pediatric oncology. Semin Oncol Nurs. 2005;21(2):125–134. doi: 10.1016/j.soncn.2004.12.011. discussion 134–144. [DOI] [PubMed] [Google Scholar]
- 9.Stewart JL, Pyke-Grimm KA, Kelly KP. Parental treatment decision making in pediatric oncology. Semin Oncol Nurs. 2005;21(2):89–97. doi: 10.1016/j.soncn.2004.12.003. discussion 98–106. [DOI] [PubMed] [Google Scholar]
- 10.Post-White J, Hawks RG. Complementary and alternative medicine in pediatric oncology. Semin Oncol Nurs. 2005;21(2):107–114. doi: 10.1016/j.soncn.2004.12.007. discussion 115–124. [DOI] [PubMed] [Google Scholar]
- 11.Haase JE. The adolescent resilience model as a guide to interventions. J Pediatr Oncol Nurs. 2004;21(5):289–299. doi: 10.1177/1043454204267922. discussion 300-284. [DOI] [PubMed] [Google Scholar]
- 12.Landier W, Leonard M, Ruccione KS. Children's Oncology Group's 2013 blueprint for research: nursing discipline. Pediatr Blood & Cancer. 2013;60(6):1031–1036. doi: 10.1002/pbc.24415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singer BH, Ryff CD. New horizons in health: an integrative approach. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 14.Haase JE, Heiney SP, Ruccione KS, Stutzer C. Research triangulation to derive meaning-based quality-of-life theory: Adolescent Resilience Model and instrument development. Int J Cancer. 1999:125–131. doi: 10.1002/(sici)1097-0215(1999)83:12+<125::aid-ijc22>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 15.Haase JE, Kintner EK, Monahan PO, Robb SL. The Resilience in Illness Model, Part 1: Exploratory Evaluation in Adolescents and Young Adults With Cancer. Cancer Nurs. 2013 doi: 10.1097/NCC.0b013e31828941bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haase JE. Components of courage in chronically ill adolescents: a phenomenological study. ANS. Advan in Nurs Sci. 1987;9(2):64–80. doi: 10.1097/00012272-198701000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Nelson AE, Haase J, Kupst MJ, Clarke-Steffen L, Brace-O'Neill J. Consensus statements: interventions to enhance resilience and quality of life in adolescents with cancer. J Pediatr Oncol Nurs. 2004;21(5):305–307. doi: 10.1177/1043454204267925. [DOI] [PubMed] [Google Scholar]
- 18.Macpherson C, Hooke MC, Friedman DL, et al. Seattle Children's Research Institute Center for Clinical and Translational Research Science Day. Seattle, WA: 2013. Fatigue and physical activity reported by adolescents and young adults (AYA) treated for Hodgkin Lymphoma: A report from the Children's Oncology Group. [Google Scholar]