Abstract
Objectives
This retrospective study describes the use of acupuncture for adult sickle cell patients in a single institution.
Methods
We identified 47 sickle cell disease (SCD) patients referred for acupuncture at the National Institutes of Health between January, 2005 and September, 2011. All patients were enrolled in a Study of the Natural History of SCD and signed consent. We reviewed patient demographics, location of acupuncture treatment sessions (inpatient versus outpatient), number of sessions received, sites of pain, patient pain reporting, and the use of other complementary therapies.
Results
Of the 47 patients (60% women, median age 36 years) referred for acupuncture, 42 had homozygous SS disease (89%) and 5 had SC disease (11%). Over half of the patients (51%) reported more than 3 sites of pain. Only 24 patients (51%) underwent acupuncture treatment. Of those who elected not to receive acupuncture, a majority (87%) accepted some other forms of complementary therapies. Nine patients underwent only inpatient acupuncture for acute vaso-occlusive crisis (VOC). Eleven patients received only outpatient acupuncture treatment for chronic pain, and four patients received both inpatient and outpatient treatments. For the patients who received inpatient acupuncture treatment for acute VOC, there was a significant reduction of reported pain score immediately after acupuncture treatment with an average pain reduction of 2.1 points on the numeric pain scale (p< 0.0001). Excluding the two outliers, 75% of patients (n=13) in the outpatient setting described their pain as improved compared to prior session.
Discussion
To our knowledge, this is the largest retrospective review of acupuncture use in the sickle cell population. This analysis describes the use of acupuncture and raises the possibility of its use as an adjuvant for pain management in this population. Future clinical trials are needed to evaluate acupuncture’s efficacy and effectiveness for pain management in different treatment settings and for various types of pain etiologies among the sickle cell population.
Keywords: sickle cell, acupuncture, pain management, acute pain, chronic pain
Introduction
Sickle cell disease (SCD) is a recessively inherited genetic disorder caused by a single point mutation in the gene encoding the β-globin chain of hemoglobin (HbS).1 SCD is a broad disease category that includes several hemoglobinopathies characterized by the presence of > 50% hemoglobin S. These disorders can affect both beta chains genes (ie: homozygous Hb SS) or can be double heterozygous, in combination with other abnormal or decreased beta hemoglobin, such as HbSC, or HbSbeta thalassemia. The clinical phenotype generally has a spectrum of decreasing disease severity, homozygous SS >SC> SB+. It is estimated that approximately 100,000 people have SCD in North America, and 1 in 600 African-Americans carries the sickle cell gene. Red blood cells that contain predominantly HbS have abnormal rigidity and membrane properties, and reduced life span, leading to chronic anemia. Vascular endothelial changes facilitate adhesion of sickle erythrocytes (along with other blood cells), release of inflammatory mediators, vaso-occlusion and end organ damage, ultimately shortening the life span of affected individuals.2
Pain is a common feature of SCD. As fetal hemoglobin production diminishes around 6 months of age, pain crises begin and recur unpredictably over a lifetime.3 SCD patients often encounter two types of pain: acute pain from vaso-occlusive crisis (VOC) and chronic pain. Frequent VOCs are associated with early mortality, and they can impact sleep, mood, social role and physical functioning.4 Alterations in peripheral nociceptors or in central pain processing may contribute to an amplification of pain signals manifesting as hyperalgesia, which is frequently observed in adult patients.5
Chronic pain may derive from objective disease complications such as chronic leg ulcers, avascular necrosis and demineralization of lower back, or a less well-understood transformation from persistent repeated acute VOCs into a chronic and intractable pain syndrome.6 Chronic pain in SCD is widespread, with nearly one-third of adults with SCD reporting pain on most days, and most pain exacerbations occurring outside of health care settings.7 Chronic pain has a significant impact on functional status and quality of life.8
Pharmacologic therapies and typically, opioids, are often offered as the preferred treatment modality for acute and chronic pain in SCD patients. The American Pain Society and the American Academy of Pain Medicine concluded that chronic opioid therapy can be an effective therapy for carefully selected and monitored patients with chronic noncancer pain.9 However, opioids are also associated with potentially serious harms, including opioid-related adverse effects and outcomes related to the abuse potential of opioids.9 Furthermore, inadequate pain relief can be just as harmful as the disease itself; the nature of SCD and frequency of pain episodes strongly impact symptom burden, emotional stress, and social functioning and negatively affect quality of life.4,5
Sickle cell experts recommend an interdisciplinary approach to pain management. This includes combining intervention modalities, including both pharmacologic therapy (acetaminophen, NSAIDs, judicious use of opioids) and non-pharmacologic therapy (e.g. heat, massage, relaxation therapies, distraction, self-hypnosis, prayer/meditation, and acupuncture).8
Acupuncture, as described by that National Institutes of Health (NIH), is the practice of insertion of fine needles into predefined acupuncture points to relieve symptoms and improve disease processes.10 Acupuncture has been practiced for thousands of years in China.11 In 1971, James Reston’s description of how acupuncture helped his post-appendectomy discomfort triggered considerable interest in acupuncture in the US.12 The practice of acupuncture is accepted by the NIH Consensus Development Panel as a valid adjunct treatment or an acceptable alternative or may be included in a comprehensive management program for a variety of disorders and pain syndromes.10 Over 3 million American adults are estimated to have received acupuncture treatment annually.13 Chronic pain is the most common reason for people receiving acupuncture.14 Most recently, a meta-analysis found acupuncture to be an effective treatment for 4 chronic pain conditions: back and neck pain, osteoarthritis, chronic headache, and shoulder pain.15
In clinical practice, traditional acupuncturists emphasize “De-Qi” feeling (soreness, numbness, heaviness and distension), which has been found to be associated with acupuncture analgesia following acupuncture manipulation.16 Acupuncture may mediate various pathways in the CNS between afferent impulses from pain regions and impulses from acupoints to alleviate pain. Existing evidence also suggests that diverse signal molecules contribute to mediating acupuncture analgesia, such as opioid peptides (m-, d- and k-receptors), glutamate (NMDA and AMPA/KA receptors), 5-hydroxytryptamine, and cholecystokinin octapeptide. Among these, the opioid peptides and their receptors in Arc-PAG-NRM-spinal dorsal horn pathway play a pivotal role in mediating acupuncture analgesia.16 Other studies on pain such as headache have shown that acupuncture can increase endogenous pain modulating substances, such as beta-endorphins, magnesium, and CSF met-enkephalin.17,18,19
To date, there are limited studies on the usefulness of acupuncture for SCD. For SCD patients who are facing significant distress due to their pain and are not being provided adequate relief with pharmacologic therapy alone, acupuncture could potentially serve as adjuvant therapy for pain management.
Acupuncture has been available to patients at the Clinical Center of the NIH for over a decade as an adjuvant for pain management. The objective of this study is to provide descriptive summaries of baseline characteristics of sickle cell patients referred for acupuncture at the NIH, location of acupuncture treatment sessions (inpatient versus outpatient), number of sessions received, sites of pain, patient pain reporting, and the use of other complementary therapies.
Materials and Methods
Study design
This is a retrospective review of all SCD patients who were referred for acupuncture treatment between January 1, 2005 and September 30, 2011, from the Sickle Cell Vascular Disease Section of the National Heart, Lung, and Blood Institute (NHLBI) at the National Institutes of Health (NIH). All of the patients were enrolled in a study of natural history of sickle cell disease and other hemolytic disorders (ClinicalTrials.gov Identifier: NCT00081523), a study approved by the NHLBI institutional review board. The study was conducted at the NIH Clinical Research Center.
Eligibility and data source
The NIH electronic medical record (EMR), Sunrise Enterprise 5.5, was the data source for inpatient and outpatient acupuncture, and contains demographic characteristics and medical information for all NIH patients. In addition we utilized outpatient medical charts for outpatient acupuncture data. For this retrospective analysis, outpatient and inpatient acupuncture assessed pain over different timeframes. In inpatient acupuncture, pain symptom severity scores were measured immediately pre- and post- treatment. In outpatient acupuncture sessions, symptom outcomes were assessed by evaluating a patient’s current pain experience compared to the prior acupuncture session – usually separated by a span of one week. The purpose of the outpatient documentation system is solely for clinical care, and as such, it is more likely to have missing data and its content is not as systematic as the inpatient documentation system which has both clinical care and research goals integrated at its implementation. For these reasons, we instituted different inclusion and exclusion criteria for the two settings. Eligibility criteria for inpatient and outpatient acupuncture patient records are listed in Table 1.
Table 1.
Eligibility criteria for review of inpatient and outpatient acupuncture data.
| Eligibility for inpatient acupuncture | |
|---|---|
Inclusion criteria:
|
Exclusion criteria:
|
| Eligibility and data source for outpatient acupuncture | |
Inclusion criteria:
|
Exclusion criteria:
|
Inpatient, or acute pain management for VOC
For SCD patients in an inpatient setting, all patients were admitted by the primary sickle cell team for acute VOCs. After initial evaluation and assessment, the primary team would implement pharmacologic therapy typically including patient controlled analgesia (PCA) along with other appropriate treatment for acute VOCs such as intravenous fluids and other supportive treatment.
Patients were referred to pain and palliative care service for further management if either the patients or the providers determined that their pain was inadequately controlled. The pain and palliative care service then further determines whether the patient will benefit from either escalation of pharmacological pain therapy or referral for other complementary therapy such as acupuncture, massage, reiki, hypnosis, or relaxation, etc.
Outpatient or chronic pain management
For SCD patients in the outpatient setting, all patients were evaluated by a primary sickle cell team for initial history and physical exam. The sickle cell team includes hematology/oncology attending, fellow and nurse practitioner. At any point after initial assessment, the primary team may refer patients to the pain and palliative care team if either the patients or the providers assess that their pain is not appropriately treated with the current pharmacologic treatment. The pain and palliative care service evaluates the patient and makes treatment recommendations in conjunction with the patient, which may include escalation of pharmacologic therapy and/or referral for other complementary approaches, such as acupuncture.
Common reasons for acupuncture referral for pain management are as follows: patient and/or provider want to utilize non-pharmacological therapy to minimize use of pharmacotherapy; poorly controlled pain despite optimal opioids and pharmacologic adjuvant therapies; use of opioids and pharmacologic adjuvant therapies limited by medication side effects; patient specifically requests acupuncture; patient has other symptoms such as anxiety, nausea, neuropathy that may benefit from acupuncture.
Acupuncture therapy
Acupuncture therapy was provided by two licensed acupuncturists from the pain and palliative care service at the NIH. One acupuncturist performed acupuncture for all inpatient participants and the other performed acupuncture for all outpatient participants. Acupuncture points and duration of treatment were determined by the acupuncturists and tailored to each patient’s needs. The number of sessions was determined by both the acupuncturist and the patient. A patient has the right to decline acupuncture treatment at any time point.
Acupuncture procedures conformed to NIH clinical care guidelines. Verbal informed consent was obtained prior to performing acupuncture. Per FDA regulations, acupuncture needles were sterile, nontoxic, and labeled for single use by a licensed, NIH-credentialed acupuncture consultant. The acupuncture points for acute pain and chronic pain were selected according to traditional Chinese acupuncture practice.20,21 The points are used to treat generalized pain and include points such as LI4, points on the disease meridians, points of the distant-local pain area, and ash points. Standard sterilization procedures were followed prior to insertion of acupuncture needles. A 30-minute acupuncture session was administered using 0.25mm × 13mm − 40mm steel needles. Hand manipulation was employed to elicit the De-Qi feeling.20,21
Any risk or discomfort associated with inpatient acupuncture treatment was evaluated using the National Cancer Institute Common Terminology Criteria for Adverse Events (Version 2.0).22 The patient was discharged from the Acupuncture consult if: 1) the symptom severity score was 0; 2) the patient was discharged from the hospital or the protocol; 3) the patient’s condition did not allow continued acupuncture.
Pain assessment for inpatient acupuncture
Pain severity was assessed using the 0–10 Numeric Pain Rating Scale.23 Immediately before and after each acupuncture session, patients were asked by the acupuncturist to rate the severity of their pain symptoms on a 0–10 scale, ranging from 0 for “no pain symptoms” to 10 for “worst pain symptoms”. The acupuncturist then documented the pain rating into their progress notes for each of the sessions. Statistical difference for pain intensity was measured using pair t-test methods.
Pain assessment for outpatient acupuncture
At the start of treatment sessions, the acupuncturist documented whether the patient’s pain was improved, stable/unchanged, or worse, compared to their previous session. This type of assessment allows providers to rapidly assess patients’ holistic perception of their pain using themselves as baselines. Descriptive statistics are used to summarize the outpatient findings.
For the purposes of this retrospective study, we defined acupuncture sessions as within the same course of treatment if the sessions were less than 1 month apart. For sessions that are separated by more than 1 month, they were considered separate courses of acupuncture treatments.
Results
Patient characteristics
Out of the 47 patients referred for acupuncture by the pain and palliative team, 42 had sickle cell anemia (HbSS) (89%) and 5 had hemoglobin SC disease (11%). Forty percent were men with median age of 36 years. Over half of the patients (51%) reported more than 3 sites of pain (Table 2).
Table 2.
Characteristics of SCD patients referred for acupuncture and the number of reported sites of pain.
| Characteristic | Patient Data |
|---|---|
| Median Age (Range), years | 36 (19–67) |
| Male | 19/47 (40%) |
| Sickle Cell Anemia(HbSS) | 42/47 (89%) |
| Hemoglobin SC disease | 5/47 (11%) |
| Number of Sites of Pain | |
| 1 | 12/47 (26%) |
| 2 | 11/47 (23%) |
| >3 | 24/47 (51%) |
Treatment characteristics
Of the 47 patients, 24 (51%) underwent acupuncture treatment. Nine patients received inpatient acupuncture only, 11 received outpatient acupuncture only, and 4 patients had both inpatient and outpatient acupuncture (Table 3). It was not documented why the other 23 patients did not receive acupuncture. Of those who did not receive acupuncture, a majority (87%) accepted other alternative forms of complementary therapy (Table 3). Services in addition to acupuncture provided by NIH include the following: massage therapy, music therapy, art therapy, physical therapy, occupational therapy, recreation therapy, spiritual care, recreation therapy, reiki, medical hypnosis, acupressure, and pet therapy.
Table 3.
Description of treatment characteristics for SCD patients referred for acupunctuncture therapy.
| Complementary Therapies For Pain | Patient Data |
|---|---|
| Utilized Acupuncture Therapy? | |
| Yes | 24/47 (51%) |
| Utilized Other Therapies | 20/23 (87%) |
| Location of Acupuncture Sessions | |
| Inpatient Only | 9/24 (37%) |
| Outpatient Only | 11/24 (46%) |
| Both In/Outpatient | 4/24 (17%) |
Inpatient acupuncture experience
Of the 9 patients who only utilized acupuncture during their inpatient stay, all were admitted for acute VOC and were placed on patient controlled analgesia for pain management. Two of 9 patients utilized acupuncture treatment for more than one of their inpatient admissions for pain. The median day of hospitalization when acupuncture was initiated was day 6 of the patient’s inpatient stay.
The median number of acupuncture sessions per patient was 3, with a range of 1–12 for a total of 48 sessions. Numerical pain score was documented for all 48 sessions pre- and post-acupuncture. There was a reduction in pain score reported after all of the sessions, which was, on average a decrease in 2.1 points on the numeric pain scale. The magnitude of the effect of acupuncture was similar whether or not the patient had received a session in a previous hospitalization. When considering all 48 sessions, before and after analysis of pain score was statistically significant with a p< 0.0001. (Figure 1).
Figure 1.
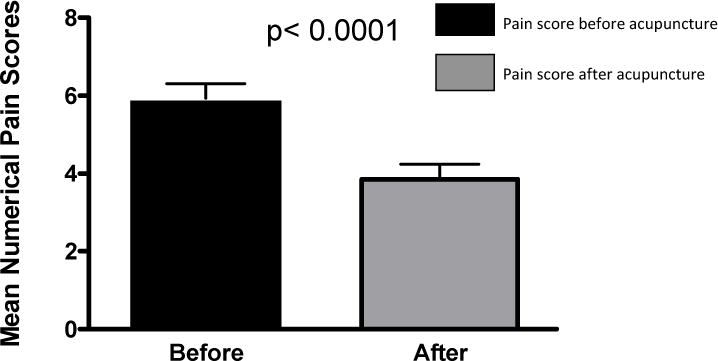
Numerical pain score for all 48 inpatient acupuncture sessions. Black box showed numerical pain score before acupuncture therapy and gray box showed numerical pain score after acupuncture. Numerical pain score prior to acupuncture was significantly decreased immediately after acupuncture treatment (6 vs. 2) with an average pain reduction of 2 points on the numeric pain scale (p< 0.0001).
Outpatient acupuncture experience
All 15 patients who underwent outpatient acupuncture treatments were on chronic opioid therapy at the start of their acupuncture treatments. Four of the 15 patients had both in and outpatient acupuncture treatments for their pain. There were a total of 262 acupuncture treatment sessions between the 15 patients. The median number of sessions per patient was 4, with a wide range of 1 to 131 sessions (Figure 2).
Figure 2.
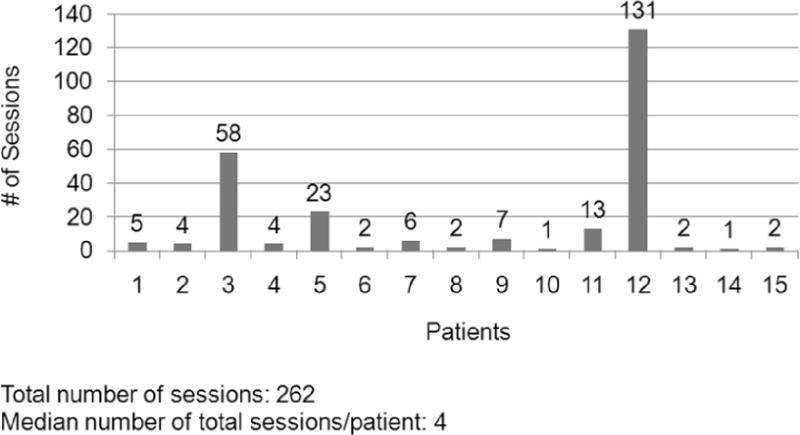
X axis denotes number of patients who received outpatient acupuncture treatments and y axis shows number of sessions received per patient. There were a total of 262 outpatient acupuncture treatment sessions between the 15 patients. The median number of sessions per patient was 4, with a wide range of 1 to 131 sessions.
Out of the 262 acupuncture sessions, we excluded the first session of every course of acupuncture treatment as they could not be compared with prior sessions. This resulted in a total of 231 sessions.
Five of the 15 patients had only 1 session per course of acupuncture, and thus did not contribute to outpatient data. Of the 10 patients who accepted more than 1 session per course of acupuncture, 2 patients, accounted for 79.2% of the 231 sessions. We therefore analyzed the results from these 2 patients separately from the other 8 patients.
Excluding the 2 patients with highest number of sessions, 75% of patients described their pain as improved compared to prior session. In 10.4% of the treatment sessions, their pain was described as stable, and in 10.4% of sessions patient reported pain to be worse. Data were not available for 4.2% of the sessions.
The 2 high-usage patients, who had pain mostly related to chronic ulcers, reported improved pain compared to prior session in 36.1% of sessions, stable pain in 28.5%, and worse pain in 11.5%. Data were not available for 23% of the sessions. Therefore the results of both analyses were not significantly different with or without their inclusion.
Discussion
This single institution retrospective analysis provides informative data on the SCD patients who utilize acupuncture as an adjunctive pain treatment modality. This analysis provides descriptions of acupuncture use during acute VOC and in chronic pain settings.
Little is known about the utility of acupuncture in SCD. To our knowledge, there has only been one study evaluating the use of acupuncture in the sickle cell population. Co et al., evaluated 16 acute painful crises experienced by 10 sickle cell patients. Patients in the study achieved pain relief in 15 of 16 acute pain episodes after receiving acupuncture using either real or sham acupuncture points.24 The authors concluded that the physical insertion of the needle itself may be useful in alleviating pain. Since their study in 1979, we are not aware of any other studies evaluating the use of acupuncture in treatment pain in SCD patients.
Our institution has a longstanding experience with integrating acupuncture as an adjuvant pain therapy, and our current study provides a comprehensive retrospective case report series of acupuncture use among sickle cell patients in outpatient and inpatient settings. Approximately half (51%) of the participants referred for acupuncture received acupuncture treatment. While it was not possible to ascertain why the other half of the patients did not undergo acupuncture, 87% of these patients utilized other forms of complementary therapies in addition to standard pharmacologic treatment. This suggests that many of our participants were open to additional non-pharmacologic interventions for their pain management.
In the inpatient setting, all 9 patients being treated for VOC were receiving what was considered optimal opioid therapy when acupuncture was administered. Overall, there was a mean pain reduction of 2.1 points immediately pre- and post-acupuncture and all patients exhibited a reduction in pain after acupuncture, whether or not it was their first and only time receiving this therapy or the patient had experienced acupuncture before, during a previous hospitalization. It is unclear what the minimal clinically significant difference (MCSD) is on a numeric pain scale for sickle cell patients experiencing a VOC episode. In an Emergency Department study measuring acute pain using the verbal numeric rating scale (0–10), the MCSD was 1.4.25 This degree of change was associated with patients recording their pain as ‘a bit better’ or ‘a bit worse.’ While this study is not specific to sickle cell population and included all adult patients who presented to the Emergency Department with acute pain, it raises the possibility that a 2.1 point reduction may have clinical implications.
In the outpatient setting, there was great variability in the frequency of acupuncture use among the 15 patients. Five patients underwent only one session of acupuncture, while two patients accounted for 79.2% of the total 231 sessions. Prospective studies are needed to discern the reasons for this discrepancy in use, whether it is due to difference in effectiveness of acupuncture for different pain etiologies, variations in patient treatment preferences, or other factors. In the majority of sessions, patients described their pain as improved or stable; however, it is not possible to determine how the outpatient missing pain data affects the results, and whether the data are randomly or systematically absent.
There are limitations to this study that deserve comment. First, as it is a retrospective study, no conclusions can be made regarding the effectiveness of acupuncture – we could not account for potential confounders of pain relief such as analgesic dosage adjustments, placebo effect, pain etiologies, and use of other complementary therapies. Second, we do not have documentation why a number of the patients who were referred for acupuncture declined its service and whether their pain symptoms were comparable to the patients who chose to undergo acupuncture. Third, this study cannot account for reporting bias. Patients may report improved pain response from acupuncture because it is socially desirable (social responsiveness bias). Similarly, patients may systematically inflate their responses in the direction perceived as favorable by the acupuncturist (obsequiousness bias).26 Finally, the number of individuals included in the study was relatively small, and this may be due to in part by the lack of awareness of the potential benefit of acupuncture by the patients and referring providers. Given that there is also a lack of evidence supporting the use of acupuncture in SCD, the primary sickle cell team may also not be mindful in referring patients to the palliative care team for sole purpose of acupuncture.
Despite these limitations, the findings in this study encourage future prospective studies that can address some of these unanswered questions. This retrospective review also highlights the benefits of combining the numerical pain scale (0–10) with clinically relevant descriptors (i.e. my pain is better/same/worse) during pain assessments. This allows for interpretation of changes in numerical data in a clinically meaningful and statistically meaningful manner (i.e. whether a decrease in one point in the numerical pain scale is perceived as ‘the same’ or ‘better.’). Finally, this study can create more awareness for both the providers caring for SCD patients and the patients themselves regarding the potential benefit of acupuncture in treating acute and chronic pain in SCD.
Pain is a common symptom experienced in SCD patients and can have significant impact on symptom burden, emotional stress, social functioning, and negatively affect quality of life.4,5 Although opioids are helpful in alleviating acute and chronic sickle cell pain, they are also associated with potentially serious harm, including opioid-related adverse effects and outcomes related to the abuse potential of opioids.9 More research is needed on the effectiveness of alternative therapies in general, and specifically on acupuncture, as adjunctive tools for pain management in different treatment settings and for various types of pain etiologies among the sickle cell population.
Acknowledgments
Source of funding support received for this work from the National Heart, Lung and Blood Institute Division of Intramural Research (1 ZIA HL006014-04).
References
- 1.Steinberg MH. Sickle Cell Disease. Annals of Internal Medicine. 2011;155:ITC3-1. doi: 10.7326/0003-4819-155-5-201109060-01003. [DOI] [PubMed] [Google Scholar]
- 2.Kato GJ, Gladwin MT, Steinberg MH. Deconstructing sickle cell disease: Reappraisal of the role of hemolysis in the development of clinical subphenotypes. Blood Reviews. 2007;21:37–47. doi: 10.1016/j.blre.2006.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Platt OS, Thorington BD, Brambilla DJ, et al. Pain in Sickle Cell Disease. New England Journal of Medicine. 1991;325:11–6. doi: 10.1056/NEJM199107043250103. [DOI] [PubMed] [Google Scholar]
- 4.Dampier C, LeBeau P, Rhee S, et al. Health-related quality of life in adults with sickle cell disease (SCD): A report from the comprehensive sickle cell centers clinical trial consortium. Am J Hematol. 2011;86:203–5. doi: 10.1002/ajh.21905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benjamin L. Pain Management in Sickle Cell Disease: Palliative Care Begins at Birth? ASH Education Program Book. 2008;2008:466–74. doi: 10.1182/asheducation-2008.1.466. [DOI] [PubMed] [Google Scholar]
- 6.Rees DC, Olujohungbe AD, Parker NE, Stephens AD, Telfer P, Wright J. Guidelines for the management of the acute painful crisis in sickle cell disease. British Journal of Haematology. 2003;120:744–52. doi: 10.1046/j.1365-2141.2003.04193.x. [DOI] [PubMed] [Google Scholar]
- 7.Smith WR, Penberthy LT, Bovbjerg VE, et al. Daily Assessment of Pain in Adults with Sickle Cell Disease. Annals of Internal Medicine. 2008;148:94–101. doi: 10.7326/0003-4819-148-2-200801150-00004. [DOI] [PubMed] [Google Scholar]
- 8.Taylor LEV, Stotts NA, Humphreys J, Treadwell MJ, Miaskowski C. A Review of the Literature on the Multiple Dimensions of Chronic Pain in Adults with Sickle Cell Disease. Journal of Pain and Symptom Management. 2010;40:416–35. doi: 10.1016/j.jpainsymman.2009.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chou R, Fanciullo GJ, Fine PG, et al. Clinical Guidelines for the Use of Chronic Opioid Therapy in Chronic Noncancer Pain. The Journal of Pain. 2009;10:113–30.e22. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Acupuncture NIHCDPo Acupuncture. JAMA: The Journal of the American Medical Association. 1998;280:1518–24. [Google Scholar]
- 11.Sierpina VS, Frenkel MA. Acupuncture: a clinical review. South Med J. 2005;98:330–7. doi: 10.1097/01.SMJ.0000140834.30654.0F. [DOI] [PubMed] [Google Scholar]
- 12.Reston J. Now about my operation in Peking. New York Times. 1971 Jul 26;1971 [Google Scholar]
- 13.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;10:1–23. [PubMed] [Google Scholar]
- 14.Sherman KJ, Cherkin DC, Eisenberg DM, Erro J, Hrbek A, Deyo RA. The Practice of Acupuncture: Who Are the Providers and What Do They Do? The Annals of Family Medicine. 2005;3:151–8. doi: 10.1370/afm.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vickers Aj, C AM, M AC, et al. Acupuncture for chronic pain: Individual patient data meta-analysis. Archives of Internal Medicine. 2012;172:1444–53. doi: 10.1001/archinternmed.2012.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao Z-Q. Neural mechanism underlying acupuncture analgesia. Progress in Neurobiology. 2008;85:355–75. doi: 10.1016/j.pneurobio.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Zhao CH, Stillman MJ, Rozen TD. Traditional and evidence-based acupuncture in headache management: theory, mechanism, and practice. Headache. 2005;45:716–30. doi: 10.1111/j.1526-4610.2005.05139.x. [DOI] [PubMed] [Google Scholar]
- 18.Pintov S, Lahat E, Alstein M, Vogel Z, Barg J. Acupuncture and the opioid system: implications in management of migraine. Pediatr Neurol. 1997;17:129–33. doi: 10.1016/s0887-8994(97)00086-6. [DOI] [PubMed] [Google Scholar]
- 19.Chen B. Effect of acupuncture on serum magnesium level in treatment of migraine. J Tradit Chin Med. 2000;20:126–7. [PubMed] [Google Scholar]
- 20.Cheng X. Chinese Acupuncture and Moxibustion. Beijing: Foreign Languages Press; 1979. [Google Scholar]
- 21.Zhang E. Chinese Acupuncture and Moxibustion. 4. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine; 1992. [Google Scholar]
- 22.Arbuck SG, I S, Setser A, et al. The Revised Common Toxicity Criteria: Version 2.0. In. [Google Scholar]
- 23.McCaffery M, P C. Pain: Clinical Manual. 2. St. Louis: 1999. [Google Scholar]
- 24.Co LL, Schmitz TH, Havdala H, Reyes A, Westerman MP. Acupuncture: An evaluation in the painful crises of sickle cell anaemia. Pain. 1979;7:181–5. doi: 10.1016/0304-3959(79)90009-5. [DOI] [PubMed] [Google Scholar]
- 25.Holdgate A, Asha S, Craig J, Thompson J. Comparison of a verbal numeric rating scale with the visual analogue scale for the measurement of acute pain. Emerg Med (Fremantle) 2003;15:441–6. doi: 10.1046/j.1442-2026.2003.00499.x. [DOI] [PubMed] [Google Scholar]
- 26.Cook C. Mode of administration bias. J Man Manip Ther. 2010;18:61–3. doi: 10.1179/106698110X12640740712617. [DOI] [PMC free article] [PubMed] [Google Scholar]


